Better Adherence to the Mediterranean Diet Could Mitigate the Adverse Consequences of Obesity on Cardiovascular Disease: The SUN Prospective Cohort
Abstract
:1. Introduction
2. Experimental Section
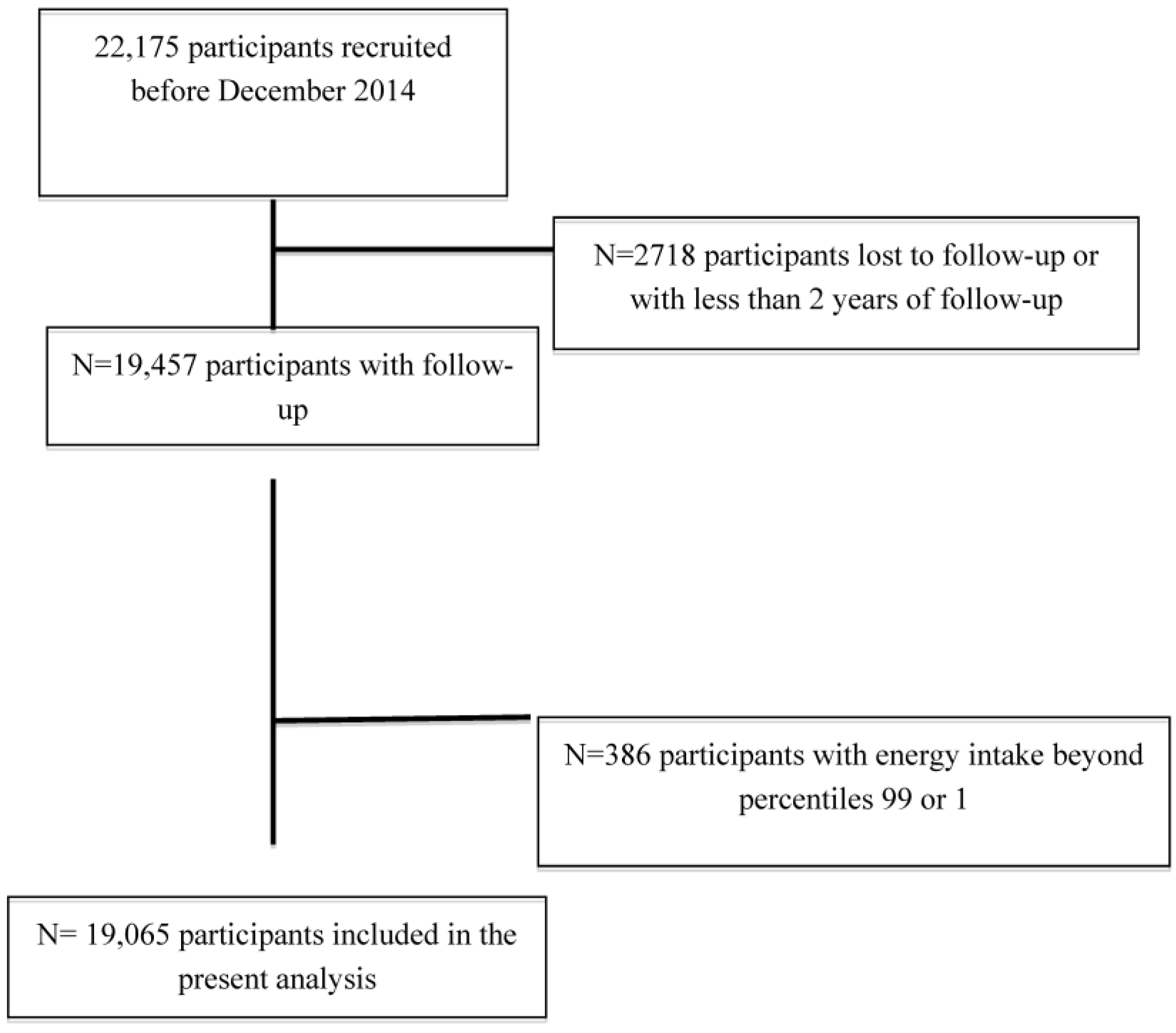
2.1. Study Population
2.2. Anthropometric Variables
2.3. Dietary Assessment
2.4. Other Covariates
2.5. Outcome Assessment
2.6. Statistical Analyses
3. Results
| Low Adherence to MedDiet (<6/9) | High Adherence to MedDiet (≥6/9) | |||||
|---|---|---|---|---|---|---|
| BMI <25 | BMI 25–30 | BMI >30 | BMI <25 | BMI 25–30 | BMI >30 | |
| N | 10,169 | 3396 | 663 | 3208 | 1396 | 233 |
| Age (years) | 35 (10) | 43 (13) | 45 (12) | 39 (12) | 48 (12) | 48 (13) |
| Women (%) | 74.3 | 30.4 | 32.0 | 71.7 | 28.2 | 23.6 |
| BMI (kg/m2) | 21.6 (1.9) | 26.9 (1.3) | 32.5 (2.4) | 21.9 (1.9) | 26.9 (1.3) | 32.7 (3.0) |
| Previous history of CVD (%) | 0.4 | 1.3 | 1.5 | 0.8 | 3.0 | 4.3 |
| Energy intake (kcal/day) | 2479 (766) | 2353 (756) | 2386 (812) | 2698 (786) | 2633 (766) | 2715 (800) |
| Leisure-time physical activity | 20.6 (22.1) | 20.4 (21.7) | 15.2 (17.7) | 26.8 (26.0) | 24.6 (23.3) | 19.7 (18.0) |
| Marital status | ||||||
| Single | 53.5 | 30.9 | 27.8 | 43.6 | 19.9 | 5.7 |
| Married | 42.4 | 63.9 | 65.6 | 50.7 | 74.4 | 70.4 |
| Others | 4.0 | 5.2 | 6.6 | 5.7 | 5.8 | 7.7 |
| Smoking current smokers (%) | 22.9 | 20.4 | 19.6 | 20.8 | 17.9 | 18.0 |
| Former smokers (%) | 22.6 | 34.9 | 39.5 | 30.5 | 44.4 | 48.1 |
| Baseline hypercholesterolemia (%) | 11.3 | 22.5 | 32.3 | 17.8 | 33.0 | 38.2 |
| Baseline triglycerides (%) | 2.9 | 12.1 | 23.5 | 4.4 | 16.3 | 30.9 |
| Diabetes at baseline (%) | 0.9 | 2.8 | 5.7 | 1.6 | 3.5 | 7.3 |
| Hypertension at baseline (%) | 3.0 | 12.5 | 25.9 | 5.2 | 19.3 | 32.6 |
| Years of university education | 5.0 (1.47) | 5.2 (1.60) | 5.0 (1.51) | 5.0 (1.50) | 5.3 (1.72) | 5.1 (1.50) |
| Leisure-time spent sitting down, h/week. | 3.8 (1.72) | 3.8 (1.91) | 3.8 (2.06) | 3.9 (1.86) | 4.0 (1.83) | 4.1 (2.01) |
| TV watching, h/week. | 1.6 (1.23) | 1.7 (1.14) | 1.8 (1.18) | 1.6 (1.16) | 1.7 (1.09) | 1.8 (1.17) |
