B Vitamins, Homocysteine and Bone Health
Abstract
:1. Introduction
2. Nutrition and B Vitamins
| VIT.B | RDA | UL (≥19 years) | Food | Serving | mcg |
|---|---|---|---|---|---|
| Vitamin B6 | Men: 1.3 mg day−1 (19–50 years), 1.7 mg day−1 (>50 years) Women: 1.3 mg day−1 (19–50 years), 1.5 mg day−1 (>50 years) | Men and Women: 100 mg day−1 | Fortified breakfast cereal | 1 cup | 0.5–2.5 |
| Salmon, wild (cooked) | 3 ounces * | 0.48–0.80 | |||
| Potato, Russet, with skin (baked) | 1 medium | 0.70 | |||
| Turkey, light meat (cooked) | 3 ounces | 0.69 | |||
| Avocado | 1 medium | 0.52 | |||
| Chicken, light meat without skin (cooked) | 3 ounces | 0.51 | |||
| Spinach (cooked) | 1 cup | 0.44 | |||
| Banana | 1 medium | 0.43 | |||
| Dried plums, pitted | 1 cup | 0.36 | |||
| Banana | 1 medium | 0.43 | |||
| Hazelnuts (dry roasted) | 1 ounce | 0.18 | |||
| Vegetable juice cocktail | 6 ounces | 0.13 | |||
| folic acid | Men and women: 400 μg day−1 | Men and women: 1000 μg day−1 | Fortified breakfast cereal | 1 cup | 200–400 |
| Orange juice (from concentrate) | 6 ounces | 83 | |||
| Spinach (cooked) | 1/2 cup | 132 | |||
| Asparagus (cooked) | 1/2 cup (~6 spears) | 134 | |||
| Lentils (cooked) | 1/2 cup | 179 | |||
| Garbanzo beans (cooked) | 1/2 cup | 141 | |||
| Lima beans (cooked) | 1/2 cup | 78 | |||
| Bread | 1 slice | 20 (folic acid) § | |||
| Pasta (cooked) | 1 cup | 60 (folic acid) § | |||
| Rice (cooked) | 1 cup | 60 (folic acid) § | |||
| Vitamin B12 | Men and women: 2.4 μg day−1 | ND | Clams (steamed) | 3 ounces | 84.1 |
| Mussels (steamed) | 3 ounces | 20.4 | |||
| Mackerel (Atlantic, cooked, dry-heat) | 3 ounces * | 16.1 | |||
| Crab (Alaska king, steamed) | 3 ounces | 9.8 | |||
| Beef (lean, plate steak, cooked, grilled) | 3 ounces | 6.9 | |||
| Salmon (chinook, cooked, dry-heat) | 3 ounces | 2.4 | |||
| Rockfish (cooked, dry-heat) | 3 ounces | 1.0 | |||
| Milk (skim) | 8 ounces | 0.9 | |||
| Turkey (cooked, roasted) | 3 ounces | 0.8 | |||
| Brie (cheese) | 1 ounce | 0.5 | |||
| Egg (poached) | 1 large | 0.4 | |||
| Chicken (light meat, cooked, roasted) | 0 ounces | 0.3 |
2.1. Vitamin B6
2.1.1. Food Sources
2.1.2. Supplements
2.2. Folic Acid
2.2.1. Food Sources
2.2.2. Supplements
2.3. Vitamin B12
2.3.1. Food Sources
2.3.2. Supplements
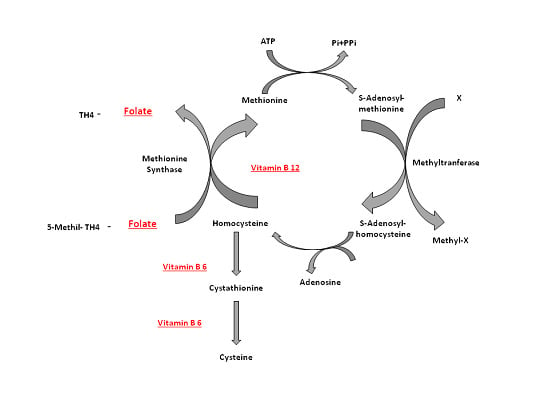
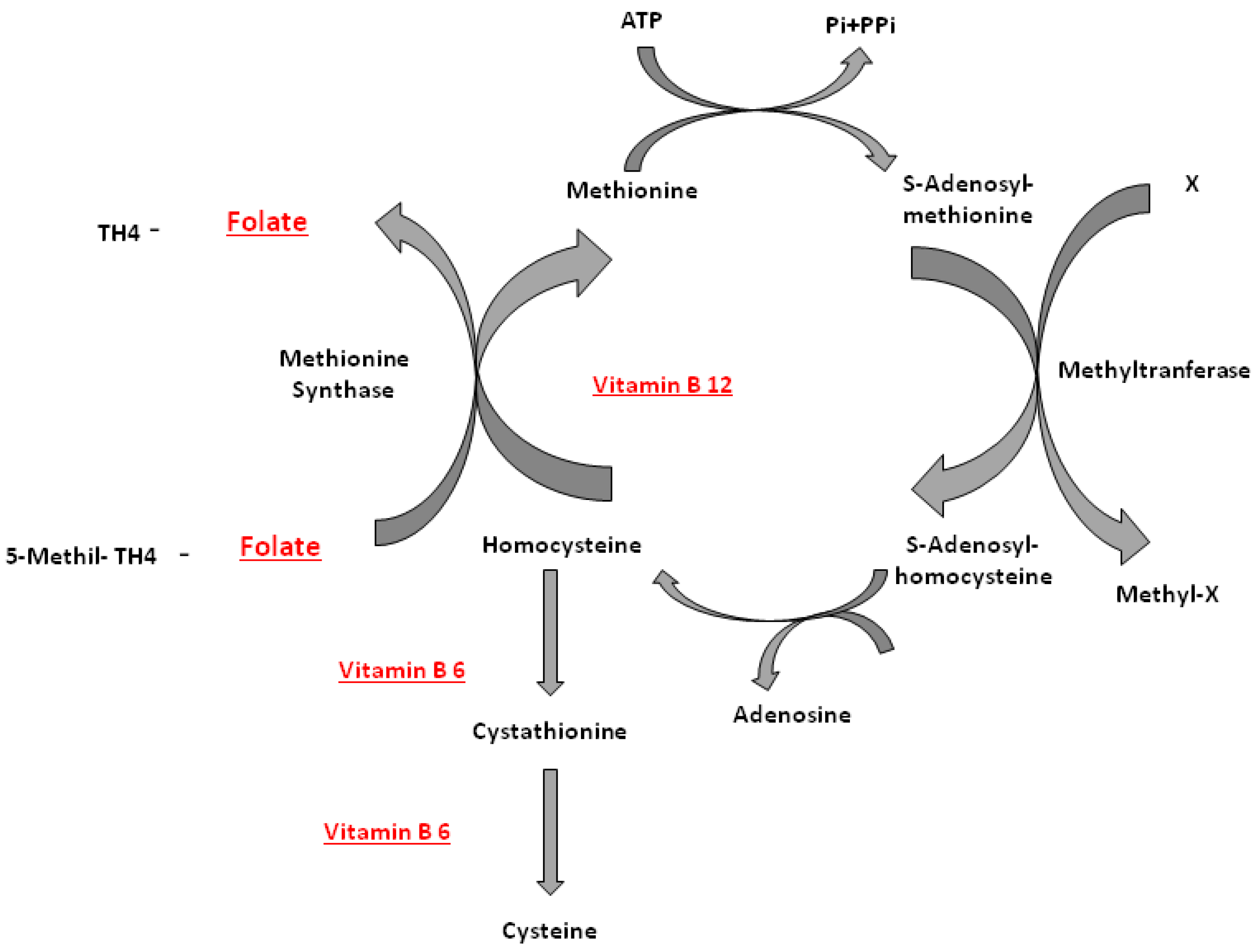
3. Bone, B Vitamins and Homocysteine
Genetic Studies
4. Conclusions
Author Contributions
Conflicts of Interest
References
- Clarke, M.; Ward, M.; Strain, J.J.; Hoey, L.; Dickey, W.; McNulty, H. B-vitamins and bone in health and disease: The current evidence. Proc. Nutr. Soc. 2014, 73, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Van Meurs, J.B.J.; Dhonukshe-Rutten, R.A.M.; Pluijm, S.M.F.; van der Klift, M.; de Jonge, R.; Lindemans, J. Homocysteine levels and the risk of osteoporotic fracture. N. Engl. J. Med. 2004, 350, 2033–2041. [Google Scholar] [CrossRef] [PubMed]
- Van Wijngaarden, J.P.; Doets, E.L.; Szczecińska, A.; Souverein, O.W.; Duffy, M.E.; Dullemeijer, C.; Cavelaars, A.E.; Pietruszka, B.; Van’t Veer, P.; Brzozowska, A.; et al. Vitamin B12, folate, homocysteine, and bone health in adults and elderly people: A systematicreview with meta-analyses. Nutr. Metable 2013, 2013, 486186. [Google Scholar] [CrossRef]
