Morphological and Structural Study of a Novel Porous Nurse’s A Ceramic with Osteoconductive Properties for Tissue Engineering
Abstract
:1. Introduction
2. Results
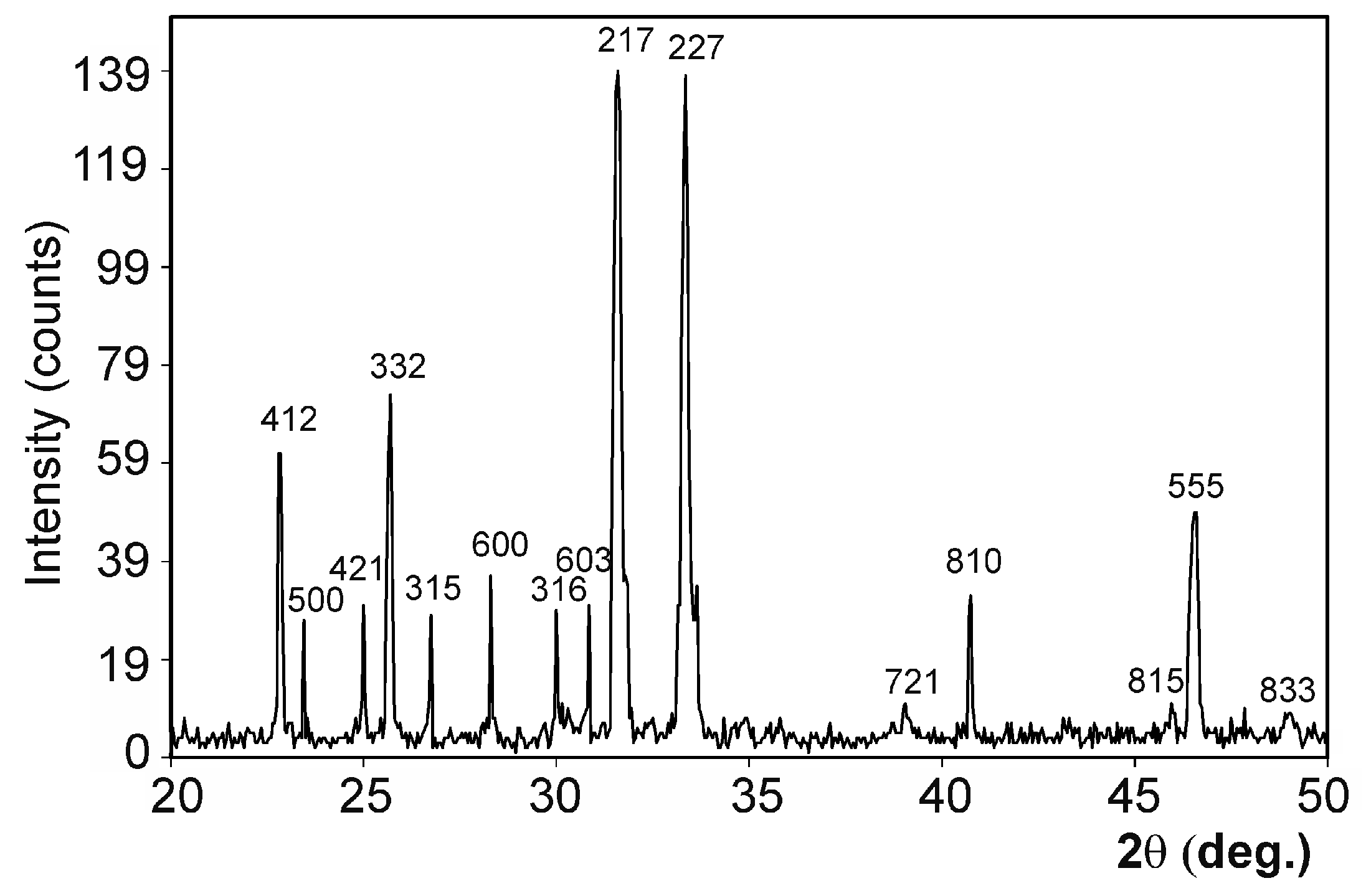
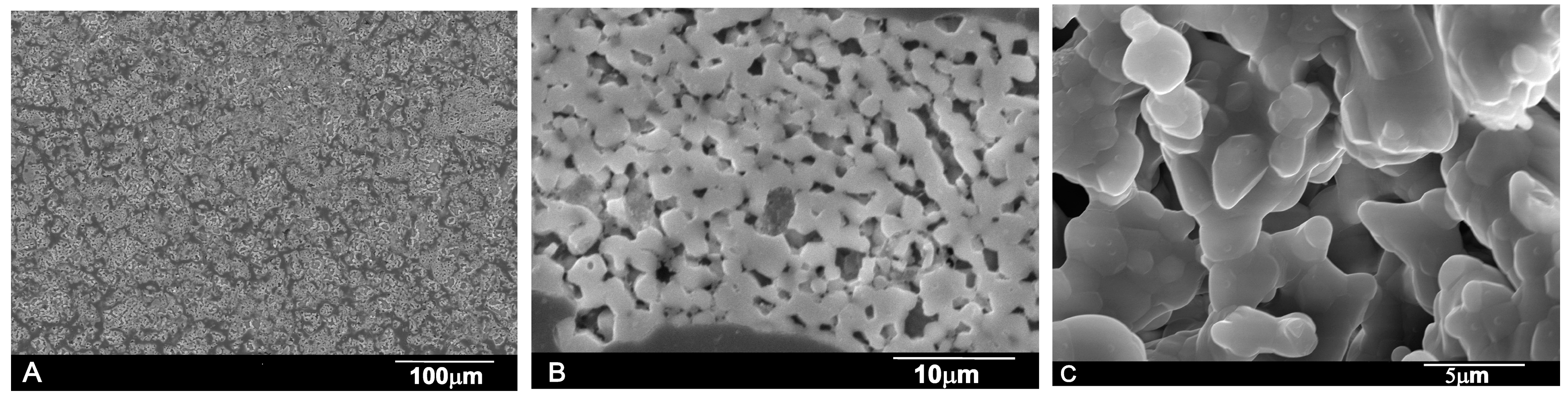
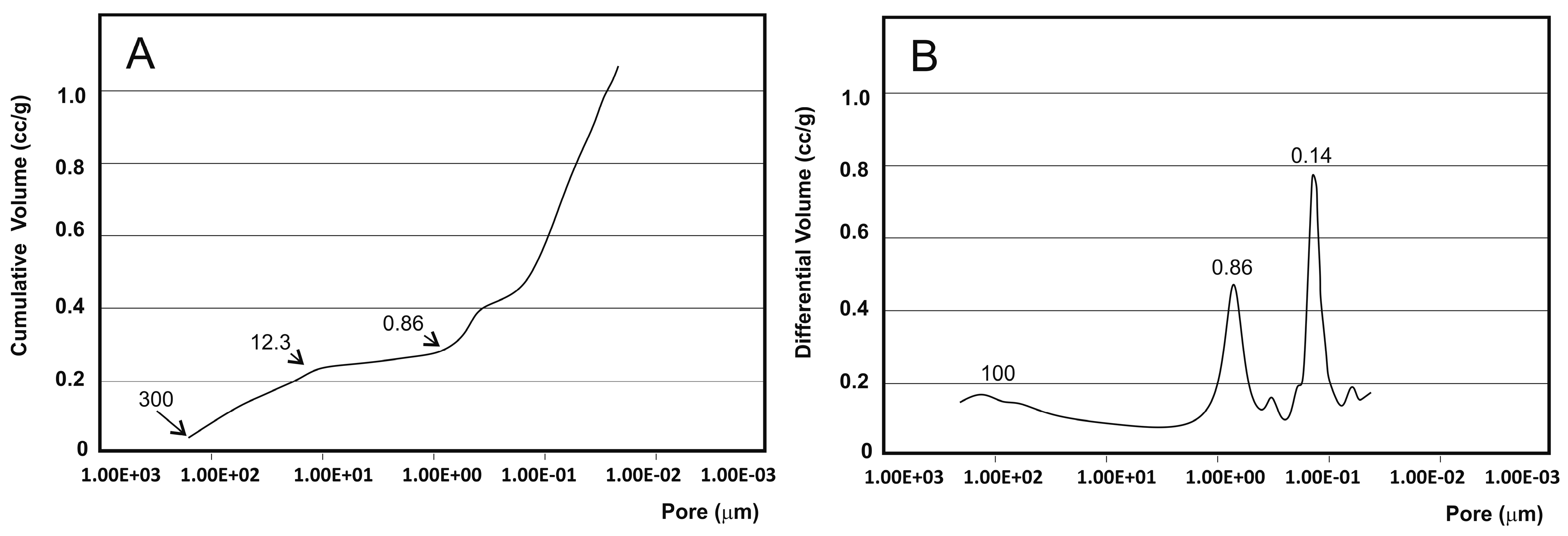
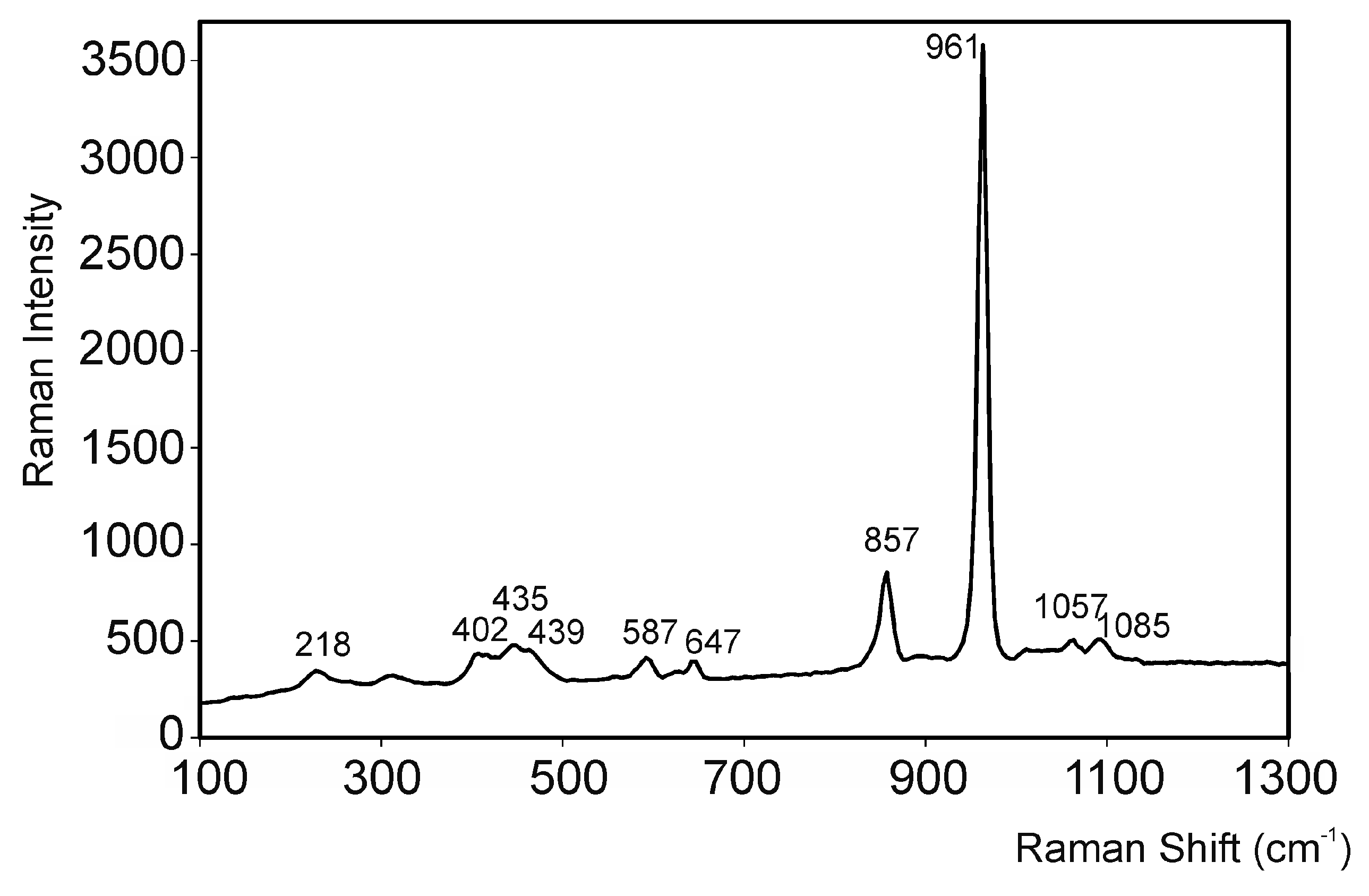
2.1. Biomaterial Characterization
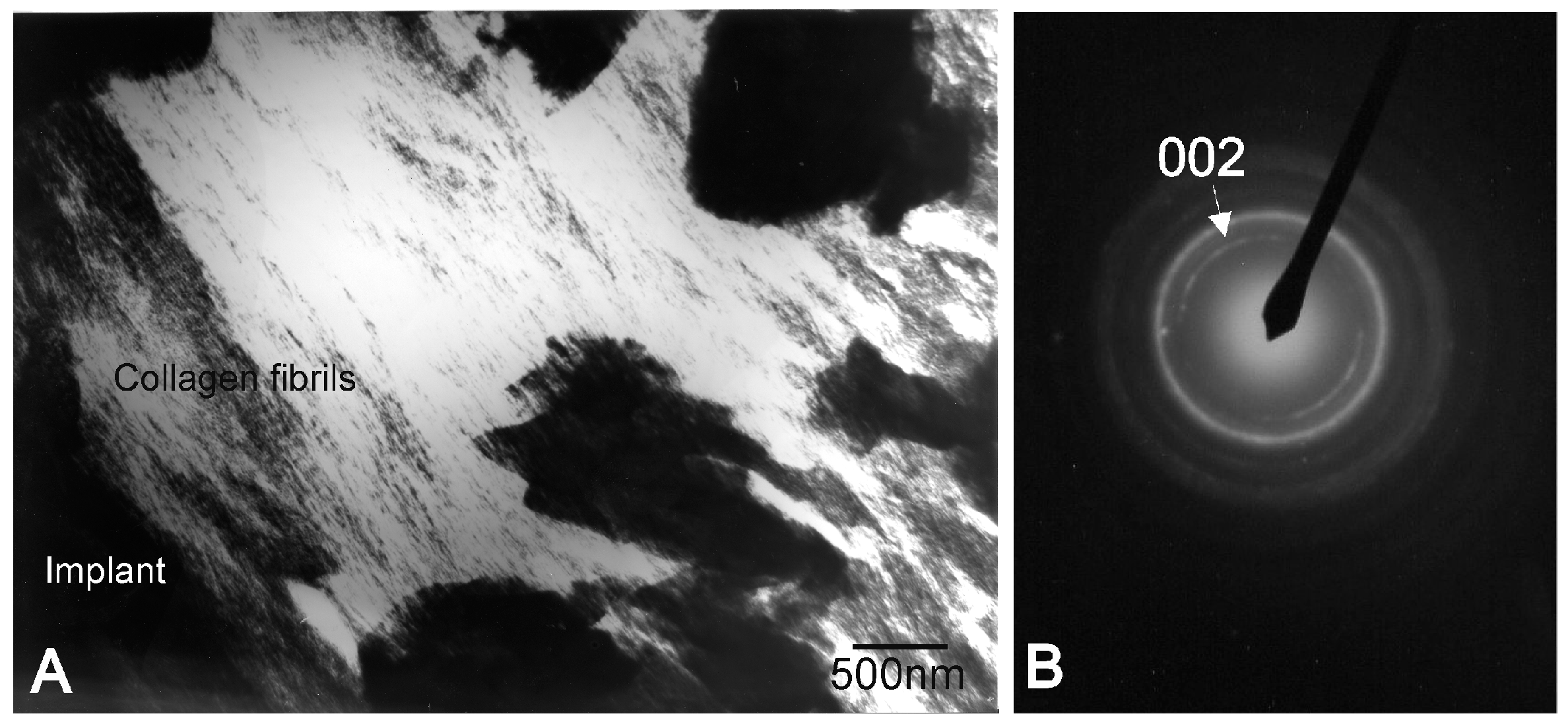
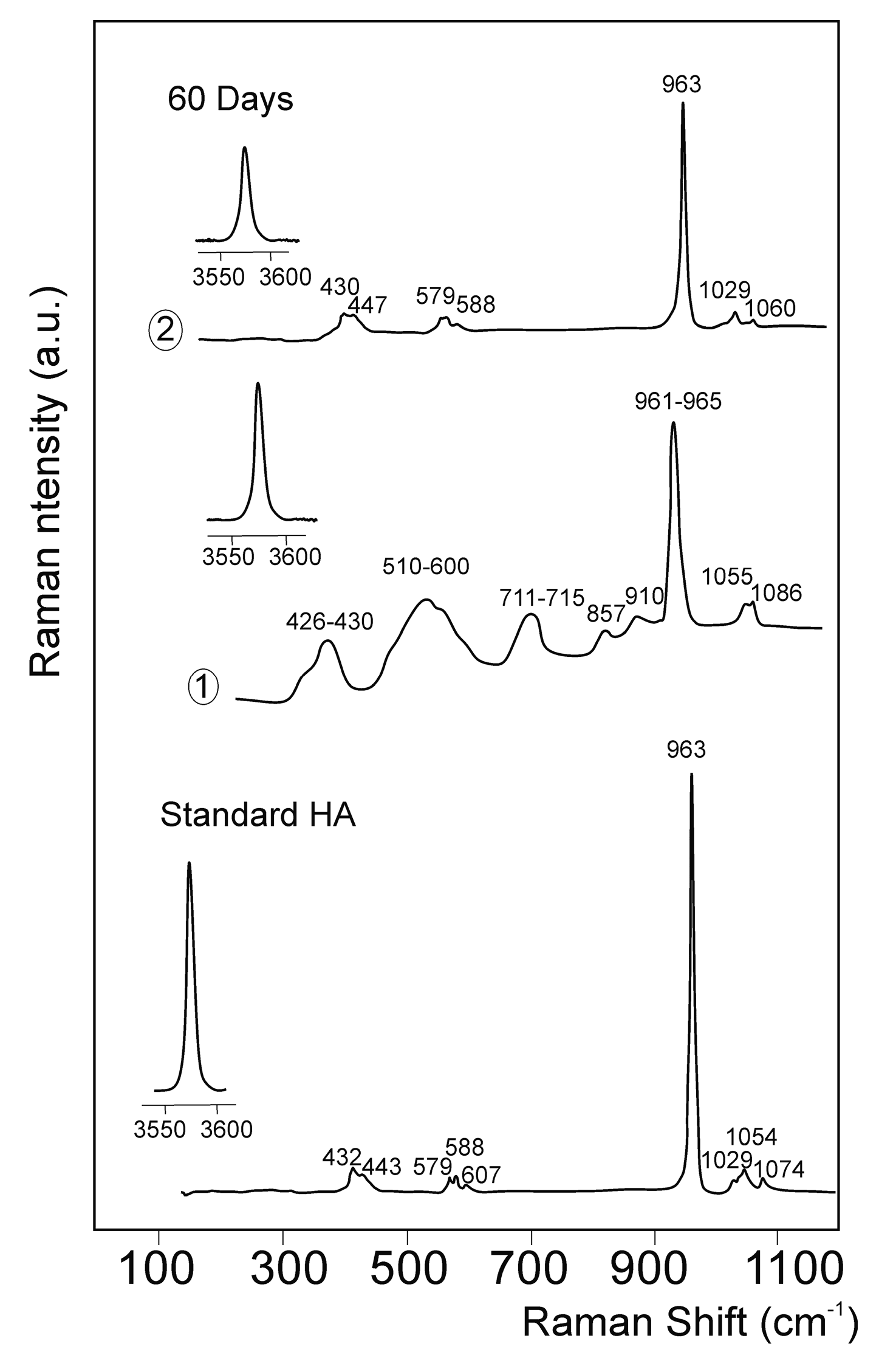
2.2. Implants Characterization
3. Discussion
4. Materials and Methods
4.1. Biomaterial
4.2. Animal Experimentation
4.2.1. Principal Protocol
4.2.2. Surgery
4.3. Implant Characterization
4.4. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Bohner, M. Silicon-substituted calcium phosphates—A critical view. Biomaterials 2009, 30, 6403–6406. [Google Scholar] [CrossRef] [PubMed]
- Chevalier, J.; Gremillard, L. Ceramics for medical applications: A picture for the next 20 years. J. Eur. Ceram. Soc. 2009, 29, 1245–1255. [Google Scholar] [CrossRef]
- Mate-Sanchez de Val, J.E.; Calvo-Guirado, J.L.; Delgado-Ruiz, R.A.; Ramirez-Fernandez, M.P.; Negri, B.; Abboud, M.; Martinez, I.M.; de Aza, P.N. Physical properties, mechanical behavior, and electron microscopy study of a new α-tcp block graft with silicon in an animal model. J. Biomed. Mater. Res. A 2012, 100, 3446–3454. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Guirado, J.L.; Ramirez-Fernandez, M.P.; Mate-Sanchez de Val, J.E.; Negri, B.; Velasquez, P.; de Aza, P.N. Enhanced bone regeneration with a novel synthetic bone substitute in combination with a new natural cross-linked collagen membrane: Radiographic and histomorphometric study. Clin. Oral Implant. Res. 2015, 26, 154–164. [Google Scholar] [CrossRef] [PubMed]
- De Aza, P.N.; Luklinska, Z.B.; Mate-Sanchez de Val, J.E.; Calvo-Guirado, J.L. Biodegradation process of α-tricalcium phosphate and α-tricalcium phosphate solid solution bioceramics in vivo: A comparative study. Microsc. Microanal. 2013, 19, 1350–1357. [Google Scholar] [CrossRef] [PubMed]
- Velasquez, P.; Luklinska, Z.B.; Meseguer-Olmo, L.; Mate-Sanchez de Val, J.E.; Delgado-Ruiz, R.A.; Calvo-Guirado, J.L.; Ramirez-Fernandez, M.P.; de Aza, P.N. αTCP ceramic doped with Dicalcium Silicate for bone regeneration applications prepared by powder metallurgy method. In vitro and in vivo studies. J. Biomed. Mater. Res. A 2013, 101, 1943–1954. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Guirado, J.L.; Ramirez-Fernandez, M.P.; Delgado-Ruiz, R.A.; Mate-Sanchez de Val, J.E.; Velasquez, P.; de Aza, P.N. Influence of biphasic α-TCP with and without the use of collagen membranes on bone healing of surgically critical size defects. A radiological, histological and histomorphometric study. Clin. Oral Implant. Res. 2014, 25, 1228–1238. [Google Scholar] [CrossRef] [PubMed]
- Serena, S.; Caballero, A.; de Aza, P.N.; Sainz, M.A. New evaluation of the in vitro response of silicocarnotite monophasic material. Ceram. Int. 2015, 41, 9411–9419. [Google Scholar] [CrossRef]
- García-Paez, I.H.; Garcıa Carrodeguas, R.; de Aza, A.H.; Baudin, C.; Pena, P. Effect of Mg and Si co-substitution on microstructure and strength of tricalcium phosphate ceramics. J. Mech. Behav. Biomed. Mater. 2014, 30, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Lugo, G.J.; Mazón, P.; de Aza, P.N. Phase transitions in single phase Si–Ca–P-based ceramic under thermal treatment. J. Eur. Ceram. Soc. 2015, 35, 3693–3700. [Google Scholar] [CrossRef]
- Jugdaohsingh, R.; Tucker, K.L.; Qiao, N.; Cupples, L.A.; Kiel, D.P.; Powell, J.J. Dietary silicon intake is positively associated with bone mineral density in men and premenopausal women of the framingham offspring cohort. J. Bone