Knowledge and Attitudes Are Related to Selected Salt-Specific Behaviours among Australian Parents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Recruitment
2.2. Shopping Center Recruitment and Data Collection
2.3. Facebook Advertisement Campaign
2.4. GMI Consumer Research Panel
2.5. Survey Instrument
2.5.1. Demographic Characteristics
2.5.2. Knowledge Related to Salt Intake
Parents’ Knowledge Related to Children’s Salt Intake
Parents’ Knowledge Related to the Salt Intake of Adults
2.5.3. Attitudes Related to Salt Intake
Parents’ Attitudes Related to Children’s Salt Intake
Parents’ Attitudes Related to Salt intake of Adults
2.5.4. Behaviours Related to Salt Intake
Salt-Related Behaviours of Parents Specific to Their Children
Parents’ Own Salt-Related Behaviours
2.6. Data Analysis
3. Results
3.1. Demographic Characteristics
3.2. Knowledge
3.3. Attitudes
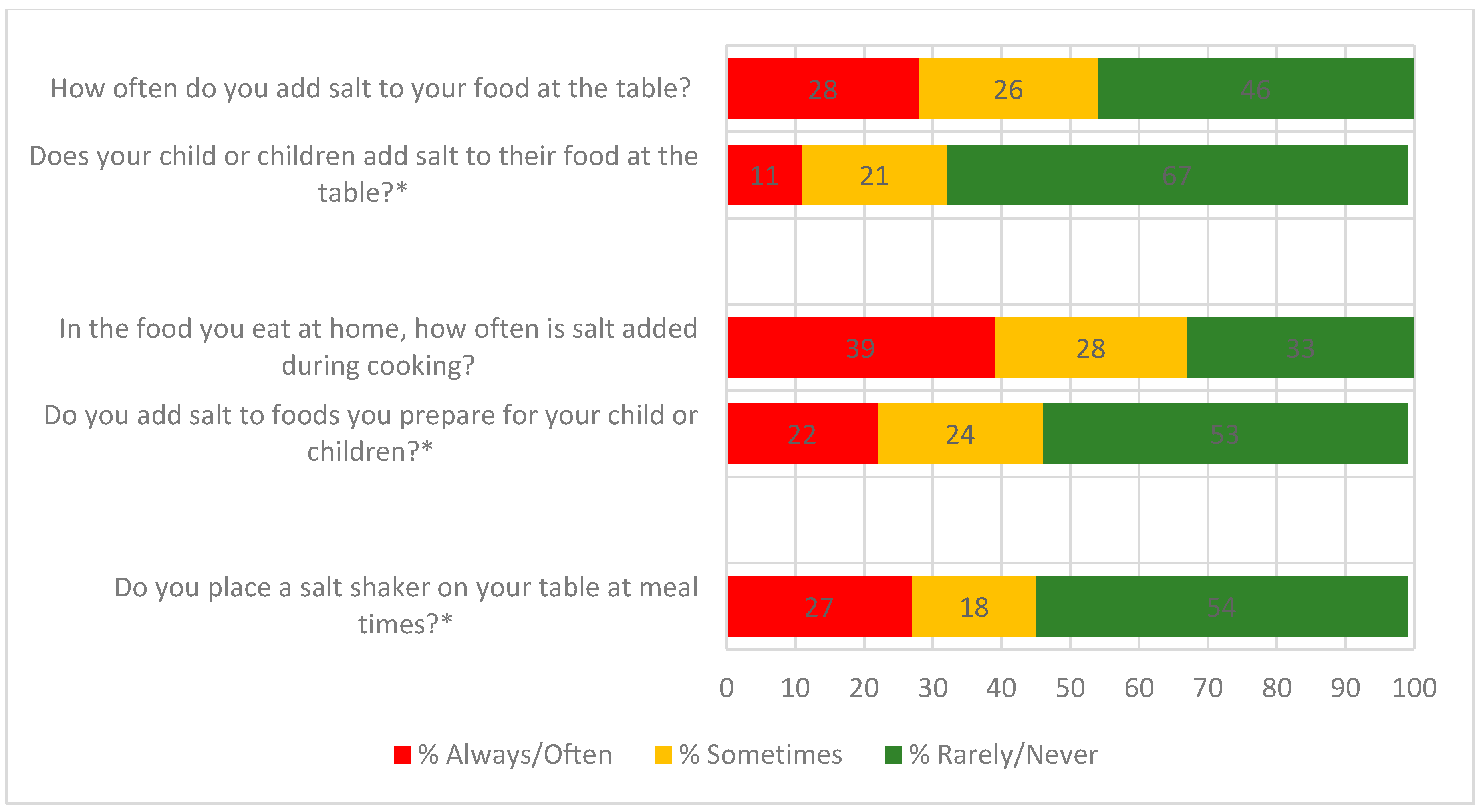
3.4. Behaviours
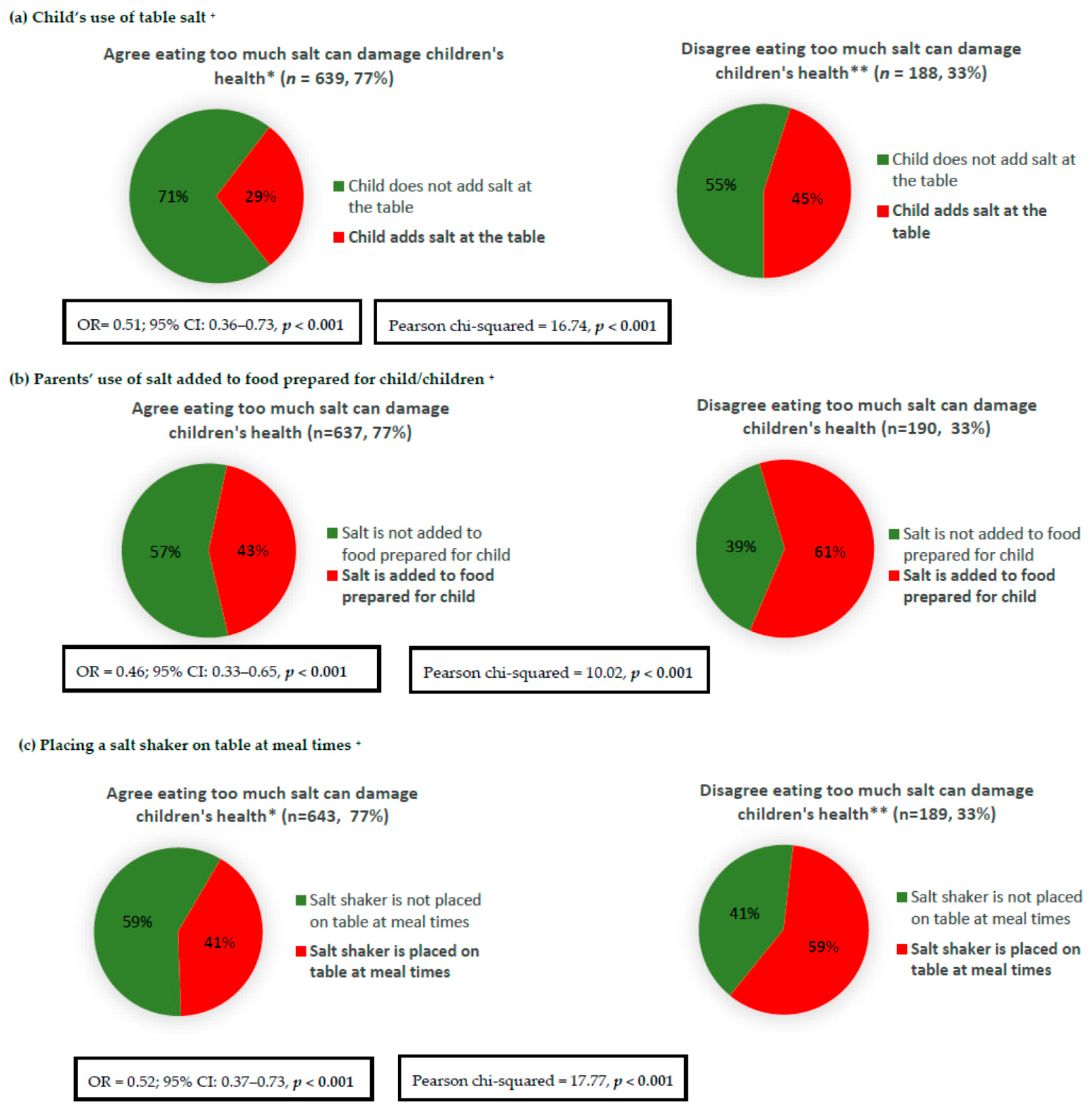
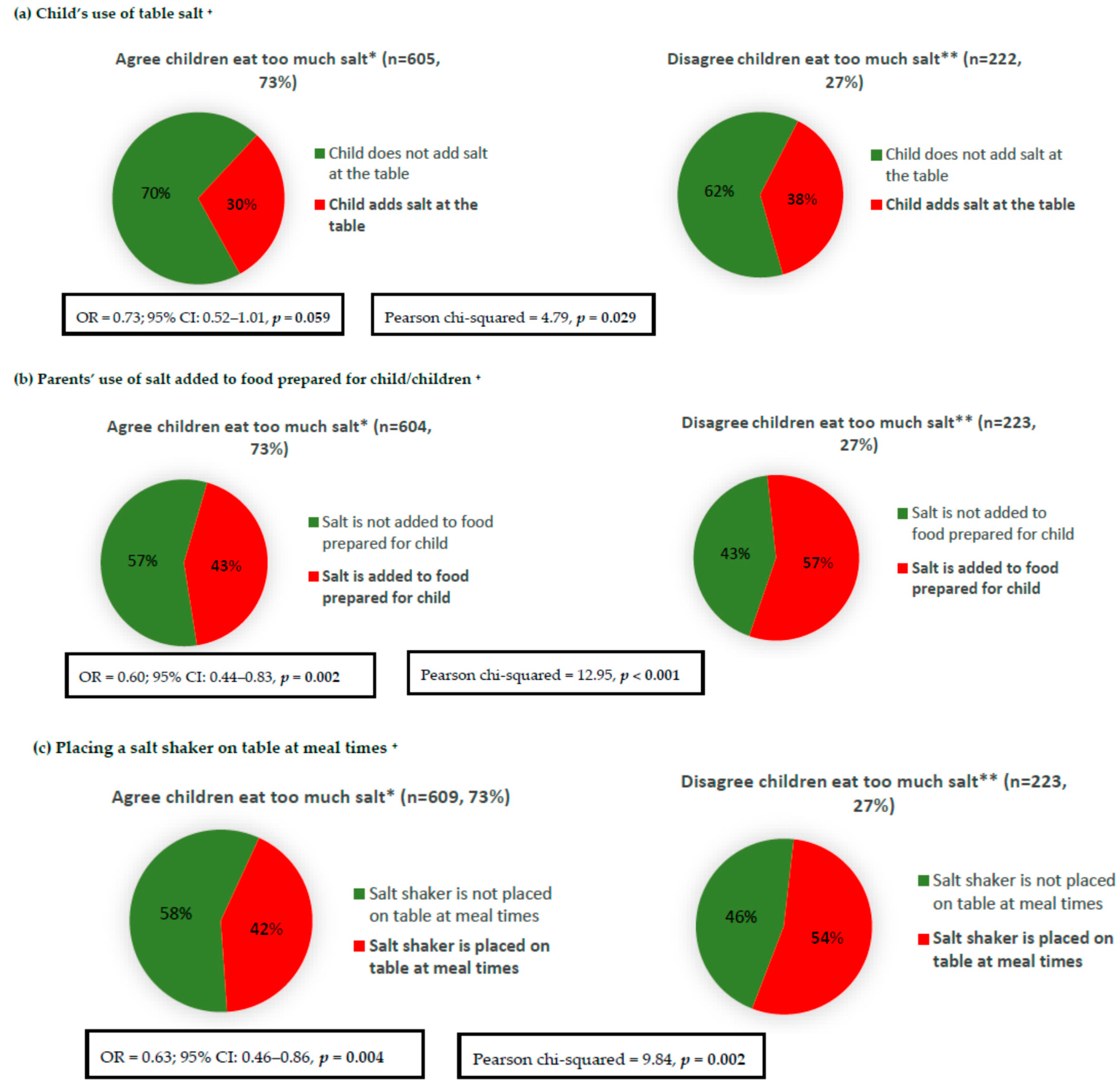
Association of Salt-Related Knowledge and Attitudes with Behaviours
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Land, M.A.; Neal, B.C.; Johnson, C.; Nowson, C.A.; Margerison, C.; Petersen, K.S. Salt consumption by Australian adults: A systematic review and meta-analysis. Med. J. Aust. 2018, 208, 75–81. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sodium Intake for Adults and Children; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Grimes, C.A.; Riddell, L.J.; Campbell, K.J.; Beckford, K.; Baxter, J.R.; He, F.J.; Nowson, C.A. Dietary intake and sources of sodium and potassium among Australian schoolchildren: Results from the