Changes in the Healthy Beverage Index in Response to an Intervention Targeting a Reduction in Sugar-Sweetened Beverage Consumption as Compared to an Intervention Targeting Improvements in Physical Activity: Results from the Talking Health Trial
Abstract
:1. Introduction
| Beverage Component | Description | Points |
|---|---|---|
| Water | Water comprises ≥20% of fluid requirements | 15 |
| No water consumption | 0 | |
| Water is >0% but <20% of fluid requirements | Proportional | |
| Coffee and Tea | Unsweetened coffee and tea comprise 0%–40% of fluid requirements | 5 |
| Low-fat Milk | <1.5% fat, fat-free, and/or soy milk comprises 0%–16% of fluid requirements | 5 |
| Diet Drinks | Artificially sweetened beverages comprise 0%–16% of fluid requirements | 5 |
| 100% Fruit Juice | 100% fruit juice comprises 0%–8% of fluid requirements | 5 |
| Alcohol | Between 0–1 drinks for women, 0–2 drinks for men | 5 |
| Full-fat Milk | 0% of fluid requirements come from 2% fat or full-fat milk | 5 |
| Sugar-sweetened Beverages | Sugar-sweetened beverages are 0%–8% of fluid requirements | 15 |
| Total Beverage Energy | Energy from beverages <10% of total energy | 20 |
| Energy from beverages ≥15% of total energy | 0 | |
| Energy from beverages is >10% but <15% of total energy | Proportional | |
| Met Fluid Requirements | Amount of beverages (mL) consumed was greater than or equal to fluid requirements | 20 |
| Amount of beverages (mL) consumed was less than fluid requirements | Proportional |
2. Experimental Section
2.1. Subjects and Study Design
2.2. Methods
2.3. Healthy Beverage Index and Healthy Eating Index
2.4. Ethics
2.5. Statistics
3. Results
3.1. Participants
| Characteristics | Total Sample (n = 292) | SIPsmartER (n = 149) | MoveMore (n = 143) |
|---|---|---|---|
| Age (years), M b (SD) c | 42.0 (13.4) | 41.8 (13.4) | 42.3 (13.4) |
| Gender | |||
| Male | 55 (19) | 30 (20) | 25 (17.5) |
| Female | 237 (81) | 119 (80) | 118 (82.5) |
| Race | |||
| Caucasian | 271 (93) | 135 (90.5) | 136 (95) |
| African American | 13 (4.5) | 10 (7) | 3 (2) |
| More than one race | 7 (2.0) | 3 (2) | 4 (3) |