Miner. Res. 2004, 19, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Sayer, M.; Stratilatov, A.D.; Reid, J.; Calderin, L.; Stott, M.J.; Yin, X.; MacKenzie, M.; Smith, T.J.N.; Hendry, J.A.; Langstaff, S.D. Structure and composition of silicon-stabilized tricalcium phosphate. Biomaterials 2003, 24, 369–382. [Google Scholar] [CrossRef]
- Reid, J.W.; Tuc, L.K.; Sayer, M.; Fargo, K.; Hendry, J.A. Synthesis and characterization of single-phase silicon-substituted α-tricalcium phosphate. Biomaterials 2006, 27, 2916–2925. [Google Scholar] [CrossRef] [PubMed]
- Martinez, I.M.; Velasquez, P.A.; Meseguer-Olmo, L.; Bernabeu-Esclapez, A.; de Aza, P.N. Preparation and characterization of novel bioactive α-Tricalcium Phosphate doped with Dicalcium Silicate ceramics. Mater. Sci. Eng. C 2012, 32, 878–886. [Google Scholar] [CrossRef]
- Martinez, I.M.; Velasquez, P.A.; Meseguer-Olmo, L.; de Aza, P.N. Production and study of in vitro behaviour of monolithic α-Tricalcium Phosphate based ceramics in the system Ca3(PO4)2–Ca2SiO4. Ceram. Int. 2011, 37, 2527–2535. [Google Scholar] [CrossRef]
- Carrodeguas, R.G.; de Aza, A.H.; Jimenez, J.; de Aza, P.N.; Pena, P.; López-Bravo, A.; de Aza, S. Preparation and in vitro characterization of wollastonite doped tricalcium phosphate bioceramics. Key Eng. Mater. 2008, 361–363, 237–240. [Google Scholar] [CrossRef]