cross-sectional Salt and Other Nutrients in Children (SONIC) study. BMJ Open 2017, 7, e016639. [Google Scholar] [CrossRef] [PubMed]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, F.J.; Li, J.; Macgregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; MacGregor, G.A. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst. Rev. 2004, CD004937. [Google Scholar] [CrossRef]
- World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013–2020; WHO: Geneva, Switzerland, 2013; Available online: http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1 (accessed on 23 June 2017).
- Victorian Health Promotion Foundation. State of Salt: The Case for Salt Reduction in Victoria; VicHealth: Victoria, Australia, 2015. Available online: https://www.vichealth.vic.gov.au/media-and-resources/publications/state-of-salt (accessed on 20 May 2016).
- He, F.J.; Brinsden, H.C.; MacGregor, G.A. Salt reduction in the United Kingdom: A successful experiment in public health. J. Hum. Hypertens. 2014, 28, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Arcand, J.; Mendoza, J.; Qi, Y.; Henson, S.; Lou, W.; L’Abbe, M.R. Results of a national survey examining Canadians’ concern, actions, barriers, and support for dietary sodium reduction interventions. Can. J. Cardiol. 2013, 29, 628–631. [Google Scholar] [CrossRef] [PubMed]
- Charlton, K.; Yeatman, H.; Houweling, F.; Guenon, S. Urinary sodium excretion, dietary sources of sodium intake and knowledge and practices around salt use in a group of healthy Australian women. Aust. N. Z. J. Public Health 2010, 34, 356–363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claro, R.M.; Linders, H.; Ricardo, C.Z.; Legetic, B.; Campbell, N.R. Consumer