| Other | 1 (0.5) | 1 (0.5) | 0 (0) |
| Ethnicity | |||
| Hispanic/Latina | 3 (1) | 2 (1) | 1 (0.5) |
| Education Level | |||
| ≤High school graduate | 90 (31) | 48 (32) | 42 (29.5) |
| Some college or greater | 202 (69) | 101 (68) | 101 (70.5) |
| Anthropometry | |||
| Weight (kg), M (SD) | 90.6 (25.4) | 90.5 (26.4) | 90.6 (24.4) |
| BMI (kg/m2), M (SD) | 33.0 (9.1) | 33.2 (9.3) | 32.8 (9.0) |
| Underweight (≤18.4) | 5 (1.5) | 3 (2) | 2 (1.5) |
| Normal weight (18.5–24.9) | 58 (20) | 28 (19) | 30 (21) |
| Overweight (25–29.9) | 63 (21.5) | 34 (23) | 29 (20.5) |
| Obese (≥30) | 166 (57) | 86 (56) | 82 (57) |
| Obese class 1 (30–34.9) | 59 (20) | 29 (19.5) | 30 (21) |
| Obese class 2 (35–39.9) | 43 (15) | 20 (13) | 23 (16) |
| Obese class 3 (≥40) | 64 (22) | 35 (23.5) | 29 (20) |
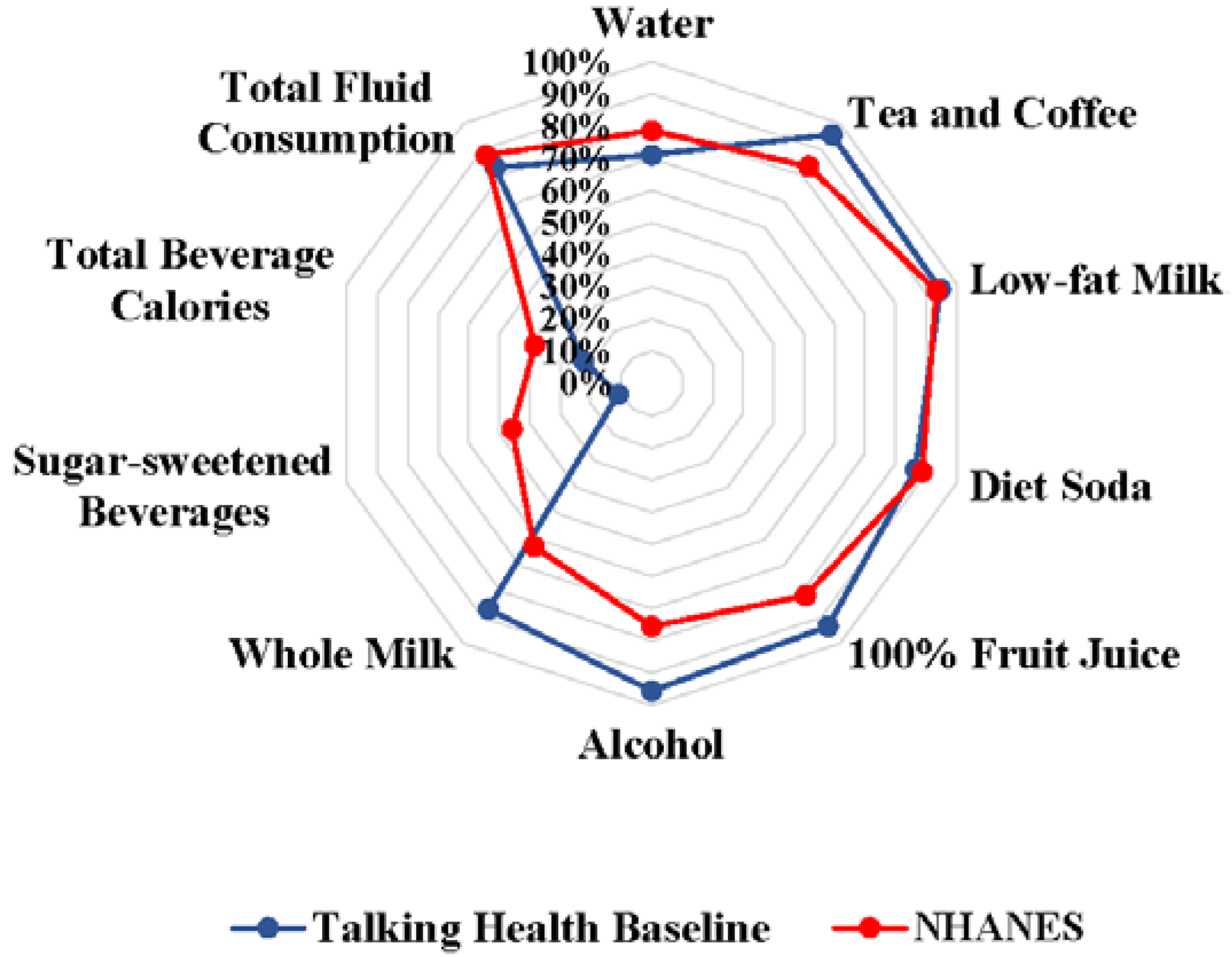
3.2. Beverage Quality
| Healthy Beverage Index Variable (Possible Score) | Group | Baseline b | 6-Month c | Adjusted Change Baseline to 6-Month c,d | p-Value Group by Time |
|---|---|---|---|---|---|
| Water (0–15) | SIPsmartER e | 10.4 (6.0) | 11.0 (6.1) | 0.6 (−0.3, 1.5) | NS e |
| MoveMore e | 11.0 (5.8) | 12.1 (5.5) | 1.1 * (0.2, 2.1) | ||
| Tea and Coffee (0–5) | SIPsmartER | 4.8 (1.0) | 4.4 (1.6) | −0.4 (−0.8, 0.1) | NS |
| MoveMore | 4.8 (1.1) | 4.7 (1.2) | −0.1 (−0.3, 0.2) | ||
| Low-fat Milk (0–5) | SIPsmartER | 4.8 (0.9) | 4.6 (1.4) | −0.2 *** (−0.4, −0.1) | ≤0.05 |
| MoveMore | 4.6 (1.3) | 4.8 (1.1) | 0.1 (−0.2, 0.4) | ||
| Diet Soda (0–5) | SIPsmartER | 4.3 (1.8) | 3.8 (2.1) | −0.4 * (−0.9, 0.0) | ≤0.05 |
| MoveMore | 4.4 (1.7) | 4.4 (1.6) | 0.0 (−0.1, 0.2) | ||
| 100% Fruit Juice (0–5) | SIPsmartER | 4.8 (1.0) | 4.7 (1.2) | −0.1 (−0.3, 0.1) | NS |
| MoveMore | 4.6 (1.4) | 4.5 (1.5) | −0.1 (−0.3, 0.2) | ||
| Alcohol (0–5) | SIPsmartER | 4.8 (1.0) | 4.9 (0.8) | 0.1 (0.0, 0.2) | NS |
| MoveMore | 4.8 (1.1) | 4.8 (1.0) | 0.0 (−0.1, 0.2) | ||
| Whole Milk (0–5) | SIPsmartER | 4.4 (1.6) | 4.7 (1.1) | 0.3 (−0.1, 0.8) | NS |
| MoveMore | 4.3 (1.8) | 4.7 (1.2) | 0.4 *** (0.2, 0.6) | ||
| Sugar-sweetened Beverages (0–15) | SIPsmartER | 1.3 (4.3) | 4.2 (6.8) | 2.9 *** (1.8, 4.0) | ≤0.01 |
