Dietary and Health Profiles of Spanish Women in Preconception, Pregnancy and Lactation
Abstract
:1. Introduction
2. Experimental Section
2.1. Subject Recruitment
2.2. The Survey
2.3. Data Collection
2.4. Statistical Analyses and Additional Calculations
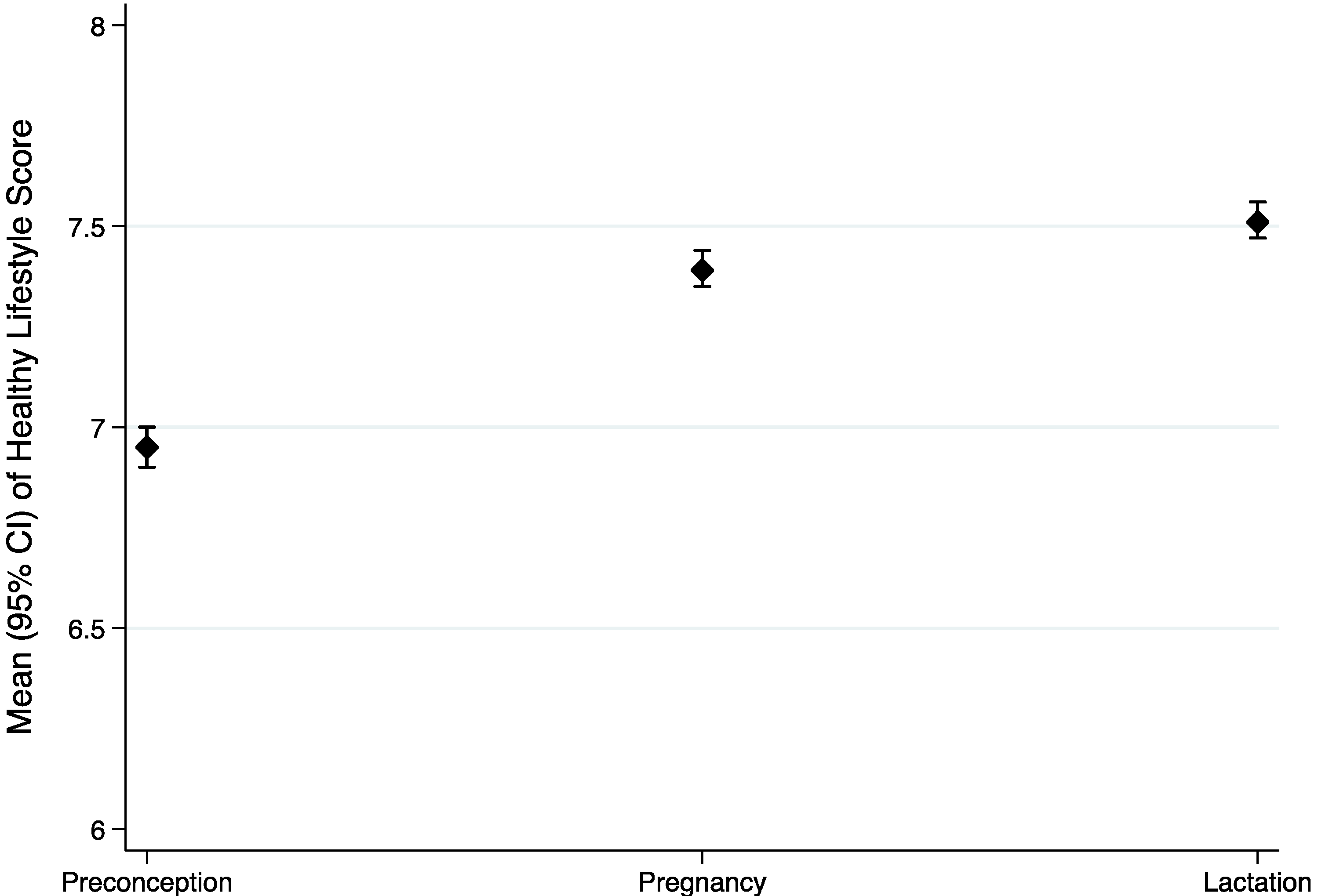
3. Results
| Characteristics | All | Pre-Conception | Pregnancy | Lactation | p a |
|---|---|---|---|---|---|
| N | 13,845 | 4471 | 5087 | 4287 | |
| Age (years) | 31.8 (4.7) | 31.4 (4.8) | 31.9 (4.6) | 32.2 (4.6) | <0.001 |
| Height (cm) | 164.0 (6.1) | 164.0 (6.1) | 164.1 (6.2) | 164.1 (6.1) | 0.621 |
| Weight (kg) | 61.3 (8.9) | 61.4 (9.6) | 61.2 (8.4) | 61.3 (8.6) | 0.432 |
| BMI (kg/m2) | 22.8 (3.3) | 22.9 (3.9) | 22.7 (3.0) | 22.8 (3.0) | 0.926 |
| Activity factor | 1.43 (0.05) | 1.43 (0.05) | 1.41 (0.05) | 1.45 (0.06) | <0.001 |
| Education level (%) | |||||
| No studies | 1.8 | 1.7 | 2.10 | 1.6 | <0.001 |
| Primary | 16.0 | 13.2 | 16.8 | 18.1 | |
| High school | 35.1 | 34.1 | 34.9 | 36.4 | |
| University graduate | 47.1 | 51.1 | 46.2 | 43.9 | |
| Self-perception of health (%) | |||||
| Very good | 21.4 | 19.4 | 22.3 | 22.4 | <0.001 |
| Good | 65.5 | 66.3 | 63.7 | 66.7 | |
| Regular | 11.3 | 12.1 | 12.1 | 9.6 | |
| Bad | 0.8 | 0.7 | 1.0 | 0.7 | |
| Very bad | 0.3 | 0.3 | 0.3 | 0.2 | |
| Don’t know | 0.7 | 1.1 | 0.7 | 0.7 | |
| Self-perception of actual nutrition * (%) | |||||
| Very Balanced | 45.9 | 44.8 | 47.3 | 45.5 | <0.001 |
| Balanced | 38.7 | 36.6 | 39.6 | 39.7 | |
| Medium balanced | 13.0 | 15.9 | 11.0 | 12.4 | |
| Non balanced | 0.6 | 0.7 | 0.4 | 0.9 | |
| Don’t know | 1.8 | 2.1 | 1.7 | 1.5 | |
| Tobacco | |||||
| Never | 63.7 | 56.3 | 67.1 | 67.4 | <0.001 |
| Former/passive | 22.9 | 23.2 | 23.9 | 21.3 | |
| Actual | 13.4 | 20.4 | 9.0 | 11.4 | |
| Alcohol | |||||
| No | 67.3 | 51.0 | 75.4 | 74.6 | <0.001 |
| Yes | 32.7 | 49 | 24.6 | 25.4 | |
| Illicit Drugs | |||||
| Never | 97.8 | 96.9 | 98.2 | 98.4 | <0.001 |
| Former | 1.3 | 1.6 | 1.3 | 1.1 | |
| Actual | 0.9 | 1.5 | 0.5 | 0.5 | |
| Special Diets ** | |||||
| No | 85.0 | 83.8 | 85.7 | 85.4 | 0.021 |
| Yes | 15.0 | 16.2 | 14.3 | 14.6 | |
| Diet supplementation (yes %) | |||||
| Enriched milk with calcium/vitamins | 24.1 | 21.1 | 24.9 | 26.2 | <0.001 |
| Folic acid/vitamin B12 | 49.5 | 48.9 | 74.7 | 20.4 | |
| Iodine/Iodine salt | 30.5 | 26.1 | 41.3 | 22.3 | |
| Iron | 32.5 | 16.0 | 46.1 | 33.7 | |
| Multivitamin and minerals | 21.3 | 14.1 | 26.7 | 22.4 | |
| Other supplements | 39.7 | 35.9 | 48.9 | 32.7 | |
| No supplementation | 18.3 | 26.1 | 5.8 | 25.2 | |