- Scott, J.M. Bioavailability of vitamin B12. Eur. J. Clin. Nutr. 1997, 51, S49–S53. [Google Scholar] [PubMed]
- Carmel, R.; Green, R.; Rosenblatt, D.S.; Watkins, D. Update on cobalamin, folate, and homocysteine. Hematol. Am. Soc. Hematol. Educ. Program. 2003, 2003, 62–81. [Google Scholar] [CrossRef]
- Kanis, J.A.; Johnell, O. Requirements for DXA for themanagement of osteoporosis in Europe. Osteoporos. Int. 2005, 16, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.M.P.; Eslick, G.D.; Nowson, C. Use of calcium or calcium in combination with vitamin D supplementationto prevent fractures and bone loss in people aged 50 years and older: A meta-analysis. Lancet 2007, 370, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Swart, K.M.; van Schoor, N.M.; Lips, P. Vitamin B12, folic acid, and bone. Curr. Osteoporos. Rep. 2013, 11, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, C. Association of MTHFR C667T polymorphism with bone mineral density and fracture risk: An updated meta-analysis. Osteoporos. Int. 2012, 23, 2625–2634. [Google Scholar] [CrossRef] [PubMed]
- Selhub, J.; Jacques, P.F.; Wilson, P.W.F.; Rush, D.; Rosenberg, I.H. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. J. Am. Med. Assoc. 1993, 270, 2693–2698. [Google Scholar] [CrossRef]
- Jacques, P.F.; Bostom, A.G.; Wilson, P.W.F.; Rich, S.; Rosenberg, I.H.; Selhub, J. Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort. Am. J. Clin. Nutr. 2001, 73, 613–621. [Google Scholar] [PubMed]
- Robert, C. Lowering blood homocysteine with folic acid based supplements: Meta-analysis of randomised trials. Homocysteine Lowering Trialists’ Collaboration. BMJ 1998, 316, 894–898. [Google Scholar]
- Herrmann, M.; Widmann, T.; Herrmann, W. Homocysteine—A newly recognised risk factor for osteoporosis. Clin. Chem. Lab. Med. 2005, 43, 1111–1117. [Google Scholar] [PubMed]
- American Cancer Society. Vitamin B Complex. Available online: http://www.cancer.org/treatment/treatmentsandsideeffects/complementaryandalternativemedicine/herbsvitaminsandminerals/vitamin-b-complex (accessed on 17 January 2013).
- Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline; National Academy Press: Washington, DC, USA, 1998; pp. 306–356. [Google Scholar]
- Morris, M.S.; Picciano, M.F.; Jacques, P.F.; Selhub, J. Plasma pyridoxal 5’-phosphate in the US population: The National Health and Nutrition Examination Survey, 2003–2004. Am. J. Clin. Nutr. 2008, 87, 1446–1454. [Google Scholar] [PubMed]
- Clayton, P.T. B6-responsive disorders: A model of vitamin dependency. J. Inherit. Metab. Dis. 2006, 29, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Schaumburg, H.; Kaplan, J.; Windebank, A.; Vick, N.; Rasmus, S.; Pleasure, D.; Brown, M.J. Sensory neuropathy from pyridoxine abuse. A new megavitamin syndrome. N. Engl. J. Med. 1983, 309, 445–448. [Google Scholar] [CrossRef]
- Zhang, X.H.; Ma, J.; Smith-Warner, S.A.; Lee, J.E.; Giovannucci, E. Vitamin B6 and colorectal cancer: Current evidence and future directions. World J. Gastroenterol. 2013, 19, 1005–1010. [Google Scholar] [CrossRef] [PubMed]
