Development of a Lethal Intranasal Exposure Model of Ebola Virus in the Cynomolgus Macaque
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Cells and Virus
2.3. Determination of Viral Titers
2.4. Effect of LMA® MAD on Ebola Virus Infectivity
2.5. Animal Studies
2.6. Experimental Inoculation of NHPs with EBOV
2.7. Determination of Viral Genome Copies
2.8. Hematology, Coagulation and Blood Chemistry
2.9. Statistics
3. Results
3.1. Effect of LMA® MAD on Ebola Virus Infectivity
3.2. Survival and Viremia in NHPs Exposed to EBOV via IN or IM Route
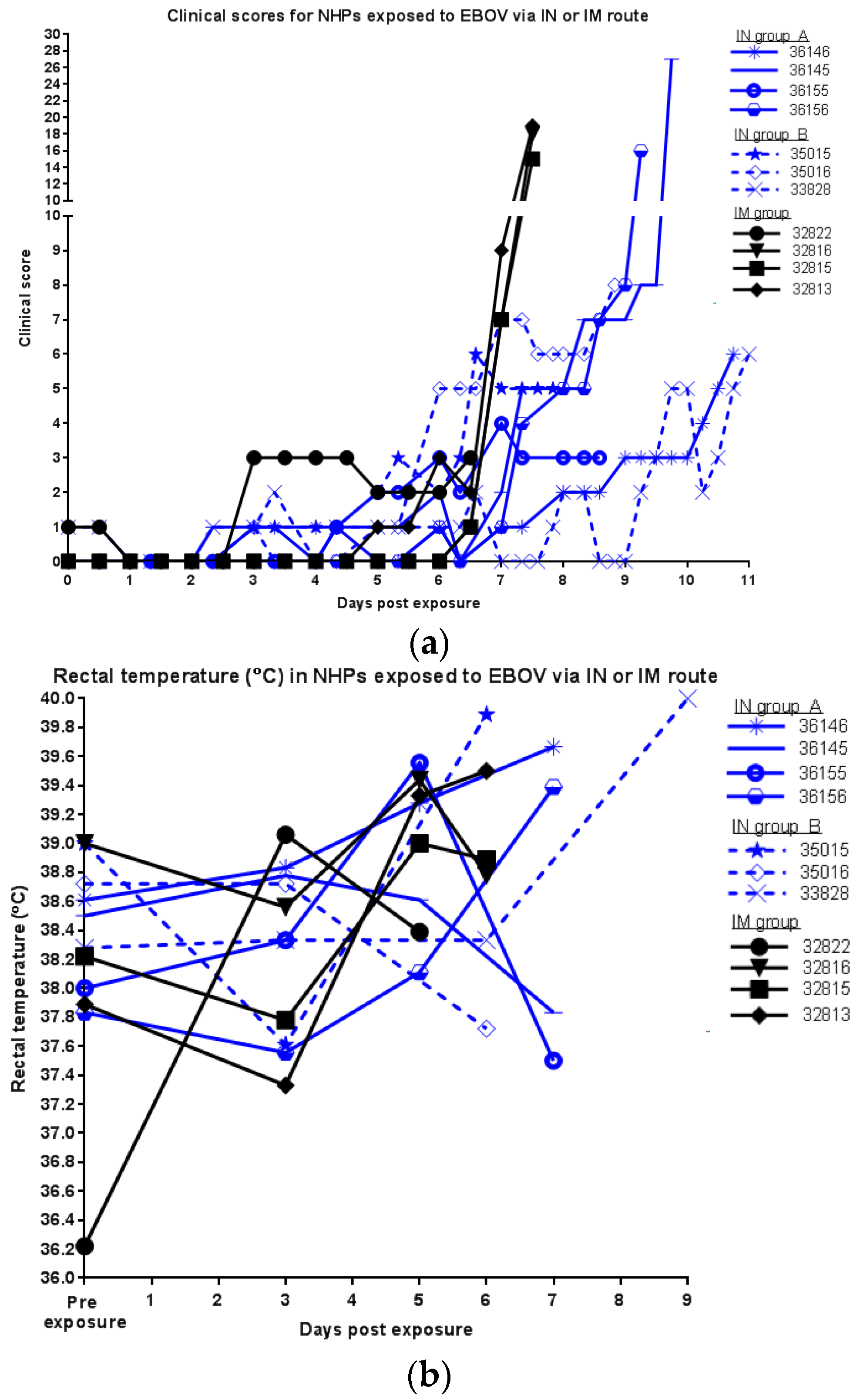
3.3. Other Clinical Parameters in NHPs Exposed to EBOV via IN or IM Route
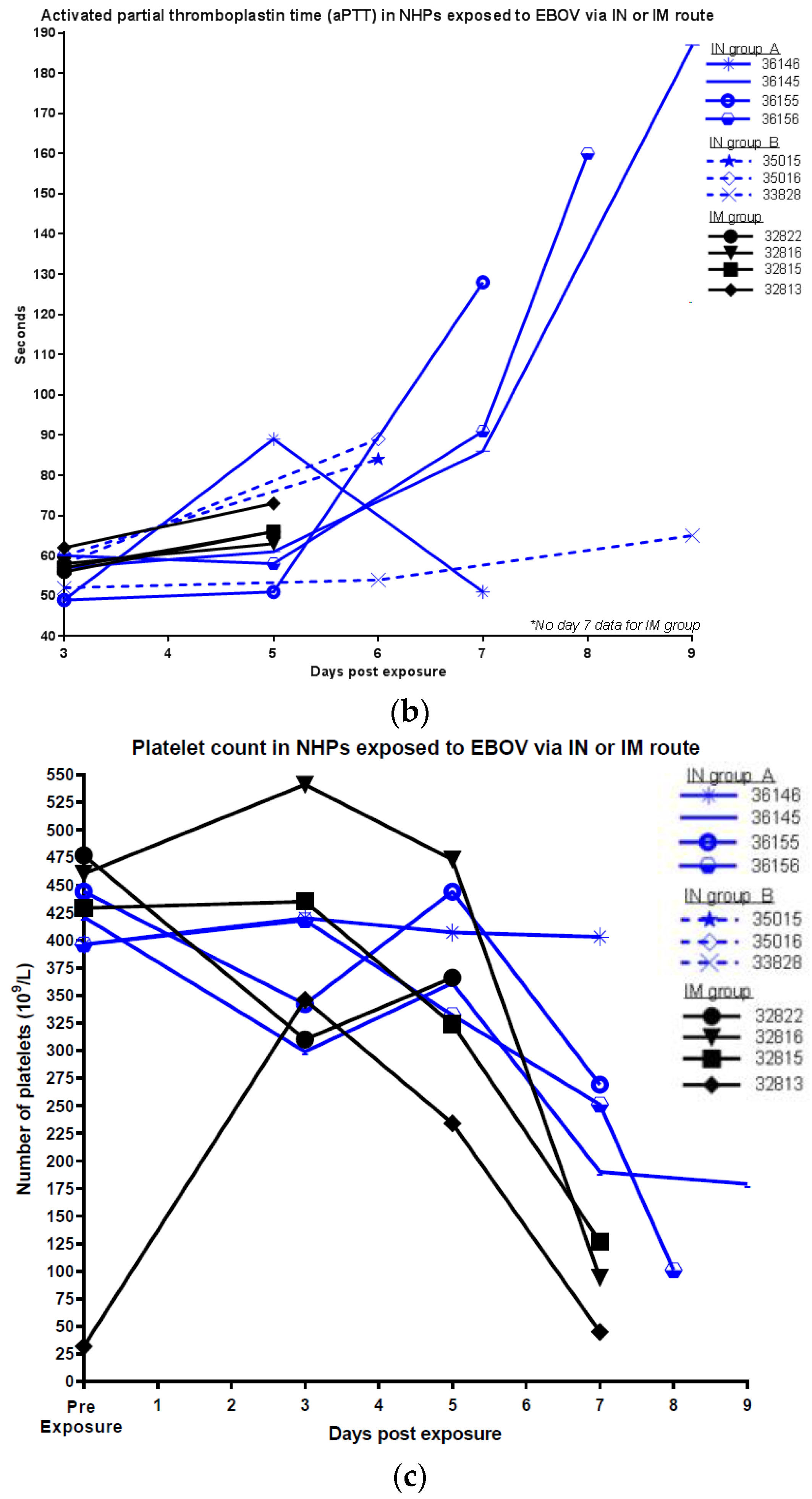
3.4. Hematology and Blood Chemistry in NHPs Exposed to EBOV via IN or IM Route
3.5. Pathology in NHPs Exposed to EBOV via IN or IM Route
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Baize, S.; Pannetier, D.; Oestereich, L.; Rieger, T.; Koivogui, L.; Magassouba, N.; Soropogui, B.; Sow, M.S.; Keïta, S.; de Clerck, H.; et al. Emergence of zaire ebola virus disease in guinea. N. Engl. J. Med. 2014, 371, 1418–1425. [Google Scholar] [CrossRef] [PubMed]
- Marsh, G.A.; Haining, J.; Robinson, R.; Foord, A.; Yamada, M.; Barr, J.A.; Payne, J.; White, J.; Yu, M.; Bingham, J.; et al. Ebola reston virus infection of pigs: Clinical significance and transmission Potential. J. Infect. Dis. 2011, 204, S804–S809. [Google Scholar] [CrossRef] [PubMed]
- Martina, B.E.E.; Osterhaus, A.D.M.E. “Filoviruses”: A real pandemic threat? EMBO Mol. Med. 2009, 1, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, R.; Leman, P.A.; Burt, F.J.; Zachariades, N.A.; Braack, L.E.; Ksiazek, T.G.; Rollin, P.E.; Zaki, S.R.; Peters, C.J. Experimental inoculation of plants and animals with ebola virus. Emerg. Infect. Dis. 1996, 2, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Gronvall, G.K.; Trent, D.; Borio, L.; Brey, R.; Nagao, L. The FDA animal efficacy rule and biodefense. Nat. Biotechnol. 2007, 25, 1084–1087. [Google Scholar] [CrossRef] [PubMed]
- Crawford, L.M. New drug and biological drug products; evidence needed to demonstrate effectiveness of new drugs when human efficacy studies are not ethical or feasible. Final Rule. Fed. Regist. 2002, 67, 37988–37998. [Google Scholar]
- Judson, S.; Prescott, J.; Munster, V. Understanding ebola virus transmission. Viruses 2015, 7, 511–512. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine; National Research Council. Research Priorities to Inform Public Health and Medical Practice for Ebola Virus Disease: Workshop in Brief; The National Academies Press: Washington, DC, USA, 2014. [Google Scholar]
- Bray, M.; Davis, K.; Geisbert, T.; Schmaljohn, C.; Huggins, J. A mouse model for evaluation of prophylaxis and therapy of ebola hemorrhagic fever. J. Infect. Dis. 1999, 179 (Suppl. 1), S248–S258. [Google Scholar] [CrossRef] [PubMed]
- Connolly, B.M.; Steele, K.E.; Davis, K.J.; Geisbert, T.W.; Kell, W.M.; Jaax, N.K.; Jahrling, P.B. Pathogenesis of experimental ebola virus infection in guinea pigs. J. Infect. Dis. 1999, 179 (Suppl. 1), S203–S217. [Google Scholar] [CrossRef] [PubMed]
- Kozak, R.; He, S.; Kroeker, A.; de La Vega, M.-A.; Audet, J.; Wong, G.; Urfano, C.; Antonation, K.; Embury-Hyatt, C.; Kobinger, G.P.; et al. Ferrets infected with bundibugyo virus or ebola virus recapitulate important aspects of human filovirus disease. J. Virol. 2016, 90, 9209–9223. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, E.; Saijo, M. Animal models for ebola and marburg virus infections. Front. Microbiol. 2013, 4, 267. [Google Scholar] [CrossRef] [PubMed]
- Feldmann, H.; Sanchez, A.; Geisbert, T.W. Filoviridae: Marburg and ebola viruses. Fields Virol. 2013, 1, 923–956. [Google Scholar]
- Osterholm, M.T.; Moore, K.A.; Kelley, N.S.; Brosseau, L.M.; Wong, G.; Murphy, F.A.; Peters, C.J.; LeDuc, J.W.; Russell, P.K.; van Herp, M.; et al. Transmission of ebola viruses: What we know and what we do not know. MBio 2015, 6, e00137. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, N.J.; Martin, J.E.; Graham, B.S.; Nabel, G.J. Correlates of protective immunity for ebola vaccines: Implications for regulatory approval by the animal rule. Nat. Rev. Microbiol. 2009, 7, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Dowell, S.F.; Mukunu, R.; Ksiazek, T.G.; Khan, A.S.; Rollin, P.E.; Peters, C.J. Transmission of Ebola hemorrhagic fever: A study of risk factors in family members, Kikwit, Democratic Republic of the Congo, 1995. Commission de Lutte contre les Epidémies à Kikwit. J. Infect. Dis. 1999, 179 (Suppl. 1), S87–S91. [Google Scholar] [CrossRef] [PubMed]
- Klenk, H.-D.; Feldmann, H. Ebola and marburg viruses; Garland Science, Horizon Bioscience: Wymondham, UK, 2004. [Google Scholar]
- Jaax, N.K.; Davis, K.J.; Geisbert, T.J.; Vogel, P.; Jaax, G.P.; Topper, M.; Jahrling, P.B. Lethal experimental infection of rhesus monkeys with ebola-zaire (mayinga) virus by the oral and conjunctival route of exposure. Arch. Pathol. Lab. Med. 1996, 120, 140–155. [Google Scholar] [PubMed]
- Mire, C.E.; Geisbert, J.B.; Agans, K.N.; Deer, D.J.; Fenton, K.A.; Geisbert, T.W. Oral and conjunctival exposure of nonhuman primates to low doses of ebola makona virus. J. Infect. Dis. 2016, 214, S263–S267. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.; Jaax, N.; White, J.; Jahrling, P. Lethal experimental infections of rhesus monkeys by aerosolized ebola virus. Int. J. Exp. Pathol 1995, 76, 227–236. [Google Scholar] [PubMed]
- Geisbert, T.W.; Daddario-Dicaprio, K.M.; Geisbert, J.B.; Reed, D.S.; Feldmann, F.; Grolla, A.; Ströher, U.; Fritz, E.A.; Hensley, L.E.; Jones, S.M.; et al. Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with ebola and marburg viruses. Vaccine 2008, 26, 6894–6900. [Google Scholar] [CrossRef] [PubMed]
- Gralton, J.; Tovey, E.; McLaws, M.-L.; Rawlinson, W.D. The role of particle size in aerosolised pathogen transmission: A review. J. Infect. 2011, 62, 1–13. [Google Scholar] [CrossRef] [PubMed]
