Mediterranean Alcohol-Drinking Pattern and the Incidence of Cardiovascular Disease and Cardiovascular Mortality: The SUN Project
Abstract
:1. Introduction
2. Methods
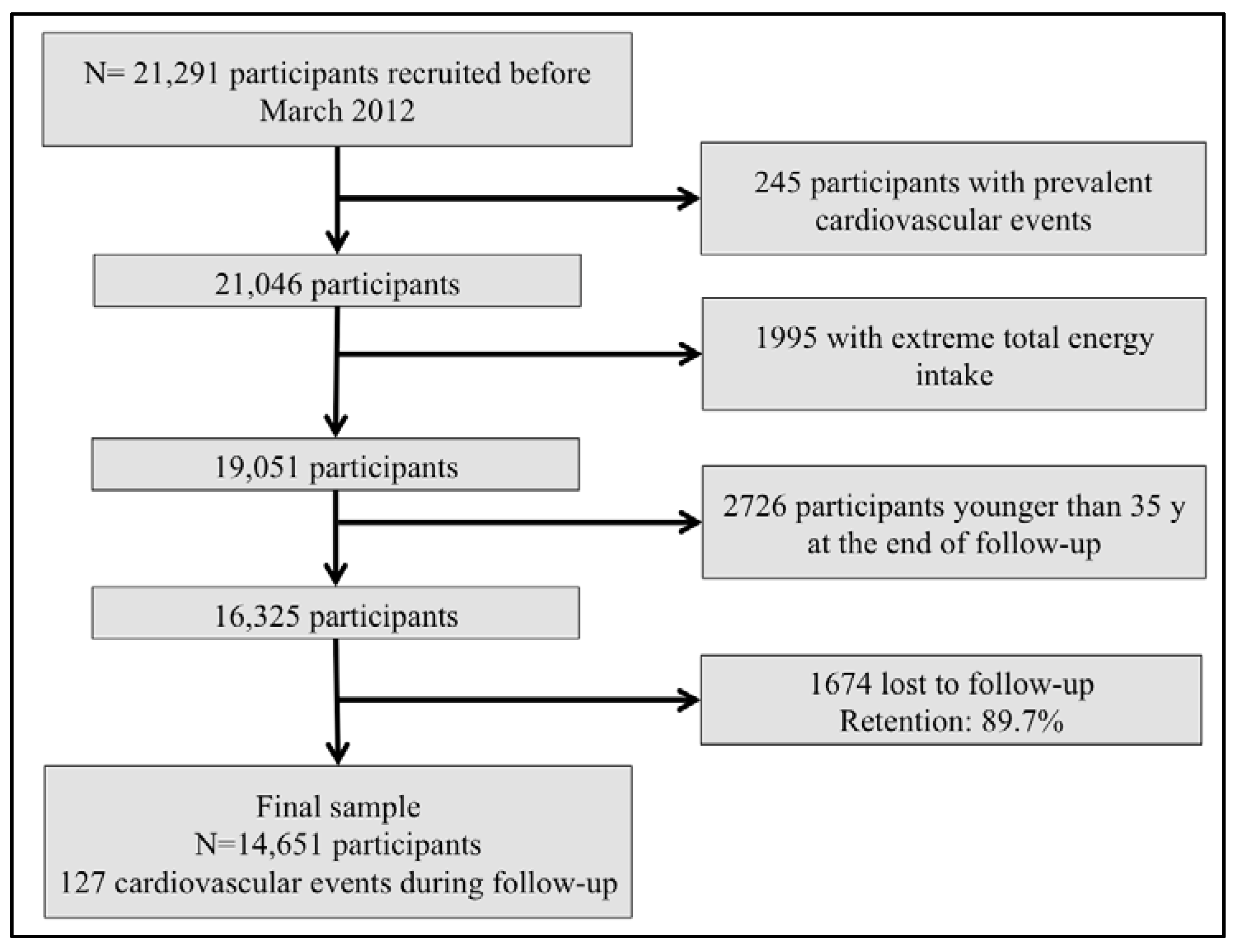
2.1. Study Population
2.2. Exposure: Mediterranean Alcohol-Drinking Pattern
2.3. Outcome: Cardiovascular Events
2.4. Covariates Assessment
2.5. Statistical Analysis
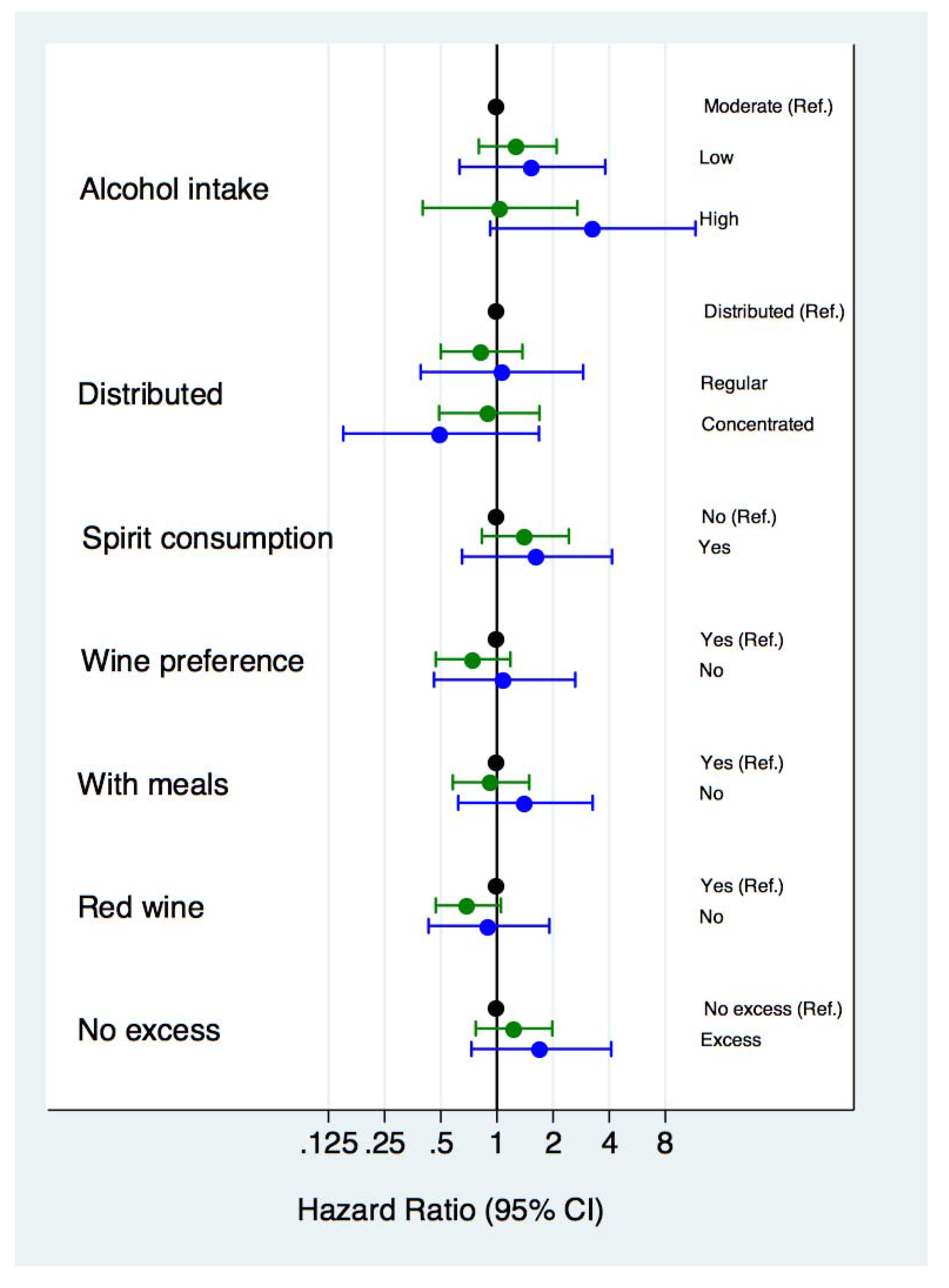
3. Results
| Abstainers | Mediterranean Alcohol-Drinking Pattern | |||
|---|---|---|---|---|
| Low (0–2) | Moderate (3–6) | High (7–9) | ||
| N | 2478 | 840 | 8192 | 3141 |
| Age (years) | 39.7 (11.1) | 33.4 (9.0) | 40.1 (11.0) | 46.5 (10.8) |
| Sex (women %) | 79.3 | 60.2 | 52.8 | 47.9 |
| BMI (kg/m2) | 23.2 (3.6) | 23.5 (3.8) | 23.9 (3.5) | 24.2(3.3) |
| Current smokers (%) | 14.7 | 32.1 | 24.1 | 16.9 |
| Former smokers (%) | 21.9 | 23.3 | 32.4 | 39.9 |
| Physical activity (MET-h/week) | 19.8 (24.1) | 19.8 (21.0) | 21.3 (22.0) | 21.5 (21.0) |
| Time spent watching television (h/day) | 1.6 (1.2) | 1.9 (1.4) | 1.6 (1.1) | 1.5 (1.1) |
| Total energy intake (Kcal/day) | 2284 (622) | 2371 (621) | 2360 (618) | 2342 (613) |
| Prevalent hypertension (%) | 8.4 | 6.4 | 8.8 | 13.1 |
| Prevalent hypercholesterolemia (%) | 16.4 | 14.4 | 18.0 | 25.3 |
| Prevalent type 2 diabetes mellitus (%) | 1.9 | 1.9 | 1.8 | 2.9 |
| Prevalent or previous cancer (%) | 4.8 | 2.4 | 3.8 | 5.2 |
| Prevalent stable coronary artery diseases (%) | 0.3 | 0.5 | 0.5 | 0.9 |
| Cardiovascular-related medication use (%) | 3.9 | 2.1 | 4.4 | 7.3 |
| Mediterranean dietary pattern (0–8) | 3.9 (1.8) | 3.7 (1.6) | 4.0 (1.7) | 4.2 (1.7) |
| Alcohol intake (g/day) | - | 7.4 (19.4) | 9.4 (12.1) | 11.8 (9.0) |
| Wine consumption (g/day) | - | 1.6 (7.6) | 3.9 (7.8) | 9.1 (7.9) |
| Red wine consumption (g/day) | - | 0.8 (4.3) | 2.3 (5.7) | 6.3 (7.2) |
| Spirit consumption (g/day) | - | 3.3 (8.6) | 1.8 (3.8) | 0.5 (1.0) |
| >5 drinks in a single occasion (%) | - | 62.9 | 36.9 | 9.0 |
| Ratio (days/week): (g/week) | - | 0.1 (0.1) | 0.3 (0.4) | 0.6 (0.6) |
| Proportion of wine consumed with meals | - | 0.6 (6.8) | 5.8 (27.6) | 13.3 (36.0) |
| Abstainers | Mediterranean Alcohol Drink Pattern | |||
|---|---|---|---|---|
| Low (0–2) | Moderate (3–6) | High (7–9) | ||