| MoveMore | 2.0 (5.1) | 2.5 (5.6) | 0.5 (−0.5, 1.6) | ||
| Total Beverage Calories (0–20) | SIPsmartER | 4.4 (7.5) | 8.6 (9.4) | 4.2 *** (2.6, 5.8) | ≤0.05 |
| MoveMore | 4.6 (7.6) | 6.2 (8.3) | 1.6 *** (0.8, 2.4) | ||
| Total Fluid Consumption (0–20) | SIPsmartER | 16.5 (4.4) | 17.1 (4.2) | 0.6 (−0.2, 1.3) | NS |
| MoveMore | 16.7 (4.2) | 17.4 (4.0) | 0.7 (−0.3, 1.6) | ||
| Total HBI Score (0–100) | SIPsmartER | 60.4 (13.4) | 67.9 (17.9) | 7.5 *** (5.4, 9.7) | ≤0.05 |
| MoveMore | 61.6 (14.6) | 64.9 (16.4) | 3.4 *** (1.6, 5.2) |
3.3. Dietary Quality versus Beverage Quality
| Variables | Empty Calorie: Healthy Eating Index-2010 | Total Healthy Eating Index-2010 |
|---|---|---|
| Sugar-sweetened Beverage: Healthy Beverage Index | 0.32 *** | 0.20 ** |
| Total Beverage Calories: Healthy Beverage Index | 0.29 *** | 0.10 |
| Total Healthy Beverage Index | 0.27 *** | 0.15 ** |
3.4. Physical Activity and Beverage Quality
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
References
- Tate, D.F.; Turner-McGrievy, G.; Lyons, E.; Stevens, J.; Erickson, K.; Polzien, K.; Diamond, M.; Wang, X.; Popkin, B. Replacing caloric beverages with water or diet beverages for weight loss in adults: Main results of the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. Am. J. Clin. Nutr. 2012, 95, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Zoellner, J.; Chen, Y.; Davy, B.; You, W.; Hedrick, V.; Corsi, T.; Estabrooks, P. Talking Health, A pragmatic randomized-controlled health literacy trial targeting sugar-sweetened beverage consumption among adults: Rationale, design & methods. Contemp. Clin. Trials 2014, 37, 43–57. [Google Scholar] [PubMed]
- Hu, F.B. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes. Rev. 2013, 14, 606–619. [Google Scholar] [CrossRef] [PubMed]
- Scientific Report of the 2015 Dietary Guidelines Advisory Committee (DGAC Report). In Dietary Guidelines Website; Released February 23. Available online: http://health.gov/dietaryguidelines/2015-scientific-report/pdfs/scientific-report-of-the-2015-dietary-guidelines-advisory-committee.pdf (accessed on 5 August 2015).