- Renwick, A.G. Toxicology of micronutrients: Adverse effects and uncertainty. J. Nutr. 2006, 136, 493S–501S. [Google Scholar] [PubMed]
- Quinlivan, E.P.; McPartlin, J.; McNulty, H. Importance of both folic acid and vitamin B12 in reduction of risk of vascular disease. Lancet 2002, 359, 227–228. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.J.; Bailey, L.; Mulinare, J.; Bower, C. Fortification of flour with folic acid. Food Nutr. Bull. 2010, 31, S22–S35. [Google Scholar] [PubMed]
- Williams, J.; Mai, C.T.; Mulinare, J.; Isenburg, J.; Flood, T.J.; Ethen, M.; Frohnert, B.; Kirby, R.S. Updated estimates of neural tube defects prevented by mandatory folic Acid fortification-United States, 1995–2011. Morb. Mortal. Wkly. Rep. 2015, 64, 1–5. [Google Scholar]
- Pitkin, R.M. Folate and neural tube defects. Am. J. Clin. Nutr. 2007, 85, 285S–288S. [Google Scholar] [PubMed]
- Lupo, P.J.; Goldmuntz, E.; Mitchell, L.E. Gene-gene interactions in the folate metabolic pathway and the risk of conotruncal heart defects. J. Biomed. Biotechnol. 2010, 2010, 630940. [Google Scholar] [CrossRef]
- Antony, A.C. In utero physiology: Role of folic acid in nutrient delivery and fetal development. Am. J. Clin. Nutr. 2007, 85, 598S–603S. [Google Scholar] [PubMed]
- Wien, T.N.; Pike, E.; Wisløff, T.; Staff, A.; Smeland, S.; Klemp, M. Cancer risk with folic acid supplements: A systematic review and meta-analysis. BMJ Open 2012, 2, e000653. [Google Scholar] [CrossRef]
- Food and Agriculture Organization. Human Vitamin and Mineral Requirements; Report of a Joint FAO/WHO Expert Consultation; FAO/WHO Non-Series Publication; Food and Agriculture Organization: Rome, Italy, 2002; pp. 53–62. [Google Scholar]
- Quinlivan, E.P.; Gregory, J.F. Effect of food fortification on folic acid intake in the United States. Am. J. Clin. Nutr. 2003, 77, 221–225. [Google Scholar] [PubMed]
- Heyssel, R.M.; Bozian, R.C.; Darby, W.J.; Bell, M.C. Vitamin B12 turnover in man. Theassimilation of vitamin B12 from natural foodstuff by man and estimates of minimal daily requirements. Am. J. Clin. Nutr. 1966, 18, 176–184. [Google Scholar]
- Stabler, S.P.; Allen, R.H. Vitamin B12 deficiency as a worldwide problem. Annu. Rev. Nutr. 2004, 24, 299–326. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, F. Vitamin B12 sources and bioavailability. Exp. Biol. Med. 2007, 232, 1266–1274. [Google Scholar] [CrossRef]
- Gilsing, A.M.; Crowe, F.L.; Lloyd-Wright, Z. Serum concentrations of Vitamin B12 and folate in British male omnivores, vegetarians and vegans: Results from a cross-sectional analysis of the EPIC-Oxford cohort study. Eur. J. Clin. Nutr. 2010, 64, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Herbert, V. Vitamin B-12. In Present Knowledge in Nutrition, 7th ed.; Ziegler, E.E., Filer, L.J., Eds.; ILSI Press: Washington, DC, USA, 1996; pp. 191–205. [Google Scholar]
- Scalabrino, G. The multi-faceted basis of vitamin B12 (cobalamin) neurotrophism in adult central nervous system: Lessons learned from its deficiency. Prog. Neurobiol. 2009, 88, 203–220. [Google Scholar] [CrossRef] [PubMed]
- Carmel, R. How I treat cobalamin (vitamin B12) deficiency. Blood 2008, 112, 2214–2221. [Google Scholar] [CrossRef] [PubMed]