| Cases/person-year | 11/23,924 | 5/8681 | 73/79,695 | 38/29,877 |
| Age and sex-adjusted model | 0.88 (0.42–1.88) | 2.25 (0.86–5.90) | 1.37 (0.91–2.07) | 1 (Ref.) |
| Multiple-adjusted model * | 0.99 (0.46–2.12) | 1.55 (0.58–4.16) | 1.30 (0.85–1.98) | 1 (Ref.) |
| Abstainers | Mediterranean Alcohol Drink Pattern | |||
|---|---|---|---|---|
| Low (0–2) | Moderate (3–6) | High (7–9) | ||
| Cases/person-year | 5/23,891 | 3/8673 | 27/79,449 | 9/29,719 |
| Age and sex-adjusted model | 1.48 (0.42–5.23) | 5.94 (1.48–23.9) | 2.67 (1.19–5.98) | 1 (Ref.) |
| Multiple-adjusted model * | 1.91 (0.52–6.98) | 3.35 (0.77–14.5) | 2.64 (1.11–6.23) | 1 (Ref.) |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. World Health Statistics; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Laonigro, I.; Correale, M.; di Biase, M.; Altomare, E. Alcohol abuse and heart failure. Eur. J. Heart Fail. 2009, 11, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Corrao, G.; Bagnardi, V.; Zambon, A.; la Vecchia, C. A meta-analysis of alcohol consumption and the risk of 15 diseases. Prev. Med. 2004, 38, 613–619. [Google Scholar] [CrossRef]
- Costanzo, S.; di Castelnuovo, A.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Alcohol consumption and mortality in patients with cardiovascular disease: A meta-analysis. J. Am. Coll. Cardiol. 2010, 55, 1339–1347. [Google Scholar] [CrossRef] [PubMed]
- Murray, R.P.; Connett, J.E.; Tyas, S.L.; Bond, R.; Ekuma, O.; Silversides, C.K.; Barnes, G.E. Alcohol volume, drinking pattern, and cardiovascular disease morbidity and mortality: Is there a U-shaped function? Am. J. Epidemiol. 2002, 155, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; García-López, M.; Bes-Rastrollo, M.; Toledo, E.; Martínez-Lapiscina, E.H.; Delgado-Rodriguez, M.; Vazquez, Z.; Benito, S.; Beunza, J.J. Mediterranean diet and the incidence of cardiovascular disease: A Spanish cohort. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Bamia, C.; Trichopoulos, D. Anatomy of health effects of Mediterranean diet: Greek EPIC prospective cohort study. BMJ 2009, 338, b2337. [Google Scholar] [CrossRef] [PubMed]
