Iodine Concentration in Breastmilk and Urine among Lactating Women of Bhaktapur, Nepal
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Ethics
2.3. Urine and Breastmilk Collection
2.4. Analytical Procedures
2.5. Definitions
2.6. Statistical Analysis
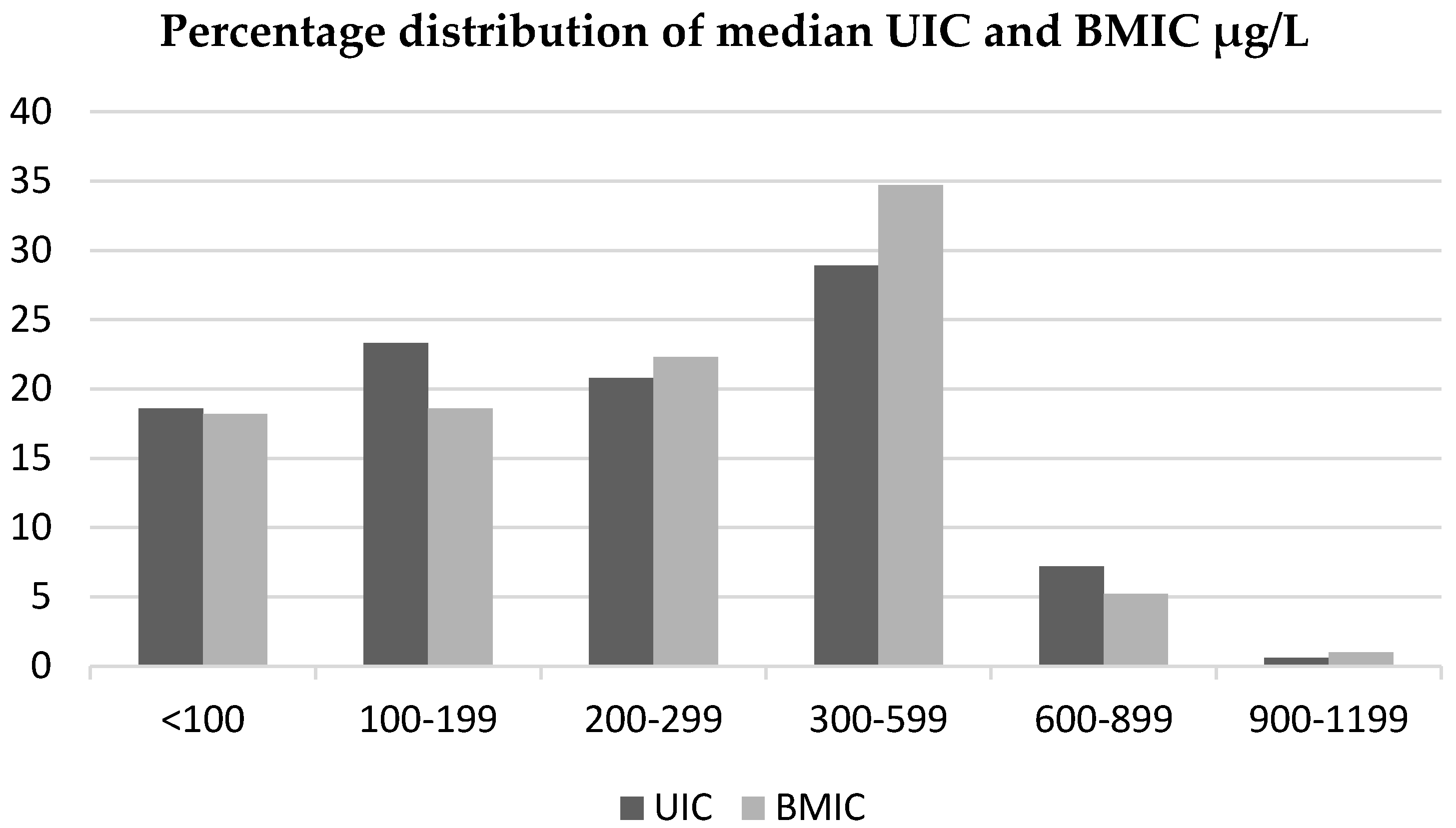
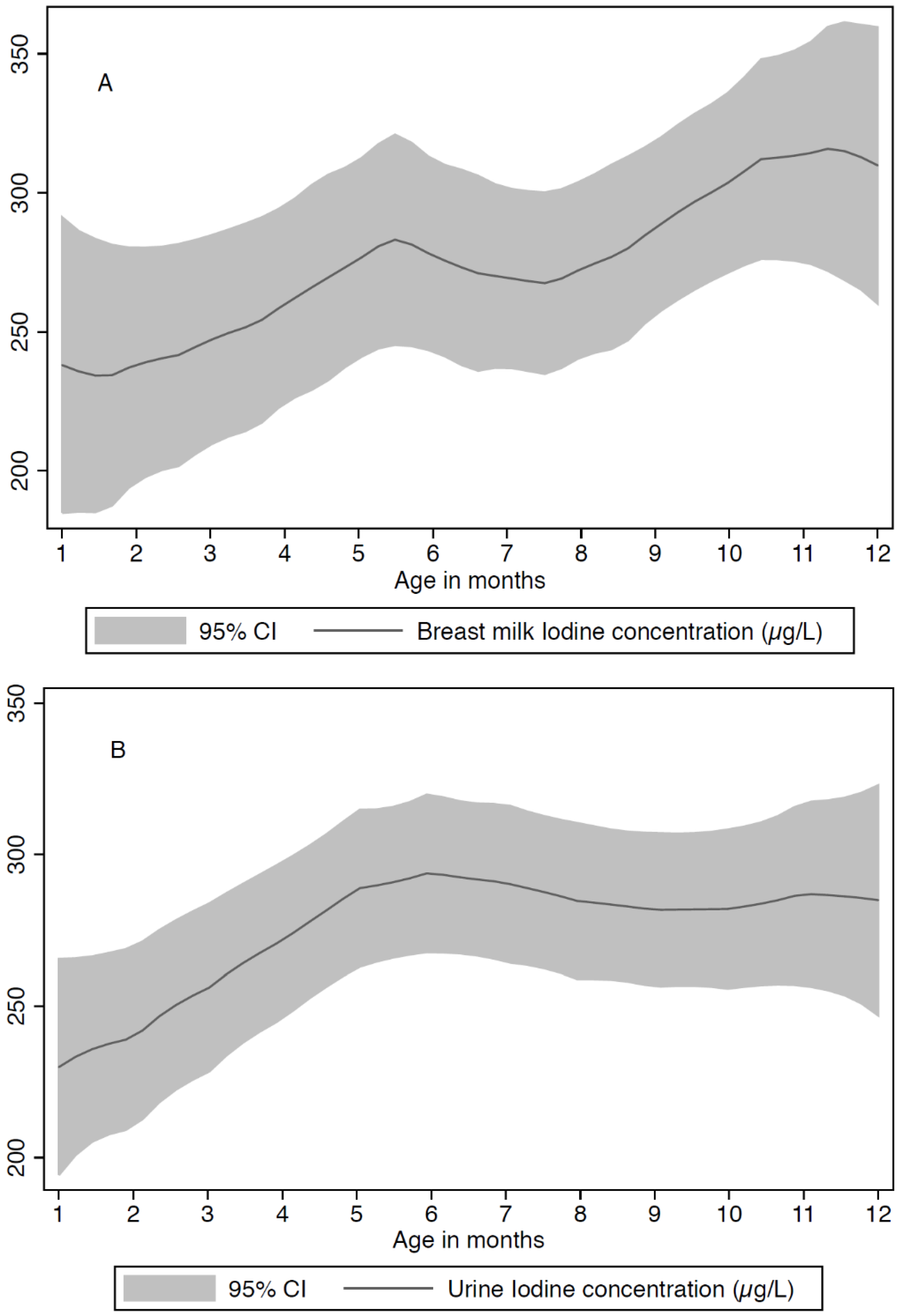
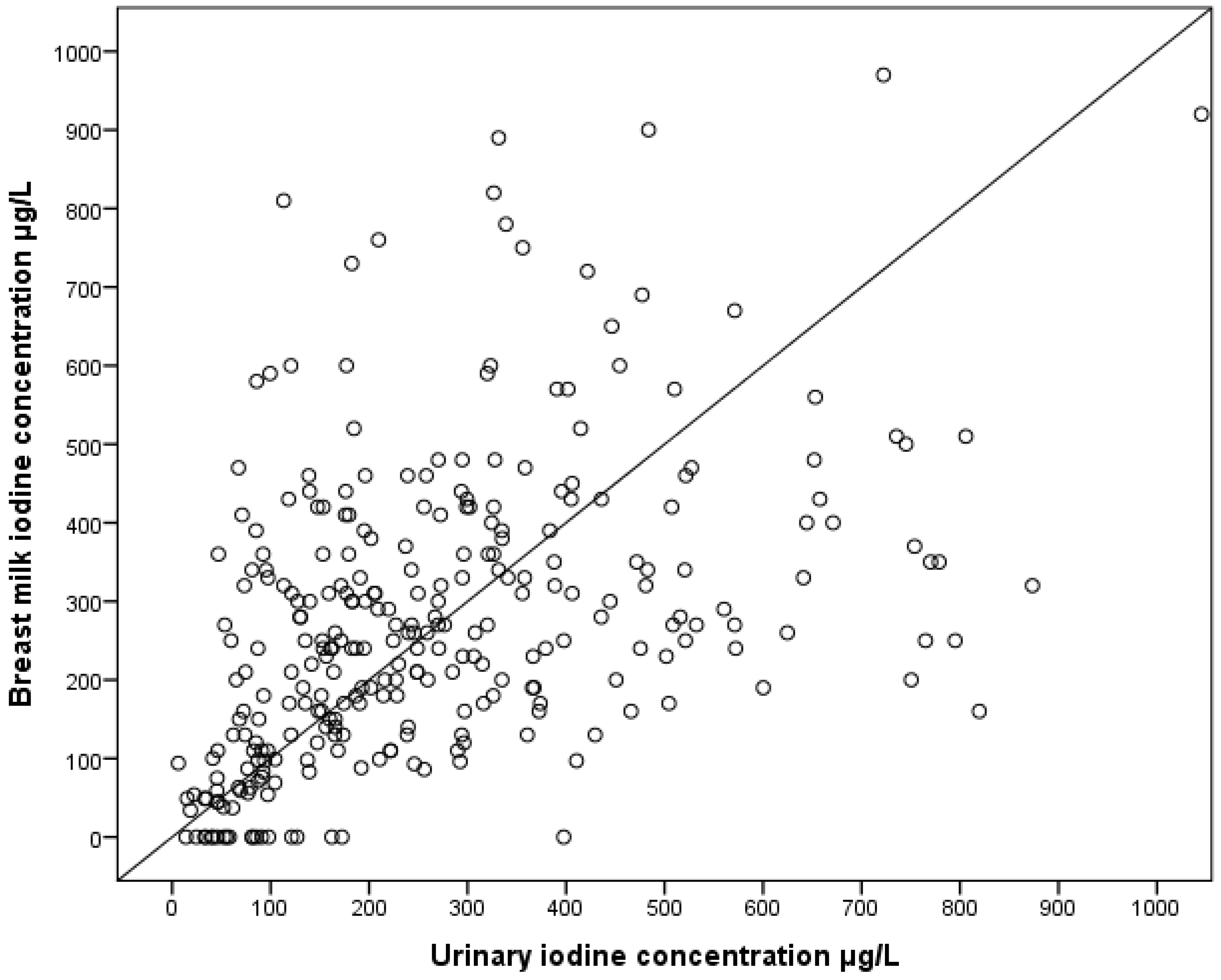
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| BMIC | Breastmilk iodine concentration |
| ERM | European Reference Material |
| IDD | Iodine deficiency disorders |
| ICP-MS | Inductive coupled plasma-mass spectrometry |