- Hultdin, J.; van Guelpen, B.; Bergh, A.; Hallmans, G.; Stattin, P. Plasma folate, Vitamin B12, and homocysteine and prostate cancer risk: A prospective study. Int. J. Cancer 2005, 113, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Heaney, R.P.; Abrams, S.; Dawson-Hughes, B. Peak bone mass. Osteoporos. Int. 2000, 11, 985–1009. [Google Scholar] [CrossRef] [PubMed]
- Barker, M.E.; Blumsohn, A. Calcium, vitamin D and weight loss. Br. J. Nutr. 2009, 102, 1538–1538. [Google Scholar] [CrossRef] [PubMed]
- Weaver, C.M. Osteoporosis: The early years. In Nutrition in the Prevention and Treatment of Disease, 2nd ed.; Coulston, A.M., Boushey, C., Eds.; Elsevier Academic Press: Amsterdam, The Netherlands, 2008; pp. 833–851. [Google Scholar]
- Krall, E.A.; Dawson-Hughes, B. Heritable and life-style determinants of bone mineral density. J. Bone Miner. Res. 1993, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, K.E.; Misra, M. Bone Health in Adolescent Athletes with a Focus on Female Athlete Triad. Phys. Sportsmed. 2011, 39, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Karaguzel, G.; Holick, M.F. Diagnosis and treatment of osteopenia. Rev. Endocr. Metab. Disord. 2010, 11, 237–251. [Google Scholar] [CrossRef] [PubMed]
- Dawson-Hughes, B. Calcium and vitamin D for bone health in adults. In Nutrition and Bone Health; Holick, M.F., Dawson-Hughes, B., Eds.; Humana Press: Totowa, NJ, USA, 2004; pp. 197–210. [Google Scholar]
- Touvier, J.; Winzenrieth, R.; Johansson, H.; Roux, J.P.; Chaintreuil, J.; Toumi, H.; Jennane, R.; Hans, D.; Lespessailles, E. Fracture discrimination by combined bone mineral density (BMD) and microarchitectural texture analysis. Calcif. Tissue Int. 2015, 96, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Looker, A.C.; Orwoll, E.S.; Johnston, C.C.J., Jr.; Lindsay, R.L.; Wahner, H.W.; Dunn, W.L. Prevalence of low femoral bone density in older U.S. adults from NHANES III. J. Bone Miner. Res. 1997, 12, 1761–1768. [Google Scholar] [CrossRef]
- Haczynski, J.; Jakimiuk, A. Vertebral fractures: A hidden problem of osteoporosis. Med. Sci. Monit. 2001, 7, 1108–1117. [Google Scholar] [PubMed]
- Cauley, J.A.; Thompson, D.E.; Ensrud, K.C.; Scott, J.C.; Black, D. Risk of mortality following clinical fractures. Osteoporos. Int. 2000, 11, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Johnell, O.; Kanis, J.A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. 2006, 17, 1726–1733. [Google Scholar] [CrossRef] [PubMed]
- Kraft, K. Complementary/alternative medicine in the context of prevention of disease and maintenance of health. Prev. Med. 2009, 49, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Rondanelli, M.; Opizzi, A.; Perna, S.; Faliva, M.A. Update on nutrients involved in maintaining healthy bone. Endocrinol. Nutr. 2013, 60, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, M.; Widmann, T.; Colaianni, G.; Colucci, S.; Zallone, A.; Herrmann, W. Increased osteoclast activity in the presence of increased homocysteine concentrations. Clin. Chem. 2005, 51, 2348–2353. [Google Scholar] [CrossRef] [PubMed]
