1. Introduction
The growth of resistance to remedies against infections is one of the world’s utmost challenges. In fact, antimicrobial resistance is estimated by the World Health Organization to already cause more than 700,000 yearly deaths from infections with resistant microbes and the number will increase dramatically in the future, if this problem is left unchecked. The unsustainable behavior of human overconsumption has been identified as a major driver of this growth [
1,
2,
3].
Limiting antibiotic resistance is a matter of sustainable development because today’s overconsumption of antibiotics compromises the ability of future generations to treat bacterial infections. However, already, antibiotic resistance dampens the potential to attain several of the United Nations’ Sustainable Development Goals (SDGs). The goals to end poverty, ensure food security, ensure access to water and sanitation, install sustainable economic growth as well as sustainable consumption and production are all likely to be impaired by the presence of untreatable infections [
4,
5].
However, like many other sustainability issues, promoting prudent human use of antibiotics has the ingredients of a collective action problem. Despite the fact that overconsumption breeds resistance, there are very limited incentives for patients or health-care providers to consider the effect of their decision about antibiotic use on the overall levels of resistance [
6,
7,
8].
This paper builds on lessons drawn from the study of other sustainability collective action dilemmas. In particular, we hypothesize that interpersonal trust, known to promote collective action in relation to climate change, fisheries and water management, also makes individuals more willing to cooperate to fight antibiotic resistance by limiting their own use of antibiotics. The aim of this article is to further our understanding of people’s antibiotic consumption by investigating if individuals’ willingness to voluntarily abstain from antibiotic use is linked to interpersonal trust.
To fulfill the aim, we implement two separate empirical investigations. In the first part, we use cross-section survey data to investigate the link between interpersonal trust—the belief that most people can be trusted—and willingness to abstain from using antibiotics. The second part is based on a between-subject survey experiment where we study the role of interpersonal trust indirectly by experimentally manipulating the trustworthiness of other people. As such, we study the causal contribution of public willingness to limit antibiotic use on respondents’ own willingness to limit their use of antibiotics.
The results from the analysis of the cross-section data show that interpersonal trust is linked to willingness to limit antibiotic use, also when controlling for potential confounders. The survey experiment demonstrates that the general willingness to abstain from using antibiotics among the general public—our indicator of trustworthiness—stimulates individuals to abstain from using antibiotics themselves. In doing so, this study contributes to the understanding of the role of interpersonal trust for individual voluntary behavior in large-scale collective action dilemmas, such as antibiotic use. In addition, the paper shows that insights from other sustainability issues may also be useful when it comes to the struggle to limit unsustainable use of antibiotics.
The structure of the paper is as follows:
Section 2 depicts previous research on antibiotics use and resistance, and we argue that when it comes to antibiotic overuse, more attention should be paid to the behavior of patients. In
Section 3 we build on findings from other sustainability issues, account for the theoretical model of collective action and present the hypotheses about the link between trust and collective action to limit antibiotic use.
Section 4 is dedicated to methods and materials, where the case of Sweden and subsequently the survey and survey experiment methods are presented.
Section 5 reports the results from the survey and the survey experiment. Lastly,
Section 6 is a concluding discussion on voluntary cooperation and proposes future studies and upcoming proposals for examining and attaining behavioral change.
2. Previous Research
Apart from variation in antibiotics use linked to different types of infections, there is also a variation related to non-medical factors [
9]. For example, in a study by Bjerrum et al. [
10] it was discovered that national differences in prescription rates do not tend to mirror the prevalence of bacterial infections, but are related to national recommendations, treatment traditions and pharmaceutical marketing. Other contextual factors found to be important in the previous literature are type of health-care system [
9], corruption [
11,
12] and a number of cultural factors [
13,
14], for example, risk aversion [
15,
16].
Antibiotic use also varies by individual factors, such as knowledge [
17], gender [
18], education [
17,
19], age [
20], trust in institutions [
6] and interpersonal trust [
6,
21].
Around the world, initiatives are now taken to ensure that antibiotics are only attainable through prescription, in addition to various attempts to limit the amount of prescribed antibiotics. These efforts have been directed towards medical practitioners (e.g., by creating guidelines), which in many countries has had the intended effect of lowering overall consumption. A prominent example here is that medical practitioners can be educated in order to diminish the prescription rates [
22]. This is the case for Sweden, which has managed to diminish the use of antibiotics, even if overconsumption still is a problem [
23,
24].