| SAC | School aged children |
| UIC | Urinary iodine concentration |
References
- WHO; UNICEF; ICCIDD. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Azizi, F.; Smyth, P. Breastfeeding and maternal and infant iodine nutrition. Clin. Endocrinol. 2009, 70, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Van den Hove, M.F.; Beckers, C.; Devlieger, H.; de Zegher, F.; De Nayer, P. Hormone synthesis and storage in the thyroid of human preterm and term newborns: Effect of thyroxine treatment. Biochimie 1999, 81, 563–570. [Google Scholar] [CrossRef]
- Zimmermann, M.B. Methods to assess iron and iodine status. Br. J. Nutr. 2008, 99, S2–S9. [Google Scholar] [CrossRef] [PubMed]
- Laurberg, P.; Andersen, S.L. Nutrition: Breast milk—A gateway to iodine-dependent brain development. Nat. Rev. Endocrinol. 2014, 10, 134–135. [Google Scholar] [CrossRef] [PubMed]
- Hetzel, B. The Story of Iodine Deficiency: An International Challenge in Nutrition; Oxford University Press: Oxford, UK, 1989. [Google Scholar]
- Ministry of Health and Population. Nepal Demographic and Health Survey; New Era, Calverton, Maryland and Icf International Inc.: Kathmandu, Nepal, 2011.
- Khatiwada, S.; Gelal, B.; Shakya, P.R.; Lamsal, M.; Baral, N. Urinary Iodine Excretion among Nepalese School Children in Terai Region. Indian J. Pediatr. 2016, 83, 15–17. [Google Scholar] [CrossRef] [PubMed]
- Chaudhari, R.K.; Gelal, B.; Brodie, D.A.; Baral, N. Thyroid function and urinary iodine status in primary school age children of the hills and the plains of Eastern Nepal. Indian Pediatr. 2012, 49, 332–333. [Google Scholar] [PubMed]
- Nepal, A.K.; Suwal, R.; Gautam, S.; Shah, G.S.; Baral, N.; Andersson, M.; Zimmermann, M.B. Subclinical Hypothyroidism and Elevated Thyroglobulin in Infants with Chronic Excess Iodine Intake. Thyroid 2015, 25, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Shakya, P.R.; Gelal, B.; Das, B.K.; Lamsal, M.; Pokharel, P.K.; Nepal, A.K.; Brodie, D.A.; Sah, G.S.; Baral, N. Urinary iodine excretion and thyroid function status in school age children of hilly and plain regions of Eastern Nepal. BMC Res. Notes 2015, 8, 374. [Google Scholar] [CrossRef] [PubMed]
- Khatiwada, S.; Lamsal, M.; Gelal, B.; Gautam, S.; Nepal, A.K.; Brodie, D.; Baral, N. Anemia, Iron Deficiency and Iodine Deficiency among Nepalese School Children. Indian J. Pediatr. 2015. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.M.; Braverman, L.E. Consequences of excess iodine. Nat. Rev. Endocrinol. 2014, 10, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Wang, D.; Liu, P.; Meng, F.; Wen, D.; Jia, Q.; Liu, J.; Zhang, X.; Jiang, P.; Shen, H. The relationship between iodine nutrition and thyroid disease in lactating women with different iodine intakes. Br. J. Nutr. 2015, 114, 1487–1495. [Google Scholar] [CrossRef] [PubMed]
- Henjum, S.; Manger, M.; Skeie, E.; Ulak, M.; Thorne-Lyman, A.L.; Chandyo, R.; Shrestha, P.S.; Locks, L.; Ulvik, R.J.; Fawzi, W.W.; et al. Iron deficiency is uncommon among lactating women in urban Nepal, despite a high risk of inadequate dietary iron intake. Br. J. Nutr. 2014, 112, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Valentiner-Branth, P.; Shrestha, P.S.; Chandyo, R.K.; Mathisen, M.; Basnet, S.; Bhandari, N.; Adhikari, R.K.; Sommerfelt, H.; Strand, T.A. A randomized controlled trial of the effect of zinc as adjuvant therapy in children 2–35 mo of age with severe or nonsevere pneumonia in Bhaktapur, Nepal. Am. J. Clin. Nutr. 2010, 91, 1667–1674. [Google Scholar] [CrossRef] [PubMed]
- Milman, N. Postpartum anemia I: Definition, prevalence, causes, and consequences. Ann. Hematol. 2011, 90, 1247–1253. [Google Scholar] [CrossRef] [PubMed]
- Jooste, P.L.; Strydom, E. Methods for determination of iodine in urine and salt. Best Pract. Res. Clin. Endocrinol. Metab. 2010, 24, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Strydom, E.E.; Jooste, P.L. A Modified Microplate Method for the Determination of Urinary Iodine Concentration, in The Challenge of Iodine Deficiency Disorder. A Decade of CDC’s ensuring the Quality of Urinary Iodine Procedures Program. Available online: http://www.cdc.gov/labstandards/pdf/equip/EQUIP_Booklet.pdf (accessed on 26 April 2016).