| Between-meal snacking (%) | 35.2 | 34.7 | 51.3 | 27.9 | 29.3 | 40.8 |
| Following special diets (%) | 5.6 | 9.6 | 15.1 | 9.2 | 12.8 | 19.3 |
| Low Adherence to MedDiet (<6/9) | High Adherence to MedDiet (≥6/9) | |||||
|---|---|---|---|---|---|---|
| Body mass index | <25 | 25–30 | >30 | <25 | 25–30 | >30 |
| n | 10,169 | 3396 | 663 | 3208 | 1396 | 233 |
| Median body mass index | 21.6 | 26.9 | 32.5 | 21.9 | 26.9 | 32.7 |
| events | 38 | 59 | 15 | 15 | 19 | 6 |
| Person-years | 95,620 | 30,961 | 5814 | 28,260 | 11,917 | 1789 |
| Age-adjusted rate/105 (95% CI) | 40 (28–55) | 74 (49–113) | 97 (53–177) | 31 (17–57) | 43 (25–76) | 86 (36–206) |
| Sex-, age-adjusted HR | 1 (ref.) | 1.52 (0.99–2.35) | 2.14 (1.14–4.00) | 1 (ref.) | 0.97 (0.48–1.95) | 1.77 (0.61–5.17) |
| Multivariable-adjusted HR * | 1 (ref.) | 1.44 (0.93–2.25) | 2.00 (1.04–3.83) | 1 (ref.) | 0.77 (0.35–1.67) | 1.15 (0.39–3.43) |
| Adherence to the Mediterranean Diet | Low 0–2 | Low-Moderate 3–4 | Moderate-High 5–6 | High 7–9 | p for Trend | For Each +2 Points |
|---|---|---|---|---|---|---|
| n | 3334 | 7160 | 6431 | 2140 | ||
| Incident cases of CVD | 23 | 57 | 51 | 21 | ||
| Person-years | 32,001 | 66,900 | 57,120 | 18,341 | ||
| Sex-, age-adjusted HR | 1 (ref.) | 0.88 (0.53–1.46) | 0.68 (0.40–1.15) | 0.58 (0.31–1.09) | 0.097 | 0.95 (0.91–0.99) |
| Multivariable-adjusted HR * | 1 (ref.) | 0.81 (0.48–1.38) | 0.58 (0.34–1.00) | 0.47 (0.25–0.89) | 0.029 | 0.93(0.89–0.98) |
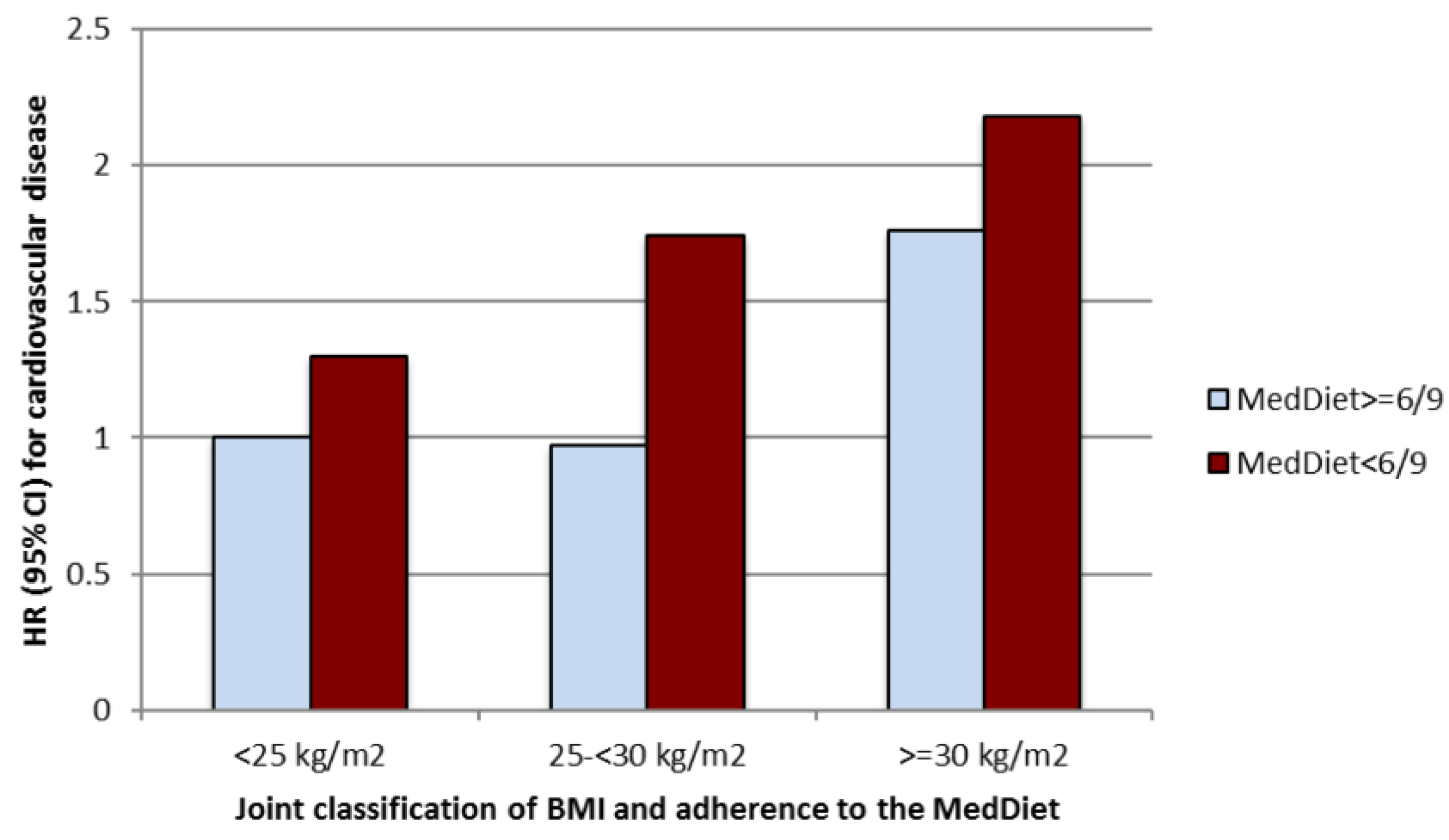
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Funding/Support
References
- World Health Organization. World Health Statistics; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Prospective Studies Collaboration; Whitlock, G.; Lewington, S.; Sherliker, P.; Clarke, R.; Emberson, J.; Halsey, J.; Qizilbash, N.; Collins, R.; Peto, R. Body-mass index and cause-specific mortality in 900,000 adults: Collaborative analyses of 57 prospective studies. Lancet 2009, 373, 1083–1096. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Yang, G.; Zhou, M.; Smith, M.; Offer, A.; Ma, J.; Wang, L.; Pan, H.; Whitlock, G.; Collins, R.; et al. Body mass index and mortality from ischaemic heart disease in a lean population: 10 year prospective study of 220,000 adult men. Int. J. Epidemiol. 2006, 35, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Berrington de Gonzalez, A.; Hartge, P.; Cerhan, J.R.; Flint, A.J.; Hannan, L.; Macinnis, R.J.; Moore, S.C.; Tobias, G.S.; Anton-Culver, H.; Freeman, L.B.; et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 2010, 363, 2211–2219. [Google Scholar] [CrossRef] [PubMed]
- Bogers, R.P.; Bemelmans, W.J.; Hoogenveen, R.T.; Boshuizen, H.C.; Woodward, M.; Knekt, P.; van Dam, R.M.; Hu, F.B.; Visscher, T.L.; Menotti, A.; et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: A meta-analysis of 21 cohort studies including more than 300,000 persons. Arch. Intern. Med. 2007, 167, 1720–1728. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B.; Willett, W.C. Optimal diets for prevention of coronary heart. JAMA 2002, 288, 2569–2578. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Appel, L.J.; van Horn, L. Components of a cardioprotective diet: New insights. Circulation 2011, 123, 2870–2891. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr. Opin. Lipidol. 2014, 25, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; Salas-Salvadó, J.; Estruch, R.; Corella, D.; Fitó, M.; Ros, E. Benefits of the Mediterranean Diet: Insights from the PREDIMED Study. Prog. Cardiovasc. Dis. 2015, 58, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literatura-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef] [PubMed]
- Eguaras, S.; Toledo, E.; Buil-Cosiales, P.; Salas-Salvadó, J.; Corella, D.; Gutierrez-Bedmar, M.; Santos-Lozano, J.M.; Arós, F.; Fiol, M.; Fitó, M.; et al. Does the Mediterranean diet counteract the adverse effects of abdominal adiposity? Nutr. Metab. Cardiovasc. Dis. 2015, 25, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; Sanchez-Villegas, A.; de Irala, J.; Marti, A.; Martínez, J.A. Mediterranean diet and stroke: Objectives and design of the SUN project. Seguimiento Universidad de Navarra. Nutr. Neurosci. 2002, 5, 65–73. [Google Scholar] [PubMed]
- Bes-Rastrollo, M.; Perez Valdivieso, J.R.; Sanchez-Villegas, A.; Alonso, A.; Martínez-González, M.A. Validation of the self-reported weight and body mass index of the participants in a cohort of university graduates. Rev. Esp. Obes. 2005, 3, 352–358. (In Spanish) [Google Scholar]
- Martínez-González, M.A.; de la Fuente-Arrillaga, C.; Nunez-Córdoba, J.M.; Basterra-Gortari, F.J.; Beunza, J.J.; Vazquez, Z.; Benito, S.; Tortosa, A.; Bes-Rastrollo, M. Adherence to Mediterranean diet and risk of developing diabetes: Prospective cohort study. BMJ 2008, 336, 1348–1351. [Google Scholar] [CrossRef] [PubMed]
- De la Fuente-Arrillaga, C.; Vazquez Ruiz, Z.; Bes-Rastrollo, M.; Sampson, L.; Martínez-González, M.A. Reproducibility of an FFQ validated in Spain. Public Health Nutr. 2010, 13, 1364–1372. [Google Scholar] [CrossRef] [PubMed]
- Mataix, J. Tabla de Composición de Alimentos (Food Composition Tables), 4th ed.; Universidad de Granada: Granada, Spain, 2003. [Google Scholar]
- Moreiras, O. Tablas de Composición de Alimentos (Food Composition Tables), 5th ed.; Ediciones Pirámide: Madrid, Spain, 2003. [Google Scholar]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Vassilakou, T.; Lipworth, L.; Trichopoulous, D. Diet and overall survival in elderly people. BMJ 1995, 311, 1457–1460. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; López-Fontana, C.; Varo, J.J.; Sánchez-Villegas, A.; Martinez, J.A. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005, 8, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; García-López, M.; Bes-Rastrollo, M.; Toledo, E.; Martínez-Lapiscina, E.H.; Delgado-Rodriguez, M.; Vazquez, Z.; Benito, S.; Beunza, J.J. Mediterranean diet and the incidence of cardiovascular disease: A Spanish cohort. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Kwagyan, J.; Retta, T.M.; Ketete, M.; Bettencourt, C.N.; Maqbool, A.R.; Xu, S.; Randall, O.S. Obesity and cardiovascular diseases in a high-risk population: Evidence-based approach to CHD risk reduction. Ethn. Dis. 2015, 25, 208–213. [Google Scholar] [PubMed]
- Masi, S.; Khan, T.; Johnson, W.; Wong, A.; Whincup, P.; Kuh, D.; Hughes, A.; Richards, M.; Hardy, R.; Deanfield, J. 4C.01: Lifetime obesity, cardiovascular disease and cognitive function: A longitudinal study from the 1946 birth cohort. J. Hypertens. 2015, 33 (Suppl. 1), e56. [Google Scholar] [CrossRef]
- Peters, A.; McEwen, B.S. Stress habituation, body shape and cardiovascular mortality. Neurosci. Biobehav. Rev. 2015, 56, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Esser, N.; Legrand-Poels, S.; Piette, J.; Scheen, A.J.; Paquot, N. Inflammation as a link between obesity, metabolic síndrome and type 2 diabetes. Diabetes. Res. Clin. Pract. 2014, 105, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Oliver, E.; McGillicuddy, F.; Philips, C.; Toomey, S.; Roche, H.M. The role of inflammation and macrophage accumulation in the development of obesity-induced type 2 diabetes mellitus and the possible therapeutic effects of long-chain n-3 PUFA. Proc. Nutr. Soc. 2010, 69, 232–243. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Mediterranean dietary pattern, inflammation and endothelial function: A systematic review and meta-analysis of intervention trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Gelber, R.P.; Gaziano, J.M.; Orav, E.J.; Manson, J.E.; Buring, J.E.; Kurth, T. Measures of obesity and cardiovascular risk among men and women. J. Am. Coll. Cardiol. 2008, 52, 605–615. [Google Scholar] [CrossRef] [PubMed]
- De Hollander, E.L.; Bemelmans, W.J.; Boshuizen, H.C.; Friedrich, N.; Wallaschofski, H.; Guallar-Castillón, P.; Walter, S.; Zillikens, M.C.; Rosengren, A.; Lissner, L.; et al. The association between waist circumference and risk of mortality considering body mass index in 65-to 74-years-olds: A meta-analysis of 29 cohorts involving more than 58,000 elderly persons. Int. J. Epidemiol. 2012, 41, 805–817. [Google Scholar] [CrossRef] [PubMed]
- Guallar-Castillón, P.; Rodríguez-Artalejo, F.; Tormo, M.J.; Sánchez, M.J.; Rodríguez, L.; Quirós, J.R.; Navarro, C.; Molina, E.; Martínez, C.; Marín, P.; et al. Major dietary patterns and risk of coronary heart disease in middle-aged persons from a Mediterranean country: The EPIC-Spain cohort study. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Taínta, A.; Estruch, R.; Bulló, M.; Corella, D.; Gómez-Gracia, E.; Fiol, M.; Algorta, J.; Covas, M.I.; Lapetra, J.; Zazpe, I.; et al. Adherence to a Mediterranean-type diet and reduced prevalence of clustered cardiovascular risk factors in a cohort of 3204 high-risk patients. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 589–593. [Google Scholar] [CrossRef] [PubMed]
- García-Férnandez, E.; Rico-Cabanas, L.; Rosgaard, N.; Estruch, R.; Bach-Faig, A. Mediterranean diet and cardiodiabesity: A review. Nutrients 2014, 6, 3474–3500. [Google Scholar] [CrossRef] [PubMed]
- Aljefree, N.; Ahmed, F. Association between dietary pattern and risk of cardiovascular disease among adults in the Middle East and North Africa region: A systematic review. Food Nutr. Res. 2015, 59, 27486. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eguaras, S.; Toledo, E.; Hernández-Hernández, A.; Cervantes, S.; Martínez-González, M.A. Better Adherence to the Mediterranean Diet Could Mitigate the Adverse Consequences of Obesity on Cardiovascular Disease: The SUN Prospective Cohort. Nutrients 2015, 7, 9154-9162. https://doi.org/10.3390/nu7115457
Eguaras S, Toledo E, Hernández-Hernández A, Cervantes S, Martínez-González MA. Better Adherence to the Mediterranean Diet Could Mitigate the Adverse Consequences of Obesity on Cardiovascular Disease: The SUN Prospective Cohort. Nutrients. 2015; 7(11):9154-9162. https://doi.org/10.3390/nu7115457
Chicago/Turabian StyleEguaras, Sonia, Estefanía Toledo, Aitor Hernández-Hernández, Sebastián Cervantes, and Miguel A. Martínez-González. 2015. "Better Adherence to the Mediterranean Diet Could Mitigate the Adverse Consequences of Obesity on Cardiovascular Disease: The SUN Prospective Cohort" Nutrients 7, no. 11: 9154-9162. https://doi.org/10.3390/nu7115457