While much attention has been directed towards changing the behavior of prescribers, relatively little attention has been given to the behavior of patients. This is of interest since previous studies have shown that medical practitioners are confronted with demands for antibiotics from patients [
25,
26,
27,
28]. Time restrictions and high demand from patients jointly influence prescribers to prescribe antibiotics, even in cases where this might not be necessary in order to treat the infection. In a study in the UK, it was found that about 96% of all patients who request antibiotics also receive it, indicating that antibiotic consumption might involve a
shared decision-making between doctors and patients [
25].
This has led scholars to argue that in order to reduce prescription rates, programs intended to change behavior must be put in place for patients, which is crucial in the struggle to promote sustainable antibiotic use [
29]. The importance of the patient perspective is further underscored by recent increases in awareness campaigns in Europe, intended to inform patients about when antibiotics are redundant [
15].
However, it is known from many other sustainability issues that an understanding of the salience of the issue is a necessary, yet insufficient, condition for cooperation to occur. In solving sustainability issues such as climate change, fisheries management and clean water, trust is a key component in creating behavioral change towards sustainable use of resources. The more people believe that others will cooperate, the more likely that they will adopt cooperative behavior [
30,
31].
Interestingly, in a study by Blommaert, Marais, Hens, Coenen, Muller, Goossens and Beutels [
21], the authors also discovered a relationship between country levels of interpersonal trust and levels of antibiotics use. This study was reinforced by individual-level evidence in a study by Rönnerstrand and Andersson Sundell [
6], who found a link between interpersonal trust and the willingness to postpone antibiotic treatment.
The aim of this article is to further our understanding of people’s antibiotic consumption by investigating if individuals’ willingness to voluntarily abstain from antibiotic use is linked to interpersonal trust.
Many other sustainability issues—such as fisheries management, climate change and access to clean water—are examples of collective action problems. The next section describes why antibiotic resistance can also be understood as such a challenge, and, based on theory and previous research, hypothesize a link between interpersonal trust and willingness to limit personal use of antibiotics.
3. Theoretical Framework and Hypotheses
A collective action problem typically occurs when a group of people share a resource but where the gain for each individual is highest if he or she disregards the group benefit and acts in self-interest, no matter what other group members do. This is valid, while the profit for everyone is nonetheless higher if all were to cooperate, since the joint resource will otherwise gradually be impoverished or depleted [
32]. Simultaneously, if a person understands the potential negative outcome, and thus chooses to cooperate (i.e., reduce his or her resource usage), he or she may easily end up in a position of a “sucker” [
33]. That means that the person is losing twofold: not receiving the individual profit and also suffering from the collective damage.
With the example of antibiotics, the key driver of resistance is overuse, but there are limited incentives for each patient or health-care provider to consider the overall consequences of antibiotic use [
7,
8]. Over time, overconsumption or lack of cooperation can turn into a tragedy of the commons, where the resource is depleted, or in the case of antibiotic resistance, when the healing properties of antibiotics are exhausted. To illustrate, it is often perceived as a sacrifice both by the patient and the treating doctor not to rely on antibiotics when the patient has an infection, even when there is no or weak evidence that such treatment would in fact cure the infection. The benefits of such a sacrifice are, on the other hand, dispersed and remote.
When it comes to resource collective action dilemmas in general, the level of worry that individuals experience and/or express is connected to whether these individuals are willing to act in favor of group concerns and resources, or not [
34,
35,
36]. Furthermore, the main focus of this paper is that we know that interpersonal trust is positively related to cooperation in collective action dilemmas [
37]. For example, there is a well-studied relationship between interpersonal trust and cooperation in small-scale dilemmas involving a limited number of actors [
31,
38,
39,
40,
41]. However, we know less about if and how interpersonal trust works in relation to cooperation in large-scale dilemmas, such as antibiotics use.