- Julshamn, K.; Dahl, L.; Eckhoff, K. Determination of iodine in seafood by inductively coupled plasma/mass spectrometry. J. AOAC Int. 2001, 84, 1976–1983. [Google Scholar] [PubMed]
- Ares, S.; Quero, J.; Morreale de Escobar, G. Neonatal iodine deficiency: Clinical aspects. J. Pediatr. Endocrinol. Metab. 2005, 18, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- Delange, F. Requirements of Iodine in Humans. In Iodine Deficiency in Europe: A Continuing Concern; Delange, F., Dunn, J.T., Glinoer, D., Eds.; Plenum Press: New York, NY, USA, 1993; pp. 5–16. [Google Scholar]
- WHO. Nutrient Adequacy of Exclusive Breastfeeding for the Term Infant during the First Six Months of Life; WHO: Geneva, Switzerland, 2002. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes; National Academy Press: Washington, DC, USA, 2006. [Google Scholar]
- WHO. Global Database on Body Mass Index: An Inter-active Surveillance Tool for Monitoring Nutrition Transition 2006; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Dorea, J.G. Iodine nutrition and breast feeding. J. Trace Elem. Med. Biol. 2002, 16, 207–220. [Google Scholar] [CrossRef]
- Semba, R.D.; Delange, F. Iodine in human milk: perspectives for infant health. Nutr. Rev. 2001, 59, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Delange, F. Iodine requirements during pregnancy, lactation and the neonatal period and indicators of optimal iodine nutrition. Public Health Nutr. 2007, 10, 1571–1580. [Google Scholar] [CrossRef] [PubMed]
- Neville, M.C.; Keller, R.; Seacat, J.; Lutes, V.; Neifert, M.; Casey, C.; Allen, J.; Archer, P. Studies in human lactation: Milk volumes in lactating women during the onset of lactation and full lactation. Am. J. Clin. Nutr. 1988, 48, 1375–1386. [Google Scholar] [PubMed]
- Singh, S.; Lamsal, M.; Baral, N.; Bhatta, N.K.; Uprety, D.K. Correlation of Iodine content of mother’s milk and urine with their child’s TSH level. Asian J. Med. Sci. 2015, 7, 40–48. [Google Scholar] [CrossRef]
- WHO Secretariat; Andersson, M.; de Benoist, B.; Delange, F.; Zupan, J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: Conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007, 10, 1606–1611. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Panel on Micronutrients. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; National Academies Press: Washington, DC, USA, 2001. [Google Scholar]
- Ulak, M.; Chandyo, R.K.; Mellander, L.; Shrestha, P.S.; Strand, T.A. Infant feeding practices in Bhaktapur, Nepal: A cross-sectional, health facility based survey. Int. Breastfeed. J. 2012, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.R.; Shin, C.H.; Yang, S.W.; Choi, C.W.; Kim, B.I. Subclinical hypothyroidism in Korean preterm infants associated with high levels of iodine in breast milk. J. Clin. Endocrinol. Metab. 2009, 94, 4444–4447. [Google Scholar] [CrossRef] [PubMed]
- Theodoropoulos, T.; Braverman, L.E.; Vagenakis, A.G. Iodide-induced hypothyroidism: A potential hazard during perinatal life. Science 1979, 205, 502–503. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B. The role of iodine in human growth and development. Semin. Cell Dev. Biol. 2011, 22, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Mahato, R.V.; Nepal, A.K.; Gelal, B.; Poudel, B.; Yadav, B.K.; Lamsal, M. Spectrum of thyroid dysfunction in patients visiting Kantipur Hospital, Kathmandu, Nepal. Mymensingh Med. J. 2013, 22, 164–169. [Google Scholar] [PubMed]
- Schulze, K.J.; West, K.P.; Gautschi, L.A., Jr.; Dreyfuss, M.L.; LeClerq, S.C.; Dahal, B.R.; Wu, L.S.; Khatry, S.K. Seasonality in urinary and household salt iodine content among pregnant and lactating women of the plains of Nepal. Eur. J. Clin. Nutr. 2003, 57, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.M.; Braverman, L.E.; He, X.; Heeren, T.; Pearce, E.N. Breastmilk iodine concentrations following acute dietary iodine intake. Thyroid 2012, 22, 1176–1180. [Google Scholar] [CrossRef] [PubMed]