- National Research Council, Division on Earth and Life Studies, Institute for Laboratory Animal Research, Committee for the Update of the Guide for the Care and Use of Laboratory Animals. National research council guide for the care and use of laboratory animals, 8th ed.; The National Academies Press: Washington, DC, USA, 2010. [Google Scholar]
- Trombley, A.R.; Wachter, L.; Garrison, J.; Buckley-Beason, V.A.; Jahrling, J.; Hensley, L.E.; Schoepp, R.J.; Norwood, D.A.; Goba, A.; Fair, J.N.; et al. Comprehensive panel of real-time TaqMan™ polymerase Chain reaction assays for detection and absolute quantification of filoviruses, arenaviruses, and new world hantaviruses. Am. J. Trop. Med. Hyg. 2010, 82, 954–960. [Google Scholar] [CrossRef] [PubMed]
- Alfson, K.J.; Avena, L.E.; Beadles, M.W.; Staples, H.; Nunneley, J.W.; Ticer, A.; Dick, E.J.; Owston, M.A.; Reed, C.; Patterson, J.L.; et al. Particle-to-PFU ratio of ebola virus influences disease course and survival in cynomolgus macaques. J. Virol. 2015, 89, 6773–6781. [Google Scholar] [CrossRef] [PubMed]
- Alfson, K.J.; Worwa, G.; Carrion, R.; Griffiths, A. Determination and therapeutic exploitation of ebola virus spontaneous mutation frequency. J. Virol. 2016, 90, 2345–2355. [Google Scholar] [CrossRef] [PubMed]
- Hirschberg, R.; Ward, L.A.; Kilgore, N.; Kurnat, R.; Schiltz, H.; Albrecht, M.T.; Christopher, G.W.; Nuzum, E. Challenges, progress, and opportunities: Proceedings of the filovirus medical countermeasures workshop. Viruses 2014, 6, 2673–2697. [Google Scholar] [CrossRef] [PubMed]
- Shurtleff, A.; Biggins, J.; Keeney, A.; Zumbrun, E.; Bloomfield, H.; Kuehne, A.; Audet, J.; Alfson, K.; Griffiths, A.; Olinger, G.; et al. Standardization of the filovirus plaque assay for use in preclinical studies. Viruses 2012, 4, 3511–3530. [Google Scholar] [CrossRef] [PubMed]
- Bausch, D.G.; Towner, J.S.; Dowell, S.F.; Kaducu, F.; Lukwiya, M.; Sanchez, A.; Nichol, S.T.; Ksiazek, T.G.; Rollin, P.E. Assessment of the risk of ebola virus transmission from bodily fluids and fomites. J. Infect. Dis. 2007, 196 (Suppl. 2), S142–S147. [Google Scholar] [CrossRef] [PubMed]
- Pond, K.; Hooper, L.; Edmunds, K.; Hunter, P. Presence and persistence of ebola or marburg virus in patients and survivors: A Rapid systematic review. PLoS Negl. Trop. Dis. 2016, 10, e0004475. [Google Scholar]
- Schnittler, H.J.; Feldmann, H. Marburg and ebola hemorrhagic fevers: Does the Primary course of infection depend on the accessibility of organ-specific macrophages? Clin. Infect. Dis. 1998, 27, 404–406. [Google Scholar] [CrossRef] [PubMed]
- Stroher, U.; West, E.; Bugany, H.; Klenk, H.D.; Schnittler, H.J.; Feldmann, H. Infection and activation of monocytes by marburg and ebola viruses. J. Virol. 2001, 75, 11025–11033. [Google Scholar] [CrossRef] [PubMed]
- Wong, G.; Qiu, X.; de La Vega, M.-A.; Fernando, L.; Wei, H.; Bello, A.; Fausther-Bovendo, H.; Audet, J.; Kroeker, A.; Kozak, R.; et al. Pathogenicity comparison between the Kikwit and Makona Ebola virus variants in rhesus macaques. J. Infect. Dis. 2016, 214, S281–S289. [Google Scholar] [CrossRef] [PubMed]
- Kortepeter, M.G.; Bausch, D.G.; Bray, M. Basic clinical and laboratory features of filoviral hemorrhagic fever. J. Infect. Dis. 2011, 204 (Suppl. 3), S810–S816. [Google Scholar] [CrossRef] [PubMed]
- Bah, E.I.; Lamah, M.-C.; Fletcher, T.; Jacob, S.T.; Brett-Major, D.M.; Sall, A.A.; Shindo, N.; Fischer, W.A.; Lamontagne, F.; Saliou, S.M.; et al. Clinical presentation of patients with ebola virus disease in conakry, guinea. N. Engl. J. Med. 2015, 372, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Roels, T.H.; Bloom, A.S.; Buffington, J.; Muhungu, G.L.; Mac Kenzie, W.R.; Khan, A.S.; Ndambi, R.; Noah, D.L.; Rolka, H.R.; Peters, C.J.; et al. Ebola hemorrhagic fever, Kikwit, Democratic Republic of the Congo, 1995: Risk Factors for patients without a reported exposure. J. Infect. Dis. 1999, 179, S92–S97. [Google Scholar] [CrossRef] [PubMed]
- Kekulé, A.S. Learning from Ebola virus: How to prevent future epidemics. Viruses 2015, 7, 3789–3797. [Google Scholar] [CrossRef] [PubMed]





| Group | Exposure Route | Number of Animals | Target Dose for EBOV Exposure [PFU] | Determined Dose for EBOV Exposure [PFU] |
|---|---|---|---|---|
| IN group A | intranasal | 4 | 120 | 80 |
| IN group B | intranasal | 3 | 500 | 64 |
| IM | intramuscular | 4 | 100 | 74 |
| Group | Petechial Rash | Testicular Hemorrhage | Dark, Red Axillary Lymph Node | Pale or Enlarged Spleen | Pale, Friable Liver | Dark, Red Lungs | Redness or Hemorrhage in GI Tract |
|---|---|---|---|---|---|---|---|
| IN (A) | 3/4 | 2/2 | 1/4 | 1/4 | 3/4 | 3/4 | 2/4 |
| IN (B) | 3/3 | 2/2 | 2/3 | 2/3 | 0/3 | 2/3 | 3/3 |
| IM | 4/4 | 2/4 | 1/4 | 1/4 | 0/4 | 3/4 | 1/4 |
| Organ | Histopathology Finding | Group (Number Exhibiting/Number in Group) | ||
|---|---|---|---|---|
| IM | IN A | IN B | ||
| Spleen | Fibrin deposition | 3/4 | 4/4 | 3/3 |
| Lymphoid depletion | 3/4 | 4/4 | 3/3 | |
| Lymphocytolysis | 3/4 | 4/4 | 3/3 | |
| Congestion/hemorrhage, marginal sinus | 2/4 | 4/4 | 3/3 | |
| Lymph node | Lymphoid depletion | 3/4 | 4/4 | 3/3 |
| Necrosis | 4/4 | 4/4 | 3/3 | |
| Liver | Hepatocellular necrosis | 2/4 | 4/4 | 3/3 |
| Lung | Edema | n.d. | 2/4 | 2/3 |
| Fibrin deposition | n.d. | 2/4 | 0/3 | |
| Inflammation | n.d. | 3/4 | 1/3 | |
| Necrosis | n.d. | 1/4 | 1/3 | |
| Hemorrhage | n.d. | 2/4 | 1/3 | |
| Adrenal gland | Individual cell necrosis | 0/4 | 3/4 | 3/3 |
| Testicle | Hemorrhage | 3/4 | 2/2 | 2/2 |
| GI Tract | Hemorrhage | 1/4 | 2/4 | 2/3 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfson, K.J.; Avena, L.E.; Worwa, G.; Carrion, R.; Griffiths, A. Development of a Lethal Intranasal Exposure Model of Ebola Virus in the Cynomolgus Macaque. Viruses 2017, 9, 319. https://doi.org/10.3390/v9110319
Alfson KJ, Avena LE, Worwa G, Carrion R, Griffiths A. Development of a Lethal Intranasal Exposure Model of Ebola Virus in the Cynomolgus Macaque. Viruses. 2017; 9(11):319. https://doi.org/10.3390/v9110319
Chicago/Turabian StyleAlfson, Kendra J., Laura E. Avena, Gabriella Worwa, Ricardo Carrion, and Anthony Griffiths. 2017. "Development of a Lethal Intranasal Exposure Model of Ebola Virus in the Cynomolgus Macaque" Viruses 9, no. 11: 319. https://doi.org/10.3390/v9110319