In fact, there are several differences between small-scale and large-scale collective action situations. Importantly, Olson’s argument is that—without an external enforcer—collective action in small groups may come about but is destined to fail in large groups. In a small group setting, social pressure and the quest for reputation and social prestige may stimulate cooperation, as long as members of the group can interact face-to-face. In large groups, Olson argues, collective action is impossible without external enforcement [
42].
However, despite Olson’s prediction, a few studies have found that interpersonal trust may also stimulate voluntary cooperation also in a large-scale setting [
43,
44,
45]. Based upon findings from the study of collective action dilemmas, we theorize that interpersonal trust is crucial for people’s propensity to cooperate to fight antibiotic resistance by limiting their own use of antibiotics. Hypothetically, people who have higher levels of interpersonal trust (the belief that most people can be trusted), will be more willing to decrease their own use of antibiotics.
Hypothesis 1 (H1). Higher levels of interpersonal trust are positively correlated with a higher propensity to take voluntary action to decrease one’s own use of antibiotics.
Previous studies of collective action show that trustworthy behavior of others elicits pro-social behavior in other collective action problems [
30,
31]. People who trust that peers will contribute or cooperate are more compelled to cooperate themselves [
30,
46,
47,
48]. However, this can also have the opposite effect, if it is believed that others are not acting pro-socially [
49]. Based on these findings, a second hypothesis concerns whether people who receive information about the trustworthiness of other people (i.e., there is a high willingness among others to limit their own antibiotic use) will have a higher propensity to abstain from using antibiotics:
Hypothesis 2 (H2). Higher belief in the trustworthiness of others has a positive effect on the propensity to take voluntary action to decrease one’s own use of antibiotics.
4. Materials and Methods
In order to test our two hypotheses, the study is separated into two parts. Making use of cross-section survey data, the first part examines the link between interpersonal trust and individual willingness to limit antibiotic use. The second part utilizes a survey experimental approach to allow for causal inference and to study the causal contribution of the proclaimed trustworthiness of other people on individuals’ willingness to limit antibiotic use.
By combining both survey data and survey experiment, we utilize the major strengths of the two methods: compensating external validity with survey data and addressing causality through the survey experiment [
50]. Furthermore, this combination also makes it possible to control for common confounders of trust and trustworthiness. [
51].
The choice of Sweden as the case was motivated by the fact that Sweden has among the highest levels of interpersonal trust in the world [
52,
53]. This is thus a so-called
tough test for our theory, because interpersonal trust will likely have a stronger relationship with cooperative behavior either by the lower the general levels of trust and/or the larger the relative differences in levels of trust. This means that if we even find support for the relationship between interpersonal trust and cooperation in Sweden, where the general level of interpersonal trust is high and the relative differences among individuals is presumably rather low, then this connection is likely to be even stronger in other countries where the level of interpersonal trust is generally lower.
Another reason for the focus on Sweden is that knowledge about antibiotic treatment and antibiotic resistance is high in this country [
15,
54]. This means that in the experiment, extensive information on the issue did not have to be provided for the experiment to materialize successfully, but was instead assumed to be endogenous.
4.1. Design of the Cross-Section Survey Study
To test our first hypothesis, we used an annual survey conducted by the Society, Opinion and Media Institute (the SOM Institute) at the University of Gothenburg. This survey captures both our main independent and dependent variables, including many other variables associated with antibiotic consumption. The survey is well established in Sweden and is based on a probability sample of the Swedish population, drawn from the public register. The sample was slightly skewed towards more educated and male participants, which motivated us to systematically control for level of education and gender in our studies. The total number of respondents in the SOM survey was 9828. However, all respondents were not asked all questions, and 3400 is the number of people who were invited to answer questions about antibiotics, thus, the number of survey respondents who answered all the questions required to be included in the analysis was 1293. The AAPOR response rate was 47%.
The question that is the dependent variable was “to what extent would you say that you are willing to abstain from using antibiotics, even if you risk additional sick days?” The four options are 1 = would certainly not abstain, 2 = would not abstain, 3 = would abstain and 4 = would certainly abstain. A majority of the respondents answered that they are willing to abstain from using antibiotics and hence this variable was skewed. We argue that the group that would certainly abstain from using antibiotics is more likely to behave this way than all others and we therefore dichotomized the four response alternatives into 1 = would certainly abstain and 0 = all other groups.
