Control Measures and Health Effects of Air Pollution: A Survey among Public Transportation Commuters in Malaysia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants and Settings
2.2. Study Questionnaire
2.3. Data Analyses
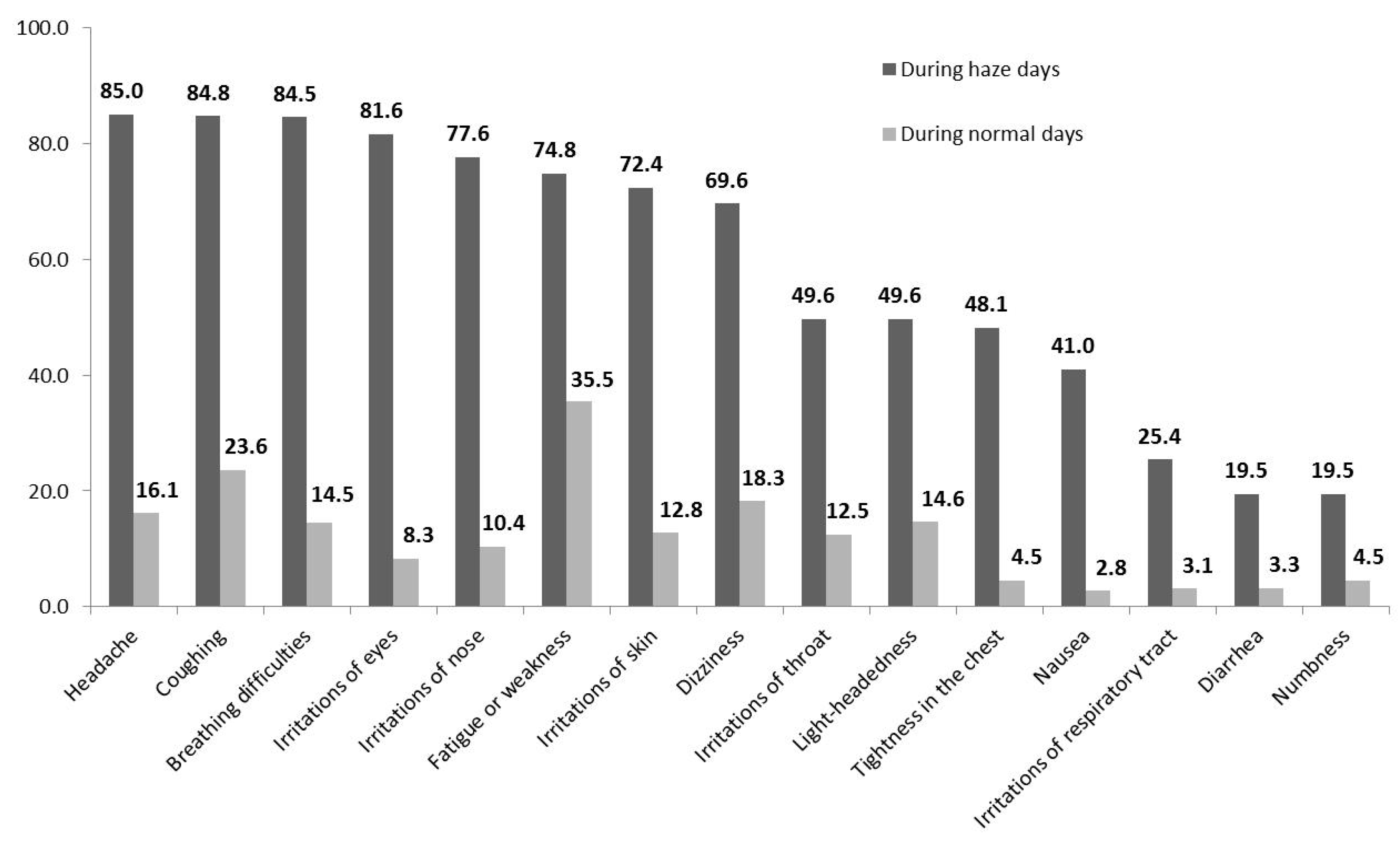
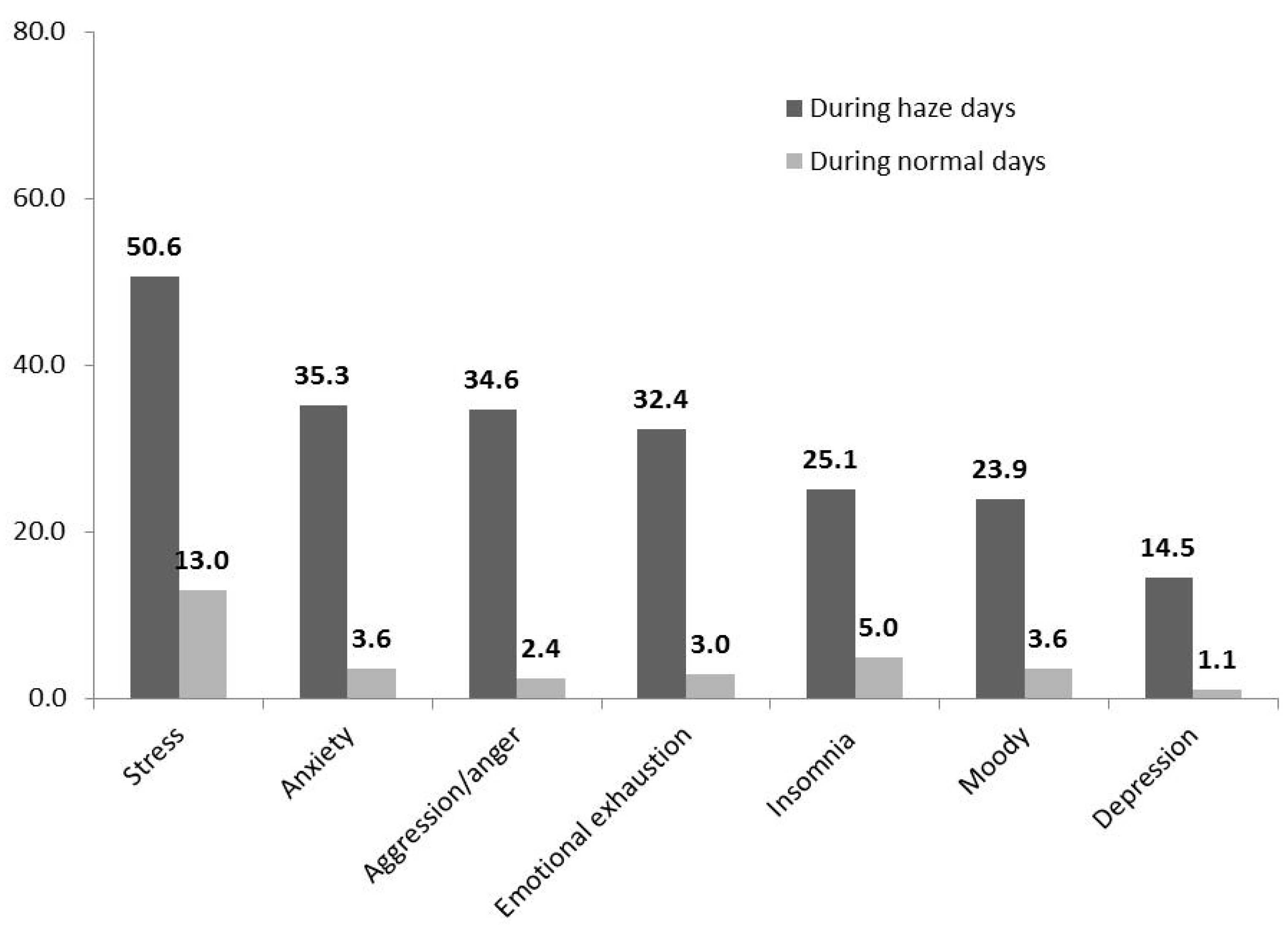
3. Results
4. Discussion
5. Conclusions
6. Limitation
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hoek, G.; Brunekreef, B.; Goldbohm, S.; Fischer, P.; van den Brandt, P.A. Association between mortality and indicators of traffic-related air pollution in the Netherlands: A cohort study. Lancet 2002, 360, 1203–1209. [Google Scholar] [CrossRef]
- Adar, S.D.; Davey, M.; Sullivan, J.R.; Compher, M.; Szpiro, A.; Liu, L.J. Predicting airborne particle levels aboard Washington State school buses. Atmos. Environ. 2008, 42, 7590–7599. [Google Scholar] [CrossRef] [PubMed]
- McCreanor, J.; Cullinan, P.; Nieuwenhuijsen, M.J.; Stewart-Evans, J.; Malliarou, E.; Jarup, L.; Harrington, R.; Svartengren, M.; Han, I.K.; Ohman-Strickland, P.; et al. Respiratory effects of exposure to diesel traffic in persons with asthma. N. Engl. J. Med. 2007, 357, 2348–2358. [Google Scholar] [CrossRef] [PubMed]
- Peters, A.; Von Klot, S.; Heier, M.; Trentinaglia, I.; Hörmann, A.; Wichmann, H.E.; Löwel, H. Exposure to traffic and the onset of myocardial infarction. N. Engl. J. Med. 2004, 351, 1721–1730. [Google Scholar] [CrossRef] [PubMed]
- Riediker, M.; Cascio, W.E.; Griggs, T.R.; Herbst, M.C.; Bromberg, P.A.; Neas, L.; Williams, R.W.; Devlin, R.B. Particulate matter exposure in cars is associated with cardiovascular effects in healthy young men. Am. J. Respir. Crit. Care Med. 2004, 169, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Strak, M.; Boogaard, H.; Meliefste, K.; Oldenwening, M.; Zuurbier, M.; Brunekreef, B.; Hoek, G. Respiratory health effects of ultrafine and fine particle exposure in cyclists. Occup. Environ. 2010, 67, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Shima, M.; Nitta, Y.; Adachi, M. Traffic-related air pollution and respiratory symptoms in children living along trunk roads in Chiba Prefecture, Japan. J. Epidemiol. 