| Main fat consumed | |||||
| Olive oil | 92.2 | 91.2 | 92.9 | 92.4 | 0.008 |
| Others | 7.8 | 8.8 | 7.1 | 7.6 |
| Servings/Day | Physiological Status | p | |||||
|---|---|---|---|---|---|---|---|
| Preconception | Pregnancy | Lactation | |||||
| Mean (SD) | SENC † | Mean (SD) | SENC † | Mean (SD) | SENC † | ||
| N | 4471 | 5087 | 2 | 4287 | 2 | ||
| Protein group | 1.96 ‡ (1.64) | 2 | 1.96 ‡ (1.18) | 1.98 (1.13) | <0.001 | ||
| Meat | 0.58 (0.58) | 0.59 (0.51) | 0.61 (0.50) | <0.001 | |||
| Fish | 0.42 (0.50) | 0.44 (0.47) | 0.43 (0.40) | <0.001 | |||
| Eggs | 0.36 (0.31) | 0.34 (0.23) | 0.35 (0.27) | 0.10 | |||
| Legumes | 0.32 (0.50) | 0.33 (0.39) | 0.32 (0.39) | 0.001 | |||
| Nuts | 0.27 (0.56) | 0.27 (0.48) | 0.26 (0.52) | 0.04 | |||
| Cereal group | 2.39 ‡ (1.56) | 3 | 2.38 ‡ (1.51) | 4 | 2.42 ‡ (1.53) | 4 | 0.34 |
| Bread | 1.72 (1.23) | 1.71 (1.23) | 1.73 (1.22) | 0.78 | |||
| Rice, pasta and potatoes | 0.66 (0.71) | 0.67 (0.68) | 0.70 (0.73) | 0.01 | |||
| Dairy | 2.00 (1.19) | 2 | 2.26 ‡ (1.26) | 3 | 2.30 ‡ (1.33) | 4 | <0.001 |
| Salad and vegetables | 1.22 ‡ (1.00) | 2 | 1.26 ‡ (1.01) | 2 | 1.24 ‡ (0.98) | 2 | 0.10 |
| Fresh fruits | 1.82 ‡ (1.33) | 2 | 2.06 (1.36) | 2 | 1.93 ‡ (1.34) | 2 | <0.001 |
| Sausages | 0.46 * (0.58) | Occasionally | 0.36 * (0.50) | Occasionally | 0.43 * (0.54) | Occasionally | <0.001 |
| Buns and pastries | 0.43 * (0.88) | Occasionally | 0.35 * (0.59) | Occasionally | 0.40 * (0.67) | Occasionally | <0.001 |
| Characteristics | Condition to Score | Points |
|---|---|---|
| Olive oil as principal fat | Yes | 1 |
| Protein group 1,4 | ≥1 serving/day | 1 |
| Cereal group 2,5 | 3–6 servings/day | 1 |
| Salad and vegetables 6 | ≥2 servings/day | 1 |
| Fresh fruits 7 | ≥2 servings/day | 1 |
| Sausages 8 | ≤1 serving/day | 1 |
| Buns and pastries 3,9 | <2 servings/week | 1 |
| Tobacco | Never | 1 |
| Former | 0 | |
| Actual | −1 | |
| Illicit drugs | Never | 1 |
| Former | 0 | |
| Actual | −1 | |
| Activity factor | Above the median | 1 |
| Pre-gestational BMI | 18.5–24.9 kg/m2 | 1 |
| Total | −2 to 11 |
| Predictors * | Simple Linear Regression | Stepwise Regression (Cumulative R2) | ||
|---|---|---|---|---|
| Preconception | Pregnancy | Lactation | Total | |
| N | 4471 | 5087 | 4287 | 13,845 |
| Healthy Score | R2 | R2 | R2 | R2 |
| Tobacco | 0.340 | 0.254 | 0.268 | 0.299 |
| Fresh fruits | 0.256 | 0.274 | 0.265 | 0.512 |
| Salads and vegetables | 0.175 | 0.238 | 0.226 | 0.614 |
| Buns and pastries | 0.157 | 0.167 | 0.148 | 0.694 |
| Activity factor | 0.125 | 0.121 | 0.098 | 0.793 |