- Lugo, G.J.; Mazón, P.; de Aza, P.N. Material processing of a new calcium silicophosphate ceramic. Ceram. Int. 2016, 42, 673–680. [Google Scholar] [CrossRef]
- Ros-Tarraga, P.; Mazón, P.; Meseguer-Olmo, L.; de Aza, P.N. Revising the subsystem nurse’s A–phase-silicocarnotite within the system Ca3(PO4)2–Ca2SiO4. Materials 2016. [Google Scholar] [CrossRef]
- Rubio, V.; de la Casa-Lillo, M.A.; de Aza, S.; de Aza, P.N. The system Ca3(PO4)2–Ca2SiO4: The sub-system Ca2SiO4–7CaOP2O5·2SiO2. J. Am. Ceram. Soc. 2011, 94, 4459–4462. [Google Scholar] [CrossRef]
- De Aza, P.N.; Guitian, F.; Santos, C.; de Aza, S.; Cusco, R.; Artus, L. Vibrational properties of calcium phosphare compounds. II Comparation between hydroxyapatite and β-tricalcium phosphate. Chem. Mater. 1997, 9, 916–922. [Google Scholar] [CrossRef]
- Remy, C.; Reynard, B.; Madon, M. Raman spectroscopic investigations of Dicalcium Silicate: Polymorphs and high-temperature phase transformations. J. Am. Ceram. Soc. 1997, 80, 413–423. [Google Scholar] [CrossRef]