2003, 13, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Brauer, M.; Hoek, G.; Van Vliet, P.; Meliefste, K.; Fischer, P.H.; Wijga, A.; Koopman, L.P.; Neijens, H.J.; Gerritsen, J.; Kerkhof, M.; et al. Air pollution from traffic and the development of respiratory infections and asthmatic and allergic symptoms in children. Am. J. Respir. Crit. Care Med. 2002, 166, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Emmanuel, S.C. Impact to lung health of haze from forest fires: The Singapore experience. Respirology 2000, 5, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; Cohen, A.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef]
- Langrish, J.P.; Li, X.; Wang, S.; Lee, M.M.; Barnes, G.D.; Miller, M.R.; Cassee, F.R.; Boon, N.A.; Donaldson, K.; Li, J.; et al. Reducing personal exposure to particulate air pollution improves cardiovascular health in patients with coronary heart disease. Environ. Health Perspect. 2012, 120, 367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cai, D.P.; He, Y.M. Daily lifestyles in the fog and haze weather. J. Thorac. Dis. 2016, 8, E75–E77. [Google Scholar] [PubMed]
- Ren, J.; Li, B.; Yu, D.; Liu, J.; Ma, Z. Approaches to prevent the patients with chronic airway diseases from exacerbation in the haze weather. J. Thorac. Dis. 2016, 8, E1–E7. [Google Scholar] [PubMed]
- Leh, O.L.; Ahmad, S.; Aiyub, K.; Jani, Y.M.; Hwa, T.K. Urban air environmental health indicators for Kuala Lumpur city. Sains. Malays. 2012, 41, 179–191. [Google Scholar]
- Hartigan, J.A.; Wong, M.A. Algorithm AS 136: A k-means clustering algorithm. J. R. Stat. Soc. Ser. C (Appl. Stat.) 1979, 28, 100–108. [Google Scholar] [CrossRef]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: New York, NY, USA, 2013. [Google Scholar]
- Lobo, V.; Patil, A.; Phatak, A.; Chandra, N. Free radicals, antioxidants and functional foods: Impact on human health. Pharmacogn. Rev. 2010, 4, 118. [Google Scholar] [CrossRef] [PubMed]
- Laumbach, R.; Meng, Q.; Kipen, H. What can individuals do to reduce personal health risks from air pollution? J. Thorac. Dis. 2015, 7, 96–107. [Google Scholar] [PubMed]
- Ben-Shlomo, Y.; Smith, G.D.; Shipley, M.; Marmot, M.G. Magnitude and causes of mortality differences between married and unmarried men. J. Epidemiol. Comm. Health 1993, 47, 200–205. [Google Scholar] [CrossRef]