- Koh, J.; Lee, Y.; Kim, Y. Homocysteine enhances bone resorption by stimulation of osteoclast formation and activity through increased intracellular ROS generation. J. Bone Miner. Res. 2006, 21, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.J.; Koh, J.; Lee, O. Homocysteine enhances apoptosis in human bone marrow stromal cells. Bone 2007, 40, 554–555. [Google Scholar] [CrossRef]
- Liu, G.; Nellaiappan, K.; Kagan, H.M. Irreversible inhibition of lysyl oxidase by homocysteinethiolactone and its selenium and oxygen analogues. Implications for homocystinuria. J. Biol. Chem. 1997, 272, 32370–32377. [Google Scholar]
- Raposo, B.; Rodriguez, C.; Martinez-Gonzalez, J.; Badimon, L. High levels of homocysteine inhibit lysyl oxidase (LOX) and downregulate LOX expression in vascular endothelial cells. Atherosclerosis 2004, 177, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, M.; Schmidt, J.; Umanskaya, N. Stimulation of osteoclast activity by low B-vitamin concentrations. Bone 2007, 41, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Thaler, R.; Agsten, M.; Spitzer, S. Homocysteine suppresses the expression of the collagen cross-linker lysyl oxidase involving IL-6, Fli1, and epigenetic DNA methylation. J. Biol. Chem. 2011, 286, 5578–5588. [Google Scholar] [CrossRef] [PubMed]
- Saito, M.; Fujii, K.; Marumo, K. Degree of mineralizationrelated collagen crosslinking in the femoral neck cancellous bone in cases of hip fracture and controls. Calcif. Tissue Int. 2006, 79, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Neetu, T.; Madhavi, K.; Charu, M.; Jonathan, C.V.; Natia, Q.; Pushpakumar, S.B.; Naria, M.; Suresh, C.T. Homocysteine mediated decrease in bone bloodflowand remodeling: Role of Folic Acid. J. Orthop. Res. 2011, 29, 1511–1516. [Google Scholar] [CrossRef] [PubMed]
- Weiss, N.; Heydrick, S.; Zhang, Y.Y.; Bierl, C.; Cap, A.; Loscalzo, J. Cellular redox state and endothelial dysfunction in mildly hyperhomocysteinemiccystathionine beta-synthase-deficient mice. Arterioscler. Thromb. Vasc. Biol. 2002, 22, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Rodriguez, M.A.; Ruiz-Ramos, M.; Correa-Munoz, E.; Mendoza-Nunez, V.M. Oxidative stress as a risk factor for osteoporosis in elderly Mexicans as characterized by antioxidant enzymes. BMC Musculoskelet. Disord. 2007, 8, 124. [Google Scholar] [CrossRef] [PubMed]
- Clemens, T.L. Vitamin B12 deficiency and bone health. N. Engl. J. Med. 2014, 371, 963–964. [Google Scholar] [CrossRef] [PubMed]
- Roman-Garcia, P.; Quiros-Gonzalez, I.; Mottram, L.; Lieben, L.; Sharan, K.; Wangwiwatsin, A.; Tubio, J.; Lewis, K.; Wilkinson, D.; Santhanam, B.; et al. Vitamin B12-dependent taurine synthesis regulates growth and bone mass. J. Clin. Investig. 2014, 124, 2988–3002. [Google Scholar]
- McLean, R.R.; Jacques, P.F.; Selhub, J. Homocysteine as a predictive factor for hip fracture in older persons. N. Engl. J. Med. 2004, 350, 2042–2049. [Google Scholar] [CrossRef] [PubMed]
- McKusick, V.A. Heritable Disorders of Connective Tissue; CV Mosby: St. Louis, MO, USA, 1966; p. 155. [Google Scholar]