- Ibáñez, J.; Artús, L.; Cuscó, R.; López, A.; Menéndez, E.; Andrade, M.C. Hydration and carbonation of monoclinic Ca2SiO4 and Ca3SiO5 studied by Raman spectroscopy. J. Raman Spectrosc. 2001, 38, 61–67. [Google Scholar] [CrossRef]
- Antonakos, A.; Liarokapis, E.; Leventouri, T. Micro-Raman and FTIR studies of synthetic and natural apatites. Biomaterials 2007, 28, 3043–3054. [Google Scholar] [CrossRef] [PubMed]
- Bonino, F.; Damin, A.; Aina, V.; Miola, M.; Vernè, E.; Bretcanu, O.; Bordiga, S.; Zecchina, A.; Morterra, C. In situ Raman study to monitor bioactive glasses reactivity. J. Raman Spectrosc. 2008, 39, 260–264. [Google Scholar] [CrossRef]
- Aguiar, H.; Solla, E.L.; Serra, J.; González, P.; León, B.; Malz, F.; Jäger, C. Raman and NMR study of bioactive Na2O–MgO–CaO–P2O5–SiO2 glasses. J. Non Cryst. Solids 2008, 354, 5004–5008. [Google Scholar] [CrossRef]
- Hadjicharalambous, C.; Prymak, O.; Loza, K.; Buyakov, A.; Kulkov, S.; Chatzinikolaidou, M. Effect of porosity of alumina and zirconia ceramics toward pre-osteoblast response. Front. Bioeng. Biotechnol. 2015, 3, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Akkineni, A.R.; Basu, B.; Gelinsky, M. Three-dimensional plotted hydroxyapatite scaffolds with predefined architecture: Comparison of stabilization by alginate cross-linking versus sintering. J. Appl. Biomater. Funct. Mater. 2015, 30, 1168–1181. [Google Scholar] [CrossRef] [PubMed]