- Leon-Munoz, L.M.; Galán, I.; Valencia-Martín, J.L.; López-García, E.; Guallar-Castillón, P.; Rodríguez-Artalejo, F. Is a specific drinking pattern a consistent feature of the Mediterranean diet in Spain in the XXI century? Nutr. Metab. Cardiovasc. Dis. 2014, 24, 1074–1081. [Google Scholar] [PubMed]
- Renaud, S.; de Lorgeril, M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet 1992, 339, 1523–1526. [Google Scholar] [CrossRef]
- Bagnardi, V.; Zatonski, W.; Scotti, L.; la Vecchia, C.; Corrao, G. Does drinking pattern modify the effect of alcohol on the risk of coronary heart disease? Evidence from a meta-analysis. J. Epidemiol. Community Health 2008, 62, 615–619. [Google Scholar] [CrossRef] [PubMed]
- Gea, A.; Bes-Rastrollo, M.; Toledo, E.; Garcia-Lopez, M.; Beunza, J.J.; Estruch, R.; Martinez-Gonzalez, M.A. Mediterranean alcohol-drinking pattern and mortality in the SUN (Seguimiento Universidad de Navarra) Project: A prospective cohort study. Br. J. Nutr. 2014, 111, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Segui-Gomez, M.; de la Fuente, C.; Vázquez, Z.; de Irala, J.; Martínez-González, M.A. Cohort profile: The “Seguimiento Universidad de Navarra” (SUN) study. Int. J. Epidemiol. 2006, 35, 1417–1422. [Google Scholar] [CrossRef] [PubMed]
- Willett, W. Nutritional Epidemiology, 2nd ed.; Oxford University Press: New York, NY, USA, 1998. [Google Scholar]
- Martin-Moreno, J.M.; Boyle, P.; Gorgojo, L.; Maisonneuve, P.; Fernandez-Rodriguez, J.C.; Salvini, S.; Willett, W.C. Development and validation of a food frequency questionnaire in Spain. Int. J. Epidemiol. 1993, 22, 512–519. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Diseases, 10th Revision (ICD-10); World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Bes-Rastrollo, M.; Pérez Valdivieso, J.R.; Sanchez-Villegas, A.; Alonso, Á.; Martínez-González, M.Á. Validity of self-reported weight and body mass index of participants in a cohort of university graduates. Rev. Esp. Obes. 2005, 3, 183–189. [Google Scholar]
- Alonso, A.; Beunza, J.J.; Delgado-Rodríguez, M.; Martínez-González, M.A. Validation of self reported diagnosis of hypertension in a cohort of university graduates in Spain. BMC Public Health 2005, 5, 94. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Montero, A.; Beunza, J.J.; Bes-Rastrollo, M.; Barrio, M.T.; de la Fuente-Arrillaga, C.; Moreno-Galarraga, L.; Martínez-González, M.A. Validity of self-reported metabolic syndrome components in a cohort study. Gac. Sanit. 2011, 25, 303–307. [Google Scholar] [PubMed]