- Lubec, B.; Fang-Kircher, S.; Lubec, T. Evidence for McKusick’s hypothesis of deficient collagen crosslinking in patients with homocystinuria. Biochim. Biophys. Acta 1996, 1315, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Holstein, J.H.; Herrmann, M.; Splett, C.; Herrmann, W.; Garcia, P.; Histing, T.; Klein, M.; Kurz, K.; Siebel, T.; Pohlemann, T.; et al. High bone concentrations of homocysteine are associated with altered bone morphology in humans. Br. J. Nutr. 2011, 106, 378–382. [Google Scholar]
- Vaes, B.L.T.; Lute, C.; van der Woning, S.P.; Piek, E.; Vermeer, J.; Blom, H.J.; Mathers, J.C.; Müller, M.; de Groot, L.C.P.G.M.; Steegenga, W.T. Inhibition of methylation decreases osteoblast differentiation via a non- DNA-dependent methylation mechanism. Bone 2010, 46, 514–523. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, M.; Tami, A.; Wildemann, B.; Wolny, M.; Wagner, A.; Schorr, H.; Taban-Shomal, O.; Umanskaya, N.; Ross, S.; Garcia, P. Hyperhomocysteinemia induces a tissue specific accumulation of homocysteine in bone by collagen binding and adversely affects bone. Bone 2009, 44, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Gjesdal, C.G.; Vollset, S.E.; Ueland, P.M.; Refsum, H.; Meyer, H.E.; Tell, G.S. Plasma homocysteine, folate, and vitamin B 12 and the risk of hip fracture: The hordalandhomocysteine study. J. Bone Miner. Res. 2007, 22, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Gerdhem, P.; Ivaska, K.K.; Isaksson, A. Associations between homocysteine, bone turnover, BMD, mortality, and fracture risk in elderly women. J. Bone Miner. Res. 2007, 22, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Perier, M.A.; Gineyts, E.; Munoz, F.; Sornay-Rendu, E.; Delmas, P.D. Homocysteine and fracture risk in postmenopausal women: The OFELY study. Osteoporos. Int. 2007, 18, 1329–1336. [Google Scholar] [CrossRef] [PubMed]
- Ravaglia, G.; Forti, P.; Maioli, F. Folate, but not homocysteine, predicts the risk of fracture in elderly persons. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1458–1462. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, F.; Samman, S. Vitamin B12 in health and disease. Nutrients 2010, 2, 299–316. [Google Scholar] [CrossRef] [PubMed]
- Holstein, J.H.; Herrmann, M.; Splett, C.; Herrmann, W.; Garcia, P.; Histing, T. Low serum folate and vitamin B-6 are associated with an altered cancellous bone structure in humans. Am. J. Clin. Nutr. 2009, 90, 1440–1445. [Google Scholar] [CrossRef] [PubMed]
- McLean, R.R.; Jacques, P.F.; Selhub, J. Plasma B Vitamins, Homocysteine, and their relation with bone loss and hip fracture in elderly men and women. J. Clin. Endocrinol. Metab. 2008, 93, 2206–2212. [Google Scholar] [CrossRef] [PubMed]
- Carmel, R.; Lau, K.H.; Baylink, D.J.; Saxena, S.; Singer, F.R. Cobalamin and osteoblast-specific proteins. N. Engl. J. Med. 1988, 319, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Dhonukshe-Rutten, R.A.; Pluijm, S.M.; de Groot, L.C.; Lips, P.; Smit, J.H.; van Staveren, W.A. Homocysteine and vitamin B12 status relate to bone turnover markers, broadband ultrasound attenuation, and fractures in healthy elderly people. J. Bone Miner. Res. 2005, 20, 921–929. [Google Scholar] [CrossRef]
- Levasseur, R. Bone tissue and hyperhomocysteinemia. Joint Bone Spine 2009, 76, 234–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofman, A.; van Duijn, C.M.; Franco, O.H.; Ikram, M.A.; Janssen, H.L.; Klaver, C.C.; Kuipers, E.J.; Nijsten, T.E.; Stricker, B.H.; Tiemeier, H.; et al. The Rotterdam Study: 2012 objectives and design update. Eur. J. Epidemiol. 2011, 26, 657–686. [Google Scholar]