| Pre-gestational BMI | 0.102 | 0.060 | 0.076 | 0.855 |
| Olive oil | 0.077 | 0.071 | 0.070 | 0.879 |
| Cereal group | 0.054 | 0.076 | 0.076 | 0.947 |
| Illicit drugs | 0.068 | 0.054 | 0.044 | 0.964 |
| Sausages | 0.036 | 0.024 | 0.021 | 0.977 |
| Protein group | 0.026 | 0.026 | 0.022 | 1.00 |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Harnisch, J.M.; Harnisch, P.H.; Harnisch, D.R., Sr. Family medicine obstetrics: Pregnancy and nutrition. Prim. Care 2012, 39, 39–54. [Google Scholar]
- Kaiser, L.; Allen, L.H.; American Dietetic Association. Position of the American dietetic association: Nutrition and lifestyle for a healthy pregnancy outcome. J. Am. Diet. Assoc. 2008, 108, 553–561. [Google Scholar]
- Lumley, J.; Watson, L.; Watson, M.; Bower, C. Periconceptional supplementation with folate and/or multivitamins for preventing neural tube defects. Cochrane Database Syst. Rev. 2001, 3, CD001056. [Google Scholar] [CrossRef]
- Gardiner, P.M.; Nelson, L.; Shellhaas, C.S.; Dunlop, A.L.; Long, R.; Andrist, S.; Jack, B.W. The clinical content of preconception care: Nutrition and dietary supplements. Am. J. Obstet. Gynecol. 2008, 199, S345–S356. [Google Scholar] [CrossRef] [PubMed]
- Temel, S.; van Voorst, S.F.; Jack, B.W.; Denktas, S.; Steegers, E.A. Evidence-based preconceptional lifestyle interventions. Epidemiol. Rev. 2014, 36, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.; Nisenblat, V.; Norman, R. Lifestyle factors in people seeking infertility treatment—A review. Aust. N. Z. J. Obstet. Gynaecol. 2010, 50, 8–20. [Google Scholar] [CrossRef]
- Toledo, E.; Lopez-del Burgo, C.; Ruiz-Zambrana, A.; Donazar, M.; Navarro-Blasco, I.; Martinez-Gonzalez, M.A.; de Irala, J. Dietary patterns and difficulty conceiving: A nested case-control study. Fertil. Steril. 2011, 96, 1149–1153. [Google Scholar] [CrossRef] [PubMed]
- Practice Committee of American Society for Reproductive Medicine in collaboration with Society for Reproductive Endocrinology and Infertility. Optimizing natural fertility: A committee opinion. Fertil. Steril. 2013, 100, 631–637.
- Symonds, M.E.; Mendez, M.A.; Meltzer, H.M.; Koletzko, B.; Godfrey, K.; Forsyth, S.; van der Beek, E.M. Early life nutritional programming of obesity: Mother-child cohort studies. Ann. Nutr. Metab. 2013, 62, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M.; Gluckman, P. Developmental origins of noncommunicable disease: Population and public health implications. Am. J. Clin. Nutr. 2011, 94, 1754S–1758S. [Google Scholar] [CrossRef] [PubMed]