- Waldron, I.; Hughes, M.E.; Brooks, T.L. Marriage protection and marriage selection—Prospective evidence for reciprocal effects of marital status and health. Soc. Sci. Med. 1996, 43, 113–123. [Google Scholar] [CrossRef]
- Robards, J.; Evandrou, M.; Falkingham, J.; Vlachantoni, A. Marital status, health and mortality. Maturitas 2012, 73, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Deeks, A.; Lombard, C.; Michelmore, J.; Teede, H. The effects of gender and age on health related behaviors. BMC Public Health. 2009, 9, 213. [Google Scholar] [CrossRef] [PubMed]
- Davidson, D.J.; Freudenburg, W.R. Gender and environmental risk concerns: A review and analysis of available research. Environ. Behav. 1996, 28, 302–339. [Google Scholar] [CrossRef]
- Crouse, D.L.; Peters, P.A.; van Donkelaar, A.; Goldberg, M.S.; Villeneuve, P.J.; Brion, O.; Khan, S.; Atari, D.O.; Jerrett, M.; Pope, C.A., III; et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: A Canadian national-level cohort study. Environ. Health Perspect. 2012, 120, 708. [Google Scholar] [CrossRef] [PubMed]
- Gan, W.; Koehoorn, M.; Davies, H.; Demers, P.; Tamburic, L.; Brauer, M. Long-term exposure to traffic-related air pollution and the risk of coronary heart disease hospitalization and mortality. Epidemiology 2011, 22, S30. [Google Scholar] [CrossRef]
- Lepeule, J.; Laden, F.; Dockery, D.; Schwartz, J. Chronic exposure to fine particles and mortality: An extended follow-up of the Harvard Six Cities study from 1974 to 2009. Environ. Health Perspect. 2012, 120, 965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lipsett, M.J.; Ostro, B.D.; Reynolds, P.; Goldberg, D.; Hertz, A.; Jerrett, M.; Smith, D.F.; Garcia, C.; Chang, E.T.; Bernstein, L. Long-term exposure to air pollution and cardiorespiratory disease in the California teachers study cohort. Am. J. Respir. Crit. Care Med. 2011, 184, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Cesaroni, G.; Badaloni, C.; Gariazzo, C.; Stafoggia, M.; Sozzi, R.; Davoli, M.; Forastiere, F. Long-term exposure to urban air pollution and mortality in a cohort of more than a million adults in Rome. Environ. Health Perspect. (Online) 2013, 121, 324. [Google Scholar] [CrossRef] [PubMed]