- Etling, N.; Padovani, E.; Fouque, F.; Tato, L. First-month variations in total iodine content of human breast milks. Early Hum. Dev. 1986, 13, 81–85. [Google Scholar] [CrossRef]
- Mulrine, H.M.; Skeaff, S.A.; Ferguson, E.L.; Gray, A.R.; Valeix, P. Breast-milk iodine concentration declines over the first 6 mo postpartum in iodine-deficient women. Am. J. Clin. Nutr. 2010, 92, 849–856. [Google Scholar] [CrossRef] [PubMed]
- Kirk, A.B.; Dyke, J.V.; Martin, C.F.; Dasgupta, P.K. Temporal patterns in perchlorate, thiocyanate, and iodide excretion in human milk. Environ. Health Perspect. 2007, 115, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, K.L.; Jones, R.; Hollowell, J.G. Urinary iodine concentration: United States National Health and Nutrition Examination Survey 2001–2002. Thyroid 2005, 15, 692–699. [Google Scholar] [CrossRef] [PubMed]
- Molla, G.M.; Arslan, M.I.; Mollah, F.H.; Khan, M.A.H.; Jinnah, C.M.K. Urinary Iodine Excretion of Lactating Mothers Predicts the Iodine Content of Their Breast Milk. J. Enam Med. Col. 2011, 1, 15–18. [Google Scholar]
- Gelal, B.; Chaudhari, R.K.; Nepal, A.K.; Sah, G.S.; Lamsal, M.; Brodie, D.A.; Baral, N. Iodine deficiency disorders among primary school children in eastern Nepal. Indian J. Pediatr. 2011, 78, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Gelal, B.; Aryal, M.; Das, B.K.; Bhatta, B.; Lamsal, M.; Baral, N. Assessment of iodine nutrition status among school age children of Nepal by urinary iodine assay. Southeast Asian J. Trop. Med. Public Health 2009, 40, 538–543. [Google Scholar] [PubMed]
- Khatiwada, S.; Gelal, B.; Gautam, S.; Lamsal, M.; Baral, N. Iodine Status among School Children of remote Hilly regions of Nepal. Indian Pediatr. 2015, 52, 436–437. [Google Scholar] [PubMed]
- Ministry of Health and Population; Department of Health Services; Government of India; Alliance Nepal. National Survey and Impact Study for Iodine Deficiency Disorders (IDD) and Availability of Iodized Salt in Nepal; Government of Nepal: Kathmandu, Nepal, 2007.
- Henjum, S.; Torheim, L.E.; Thorne-Lyman, A.L.; Chandyo, R.; Fawzi, W.W.; Shrestha, P.S.; Strand, T.A. Low dietary diversity and micronutrient adequacy among lactating women in a peri-urban area of Nepal. Public Health Nutr. 2015, 18, 3201–3210. [Google Scholar] [CrossRef] [PubMed]
| Age of women, years (mean, SD) | 25.7 ± 4.1 |
| Age of child, months (mean, SD) | 6.8 ± 3.0 |
| Home delivery, % | 10.1 |
| Parity | |
| One, % | 40.9 |
| Two, % | 41.5 |
| Three or more, % | 17.6 |
| Exclusive breastfeeding 1 3 months, % | 50.2 |
| Exclusive breastfeeding 6 months, % | 16.4 |
| Frequency of breastfeeding (mean, SD) | 9.7 ± 3.4 |
| Body Mass Index (kg/m2) (mean, SD) | 22.4 ± 3.1 |
| <18.5, % | 4.7 |
| 18.5–25, % | 78.7 |
| >25, % | 16.6 |
| Dependent Variables a | Predictor Variables | Unadjusted Beta Coefficients d (95% CI) | p | Adjusted Beta Coefficients d (95% CI) b | p | Stand Beta |
|---|---|---|---|---|---|---|
| BMIC, µg/L | Constant | 5.58 (4.58, 6.59) | ||||
| UIC, µg/L | 0.2 (0.1, 0.2) | 1.0 (0.1, 2.0) | <0.01 | 0.41 | ||
| Time since birth c | 4.0 (1.0, 6.0) | <0.001 | 3.0 (0.2, 5.0) | 0.03 | 0.12 | |
| R2 | 0.26 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Henjum, S.; Kjellevold, M.; Ulak, M.; Chandyo, R.K.; Shrestha, P.S.; Frøyland, L.; Strydom, E.E.; Dhansay, M.A.; Strand, T.A. Iodine Concentration in Breastmilk and Urine among Lactating Women of Bhaktapur, Nepal. Nutrients 2016, 8, 255. https://doi.org/10.3390/nu8050255
Henjum S, Kjellevold M, Ulak M, Chandyo RK, Shrestha PS, Frøyland L, Strydom EE, Dhansay MA, Strand TA. Iodine Concentration in Breastmilk and Urine among Lactating Women of Bhaktapur, Nepal. Nutrients. 2016; 8(5):255. https://doi.org/10.3390/nu8050255
Chicago/Turabian StyleHenjum, Sigrun, Marian Kjellevold, Manjeswori Ulak, Ram K. Chandyo, Prakash S. Shrestha, Livar Frøyland, Emmerentia E. Strydom, Muhammad A. Dhansay, and Tor A. Strand. 2016. "Iodine Concentration in Breastmilk and Urine among Lactating Women of Bhaktapur, Nepal" Nutrients 8, no. 5: 255. https://doi.org/10.3390/nu8050255