- Wadhwa, P.D.; Buss, C.; Entringer, S.; Swanson, J.M. Developmental origins of health and disease: Brief history of the approach and current focus on epigenetic mechanisms. Semin. Reprod. Med. 2009, 27, 358–368. [Google Scholar] [CrossRef]
- Bautista-Castano, I.; Henriquez-Sanchez, P.; Aleman-Perez, N.; Garcia-Salvador, J.J.; Gonzalez-Quesada, A.; Garcia-Hernandez, J.A.; Serra-Majem, L. Maternal obesity in early pregnancy and risk of adverse outcomes. PLoS One 2013, 8, e80410. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Liu, E.; Guo, J.; Pan, L.; Li, B.; Wang, P.; Liu, J.; Wang, Y.; Liu, G.; Baccarelli, A.A.; et al. Maternal prepregnancy body mass index and gestational weight gain on pregnancy outcomes. PLoS One 2013, 8, e82310. [Google Scholar] [CrossRef]
- Tobias, D.K.; Zhang, C.; Chavarro, J.; Bowers, K.; Rich-Edwards, J.; Rosner, B.; Mozaffarian, D.; Hu, F.B. Prepregnancy adherence to dietary patterns and lower risk of gestational diabetes mellitus. Am. J. Clin. Nutr. 2012, 96, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Sotres-Alvarez, D.; Siega-Riz, A.M.; Herring, A.H.; Carmichael, S.L.; Feldkamp, M.L.; Hobbs, C.A.; Olshan, A.F.; National Birth Defects Prevention Study. Maternal dietary patterns are associated with risk of neural tube and congenital heart defects. Am. J. Epidemiol. 2013, 177, 1279–1288. [Google Scholar] [CrossRef]
- Mendez, M.A.; Kogevinas, M. A comparative analysis of dietary intakes during pregnancy in Europe: A planned pooled analysis of birth cohort studies. Am. J. Clin. Nutr. 2011, 94, 1993S–1999S. [Google Scholar] [CrossRef] [PubMed]
- Blumfield, M.L.; Hure, A.J.; Macdonald-Wicks, L.K.; Patterson, A.J.; Smith, R.; Collins, C.E. Disparities exist between national food group recommendations and the dietary intakes of women. BMC Womens Health 2011, 11, 37. [Google Scholar] [CrossRef] [PubMed]
- Blumfield, M.L.; Hure, A.J.; Macdonald-Wicks, L.; Smith, R.; Collins, C.E. Systematic review and meta-analysis of energy and macronutrient intakes during pregnancy in developed countries. Nutr. Rev. 2012, 70, 322–336. [Google Scholar] [CrossRef] [PubMed]
- Haider, B.A.; Bhutta, Z.A. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst. Rev. 2012, 11, CD004905. [Google Scholar] [CrossRef]
- Blumfield, M.L.; Hure, A.J.; Macdonald-Wicks, L.; Smith, R.; Collins, C.E. A systematic review and meta-analysis of micronutrient intakes during pregnancy in developed countries. Nutr. Rev. 2013, 71, 118–132. [Google Scholar] [CrossRef] [PubMed]