Since the dependent variable was dichotomous, a binary logistic regression, and more specifically, an odds ratio, was used [
55]. We did this in order to assess whether higher levels of interpersonal trust are associated with a higher propensity to abstain from using antibiotics.
There are several factors that can potentially affect the relationship between interpersonal trust and willingness to abstain from using antibiotics. The first is
age, since older patients have been found to consume more antibiotics [
20], while this group also tends to report higher levels of interpersonal trust [
56,
57]. A second aspect is that
gender has been related to cooperation in some collective action dilemmas [
58], while women consume more antibiotics [
18]. Furthermore,
subjective health is linked to higher levels of interpersonal trust [
59], and positive health decisions [
60], while people with higher stated well-being are more willing to wait to consume antibiotics [
6]. Lastly,
education can influence the focal relationship through higher levels of education being associated with more knowledge on appropriate use [
17,
19], while people who are more educated also tend to be more worried about the growth of resistance [
6]. Controlling for education is also important since it could be related to levels of interpersonal trust [
61].
4.2. Design of the Survey Experiment
For the survey experiment, we make use of a web survey called The Citizen Panel, accessible through the Laboratory of Opinion Research at the University of Gothenburg, where 5000 participants in the panel received the survey and 3605 responded, resulting in a participation rate of 72.1%. The recruitment of participants in the Citizen Panel is mostly comprised of self-selection yet some are recruited using random probability sampling [
62].
We manipulate the mechanism hypothesized to be the link between interpersonal trust and cooperation, that is, the belief about the trustworthiness of others. Group means are assumed to be equal and this null hypothesis is rejected if differences are larger than would be expected to occur in repeated trials on a 95% confidence level. ANOVA is used to compare group means and a post-hoc test, Tukey’s HSD, is used to discern if and which group means are different from one another. The effect size of the manipulation is measured in eta squared.
A between-subject design is used and respondents are randomly assigned to one out of four treatment groups and receive a vignette with a hypothetical scenario. In
Table 1 the information given to the different groups is displayed. Groups 1 and 2 are the main experiment groups who receive information on the cooperation of others (see
Appendix A for vignettes). Group 1 receives information that 80% of people with a similar infection and situation tend to cooperate and choose to abstain from using antibiotics whereas Group 2 receives information that only 20% tend to cooperate. Both groups receive information on the salience of the issue, such as the problem of growing resistance dampening the effectiveness of modern medicine (e.g., in treating severe infections) [
5]. They also receive information that a physician has prescribed antibiotics and that it is not always necessary to consume antibiotics to treat this illness. Lastly, Groups 1 and 2 are told to imagine that they have a minor infection and are asked how likely they are to abstain from using antibiotics, even if they risk additional sick days. Group 3 is then installed to disentangle if there is an independent effect of the said cooperation of others on the cooperativeness that does not depend on the salience of the issue. Group 4 is a pure control group that only receives the question about their willingness to abstain from using antibiotics. Control variables are used to ensure random selection to the treatment groups (see
Supplementary Materials for proof of random selection).
The dependent variable is measured through the question “Imagine that you have a respiratory tract infection. How likely are you to abstain from using antibiotics, even if you risk additional sick days?” The options are numbered from 1 to 5 where 1 = not at all likely, 2 = not likely, 3 = neither likely nor unlikely, 4 = likely and 5 = very likely.
4.3. Ethics
Those responsible for the SOM survey and the Citizen Panel at the University of Gothenburg conducted internal ethical reviews of the protocols before the studies were approved and underway. The participants of the survey experiment were informed that the vignettes were hypothetical.
5. Results
5.1. Results from the Analysis of Cross-Section Data
A logistic regression model is created to analyze the relationship between interpersonal trust and stated willingness to abstain from using antibiotics. The results from the logistic regression models are presented in
Table 2. Model 1 is a significant improvement from Model 0 to estimate the odds of a respondent being willing to abstain from antibiotics. Interpersonal trust is a significant predictor of odds to abstain from using antibiotics on a
p-level = 0.01. This is interpreted as for each increase in level of interpersonal trust the odds of abstaining from using antibiotics increases with 11%.