- Martinez-Gonzalez, M.A.; López-Fontana, C.; Varo, J.J.; Sánchez-Villegas, A.; Martinez, J.A. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005, 8, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Ronksley, P.E.; Brien, S.E.; Turner, B.J.; Mukamal, K.J.; Ghali, W.A. Association of alcohol consumption with selected cardiovascular disease outcomes: A systematic review and meta-analysis. BMJ 2011, 342, d671. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; Chiuve, S.E.; Rimm, E.B. Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Arch. Intern. Med. 2006, 166, 2145–2150. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; Conigrave, K.M.; Mittleman, M.A.; Camargo, C.A., Jr.; Stampfer, M.J.; Willett, W.C.; Rimm, E.B. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N. Engl. J. Med. 2003, 348, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C.; Stefanadis, C.; Toutouzas, P. Risk stratification of coronary heart disease through established and emerging lifestyle factors in a Mediterranean population: CARDIO2000 epidemiological study. J. Cardiovasc. Risk 2001, 8, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Chrysohoou, C.; Panagiotakos, D.B.; Pitsavos, C.; Skoumas, J.; Toutouza, M.; Papaioannou, I.; Toutouzas, P.K.; Stefanadis, C. Effects of chronic alcohol consumption on lipid levels, inflammatory and haemostatic factors in the general population: The “ATTICA” Study. Eur. J. Cardiovasc. Prev. Rehabil. 2003, 10, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Wallerath, T.; Poleo, D.; Li, H.; Förstermann, U. Red wine increases the expression of human endothelial nitric oxide synthase: A mechanism that may contribute to its beneficial cardiovascular effects. J. Am. Coll. Cardiol. 2003, 41, 471–478. [Google Scholar] [CrossRef]
- Demrow, H.S.; Slane, P.R.; Folts, J.D. Administration of wine and grape juice inhibits in vivo platelet activity and thrombosis in stenosed canine coronary arteries. Circulation 1995, 91, 1182–1188. [Google Scholar] [CrossRef] [PubMed]