- Yang, Q.; Zhang, Z.; Gregg, E.W.; Flanders, W.D.; Merritt, R.; Hu, F.B. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern. Med. 2014, 174, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Imamura, F.; O’Connor, L.; Ye, Z.; Mursu, J.; Hayashino, Y.; Bhupathiraju, S.N.; Forouhi, N.G. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: Systematic review, meta-analysis, and estimation of population attributable fraction. BMJ 2015, 351. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.; Popkin, B.; Bray, G.; Despres, J.; Hu, F. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010, 121, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, L.; Imamura, F.; Lentjes, M.A.; Khaw, K.T.; Wareham, N.J.; Forouhi, N.G. Prospective associations and population impact of sweet beverage intake and type 2 diabetes, and effects of substitutions with alternative beverages. Diabetologia 2015, 58, 1474–1483. [Google Scholar] [CrossRef] [PubMed]
- Hedrick, V.; Davy, B.; Duffey, K. Is beverage consumption related to specific dietary pattern intakes. Curr. Nutr. Rep. 2015, 4, 72–81. [Google Scholar] [CrossRef]
- Goodman, A.B.; Blanck, H.M.; Sherry, B.; Park, S.; Nebeling, L.; Yaroch, A.L. Behaviors and attitudes associated with low drinking water intake among US adults, Food Attitudes and Behaviors Survey, 2007. Prev. Chronic Dis. 2013, 10, E51. [Google Scholar] [CrossRef] [PubMed]
- Kit, B.K.; Fakhouri, T.H.; Park, S.; Nielsen, S.J.; Ogden, C.L. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am. J. Clin. Nutr. 2013, 98, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; D’Anci, K.E.; Rosenberg, I.H. Water, hydration, and health. Nutr. Rev. 2010, 68, 439–458. [Google Scholar] [CrossRef] [PubMed]
- Daniels, M.C.; Popkin, B.M. Impact of water intake on energy intake and weight status: A systematic review. Nutr. Rev. 2010, 68, 505–521. [Google Scholar] [CrossRef] [PubMed]
- Sievenpiper, J.L.; de Souza, R.J. Are sugar-sweetened beverages the whole story? Am. J. Clin. Nutr. 2013, 98, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Guenther, P.M.; Casavale, K.O.; Reedy, J.; Kirkpatrick, S.I.; Hiza, H.A.; Kuczynski, K.J.; Kahle, L.L.; Krebs-Smith, S.M. Update of the Healthy Eating Index: HEI-2010. J. Acad. Nutr. Diet. 2013, 113, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Duffey, K.J.; Davy, B.M. The Healthy Beverage Index Is Associated with Reduced Cardiometabolic Risk in US Adults: A Preliminary Analysis. J. Acad. Nutr. Diet. 2015, 115, 1682–1689. [Google Scholar] [CrossRef] [PubMed]
- Myers, E.F.; Khoo, C.S.; Murphy, W.; Steiber, A.; Agarwal, S. A critical assessment of research needs identified by the dietary guidelines committees from 1980 to 2010. J. Acad. Nutr. Diet. 2013, 113, 957–971. [Google Scholar] [CrossRef] [PubMed]
- Duffey, K.J.; Popkin, B.M. Adults with healthier dietary patterns have healthier beverage patterns. J. Nutr. 2006, 136, 2901–2907. [Google Scholar] [PubMed]
- Zoellner, J.; Hedrick, V.; You, W.; Chen, Y.; Davy, B.; Porter, K.; Bailey, A.; Lane, H.; Alexander, R.; Estabrooks, P. Effects of a behavioral and health literacy intervention to reduce sugar-sweetened beverages: A randomized-controlled trial. IJBNPA. (submitted).
- U.S. Department of Health and Human Services, Health Resources and Services Administration Website. Medically Underserved Areas/Populations: Guidelines for MUA and MUP Designation. Available online: http://www.hrsa.gov/shortage/mua/ (accessed on 1 September 2015).
- Johnson, R.K.; Appel, L.J.; Brands, M.; Howard, B.V.; Lefevre, M.; Lustig, R.H.; Sacks, F.; Steffen, L.M.; Wylie-Rosett, J. Dietary sugars intake and cardiovascular health: A scientific statement from the American Heart Association. Circulation 2009, 120, 1011–1020. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Armstrong, L.E.; Bray, G.M.; Caballero, B.; Frei, B.; Willett, W.C. A new proposed guidance system for beverage consumption in the United States. Am. J. Clin. Nutr. 2006, 83, 529–542. [Google Scholar] [PubMed]
- Hedrick, V.E.; Comber, D.L.; Estabrooks, P.A.; Savla, J.; Davy, B.M. The beverage intake questionnaire: Determining initial validity and reliability. J. Am. Diet. Assoc. 2010, 110, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- Hedrick, V.E.; Comber, D.L.; Ferguson, K.E.; Estabrooks, P.A.; Savla, J.; Dietrich, A.M.; Serrano, E.; Davy, B.M. A rapid beverage intake questionnaire can detect changes in beverage intake. Eat. Behav. 2013, 14, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Hedrick, V.E.; Savla, J.; Comber, D.L.; Flack, K.D.; Estabrooks, P.A.; Nsiah-Kumi, P.A.; Ortmeier, S.; Davy, B.M. Development of a brief questionnaire to assess habitual beverage intake (BEVQ-15): Sugar-sweetened beverages and total beverage energy intake. J. Acad. Nutr. Diet. 2012, 112, 840–849. [Google Scholar] [CrossRef] [PubMed]
- Riebl, S.K.; Paone, A.C.; Hedrick, V.E.; Zoellner, J.M.; Estabrooks, P.A.; Davy, B.M. The comparative validity of interactive multimedia questionnaires to paper-administered questionnaires for beverage intake and physical activity: Pilot study. JMIR Res. Protoc. 2013, 2, e40. [Google Scholar] [CrossRef] [PubMed]
- Monsen, E. Research: Successful Approaches, 2nd ed.; American Dietetic Association: Chicago, IL, USA, 2003. [Google Scholar]
- Willett, W.; Lenart, E. Nutritional Epidemiology, 2nd ed.; Oxford University Press: New York, NY, USA, 1998. [Google Scholar]
- Godin, G.; Shephard, R. A simple method to assess exercise behavior in the community. Can. J. Appl. Sport Sci. 1985, 10, 141–146. [Google Scholar] [PubMed]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010; U.S. Government Printing Office: Washington, DC, USA, 2010.
- Halliday, T.M.; Davy, B.M.; Clark, A.G.; Baugh, M.E.; Hedrick, V.E.; Marinik, E.L.; Flack, K.D.; Savla, J.; Winett, S.; Winett, R.A. Dietary intake modification in response to a participation in a resistance training program for sedentary older adults with prediabetes: Findings from the Resist Diabetes study. Eat. Behav. 2014, 15, 379–382. [Google Scholar] [CrossRef] [PubMed]
- Hedrick, V.; Davy, B.; You, W.; Porter, K.; Zoellner, J. Diet quality changes in response to a sugar-sweetened beverage reduction intervention. Results from the Talking Health randomized controlled clinical trial. Unpublished; manuscript in preparation.
- Institute of Medicine of the National Academies. Dietary Reference Intakes: Research Synthesis Workshop Summary; The National Academies Press: Washington, DC, USA, 2007. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hedrick, V.E.; Davy, B.M.; Myers, E.A.; You, W.; Zoellner, J.M. Changes in the Healthy Beverage Index in Response to an Intervention Targeting a Reduction in Sugar-Sweetened Beverage Consumption as Compared to an Intervention Targeting Improvements in Physical Activity: Results from the Talking Health Trial. Nutrients 2015, 7, 10168-10178. https://doi.org/10.3390/nu7125525
Hedrick VE, Davy BM, Myers EA, You W, Zoellner JM. Changes in the Healthy Beverage Index in Response to an Intervention Targeting a Reduction in Sugar-Sweetened Beverage Consumption as Compared to an Intervention Targeting Improvements in Physical Activity: Results from the Talking Health Trial. Nutrients. 2015; 7(12):10168-10178. https://doi.org/10.3390/nu7125525
Chicago/Turabian StyleHedrick, Valisa E., Brenda M. Davy, Emily A. Myers, Wen You, and Jamie M. Zoellner. 2015. "Changes in the Healthy Beverage Index in Response to an Intervention Targeting a Reduction in Sugar-Sweetened Beverage Consumption as Compared to an Intervention Targeting Improvements in Physical Activity: Results from the Talking Health Trial" Nutrients 7, no. 12: 10168-10178. https://doi.org/10.3390/nu7125525