In Model 2, potential confounders and control variables are introduced. These are how worried people are for increasing antibiotic resistance in the future, the number of antibiotic courses people have taken in the last year and a measure of self-estimated health. We expect that higher values of worry, consumption and health are correlated with an increased propensity to limit one’s consumption of antibiotics. When these variables are added, the individual contribution of interpersonal trust still remains, where the odds of certainly wanting to abstain from taking antibiotics increases by 8% for every one-step increase in interpersonal trust on the p-level = 0.01. In general, the added variables follow the prediction, a person who consumes the highest number of antibiotics courses has lower odds to answer that they most certainly would abstain from using antibiotics (p = 0.1). The group that only consumed one course of antibiotics has higher odds to abstain from using antibiotics than any other category (p = 0.01). These results are curved and indicate that the number of antibiotics courses does not contribute a lot to explaining abstention decisions. Worry about increased resistance in the future sometimes contributes to explain abstention decisions. For example, if you are not worried at all, you have lower odds of abstaining from using antibiotics and are significantly different than other categories. The group that is most worried is four times more likely to abstain from using antibiotics than the other categories. However, only the lowest and highest levels of worry are statistically significant. Higher levels of self-estimated health increase the odds of certainly abstaining from using antibiotics. A one-step increase in self-estimated health results in 43% increased odds of certainly abstaining from using antibiotics. Most of the model fit estimates show an increase in model fit, however not all of them, indicating that Model 2 only offers a slightly better prediction of abstention decisions.
In Model 3, level of education and institutional trust are added to the model. We expect that higher levels of institutional trust and education are linked to a higher likelihood of abstaining from using antibiotics. This holds true for education since respondents with the highest level of education have almost two and a half times higher odds of abstaining from using antibiotics. Interestingly, institutional trust does not explain any of the variation in likelihood to abstain from using antibiotics. When these variables are introduced, the relationship between interpersonal trust and willingness to certainly abstain from using antibiotics diminishes (from Exp(B) = 1.08 to Exp(B) = 1.06). While education contributes most to explaining abstemiousness, interpersonal trust remains significant on the p-level = 0.05. The individual relationship between self-estimated health and antibiotics use on the willingness to abstain from using antibiotics diminish when education and institutional trust are in the model. All model fit estimates indicate a model improvement when education and institutional trust are introduced.
In Model 4, age and gender are added as explanatory variables of abstemiousness. Women are 6% less likely than men to abstain from using antibiotics, yet this difference is not statistically significant. The oldest age category is 36% less likely to abstain from using antibiotics (p-level = 0.05). The two oldest age groups are less likely to abstain from using antibiotics than the youngest groups, however, not all of these differences are significant. When age and gender are added to the model, the individual contribution from the independent variable interpersonal trust remains at 6% and is still significant on the p-level = 0.05. Education continues to have an individual contribution. Level of worry contributes to predict the outcome in the lowest and highest categories. Self-estimated health does not contribute to explain the outcome in Model 4 on the p-level = 0.1. Lastly, only the most frequent users of antibiotics predict the outcome on the p-level = 0.05.
Model 4 has a lower—2 Log Likelihood (−2 LL) and a high, as well as significant, model chi2 indicating a better model fit compared to the other models. Nagelkerke’s R2 has increased while the Hosmer and Lemeshow statistic remains insignificant, which indicates a good fit. While the number of correct classifications remain at 63.9%, we argue that this model best explains the variation in the data.
5.2. Results from the Analysis of Survey Experimental Data
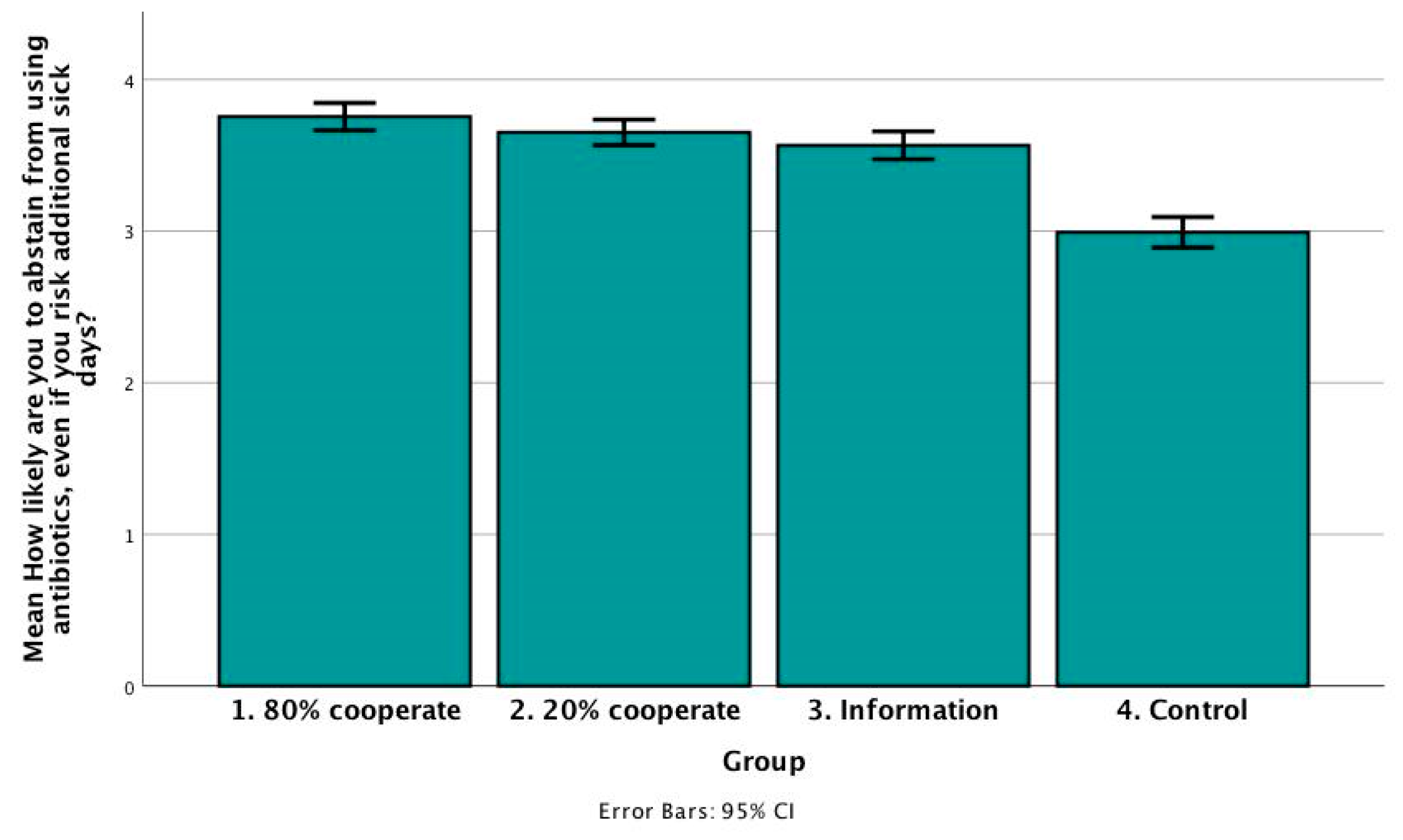
To attain causality of our findings, we conducted a survey experiment. First, we perform an ANOVA (between group Sum of Squares = 313.54, F = 52.87, df = 3, p = 0.00), where at least one experiment group is found to have a significantly different mean than other experiment groups (within groups SSQ = 7135.77, df = 3610).
Figure 1 presents the group means. As in the logistic regression model, Swedes have a generally high level of cooperation. The groups do not seem to have significantly different group means since some of the confidence intervals overlap. Group 1 estimated the likelihood to abstain from using antibiotics to a mean of 3.75 (
N = 885, std. dev = 1.36, std. err = 0.05, 95% CI = 3.66–3.84). Group 2 estimated the likelihood of abstention to be slightly lower with a mean of 3.65 (
N = 958, std. dev = 1.33, std. err = 0.04, 95% CI = 3.57–3.74). Group 3 does not differ as much from group 2 with a mean of 3.57 (
N = 877, std. dev = 1.39, std. err = 0.05, 95% CI = 3.47–3.66) Yet the control group has a significantly lower group mean of 2.99 (
N = 894, std. dev = 1.54, std. err = 0.05, 95% CI = 2.89–3.09).
To discern which group means are significantly different from each other, we conducted a post-hoc test. With this test, it is possible to observe how successful the manipulations were. Groups 1 and 2 do not have group means that show a significant difference on the p-level = 0.05 (mean diff. = 0.10, std. err. = 0.06). This means that people who receive information that 80% cooperate compared to 20% do not necessarily estimate a higher likelihood to abstain from using antibiotics. Notably, the group means differ significantly between Group 1 and Group 3 (mean diff. = 0.19, std. err. = 0.06, p = 0.05), meaning that if you also receive information that a lot of people cooperate you state you are more likely to abstain compared to the groups that only received information on the salience of the issue. It is also interesting to note that there is no difference in means between the group that only received information on the salience of the issue and the group that received information that 20% cooperate (mean diff. = −0.09, std. err. = 0.07, p = 0.56). The control group is significantly different from all other groups on the p-level = 0.00 (mean diff. from Group 1 = −0.76, std. err. = 0.07, mean diff. from Group 2 = −0.66, std. err. = 0.07, mean diff. from Group 3 = −0.57, std. err. = 0.07).
The effect size estimate, eta squared, tests how much of the variance can be related to group differences, or in other words how much of the variance is affected by the experimental condition. It was calculated to be 0.21 which entails that 21% of the variance is explained by the stimuli.
6. Discussion
Making use of unique cross-section data, we find that interpersonal trust, the belief that most people can be trusted, is associated with a willingness to limit personal use of antibiotics, also when controlling for a number of potential confounders. We thus find support for the first hypothesis of this paper and add to the emerging literature about the link between interpersonal trust and large-scale collective action.
The survey experiment demonstrates that respondents in the stimuli group who received information that 80% of other people cooperate were significantly more willing to limit their own use of antibiotics, as compared to respondents in the group who did not get any information about other people’s cooperativeness. However, contrary to the theoretical expectations, there was no significant difference in the willingness to limit antibiotic use between the “20%” and the “80%” treatment groups. Thus, while not finding unanimous support for our hypothesis, there is still an interesting relation between the trustworthiness of others and respondents’ own decisions to cooperate.
Thus, similar to many other sustainability and collective action resource dilemmas, the results of this study signify that trust and trustworthiness may be important for individuals’ willingness to reduce their personal use of antibiotics in order to prevent antibiotic resistance. However, contrasting the theoretical prediction, the experiment did not show any significant difference in the willingness to abstain from using antibiotics between the groups that received information that 20% cooperate or 80% cooperate. What could be the reason for this? This could possibly be due to the fact that 20% cooperation in large-scale collective action situations in fact shows that many people are ready to bear the cost of cooperation for the common good. To illustrate, 20% of Sweden’s population would entail that as many as 2 million people cooperate. However, if this occurred in a small-scale interaction, it would signify that the actual number of people cooperating is quite small. Further research may study the potential difference in the cut-off point for what is considered trustworthy behavior among other people in large-scale and small-scale collective action.
Antibiotics overuse and the development of antibiotic resistance is a transboundary and global problem. Hence, it is important to know who is being trusted in studies like this one. Future studies could replicate the current study but also compare the results with local and global framings.
Indeed, the results from this study are unique and an important contribution to the existing knowledge about factors that influence citizens’ willingness to limit antibiotic consumption for the sake of preventing resistance. In doing so, the study also adds to what is known about the role of interpersonal trust in stimulating large-scale collective action. Even so, the study has several limitations. Firstly, social desirability might make people more disposed to answer that they would be willing to limit their use of antibiotics to prevent resistance, and this bias may be more pronounced among high-trusting individuals. Secondly, the evidence found in the survey experiment could be an effect of “bandwagoning” rather than being about the trustworthiness of other people. Thirdly, the survey experiment is hypothetical and it can be brought into question to what extent the findings travel to a real-world setting.
In conclusion, using a mixed-methods approach, this paper demonstrates a link between interpersonal trust and willingness to limit personal use of antibiotics in order to prevent antibiotic resistance. Thus, interpersonal trust seems to be an invaluable asset for preserving the therapeutic capacity of antibiotics for future generations, as well as for successful realization of many of the Sustainable Development Goals.