- Brugge, D.; Durant, J.L.; Rioux, C. Near-highway pollutants in motor vehicle exhaust: A review of epidemiologic evidence of cardiac and pulmonary health risks. Environ. Health 2007, 6, 23. [Google Scholar] [CrossRef] [PubMed]
- Lercher, P.; Schmitzberger, R.; Kofler, W. Perceived traffic air pollution, associated behavior and health in an alpine area. Sci. Total Environ. 1995, 169, 71–74. [Google Scholar] [CrossRef]
- Zuurbier, M.; Hoek, G.; Oldenwening, M.; Meliefste, K.; van den Hazel, P.; Brunekreef, B. Respiratory effects of commuters' exposure to air pollution in traffic. Epidemiology 2011, 22, 219–227. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice: Summary Report; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Lundberg, A. Psychiatric aspects of air pollution. Otolaryngol. Head Neck Surg. 1996, 114, 227–231. [Google Scholar] [CrossRef]
- Genc, S.; Zadeoglulari, Z.; Fuss, S.H.; Genc, K. The adverse effects of air pollution on the nervous system. J. Toxicol. 2012. [Google Scholar] [CrossRef] [PubMed]
- Power, M.C.; Kioumourtzoglou, M.A.; Hart, J.E.; Okereke, O.I.; Laden, F.; Weisskopf, M.G. The relation between past exposure to fine particulate air pollution and prevalent anxiety: observational cohort study. BMJ 2015, 350, h1111. [Google Scholar] [CrossRef] [PubMed]
- Vijayan, V.K.; Paramesh, H.; Salvi, S.S.; Dalal, A.A. Enhancing indoor air quality—The air filter advantage. Lung India 2015, 32, 473. [Google Scholar] [CrossRef] [PubMed]
- Claudio, L. Planting healthier indoor air. Environ. Health Perspect. 2011, 119, a426–427. [Google Scholar] [CrossRef] [PubMed]
- Manigrasso, M.; Natale, C.; Vitali, M.; Protano, C.; Avino, P. Pedestrians in Traffic Environments: Ultrafine Particle Respiratory Doses. Int. J. Environ. Res. Public Health. 2017, 14, E288. [Google Scholar] [CrossRef] [PubMed]
| Details | Frequency, n (%) |
|---|---|
| (A) Socio-demographic data | |
| Age group (years old) | |
| 30 and below | 452 (56.5) |
| 31–40 | 265 (33.1) |
| >40 | 83 (10.4) |
| Gender | |
| Male | 424 (53.0) |
| Female | 376 (47.0) |
| Marital status | |
| Single | 414 (51.8) |
| Married | 386 (48.3) |
| Ethnicity | |
| Malay | 388 (48.5) |