- Yazdanpanah, N.; Zillikens, M.C.; Rivadeneira, F.; de Jong, R.; Lindemans, J.; Uitterlinden, A.G.; Pols, H.A.; van Meurs, J.B. Effect of dietary B vitamins on BMD and risk of fracture in elderly men and women: The Rotterdam study. Bone 2007, 41, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, T.; Marshall, P.; Brain, A. Patients with hip fracture may be vitamin B6 deficient. Acta Orthop. Scand. 1992, 63, 635–638. [Google Scholar] [PubMed]
- Gjesdal, C.G.; Vollset, S.E.; Ueland, P.M. Plasma total homocysteine level and bone mineral density—The Hordalandhomocysteine Study. Arch Intern. Med. 2006, 166, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Cagnacci, A.; Bagni, B.; Zini, A.; Cannoletta, M.; Generali, M.; Volpe, A. Relation of folates, vitamin B12 and homocysteine to vertebral bone mineral density change in postmenopausal women. A five-year longitudinal evaluation. Bone 2008, 42, 314–320. [Google Scholar]
- Sleight, P. The HOPE Study (Heart Outcomes Prevention Evaluation). J. Renin Angiotensin Aldosterone Syst. 2000, 1, 18–20. [Google Scholar] [CrossRef] [PubMed]
- Sawka, A.M.; Ray, J.G.; Yi, Q.; Josse, R.G.; Lonn, E. Randomized clinical trial of homocysteine level lowering therapy and fractures. Arch Intern. Med. 2007, 167, 2136–2139. [Google Scholar] [CrossRef] [PubMed]
- Van Wijngaarden, J.P.; Dhonukshe-Rutten, R.A.; van Schoor, N.M.; van der Velde, N.; Swart, K.M.; Enneman, A.W.; van Dijk, S.C.; Brouwer-Brolsma, E.M.; Zillikens, M.C.; van Meurs, J.B.; et al. Rationale and design of the B-PROOF study, a randomized controlled trial on the effect of supplemental intake of Vitamin B12 and folic acid on fracture incidence. BMC Geriatr. 2011, 11. [Google Scholar]
- Van Wijngaarden, J.P.; Swart, K.M.; Enneman, A.W.; Dhonukshe-Rutten, R.A.; van Dijk, S.C.; Ham, A.C.; Brouwer-Brolsma, E.M.; van der Zwaluw, N.L.; Sohl, E.; van Meurs, J.B.; et al. Effect of daily vitamin B-12 and folic acid supplementation on fracture incidence in elderly individuals with an elevated plasma homocysteine concentration: B-PROOF, a randomized controlled trial. Am. J. Clin. Nutr. 2014, 100, 1578–1586. [Google Scholar]
- Gommans, J.; Yi, Q.; Eikelboom, J.W.; Hankey, G.J.; Chen, C.; Rodgers, H. The effect of homocysteine-lowering with B-vitamins on osteoporotic fractures inpatients with cerebrovascular disease: Substudyof VITATOPS, a randomised placebo-controlled trial. BMC Geriatr. 2013, 13, 88. [Google Scholar] [CrossRef] [PubMed]
- Hong, X.; Hsu, Y.H.; Terwedow, H.; Tang, G.; Liu, X.; Jiang, S.; Xu, X.; Xu, X. Association of the methylenetetrahydrofolatereductase C677T polymorphism and fracture risk in Chinese postmenopausal women. Bone 2007, 40, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Riancho, J.A.; Valero, C.; Zarrabeitia, M.T. MTHFR polymorphism and bone mineral density: Meta-analysis of published studies. Calcif. Tissue Int. 2006, 79, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Green, T.; McMahon, J.; Skeaff, C. Lowering homocysteine with B Vitamins has no effect on biomarkers of bone turnover in older persons: A 2-y randomized controlled trial. Am. J. Clin. Nutr. 2007, 85, 460–464. [Google Scholar] [PubMed]
- Sato, Y.; Honda, Y.; Iwamoto, J.; Kanoko, T.; Satoh, K. Effect of folate and mecobalamin on hip fractures in patients with stroke: A randomized controlled trial. JAMA 2005, 293, 1082–1088. [Google Scholar] [CrossRef] [PubMed]
- Malinow, M.R.; Bostom, A.G.; Krauss, R.M. Homocyst(e)ine, diet, and cardiovascular diseases: A statement for healthcare professionals from the Nutrition Committee, American Heart Association. Circulation 1999, 99, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Frosst, P.; Blom, H.J.; Milos, R.; Goyette, P.; Sheppard, C.A.; Matthews, R.G.; Boers, G.J.; den Heijer, M.; Kluijtmans, L.A.; van den Heuvel, L.P.; et al. A candidate genetic risk factor for vascular disease: A common mutation in methylenetetrahydrofolatereductase. Nat. Genet. 1995, 10, 111–113. [Google Scholar]
- Molloy, A.; Daly, S.; Mills, J. Thermolabile variant of 5,10-methylenetetrahydrofolate reductase associated with low red-cell folates: Implications for folate intake recommendations. Lancet 1997, 349, 1591–1593. [Google Scholar] [CrossRef] [PubMed]
- Casas, J.P.; Bautista, L.E.; Smeeth, L.; Sharma, P.; Hingorani, A.D. Homocysteine and stroke: Evidence on a causal link from mendelianrandomisation. Lancet 2005, 365, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Reilly, R.; McNulty, H.; Pentieva, K.; Strain, J.J.; Ward, M. MTHFR 677TT genotype and disease risk: Is there a modulating role for B-Vitamins? Proc. Nutr. Soc. 2014, 73, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Chen, Z.; Rozen, R. Effects of common polymorphisms on the properties of recombinant human methylenetetrahydrofolatereductase. Proc. Natl. Acad. Sci. USA 2001, 98, 14853–14858. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, H.M.; McGuigan, F.E.; Fraser, W.D.; New, S.A.; Ralston, S.H.; Reid, D.M. Methylenetetrahydrofolatereductase polymorphism interacts with riboflavin intake to influence bone mineral density. Bone 2004, 35, 957–964. [Google Scholar] [CrossRef] [PubMed]
- McLean, R.R.; Karasik, D.; Selhub, J. Association of a common polymorphism in the methylenetetrahydrofolatereductase (MTHFR) gene with bone phenotypes depends on plasma folate status. J. Bone Miner. Res. 2004, 19, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsen, B.; Madsen, J.S.; Tofteng, C.L.; Stilgren, L.; Bladbjerg, E.M.; Kristensen, S.R; Brixen, X.; Mosekilde, L. Are effects of MTHFR (C677T) genotype on BMD confined to women with low folate and riboflavin intake? Analysis of food records from the Danish osteoporosis prevention study. Bone 2005, 36, 577–583. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fratoni, V.; Brandi, M.L. B Vitamins, Homocysteine and Bone Health. Nutrients 2015, 7, 2176-2192. https://doi.org/10.3390/nu7042176
Fratoni V, Brandi ML. B Vitamins, Homocysteine and Bone Health. Nutrients. 2015; 7(4):2176-2192. https://doi.org/10.3390/nu7042176
Chicago/Turabian StyleFratoni, Valentina, and Maria Luisa Brandi. 2015. "B Vitamins, Homocysteine and Bone Health" Nutrients 7, no. 4: 2176-2192. https://doi.org/10.3390/nu7042176