- Lazáry, A.; Balla, B.; Kósa, J.P.; Bácsi, K.; Nagy, Z.; Takács, I.; Varga, P.P.; Speer, G.; Lakatos, P. Effect of gypsum on proliferation and differentiation of MC3T3-E1 mouse osteoblastic cells. Biomaterials 2007, 28, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Carlisle, E.M. Silicon: A possible factor in bone calcification. Science 1970, 167, 279–280. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, K.A. Bound form of silicon in glycosaminoglycans and polyuronides. Proc. Natl. Acad. Sci. USA 1973, 70, 1608–1612. [Google Scholar] [CrossRef] [PubMed]
- De Aza, P.N.; Mate-Sanchez de Val, J.E.; Baudin, C.; Perez Albacete-Martinez, C.; Armijo-Salto, A.; Calvo-Guirado, J.L. Bone neoformation of a novel porous resorbable Si-Ca-P-based ceramic with osteocondutive properties: Physical and mechanical characterization, histological and histomorphometric study. Clin. Oral Implant. Res. 2016. [Google Scholar] [CrossRef] [PubMed]
- De Aza, P.N.; Peña, J.I.; Luklinska, Z.B.; Meseguer-Olmo, L. Bioeutectic℘ ceramics for biomedical application obtained by Laser Floating Zone Method: In vivo evaluation. Materials 2014, 7, 2395–2410. [Google Scholar] [CrossRef]