- Shimada, K.; Watanabe, H.; Hosoda, K.; Takeuchi, K.; Yoshikawa, J. Effect of red wine on coronary flow-velocity reserve. Lancet 1999, 354, 1002. [Google Scholar] [CrossRef] [PubMed]
- Rehm, J.; Greenfield, T.K.; Rogers, J.D. Average volume of alcohol consumption, patterns of drinking, and all-cause mortality: Results from the US National Alcohol Survey. Am. J. Epidemiol. 2001, 153, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Gronbaek, M.; Becker, U.; Johansen, D.; Gottschau, A.; Schnohr, P.; Hein, H.O.; Jensen, G.; Sørensen, T.I. Type of alcohol consumed and mortality from all causes, coronary heart disease, and cancer. Ann. Intern. Med. 2000, 133, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Di Castelnuovo, A.; Rotondo, S.; Iacoviello, L.; Donati, M.B.; de Gaetano, G. Meta-analysis of wine and beer consumption in relation to vascular risk. Circulation 2002, 105, 2836–2844. [Google Scholar] [CrossRef] [PubMed]
- Klatsky, A.L.; Friedman, G.D.; Armstrong, M.A.; Kipp, H. Wine, liquor, beer, and mortality. Am. J. Epidemiol. 2003, 158, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Brien, S.E.; Ronksley, P.E.; Turner, B.J.; Mukamal, K.J.; Ghali, W.A. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: Systematic review and meta-analysis of interventional studies. BMJ 2011, 342, d636. [Google Scholar] [CrossRef] [PubMed]
- Imhof, A.; Woodward, M.; Doering, A.; Helbecque, N.; Loewel, H.; Amouyel, P.; Lowe, G.D.; Koenig, W. Overall alcohol intake, beer, wine, and systemic markers of inflammation in western Europe: Results from three MONICA samples (Augsburg, Glasgow, Lille). Eur. Heart J. 2004, 25, 2092–2100. [Google Scholar] [CrossRef] [PubMed]
- Opie, L.H.; Lecour, S. The red wine hypothesis: From concepts to protective signalling molecules. Eur. Heart J. 2007, 28, 1683–1693. [Google Scholar] [CrossRef] [PubMed]
- Fuhrman, B.; Lavy, A.; Aviram, M. Consumption of red wine with meals reduces the susceptibility of human plasma and low-density lipoprotein to lipid peroxidation. Am. J. Clin. Nutr. 1995, 61, 549–554. [Google Scholar] [PubMed]