| Chinese | 271 (33.9) |
| Indian | 138 (17.3) |
| Others | 3 (0.4) |
| Education | |
| Secondary level and below | 146 (18.2) |
| Tertiary level | 654 (81.8) |
| Occupation | |
| Professional/managerial | 419 (52.4) |
| Skilled/non-skilled worker | 314 (40.6) |
| Student | 54 (6.8) |
| Housewife | 2 (0.2) |
| Monthly income (MYR) | |
| 5000 and below | 651 (81.4) |
| >5000 | 149 (18.6) |
| (B) Other exposure risks | |
| Chronic diseases | |
| Yes | 51 (6.4) |
| No | 749 (93.6) |
| Smoking status | |
| Yes | 309 (38.6) |
| No | 491 (61.4) |
| Living near highway | |
| Yes | 292 (36.5) |
| No | 508 (63.5) |
| Duration spent commuting by public transport (hours) | |
| 1 h and below | 472 (59.0) |
| >1 h | 328 (41.0) |
| During Daily Commute | During Haze Days | |||
|---|---|---|---|---|
| Never/Rarely n (%) | Sometimes/Often n (%) | Never/Rarely n (%) | Sometimes/Often n (%) | |
| Use normal surgical mask | 597 (74.6) | 203 (25.4) | 63 (7.9) | 737 (92.1) |
| Use dust masks N95 during severe haze day | 703 (87.9) | 97 (12.1) | 272 (34.0) | 528 (66.0) |
| Drink more water | 175 (21.9) | 625 (78.1) | 7 (0.9) | 793 (99.1) |
| Increase the intake of fresh fruits or vegetables | 327 (40.9) | 473 (59.1) | 65 (8.1) | 735 (91.9) |
| Take food supplements (vitamins, nutrients, herbal products) | 481 (60.1) | 319 (39.9) | 254 (31.8) | 546 (68.2) |
| As much as possible commute using alternative transportation (e.g., friends car) to avoid exposure | 450 (56.3) | 350 (43.8) | 316 (39.5) | 484 (60.5) |
| Total Control Measure Score | |||||||
|---|---|---|---|---|---|---|---|
| During Daily Commute | During Haze Days | ||||||
| Total | Cluster I 0–8 (n = 440) | Cluster II 9–18 (n = 360) | p-Value | Cluster I 0–11 (n = 154) | Cluster II 12–18 (n = 646) | p-Value | |
| (A) SOCIO-DEMOGRAPHIC DATA | |||||||
| Age group (years old) | |||||||
| 30 and below | 452 (56.5) | 244 (54.0) | 208 (46.0) | 100 (22.1) | 352 (77.9) | ||
| 31–40 | 265 (33.1) | 147 (55.5) | 118 (44.5) | 0.684 | 39 (14.7) | 226 (85.3) | 0.050 |
| >40 | 83 (10.4) | 49 (59.0) | 34 (41.0) | 15 (18.1) | 68 (81.9) | ||
| Gender | |||||||
| Male | 424 (53.0) | 233 (55.0) | 191 (45.0) | 1.000 | 82 (19.3) | 342 (80.7) | 1.000 |
| Female | 376(47.0) | 207 (55.1) | 169 (44.9) | 72 (19.1) | 304 (80.9) | ||
| Marital status | |||||||
| Single | 414 (51.8) | 235 (56.8) | 179 (43.2) | 0.320 | 92 (22.2) | 322 (77.8) | 0.031 |
| Married | 386 (48.3) | 205 (53.1) | 181 (46.9) | 62 (16.1) | 324 (83.9) | ||
| Ethnicity | |||||||
| Malay | 388 (48.5) | 212 (54.6) | 176 (45.4) | 81 (20.9) | 307 (79.1) | ||
| Chinese | 271 (33.9) | 143 (52.8) | 128 (47.2) | 0.383 | 52 (19.2) | 219 (80.8) | 0.053 |
| Indian | 138 (17.3) | 84 (60.9) | 54 (39.1) | 19 (13.8) | 119 (86.2) | ||
| Others | 3 (0.4) | 1 (33.3) | 2 (66.7) | 2 (66.7) | 1 (33.3) | ||
| Highest education level | |||||||
| Secondary level and below | 146 (18.2) | 88 (60.3) | 58 (39.7) | 0.168 | 28 (19.2) | 118 (80.8) | 1.000 |
| Tertiary level | 654 (81.8) | 352 (53.8) | 302 (46.2) | 126 (19.3) | 528 (80.7) | ||
| Occupation | |||||||
| Professional/managerial | 419 (52.4) | 224 (53.5) | 195 (46.5) | 87 (20.8) | 332 (79.2) | ||
| Skilled/non-skilled worker | 314 (40.6) | 184 (56.6) | 141 (43.4) | 0.310 | 55 (16.9) | 270 (83.1) | 0.469 |
| Student | 54 (6.8) | 32 (59.3) | 22 (40.7) | 12 (22.2) | 42 (77.8) | ||
| Housewife | 2 (0.2) | 0 (100.0) | 2 (100.0) | 0 (0.0) | 2 (100.0) | ||
| Monthly income (MYR) | |||||||
| 5000 and below | 651 (81.4) | 359 (55.1) | 292 (44.9) | 125 (19.2) | 526 (80.8) | ||
| >5000 | 149 (18.6) | 81 (54.4) | 68 (45.6) | 0.927 | 29 (19.5) | 120 (80.5) | 0.909 |
| (B) OTHER RISKS | |||||||
| Chronic diseases | |||||||
| Yes | 51 (6.4) | 25 (49.0) | 26 (51.0) | 0.386 | 10 (19.6) | 41 (80.4) | 1.000 |
| No | 749 (93.6) | 415 (55.4) | 334 (44.6) | 144 (19.2) | 605 (80.8) | ||
| Smoking status | |||||||
| Yes | 309 (38.6) | 184 (59.5) | 125 (40.5) | 0.041 | 56 (18.1) | 253 (81.9) | 0.581 |
| No | 491 (61.4) | 256 (52.1) | 235 (47.9) | 98 (20.0) | 393 (80.0) | ||
| Living near highway | |||||||
| Yes | 292 (36.5) | 159 (54.5) | 133 (45.5) | 0.825 | 67 (22.9) | 225 (77.1) | 0.050 |
| No | 508 (63.5) | 281 (55.3) | 227 (44.7) | 87 (17.1) | 421 (82.9) | ||
| Duration spent commuting by public transport (hours) | |||||||
| 1 h and below | 472 (59.0) | 258 (54.7) | 214 (45.3) | 0.829 | 98 (20.8) | 374 (79.2) | 0.203 |
| >1 h | 328 (41.0) | 182 (55.5) | 146 (44.5) | 56 (17.1) | 272 (82.9) | ||
| Total Physical and Psychological Health Experience Score | ||||||||
|---|---|---|---|---|---|---|---|---|
| During Daily Commute Days | During Haze Days | |||||||
| Cluster I 0–4 (n = 684) | Cluster II 5–22 (n = 116) | p-Value | Cluster I 0–11 (n = 434) | Cluster II 12–22 (n = 366) | p-Value | Multiple Logistic Regression for 12–22 vs. 0–11 ¥ | ||
| (A) SOCIO-DEMOGRAPHIC DATA | ||||||||
| Age group (years old) | ||||||||
| 30 and below | 452 (56.5) | 387 (85.6) | 65 (14.4) | 248 (54.9) | 204 (45.1) | 1.580 (0.967–2.583) | ||
| 31–40 | 265(33.1) | 230 (86.8) | 35 (13.2) | 0.389 | 132 (49.8) | 133 (50.2) | 0.048 | 1.852 (1.107–3.099) * |
| >40 | 83(10.4) | 67 (80.7) | 16 (19.3) | 54 (65.1) | 29 (34.9) | Reference | ||
| Gender | ||||||||
| Male | 424 (53.0) | 370 (87.3) | 54 (12.7) | 0.159 | 288 (53.8) | 196 (46.2) | 0.777 | |
| Female | 376(47.0) | 314 (83.5) | 62 (16.5) | 206 (54.8) | 170 (45.2) | |||
| Marital status | ||||||||
| Single | 414 (51.8) | 356 (86.0) | 58 (14.0) | 0.689 | 234 (56.5) | 180 (43.5) | 0.201 | |
| Married | 386 (48.3) | 328 (85.0) | 58 (15.0) | 200 (51.8) | 186 (48.2) | |||
| Ethnicity | ||||||||
| Malay | 388 (48.5) | 332 (85.6) | 56 (14.4) | 206 (53.1) | 182 (46.9) | |||
| Chinese | 271 (33.9) | 235 (86.7) | 36 (13.3) | 0.636 | 151 (55.7) | 120 (44.3) | 0.798 | |
| Indian | 138 (17.3) | 115 (83.3) | 23 (16.7) | 76 (55.1) | 62 (44.9) | |||
| Others | 3 (0.4) | 2 (66.7) | 1 (33.3) | 1 (33.3) | 2 (66.7) | |||
| Highest education level | ||||||||
| Secondary level and below | 146 (18.2) | 124 (84.9) | 22 (15.1) | 0.796 | 78 (53.4) | 68 (46.6) | 0.854 | |
| Tertiary level | 654 (81.8) | 560 (85.6) | 94 (14.4) | 356 (54.4) | 298 (45.6) | |||
| Occupation | ||||||||
| Professional and managerial | 419 (52.4) | 358 (85.4) | 61 (14.6) | 216 (51.6) | 203 (48.4) | |||
| Skilled/non-skilled worker | 314 (40.6) | 278 (85.5) | 47 (14.5) | 0.951 | 186 (57.2) | 139 (42.8) | 0.249 | |
| Student | 54 (6.8) | 46 (85.2) | 8 (14.8) | 30 (55.6) | 24 (44.4) | |||
| Housewife | 2 (0.2) | 2 (100.0) | 0 (0.0) | 2 (100.0) | 0 (0.0) | |||
| Monthly income (MYR) | ||||||||
| 5000 and below | 651 (81.4) | 559 (85.9) | 36 (14.1) | 143 (56.1) | 112 (43.9) | |||
| >5000 | 149 (18.6) | 125 (83.9) | 56 (14.1) | 0.826 | 205 (51.8) | 191 (48.2) | 0.359 | |
| (B) OTHER RISKS | ||||||||
| Chronic diseases | ||||||||
| Yes | 51 (6.4) | 40 (78.4) | 92 (14.1) | 0.521 | 348 (53.5) | 303 (46.5) | 0.363 | |
| No | 749 (93.6) | 644 (86.0) | 24 (16.1) | 86 (57.7) | 63 (42.3) | |||
| Smoking status | ||||||||
| Yes | 309 (38.6) | 266 (86.1) | 43 (13.9) | 0.758 | 164 (53.1) | 145 (46.9) | 0.610 | |
| No | 491 (61.4) | 418 (85.1) | 73 (14.9) | 270 (55.0) | 221 (45.0) | |||
| Living near highway | ||||||||
| Yes | 292 (36.5) | 255 (87.3) | 37 (12.7) | 0.297 | 145 (49.7) | 147 (50.3) | 0.055 | |
| No | 508 (63.5) | 429 (84.4) | 79 (15.6) | 289 (56.9) | 219 (43.1) | |||
| Duration spent commuting by public transport (hours) | ||||||||
| 1 h and below | 472 (59.0) | 412 (87.3) | 60 (12.7) | 0.102 | 252 (53.4) | 220 (46.6) | 0.565 | |
| >1 h | 328 (41.0) | 272 (82.9) | 56 (17.1) | 182 (55.5) | 146 (44.5) | |||
| (C) CONTROL MEASURES | ||||||||
| DURING DAILY COMMUTE DAYS | ||||||||
| Total control measure score | ||||||||
| Cluster I (0–8) | 440 (55.0) | 371 (84.3) | 69 (15.7) | 0.314 | ||||
| Cluster II (9–18) | 360 (45.0) | 313 (86.9) | 47 (13.1) | |||||
| DURING HAZE DAYS | ||||||||
| Total control measure score | ||||||||
| Cluster I (0–11) | 103 (66.9) | 51 (33.1) | 0.000 | Reference | ||||
| Cluster II (12–18) | 331 (51.2) | 315 (48.8) | 1.907 (1.315–2.765) ** | |||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, L.P.; Alias, H.; Aghamohammadi, N.; Ghadimi, A.; Sulaiman, N.M.N. Control Measures and Health Effects of Air Pollution: A Survey among Public Transportation Commuters in Malaysia. Sustainability 2017, 9, 1616. https://doi.org/10.3390/su9091616
Wong LP, Alias H, Aghamohammadi N, Ghadimi A, Sulaiman NMN. Control Measures and Health Effects of Air Pollution: A Survey among Public Transportation Commuters in Malaysia. Sustainability. 2017; 9(9):1616. https://doi.org/10.3390/su9091616
Chicago/Turabian StyleWong, Li Ping, Haridah Alias, Nasrin Aghamohammadi, Azadeh Ghadimi, and Nik Meriam Nik Sulaiman. 2017. "Control Measures and Health Effects of Air Pollution: A Survey among Public Transportation Commuters in Malaysia" Sustainability 9, no. 9: 1616. https://doi.org/10.3390/su9091616