- Baier, R.E. The organisation of blood components near interface. Ann. N. Y. Acad. Sci. 1977, 283, 17–36. [Google Scholar] [CrossRef]
- Kochwa, S.; Litwak, R.S.; Rosenfield, R.E.; Leonard, E.F. Blood elements at foreign surfaces: A biochemical approach to the study of the adsorption of plasma proteins. Ann. N. Y. Acad. Sci. 1977, 283, 37–49. [Google Scholar] [CrossRef]
- Breemhaar, W.; Brinkman, E.; Ellens, D.J.; Beugeling, T.; Bantjes, A. Preferential adsorption of high-density lipoprotein form blood plasma onto biomaterial surfaces. Biomaterials 1984, 5, 269–274. [Google Scholar] [CrossRef]
- Xynos, I.D.; Edgar, A.J.; Buttery, L.D.K.; Hench, L.L.; Polak, J.M. Ionic products of bioactive glass dissolution increase proliferation of human osteoblasts and induce insulin-like growth factor II mRNA expression and protein synthesis. Biomed. Biophys. Res. Commun. 2000, 276, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Beltrame, F.; Cancedda, R.; Canesi, B.; Crovace, A.; Mastrogiacomo, M.; Quarto, R.; Scaglione, S.; Valastro, C.; Viti, F. A simple non invasive computerized method for the assessment of bone repair within osteoconductive porous bioceramic grafts. