The Controversial Role of Food Allergy in Infantile Colic: Evidence and Clinical Management
Abstract
:1. Introduction
2. Evidence
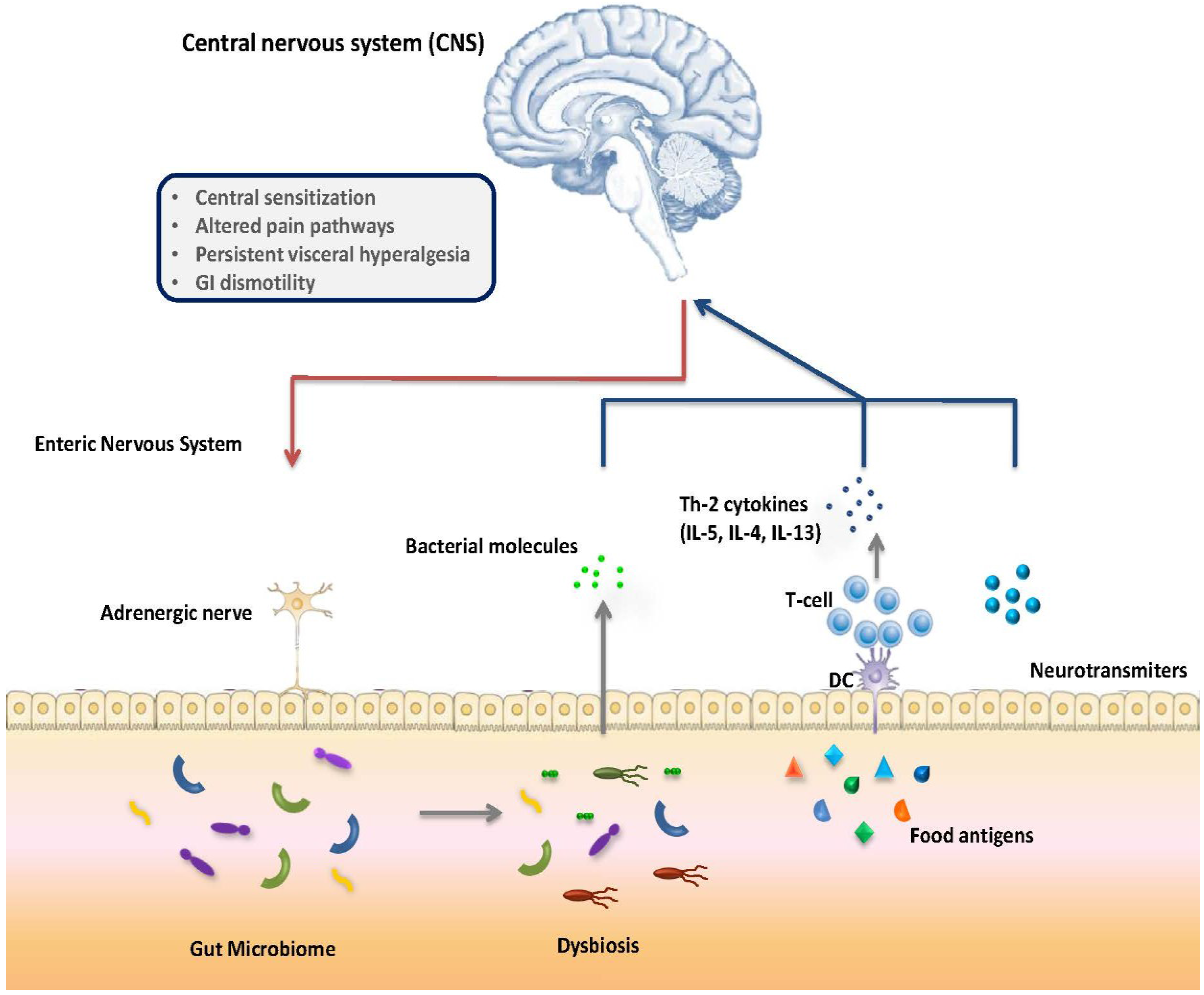
2.1. Dysmotility and Dysbiosis
2.2. Dietary Intervention
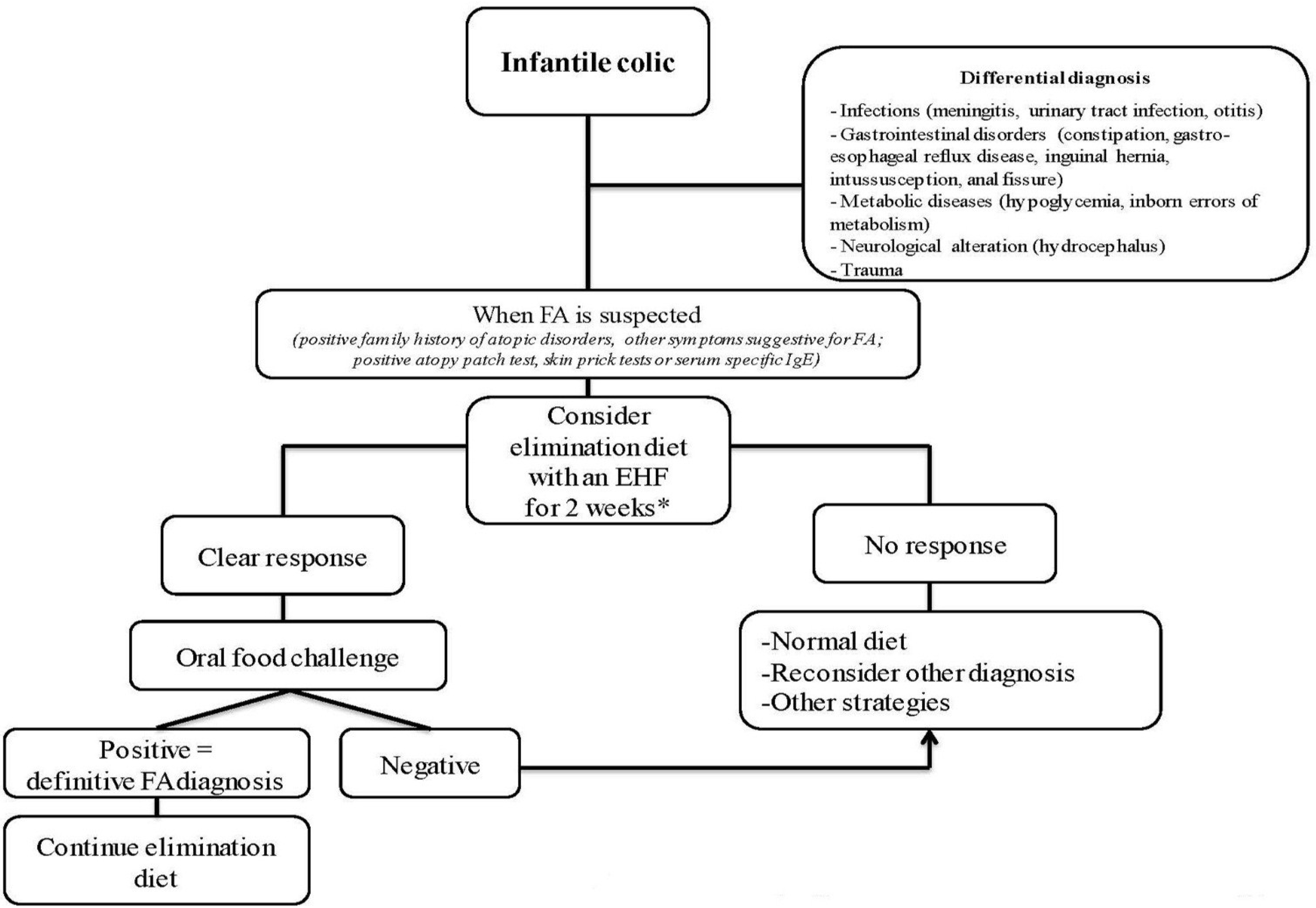
2.3. The Management of an Infant with Suspected FA-Induced IC
2.4. Dietary Approach
3. Conclusions
Author Contributions
Conflicts of Interest
References
- Nwaru, B.I.; Hickstein, L.; Panesar, S.S.; Muraro, A.; Werfel, T.; Cardona, V.; Dubois, A.E.J.; Halken, S.; Hoffmann-Sommergruber, K.; Poulsen, L.K.; et al. The epidemiology of food allergy in Europe: A systematic review and meta-analysis. Allergy 2014, 69, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Prescott, S.L.; Pawankar, R.; Allen, K.J.; Campbell, D.E.; Sinn, J.K.H.; Fiocchi, A.; Ebisawa, M.; Sampson, H.A.; Beyer, K.; Lee, B.W. A global survey of changing patterns of food allergy burden in children. World Allergy Organ. J. 2013, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Høst, A. Frequency of cow’s milk allergy in childhood. Ann. Allergy Asthma Immunol. 2002, 89, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Muraro, A.; Werfel, T.; Hoffmann-Sommergruber, K.; Roberts, G.; Beyer, K.; Bindslev-Jensen, C.; Cardona, V.; Dubois, A.; duToit, G.; Eigenmann, P.; et al. EAACI food allergy and anaphylaxis guidelines: Diagnosis and management of food allergy. Allergy 2014, 69, 1008–1025. [Google Scholar] [CrossRef] [PubMed]
- Lack, G.J. Update on risk factors for food allergy. Allergy Clin. Immunol. 2012, 129, 1187–1197. [Google Scholar] [CrossRef]
- Leonardi, S.; Pecoraro, R.; Filippelli, M.; del Giudice, M.M.; Marseglia, G.; Salpietro, C.; Arrigo, T.; Stringari, G.; Ricò, S.; La Rosa, M.; et al. Allergic reactions to foods by inhalation in children. All Asthma Proc. 2014, 35, 288–294. [Google Scholar] [CrossRef]
- Hyman, P.E.; Milla, P.J.; Benninga, M.A.; Davidson, G.P.; Fleisher, D.F.; Taminiau, J. Childhood functional gastrointestinal disorders: Neonate/toddler. Gastroenterology 2006, 130, 1519–1526. [Google Scholar] [CrossRef] [PubMed]
- De Weerth, C.; Fuentes, S.; de Vos, W.M. Crying in infants: On the possible role of intestinal microbiota in the development of colic. Gut Microbes 2013, 4, 416–421. [Google Scholar]
- Roberts, D.M.; Ostapchuk, M.; O’BRIEN, J.G. Infantile colic. Am. Fam. Phys. 2004, 70, 735–740. [Google Scholar]
- Vandenplas, Y.; Gutierrez-Castrellon, P.; Velasco-Benitez, C.; Palacios, J.; Jaen, D.; Ribeiro, H.; Shek, L.P.; Lee, B.W.; Alarcon, P. Practical algorithms for managing common gastrointestinal symptoms in infants. Nutrition 2013, 29, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Akhavein, M.A.; Patel, N.R.; Muniyappa, P.K.; Glover, S.C. Allergic mastocytic gastroenteritis and colitis: An unexplained etiology in chronic abdominal pain and gastrointestinal dysmotility. Gastroenterol. Res. Pract. 2012, 2012, 950582. [Google Scholar] [CrossRef] [PubMed]
- Valeur, J.; Lappalainen, J.; Rita, H.; Lin, A.H.; Kovanen, P.T.; Berstad, A.; Eklund, K.K.; Vaali, K. Food allergy alters jejunal circular muscle contractility and induces local inflammatory cytokine expression in a mouse model. BMC Gastroenterol. 2009, 9, 33. [Google Scholar] [CrossRef]
- Murch, S. Allergy and intestinal dysmotility—Evidence of genuine causal linkage? Curr. Opin. Gastroenterol. 2006, 22, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Thompson-Chagoyan, O.C.; Fallani, M.F.; Maldonado, J.; Vieites, J.M.; Khanna, S.; Edwards, C.; Doré, J.; Gil, A. Faecal microbiota and short-chain fatty acid levels in faeces from infants with cow’s milk protein allergy. Int. Arch. Allergy Immunol. 2011, 156, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Lozinsky, A.C.; Morais, M.B. Eosinophilic colitis in infants. J. Pediatr. 2014, 90, 16–21. [Google Scholar] [CrossRef] [Green Version]
- Hill, D.J.; Roy, N.; Heine, R.G.; Hosking, C.S.; Francis, D.E.; Brown, J.; Speirs, B.; Sadowsky, J.; Carlin, J.B. Effect of a low-allergen maternal diet on colic among breastfed infants: A randomized, controlled trial. Pediatrics 2005, 116, e709. [Google Scholar] [CrossRef] [PubMed]
- De Weerth, C.; Fuentes, S.; Puylaert, P.; de Vos, W.M. Intestinal microbiota of infants with colic: Development and specific signatures. Pediatrics 2013, 131, e550–e558. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.J.; Hudson, I.L.; Sheffield, J.; Shelton, M.J.; Menahem, S.; Hosking, C.S. A low allergen diet is a significant intervention in infantile colic: Results of a community-based study. J. Allergy Clin. Immunol. 1995, 96, 886–892. [Google Scholar] [CrossRef] [PubMed]
- Jakobsson, I.; Lothe, L.; Ley, D.; Borschel, M.W. Effectiveness of casein hydrolysate feedings in infants with colic. Acta Paediatr. 2000, 89, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Ravelli, A.M.; Tobanelli, P.; Steffen, R.M.; Banez, G.A. Vomiting and gastric motility in infants with cow’s milk allergy. J. Pediatr. Gastroenterol. Nutr. 2001, 32, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Nowak-Wegrzyn, A.; Muraro, A. Food protein-induced enterocolitis syndrome. Curr. Opin. Allergy Clin. Immunol. 2009, 9, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.C.; Tsai, C.L.; Yang, Y.J.; Yang, S.S.; Wang, L.H.; Lee, C.T.; Jan, R.L.; Wang, J.Y. Allergic colitis in infants related to cow’s milk: Clinical characteristics, pathologic changes, and immunologic findings. Pediatr. Neonatol. 2013, 54, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Morita, H.; Nomura, I.; Orihara, K.; Yoshida, K.; Akasawa, A.; Tachimoto, H.; Ohtsuka, Y.; Namai, Y.; Futamura, M.; Shoda, T.; et al. Antigen-specific T-cell responses in patients with non-IgE mediated gastrointestinal food allergy are predominantly skewed to T(H)2. J. Allergy Clin. Immunol. 2013, 131, 590–592. [Google Scholar] [CrossRef] [PubMed]
- Saps, M.; Lu, P.; Silvana, B. Cow’s-milk allergy is a risk factor for the development of FGIDs in children. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Saavedra, Y.; Vergara, P. Hypersensitivity to ovalbumin induces chronic intestinal dysmotility and increases the number of intestinal mast cells. Neurogastroenterol. Motil. 2005, 17, 112–122. [Google Scholar] [CrossRef] [PubMed]
- Wood, J.D. Histamine, mast cells, and the enteric nervous system in the irritable bowel syndrome, enteritis, and food allergies. Gut 2006, 55, 445–447. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, S.M.; Hyland, N.P.; Dinan, T.G.; Cryan, J.F. Maternal separation as a model of brain-gut axis dysfunction. Psychopharmacology 2011, 214, 71–88. [Google Scholar] [CrossRef] [PubMed]
- Mayer, E.A. Gut feelings: The emerging biology of gut-brain communication. Nat. Rev. Neurosci. 2011, 12, 453–466. [Google Scholar] [CrossRef] [PubMed]
- Rhee, S.H.; Pothoulakis, C.; Mayer, E.A. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 306–314. [Google Scholar] [CrossRef] [PubMed]
- El-Salhy, M. Irritable bowel syndrome: Diagnosis and pathogenesis. World J. Gastroenterol. 2012, 18, 5151–5163. [Google Scholar] [CrossRef] [PubMed]
- El-Salhy, M.; Seim, I. Irritable bowel syndrome: The role of gut neuroendocrine peptides. Front. Biosci. 2012, 4, 2783–2800. [Google Scholar] [CrossRef]
- Verdú, E.F.; Bercik, P.; Chopin, L.; Gundersen, D.; Hatlebakk, J.G.; Hausken, T. Specific probiotic therapy attenuates antibiotic induced visceral hypersensitivity in mice. Gut 2006, 55, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Bercik, P.; Verdú, E.F.; Foster, J.A.; Lu, J.; Scharringa, A.; Kean, I.; Wang, L.; Blennerhassett, P.; Collins, S.M. Role of gut-brain axis in persistent abnormal feeding behavior in mice following eradication of Helicobacter pylori infection. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 296, R587–R594. [Google Scholar] [CrossRef] [PubMed]
- Ibeakanma, C.; Miranda-Morales, M.; Richards, M.; Bautista-Cruz, F.; Martin, N.; Hurlbut, D.; Vanner, S. Citrobacter rodentium colitis evokes post-infectious hyperexcitability of mouse nociceptive colonic dorsal root ganglion neurons. J. Physiol. 2009, 587, 3505–3521. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, S.M.; Clarke, G.; McKernan, D.P.; Bravo, J.A.; Dinan, T.G.; Cryan, J.F. Differential visceral nociceptive, behavioural and neurochemical responses to an immune challenge in the stress-sensitive Wistar Kyoto rat strain. Behav. Brain Res. 2013, 253, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Ling, Z.; Li, Z.; Liu, X.; Cheng, Y.W.; Luo, Y.Q.; Tong, X.J.; Yuan, L.; Wange, Y.Z.; Sunc, J.; Li, L.J.; et al. Altered fecal microbiota composition associated with food allergy in infants. Appl. Environ. Microbiol. 2014, 80, 2546–2554. [Google Scholar] [CrossRef] [PubMed]
- Molloy, J.; Allen, K.; Molloy, J.; Allen, K.; Collier, F.; Tang, M.L.K.; Ward, A.C.; Vuillermin, P. The potential link between gut microbiota and IgE-mediated food allergy in early life. Int. J. Environ. Res. Public Health 2013, 10, 7235–7256. [Google Scholar] [CrossRef] [PubMed]
- Berni Canani, R.; di Costanzo, M. Gut microbiota as potential therapeutic target for the treatment of cow’s milk allergy. Nutrients 2013, 5, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Infante, D.; Segarra, O.; Luyer, B.L. Dietary treatment of colic caused by excess gas in infants: Biochemical evidence. World J. Gastroenterol. 2011, 17, 2104–2108. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Ceratto, S.; De Marco, A.; di Montezemolo, L.C. Looking for new treatments of infantile colic. Ital. J. Pediatr. 2014, 5, 40–53. [Google Scholar]
- Rhoads, J.M.; Fatheree, N.Y.; Norori, J.; Liu, Y.; Lucke, J.F.; Tyson, J.E.; Ferris, M.J. Altered fecal microflora and increased fecal calprotectin in infants with colic. J. Pediatr. 2009, 155, 823–828. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.W.; Fergusson, D.M.; Allardyce, R.A.; Taylor, B. Maternal diet and infantile colic in breast-fed infants. Lancet 1981, 1, 1340–1342. [Google Scholar] [CrossRef] [PubMed]
- Lucassen, P.L.; Assendelft, W.J.; Gubbels, J.W.; van Eijk, J.T.; Douwes, A.C. Infantile colic: Crying time reduction with a whey hydrolysate: A double-blind, randomized, placebo-controlled trial. Pediatrics 2000, 106, 1349–1354. [Google Scholar] [CrossRef] [PubMed]
- Arikan, D.; Alp, H.; Gözüm, S.; Orbak, Z.; Cifçi, E.K. Effectiveness of massage, sucrose solution, herbal tea or hydrolysed formula in the treatment of infantile colic. J. Clin. Nurs. 2008, 17, 1754–1761. [Google Scholar] [CrossRef] [PubMed]
- Forsyth, B.W. Colic and the effect of changing formulas: A double-blind, multiple-crossover study. J. Pediatr. 1989, 115, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Iacono, G.; Carroccio, A.; Montalto, G.; Cavataio, F.; Bragion, E.; Lorello, D.; Balsamo, V.; Notarbartolo, A. Severe infantile colic and food intolerance: A long-term prospective study. J. Pediatr. Gastroenterol. Nutr. 1991, 12, 332–335. [Google Scholar] [CrossRef] [PubMed]
- Lothe, L.; Lindberg, T.; Jakobsson, I. Cow’s milk formula as a cause of infantile colic: A double-blind study. Pediatrics 1982, 70, 7–10. [Google Scholar] [PubMed]
- Berseth, C.L.; Johnston, W.H.; Stolz, S.I.; Harris, C.L.; Mitmesser, S.H. Clinical response to 2 commonly used switch formulas occurs within 1 day. Clin Pediatr 2009, 48, 58–65. [Google Scholar] [CrossRef]
- Berni Canani, R.; Nocerino, R. Diagnosing and treating food allergy. Curr. Pediatr. Rep. 2013, 1, 189–197. [Google Scholar] [CrossRef]
- Nocerino, R.; Granata, V.; Di Costanzo, M.; Pezzella, V.; Leone, L.; Passariello, A.; Terrin, G.; Troncone, R.; Berni, C.R. Atopy patch tests are useful to predict oral tolerance in children with gastrointestinal symptoms related to non-IgE-mediated cow’s milk allergy. Allergy 2013, 68, 246–248. [Google Scholar] [CrossRef] [PubMed]
- Berni Canani, R.; Buongiovanni, A.; Nocerino, R.; Cosenza, L.; Troncone, R. Toward a standardized reading of the atopy patch test in children with suspected cow’s milk allergy-related gastrointestinal symptoms. Allergy 2011, 66, 1499–1500. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Tarasco, V. New treatments for infant colic. Curr. Opin. Pediatr. 2010, 22, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Berni Canani, R.; Leone, L.; D’Auria, E.; Riva, E.; Nocerino, R.; Ruotolo, S.; Terrin, G.; Cosenza, L.; Di Costanzo, M.; Passariello, A.; et al. The effects of dietary counseling on children with food allergy: A prospective, multicenter intervention study. J. Acad. Nutr. Diet. 2014, 114, 1432–1439. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, M.; D’Auria, E.; Caffarelli, C.; Verduci, E.; Barberi, S.; Indinnimeo, L.; Iacono, I.D.; Martelli, A.; Riva, E.; Bernardini, R. Nutritional management and follow up of infants and children with food allergy: Italian Society of Pediatric Nutrition/Italian Society of Pediatric Allergy and Immunology Task Force Position Statement. Ital. J. Pediatr. 2014, 40, 1. [Google Scholar] [CrossRef] [PubMed]
- Chau, K.; Lau, E.J.; Greenberg, S.; Jacobson, S.; Yazdani-Brojeni, P.; Verma, N.; Koren, G. Probiotics for Infantile Colic: A Randomized, Double-Blind, Placebo-Controlled Trial Investigating Lactobacillus reuteri DSM 17938. J. Pediatr. 2015, 166, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Cordisco, L.; Tarasco, V.; Palumeri, E.; Calabrese, R.; Oggero, R.; Roos, S.; Matteuzzi, D. Lactobacillus reuteri DSM 17938 in infantile colic: A randomized, double-blind, placebo-controlled trial. Pediatrics 2010, 126, e526–e533. [Google Scholar] [CrossRef] [PubMed]
- Sung, V.; Hiscock, H.; Tang, M.L.K.; Mensah, F.K.; Nation, M.L.; Satzke, C.; Heine, R.G.; Stock, A.; Barr, R.G.; Wake, M. Treating infant colic with the probiotic Lactobacillus reuteri: Doubleblind, placebo-controlled randomised trial. BMJ 2014, 348, g2107. [Google Scholar] [CrossRef] [PubMed]
- Szajewska, H.; Gyrczuk, E.; Horvath, A. Lactobacillus reuteri DSM 17938 for the management of infantile colic in breastfed infants: A randomized, double-blind, placebo-controlled trial. J. Pediatr. 2013, 162, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Shergill-Bonner, R. Infantile colic: Practicalities of management, including dietary aspects. J. Fam. Health care 2010, 20, 206–209. [Google Scholar] [PubMed]
- Agostoni, C.; Axelsson, I.; Goulet, O.; Koletzko, B.; Michaelsen, K.F.; Puntis, J.; Rieu, D.; Rigo, J.; Shamir, R.; Szajewska, H.; et al. Soy protein infant formulae and follow-on formulae: A commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2006, 42, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, J.; Greer, F.; The Committee on Nutrition. Use of soy protein-based formulas in infant feeding. Pediatrics 2008, 121, 1062–1068. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Gottrand, F.; Veereman-Wauters, G.; De Greef, E.; Devreker, T.; Hauser, B.; Benninga, M.; Heymans, H.S. Gastrointestinal manifestations of cow’s milk protein allergy and gastrointestinal motility. Acta Paediatr. 2012, 101, 1105–1109. [Google Scholar] [CrossRef] [PubMed]
- Lifschitz, C.; Szajewska, H. Cow’s milk allergy: Evidence-based diagnosis and management for the practitioner. Eur. J. Pediatr. 2015, 174, 141–150. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nocerino, R.; Pezzella, V.; Cosenza, L.; Amoroso, A.; Di Scala, C.; Amato, F.; Iacono, G.; Canani, R.B. The Controversial Role of Food Allergy in Infantile Colic: Evidence and Clinical Management. Nutrients 2015, 7, 2015-2025. https://doi.org/10.3390/nu7032015
Nocerino R, Pezzella V, Cosenza L, Amoroso A, Di Scala C, Amato F, Iacono G, Canani RB. The Controversial Role of Food Allergy in Infantile Colic: Evidence and Clinical Management. Nutrients. 2015; 7(3):2015-2025. https://doi.org/10.3390/nu7032015
Chicago/Turabian StyleNocerino, Rita, Vincenza Pezzella, Linda Cosenza, Antonio Amoroso, Carmen Di Scala, Francesco Amato, Giuseppe Iacono, and Roberto Berni Canani. 2015. "The Controversial Role of Food Allergy in Infantile Colic: Evidence and Clinical Management" Nutrients 7, no. 3: 2015-2025. https://doi.org/10.3390/nu7032015