- Hatonen, K.A.; Virtamo, J.; Eriksson, J.G.; Perälä, M.M.; Sinkko, H.K.; Leiviskä, J.; Valsta, L.M. Modifying effects of alcohol on the postprandial glucose and insulin responses in healthy subjects. Am. J. Clin. Nutr. 2012, 96, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Ruidavets, J.B.; Bataille, V.; Dallongeville, J.; Simon, C.; Bingham, A.; Amouyel, P.; Arveiler, D.; Ducimetière, P.; Ferrières, J. Alcohol intake and diet in France, the prominent role of lifestyle. Eur. Heart J. 2004, 25, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Barefoot, J.C.; Grønbaek, M.; Feaganes, J.R.; McPherson, R.S.; Williams, R.B.; Siegler, I.C. Alcoholic beverage preference, diet, and health habits in the UNC Alumni Heart Study. Am. J. Clin. Nutr. 2002, 76, 466–472. [Google Scholar] [PubMed]
- Laatikainen, T.; Manninen, L.; Poikolainen, K.; Vartiainen, E. Increased mortality related to heavy alcohol intake pattern. J. Epidemiol. Community Health 2003, 57, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Malyutina, S.; Bobak, M.; Kurilovitch, S.; Gafarov, V.; Simonova, G.; Nikitin, Y.; Marmot, M. Relation between heavy and binge drinking and all-cause and cardiovascular mortality in Novosibirsk, Russia: A prospective cohort study. Lancet 2002, 360, 1448–1454. [Google Scholar] [CrossRef]
- Schulz, K.F.; Grimes, D.A. Sample size calculations in randomised trials: Mandatory and mystical. Lancet 2005, 365, 1348–1353. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernandez-Hernandez, A.; Gea, A.; Ruiz-Canela, M.; Toledo, E.; Beunza, J.-J.; Bes-Rastrollo, M.; Martinez-Gonzalez, M.A. Mediterranean Alcohol-Drinking Pattern and the Incidence of Cardiovascular Disease and Cardiovascular Mortality: The SUN Project. Nutrients 2015, 7, 9116-9126. https://doi.org/10.3390/nu7115456
Hernandez-Hernandez A, Gea A, Ruiz-Canela M, Toledo E, Beunza J-J, Bes-Rastrollo M, Martinez-Gonzalez MA. Mediterranean Alcohol-Drinking Pattern and the Incidence of Cardiovascular Disease and Cardiovascular Mortality: The SUN Project. Nutrients. 2015; 7(11):9116-9126. https://doi.org/10.3390/nu7115456
Chicago/Turabian StyleHernandez-Hernandez, Aitor, Alfredo Gea, Miguel Ruiz-Canela, Estefania Toledo, Juan-José Beunza, Maira Bes-Rastrollo, and Miguel A. Martinez-Gonzalez. 2015. "Mediterranean Alcohol-Drinking Pattern and the Incidence of Cardiovascular Disease and Cardiovascular Mortality: The SUN Project" Nutrients 7, no. 11: 9116-9126. https://doi.org/10.3390/nu7115456