- Amorim Adegboye, A.R.; Linne, Y.M. Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst. Rev. 2013, 7, CD005627. [Google Scholar] [CrossRef]
- James, D.C.; Lessen, R.; American Dietetic Association. Position of the American dietetic association: Promoting and supporting breastfeeding. J. Am. Diet. Assoc. 2009, 109, 1926–1942. [Google Scholar]
- Valentine, C.J.; Wagner, C.L. Nutritional management of the breastfeeding dyad. Pediatr. Clin. N. Am. 2013, 60, 261–274. [Google Scholar] [CrossRef]
- Innis, S.M. Impact of maternal diet on human milk composition and neurological development of infants. Am. J. Clin. Nutr. 2014, 99, 734S–741S. [Google Scholar] [CrossRef] [PubMed]
- Cuco, G.; Fernandez-Ballart, J.; Sala, J.; Viladrich, C.; Iranzo, R.; Vila, J.; Arija, V. Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur. J. Clin. Nutr. 2006, 60, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Cárcel, C.; Quiles, J.; Rico, B.; Sanchis, T.; Quiles, J.; Rico, B.; Sanchis, T. Adecuación de la ingesta nutricional de embarazadas de segundo y tercer trimestre. Rev. Esp. Nutr. Comunitaria 2005, 11, 136–144. [Google Scholar]
- Larranaga, I.; Santa-Marina, L.; Begiristain, H.; Machon, M.; Vrijheid, M.; Casas, M.; Tardon, A.; Fernandez-Somoano, A.; Llop, S.; Rodriguez-Bernal, C.L.; et al. Socio-economic inequalities in health, habits and self-care during pregnancy in Spain. Matern. Child Health J. 2013, 17, 1315–1324. [Google Scholar] [CrossRef]
- Goni, L.; Martínez, J.A.; Santiago, S.; Cuervo, M. Validación de una encuesta para evaluar el estado nutricional y los estilos de vida en las etapas preconcepcional, embarazo y lactancia. Rev. Esp. Nutr. Comunitaria 2013, 19, 105–113. [Google Scholar]
- Chatzi, L.; Mendez, M.; Garcia, R.; Roumeliotaki, T.; Ibarluzea, J.; Tardon, A.; Amiano, P.; Lertxundi, A.; Iniguez, C.; Vioque, J.; et al. Mediterranean diet adherence during pregnancy and fetal growth: INMA (Spain) and RHEA (Greece) mother-child cohort studies. Br. J. Nutr. 2012, 107, 135–145. [Google Scholar] [CrossRef]
- Aranda, N.; Ribot, B.; Garcia, E.; Viteri, F.E.; Arija, V. Pre-pregnancy iron reserves, iron supplementation during pregnancy, and birth weight. Early Hum. Dev. 2011, 87, 791–797. [Google Scholar] [CrossRef]
- Vila, L.; Serra-Prat, M.; de Castro, A.; Palomera, E.; Casamitjana, R.; Legaz, G.; Barrionuevo, C.; Munoz, J.A.; Garcia, A.J.; Lal-Trehan, S.; et al. Iodine nutritional status in pregnant women of two historically different iodine-deficient areas of Catalonia, Spain. Nutrition 2011, 27, 1029–1033. [Google Scholar] [CrossRef]
- Palma, S.; Perez-Iglesias, R.; Pardo-Crespo, R.; Llorca, J.; Mariscal, M.; Delgado-Rodriguez, M. Smoking among pregnant women in Cantabria (Spain): Trend and determinants of smoking cessation. BMC Public Health 2007, 7, 65. [Google Scholar] [CrossRef] [PubMed]
- Delgado Pena, Y.P.; Rodriguez Martinez, G.; Samper Villagrasa, M.P.; Caballero Perez, V.; Cuadron Andres, L.; Alvarez Sauras, M.L.; Moreno Aznar, L.A.; Olivares Lopez, J.L.; Grupo Colaborativo CALINA. Socio-cultural, obstetric and anthropometric characteristics of newborn children of mothers who smoke in Spain. An. Pediatr. (Barc.) 2012, 76, 4–9. [Google Scholar]
- Jimenez-Muro, A.; Samper, M.P.; Marqueta, A.; Rodriguez, G.; Nerin, I. Prevalence of smoking and second-hand smoke exposure: Differences between Spanish and immigrant pregnant women. Gac. Sanit. 2012, 26, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, C.; Garcia-Esteban, R.; Mendez, M.; Romieu, I.; Torrent, M.; Sunyer, J. Social determinants of dietary patterns during pregnancy. Gac. Sanit. 2009, 23, 38–43. [Google Scholar] [CrossRef]
- Rius, J.M.; Ortuno, J.; Rivas, C.; Maravall, M.; Calzado, M.A.; Lopez, A.; Aguar, M.; Vento, M. Factors associated with early weaning in a Spanish region. An. Pediatr. (Barc.) 2014, 80, 6–15. [Google Scholar] [CrossRef]
- Aurrekoetxea, J.J.; Murcia, M.; Rebagliato, M.; Lopez, M.J.; Castilla, A.M.; Santa-Marina, L.; Guxens, M.; Fernandez-Somoano, A.; Espada, M.; Lertxundi, A.; et al. Determinants of self-reported smoking and misclassification during pregnancy, and analysis of optimal cut-off points for urinary cotinine: A cross-sectional study. BMJ Open 2013, 3, e002034. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence, NICE. Weight Management before, during and after Pregnancy; NICE: London, UK, 2010; p. 61. [Google Scholar]
- Renfrew, M.J.; McCormick, F.M.; Wade, A.; Quinn, B.; Dowswell, T. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst. Rev. 2012, 5, CD001141. [Google Scholar] [CrossRef] [PubMed]
- Claudot, F.; Fresson, J.; Coudane, H.; Guillemin, F.; Demore, B.; Alla, F. Research in clinical epidemiology: Which rules should be applied? Rev. Epidemiol. Sante Publique 2008, 56, 63–70. [Google Scholar] [CrossRef]
- Portalfarma. Available online www.portalfarma.com (accessed on 5 June 2014).
- Plenufar IV: Educación Nutricional en la Etapa Preconcepcional, Embarazo y Lactancia. Guía para Completar la Encuesta Nutricional. Available online: http://www.portalfarma.com/Profesionales/campanaspf/categorias/Documents/PLFIV_AB_GUIA%20APLICACION%20DE%20LA%20ENCUESTA.pdf (accessed on 5 June 2014).
- Cuervo, M.; Garcia, A.; Ansorena, D.; Sanchez-Villegas, A.; Martinez-Gonzalez, M.; Astiasaran, I.; Martinez, J. Nutritional assessment interpretation on 22,007 Spanish community-dwelling elders through the mini nutritional assessment test. Public Health Nutr. 2009, 12, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Consejo General de Colegios Oficiales de Farmacéuticos. Plan de Educación Nutricional por el Farmacéutico (PLENUFAR 3): Alimentación y Salud en las Personas Mayores; Eurograf Navarra S.L.: Pamplona. Spain, 2005; p. 112. [Google Scholar]
- Food and Agriculture Organization of the United Nations/World Health Organization. Human Vitamins and Mineral Requirements; Report of a Joint FAO/WHO Expert Consultation; FAO: Rome, Italy; WHO: Geneva, Switzerland, 2002. [Google Scholar]
- Sociedad Española de Nutrición Comunitaria (SENC). Consejos para una Alimentación Saludable; SENC: Madrid, Spain, 2007; p. 42. [Google Scholar]
- Wilkinson, S.A.; McIntyre, H.D. Evaluation of the “healthy start to pregnancy” early antenatal health promotion workshop: A randomized controlled trial. BMC Pregnancy Childbirth 2012, 12, 131. [Google Scholar] [CrossRef] [PubMed]
- Rautiainen, S.; Wang, L.; Gaziano, J.M.; Sesso, H.D. Who uses multivitamins? A cross-sectional study in the physicians’ health study. Eur. J. Nutr. 2014, 53, 1065–1072. [Google Scholar] [CrossRef] [PubMed]
- Hu, E.A.; Toledo, E.; Diez-Espino, J.; Estruch, R.; Corella, D.; Salas-Salvado, J.; Vinyoles, E.; Gomez-Gracia, E.; Aros, F.; Fiol, M.; et al. Lifestyles and risk factors associated with adherence to the Mediterranean diet: A baseline assessment of the PREDIMED trial. PLoS One 2013, 8, e60166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [PubMed]
- Navarrete-Munoz, E.M.; Gimenez Monzo, D.; Garcia de La Hera, M.; Climent, M.D.; Rebagliato, M.; Murcia, M.; Iniguez, C.; Ballester, F.; Ramon, R.; Vioque, J. Folic acid intake from diet and supplements in a population of pregnant women in Valencia, Spain. Med. Clin. (Barc.) 2010, 135, 637–643. [Google Scholar] [CrossRef]
- Martinez-Frias, M.L.; Grupo de trabajo del ECEMC. Folic acid dose in the prevention of congenital defects. Med. Clin. (Barc.) 2007, 128, 609–616. [Google Scholar] [CrossRef]
- Ministerio de Sanidad Servicios Sociales e Igualdad. Evaluación Nutricional de la Dieta Española. II. Micronutrientes. Available online: http://aesan.msssi.gob.es/AESAN/docs/docs/evaluacion_riesgos/estudios_evaluacion_nutricional/Valoracion_nutricional_ENIDE_micronutrientes.pdf (accessed on 5 June 2014).
- De-Regil, L.M.; Fernandez-Gaxiola, A.C.; Dowswell, T.; Pena-Rosas, J.P. Effects and safety of periconceptional folate supplementation for preventing birth defects. Cochrane Database Syst. Rev. 2010, 10, CD007950. [Google Scholar] [CrossRef] [PubMed]
- Ray, J.G.; Singh, G.; Burrows, R.F. Evidence for suboptimal use of periconceptional folic acid supplements globally. BJOG 2004, 111, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Tort, J.; Lelong, N.; Prunet, C.; Khoshnood, B.; Blondel, B. Maternal and health care determinants of preconceptional use of folic acid supplementation in France: Results from the 2010 national perinatal survey. BJOG 2013, 120, 1661–1667. [Google Scholar] [CrossRef]
- Sicinska, E.; Wyka, J. Folate intake in Poland on the basis of literature from the last ten years (2000–2010). Rocz. Panstw. Zakl. Hig. 2011, 62, 247–256. [Google Scholar]
- McNally, S.; Bourke, A. Periconceptional folic acid supplementation in a nationally representative sample of mothers. Ir. Med. J. 2012, 105, 236–238. [Google Scholar] [PubMed]
- Silva-del Valle, M.A.; Sanchez-Villegas, A.; Serra-Majem, L. Association between the adherence to the Mediterranean diet and overweight and obesity in pregnant women in Gran Canaria. Nutr. Hosp. 2013, 28, 654–659. [Google Scholar] [PubMed]
- Rodriguez-Bernal, C.L.; Ramon, R.; Quiles, J.; Murcia, M.; Navarrete-Munoz, E.M.; Vioque, J.; Ballester, F.; Rebagliato, M. Dietary intake in pregnant women in a Spanish Mediterranean area: As good as it is supposed to be? Public Health Nutr. 2013, 16, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, A.L.; Logue, K.M.; Thorne, C.; Badal, H.J. Change in women’s knowledge of general and personal preconception health risks following targeted brief counseling in publicly funded primary care settings. Am. J. Health Promot. 2013, 27, S50–S57. [Google Scholar] [PubMed]
- Juarez, S.; Revuelta-Eugercios, B.A.; Ramiro-Farinas, D.; Viciana-Fernandez, F. Maternal education and perinatal outcomes among Spanish women residing in southern Spain (2001–2011). Matern. Child Health J. 2013, 18, 1814–1822. [Google Scholar] [CrossRef]
- Zhou, S.J.; Anderson, A.J.; Gibson, R.A.; Makrides, M. Effect of iodine supplementation in pregnancy on child development and other clinical outcomes: A systematic review of randomized controlled trials. Am. J. Clin. Nutr. 2013, 98, 1241–1254. [Google Scholar] [CrossRef]
- Donnay, S.; Arena, J.; Lucas, A.; Velasco, I.; Ares, S.; Working Group on Disorders Related to Iodine Deficiency and Thyroid Dysfunction of the Spanish Society of Endocrinology and Nutrition. Iodine supplementation during pregnancy and lactation. Position statement of the working group on disorders related to iodine deficiency and thyroid dysfunction of the Spanish society of endocrinology and nutrition. Endocrinol. Nutr. 2014, 61, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, C.L.; Rodriguez, A.B.; Sanchez, J.; Gonzalez, R.; Rivero, M.; Barriga, C.; Cubero, J. Calcium intake nutritional status in breastfeeding women. Arch. Latinoam. Nutr. 2008, 58, 371–376. [Google Scholar] [PubMed]
- Arija, V.; Cuco, G.; Vila, J.; Iranzo, R.; Fernandez-Ballart, J. Food consumption, dietary habits and nutritional status of the population of Reus: Follow-up from preconception throughout pregnancy and after birth. Med. Clin. (Barc.) 2004, 123, 5–11. [Google Scholar] [CrossRef]
- Anderson, A.S. Symposium on “nutritional adaptation to pregnancy and lactation”. Pregnancy as a time for dietary change? Proc. Nutr. Soc. 2001, 60, 497–504. [Google Scholar]
- Renfrew, M.J.; McFadden, A.; Bastos, M.H.; Campbell, J.; Channon, A.A.; Cheung, N.F.; Silva, D.R.; Downe, S.; Kennedy, H.P.; Malata, A.; et al. Midwifery and quality care: Findings from a new evidence-informed framework for maternal and newborn care. Lancet 2014, 384, 1129–1145. [Google Scholar] [CrossRef] [PubMed]
- Wallner, S.; Kendall, P.; Hillers, V.; Bradshaw, E.; Medeiros, L.C. Online continuing education course enhances nutrition and health professionals’ knowledge of food safety issues of high-risk populations. J. Am. Diet. Assoc. 2007, 107, 1333–1338. [Google Scholar] [CrossRef] [PubMed]
- Suominen, M.H.; Kivisto, S.M.; Pitkala, K.H. The effects of nutrition education on professionals’ practice and on the nutrition of aged residents in dementia wards. Eur. J. Clin. Nutr. 2007, 61, 1226–1232. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuervo, M.; Sayon-Orea, C.; Santiago, S.; Martínez, J.A. Dietary and Health Profiles of Spanish Women in Preconception, Pregnancy and Lactation. Nutrients 2014, 6, 4434-4451. https://doi.org/10.3390/nu6104434
Cuervo M, Sayon-Orea C, Santiago S, Martínez JA. Dietary and Health Profiles of Spanish Women in Preconception, Pregnancy and Lactation. Nutrients. 2014; 6(10):4434-4451. https://doi.org/10.3390/nu6104434
Chicago/Turabian StyleCuervo, Marta, Carmen Sayon-Orea, Susana Santiago, and Jose Alfredo Martínez. 2014. "Dietary and Health Profiles of Spanish Women in Preconception, Pregnancy and Lactation" Nutrients 6, no. 10: 4434-4451. https://doi.org/10.3390/nu6104434