attitudes, knowledge, and behavior related to salt consumption in sentinel countries of the Americas. Rev. Panam. Salud Publica 2012, 32, 265–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grimes, C.; Kelley, S.J.; Stanley, S.; Bolam, B.; Wesbter, J.; Khokhar, D.; Nowson, C.A. Knowledge, attitudes and behaviours related to dietary salt among adults in the state of Victoria, Australia 2015. BMC Public Health 2017, 17, 532–547. [Google Scholar] [CrossRef] [PubMed]
- Grimes, C.A.; Riddell, L.J.; Nowson, C.A. Consumer knowledge and attitudes to salt intake and labelled salt information. Appetite 2009, 53, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.; Mohan, S.; Rogers, K.; Shivashankar, R.; Thout, S.R.; Gupta, P.; He, F.J.; MacGregor, G.A.; Webster, J.; Krishnan, A.; et al. The Association of Knowledge and Behaviours Related to Salt with 24-h Urinary Salt Excretion in a Population from North and South India. Nutrients 2017, 9, 144. [Google Scholar] [CrossRef] [PubMed]
- Land, M.A.; Webster, J.; Christoforou, A.; Johnson, C.; Trevena, H.; Hodgins, F.; Chalmers, J.; Woodward, M.; Barzi, F.; Smith, W.; et al. The association of knowledge, attitudes and behaviours related to salt with 24-hour urinary sodium excretion. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magalhaes, P.; Sanhangala, E.J.; Dombele, I.M.; Ulundo, H.S.; Capingana, D.P.; Silva, A.B. Knowledge, attitude and behaviour regarding dietary salt intake among medical students in Angola. Cardiovasc. J. Afr. 2015, 26, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Marakis, G.; Tsigarida, E.; Mila, S.; Panagiotakos, D.B. Knowledge, attitudes and behaviour of Greek adults towards salt consumption: A Hellenic Food Authority project. Public Health Nutr. 2014, 17, 1877–1893. [Google Scholar] [CrossRef] [PubMed]
- Nasreddine, L.; Akl, C.; Al-Shaar, L.; Almedawar, M.M.; Isma’eel, H. Consumer knowledge, attitudes and salt-related behavior in the Middle-East: The case of Lebanon. Nutrients 2014, 6, 5079–5102. [Google Scholar] [CrossRef] [PubMed]
- Papadakis, S.; Pipe, A.L.; Moroz, I.A.; Reid, R.D.; Blanchard, C.M.; Cote, D.F.; Mark, A.E. Knowledge, attitudes and behaviours related to dietary sodium among 35- to 50-year-old Ontario residents. Can. J. Cardiol. 2010, 26, e164–e169. [Google Scholar] [CrossRef] [Green Version]
- Webster, J.L.; Li, N.; Dunford, E.K.; Nowson, C.A.; Neal, B.C. Consumer awareness and self-reported behaviours related to salt consumption in Australia. Asia Pac. J. Clin. Nutr. 2010, 19, 550–554. [Google Scholar] [PubMed]
- Zhang, J.; Xu, A.Q.; Ma, J.X.; Shi, X.M.; Guo, X.L.; Engelgau, M.; Yan, L.X.; Li, Y.; Li, Y.C.; Wang, H.C.; et al. Dietary sodium intake: Knowledge, attitudes and practices in Shandong Province, China, 2011. PLoS ONE 2013, 8, e58973. [Google Scholar] [CrossRef] [PubMed]
- Australian Division of World Action on Salt and Health. 2008 Consumer Survey on Parents’ Attitudes to Salt and Children; AWASH: Canberra, Australia, 2008. [Google Scholar]
- Birch, L.; Savage, J.S.; Ventura, A. Influences on the Development of Children’s Eating Behaviours: From Infancy to Adolescence. Can. J. Diet Pract. Res. 2007, 68, s1–s56. [Google Scholar] [PubMed]
- Savage, J.S.; Fisher, J.O.; Birch, L.L. Parental influence on eating behavior: Conception to adolescence. J. Law Med. Ethics 2007, 35, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2011; ABS: Canberra, Australia, 2013. Available online: http://www.abs.gov.au/ausstats/[email protected]/mf/2033.0.55.001 (accessed on 10 January 2016).
- Australian Division of World Action on Salt and Health. 2007 Survey of Australian Consumer Awareness and Practices Relating to Salt Report; AWASH: Sydney, Australia, 2007. [Google Scholar]
- Consensus Action on Salt & Health. Consensus Action on Salt and Health and Your Health—TNS Public Opinion Survey Summary Report. 2010. Available online: http://www.actiononsalt.org.uk/Docs/39307.pdf (accessed on 24 October 2017).
- Food Standards Agency & COI Comminucations. Consumer Attitudes to Food Standards Wave 5; Food Standards Agency & COI Comminucations: London, UK, 2005. [Google Scholar]
- New Zealand Food Safety Authority. Salt Consumer Survey. 2011. Available online: http://www.foodsafety.govt.nz/elibrary/industry/salt-survey.pdf (accessed on 9 December 2015).
- Newson, R.S.; Elmadfa, I.; Biro, G.; Cheng, Y.; Prakash, V.; Rust, P.; Barna, M.; Lion, R.; Meijer, G.W.; Neufingerl, N.; et al. Barriers for progress in salt reduction in the general population. An international study. Appetite 2013, 71, 22–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarmugam, R.; Worsley, A.; Flood, V. Development and validation of a salt knowledge questionnaire. Public Health Nutr. 2014, 17, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. WHO Steps Instrument (Core and Expanded) v3. 2015. Available online: http://www.who.int/chp/steps/instrument/en/ (accessed on 28 January 2016).
- World Health Organisation. BMI Classification; WHO: Geneva, Switzerland, 2016; Available online: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html (accessed on 25 May 2015).
- Sarmugam, R.; Worsley, A.; Wang, W. An examination of the mediating role of salt knowledge and beliefs on the relationship between socio-demographic factors and discretionary salt use: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 25. [Google Scholar] [CrossRef] [PubMed]
- Parmenter, K.; Waller, J.; Wardle, J. Demographic variation in nutrition knowledge in England. Health Educ. Res. 2000, 15, 163–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dallongeville, J.; Marecaux, N.; Cottel, D.; Bingham, A.; Amouyel, P. Association between nutrition knowledge and nutritional intake in middle-aged men from Northern France. Public Health Nutr. 2001, 4, 27–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wardle, J.; Parmenter, K.; Waller, J. Nutrition knowledge and food intake. Appetite 2000, 34, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Steptoe, A. Socioeconomic differences in attitudes and beliefs about healthy lifestyles. J. Epidemiol. Community Health 2003, 57, 440–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birch, L.L. Development of food preferences. Annu. Rev. Nutr. 1999, 19, 41–62. [Google Scholar] [CrossRef] [PubMed]
- Worsley, A. Nutrition knowledge and food consumption: Can nutrition knowledge change food behaviour? Asia Pac. J. Clin. Nutr. 2002, 11 (Suppl. 3), S579–S585. [Google Scholar] [CrossRef] [PubMed]
- Carson, J.A.; Gillham, M.B.; Kirk, L.M.; Reddy, S.T.; Battles, J.B. Enhancing self-efficacy and patient care with cardiovascular nutrition education. Am. J. Prev. Med. 2002, 23, 296–302. [Google Scholar] [CrossRef]
- Kristjansdottir, A.G.; Thorsdottir, I.; De Bourdeaudhuij, I.; Due, P.; Wind, M.; Klepp, K.I. Determinants of fruit and vegetable intake among 11-year-old schoolchildren in a country of traditionally low fruit and vegetable consumption. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Characteristic | ||
|---|---|---|
| N (%) | Mean (±SD) | |
| Gender | ||
| Male | 347 (41%) | |
| Female | 490 (59%) | |
| Age (years) | 41 (10) | |
| Age group (years) | ||
| 18–24 | 37 (4%) | |
| 25–34 | 185 (22%) | |
| 35–44 | 319 (38%) | |
| 45–54 | 211 (25%) | |
| 55–66 | 85 (10%) | |
| Country of birth 1 | ||
| Australia | 686 (83%) | |
| UK | 17 (2%) | |
| New Zealand | 9 (1%) | |
| Other * | 113 (14%) | |
| Language spoken other than English 2 | ||
| English only | 672 (81%) | |
| Other ** | 157 (19%) | |
| Socioeconomic status 3 | ||
| High SES | 369 (44%) | |
| Mid SES | 248 (30%) | |
| Low SES | 212 (26%) | |
| Height (cm) | 169 (10) | |
| Weight (kg) | 78 (18) | |
| BMI (kg/m2) 4 | 27 (6) | |
| Weight Category Distribution4 | ||
| Underweight | 15 (2%) | |
| Healthy weight | 298 (40%) | |
| Overweight | 234 (31%) | |
| Obese | 202 (27%) | |
| No. of children in age groups 5 | ||
| 0–1 years | 133 | |
| 2–4 years | 250 | |
| 5–12 years | 437 | |
| 13–17 years | 303 | |
| Child age group | ||
| Infant/toddler | 196 (23%) | |
| Mid-childhood/adolescence | 505 (60%) | |
| Both | 136 (16%) | |
| Variables | Looked at Food Labels to Check Sodium Content (Yes) * | Avoided Eating Packaged, Ready-To-Eat Foods (Yes) * | Used Spices and Herbs Instead of Salt When Cooking (Yes) * | Avoided Eating from Fast Food Restaurants (Yes) * | Avoided Eating from Asian-Style Restaurants or Takeaway Store (Yes) * | Purchased Foods Labelled ‘No Added Salt’, ‘Reduced Salt/Sodium’ (Yes) * | When Eating out, Asked to Have Meal Prepared without Salt (Yes) * |
|---|---|---|---|---|---|---|---|
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| In the long term eating too much salt may have harmful effects on children’s health | |||||||
| Disagree 1 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Agree 2 | 1.73 (1.23–2.42) | 1.82 (1.24–2.65) | 1.66 (1.11–2.48) | 1.52 (1.03–2.25) | 1.32 (0.93–1.88) | 2.34 (1.65–3.32) | 0.58 (0.41–0.85) |
| How much salt do you think Australian children eat? | |||||||
| Too little 3 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Too much 4 | 1.20 (0.87–1.65) | 1.11 (0.76–1.61) | 1.29 (0.87–1.90) | 1.03 (0.70–1.51) | 0.95 (0.68–1.34) | 1.55 (1.11–2.16) | 0.45 (0.32–0.63) |
| Limiting the amount of salt my child eats is important to me | |||||||
| Disagree 1 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Agree 2 | 1.88 (1.38–2.57) | 2.07 (1.46–2.94) | 1.73 (1.19–2.52) | 1.82 (1.27–2.60) | 1.81 (1.31–2.49) | 2.75 (1.99–3.80) | 0.82 (0.58–1.16) |
| Adding Salt at the Table (Yes) * | Adding Salt during Cooking (Yes) * | Placing Salt Shaker on Table at Meal Times (Yes) * | Looked at Food Labels to Check Sodium Content (Yes) * | Avoided Eating Packaged, Ready-To-Eat Foods (Yes) * | Used Spices and Herbs Instead of Salt When Cooking (Yes) * | Avoided Eating from Fast Food Restaurants (Yes) * | Avoided Eating from Asian-Style Restaurants or Takeaway Store (Yes) * | Purchased Foods Labelled ‘No Added Salt’, ‘Reduced Salt/Sodium’ (Yes) * | When Eating out, Asked to Have Meal Prepared without Salt (Yes) * | |
|---|---|---|---|---|---|---|---|---|---|---|
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| Do you think eating too much salt could damage your health | ||||||||||
| No 1 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Yes | 0.48 (0.36–0.65) | 0.57 (0.41–0.80) | 0.52 (0.39–0.70) | 3.13 (1.84–5.35) | 3.10 (1.82–5.26) | 2.30 (1.34–3.96) | 2.08 (1.21–3.59) | 1.91 (1.14–3.23) | 3.20 (1.92–5.32) | 1.02 (0.59–1.78) |
| How much salt do you think Australian’s eat? | ||||||||||
| Too little 2 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Too much 3 | 0.60 (0.48–0.76) | 0.60 (0.47–0.78) | 0.71 (0.56–0.89) | 0.96 (0.65–1.41) | 1.14 (0.72–1.79) | 1.19 (0.74–1.91) | 1.25 (0.79–1.98) | 0.93 (0.62–1.41) | 1.83 (1.23–2.72) | 0.49 (0.33–0.74) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khokhar, D.; Nowson, C.A.; Margerison, C.; Bolam, B.; Grimes, C.A. Knowledge and Attitudes Are Related to Selected Salt-Specific Behaviours among Australian Parents. Nutrients 2018, 10, 720. https://doi.org/10.3390/nu10060720
Khokhar D, Nowson CA, Margerison C, Bolam B, Grimes CA. Knowledge and Attitudes Are Related to Selected Salt-Specific Behaviours among Australian Parents. Nutrients. 2018; 10(6):720. https://doi.org/10.3390/nu10060720
Chicago/Turabian StyleKhokhar, Durreajam, Caryl Anne Nowson, Claire Margerison, Bruce Bolam, and Carley Ann Grimes. 2018. "Knowledge and Attitudes Are Related to Selected Salt-Specific Behaviours among Australian Parents" Nutrients 10, no. 6: 720. https://doi.org/10.3390/nu10060720





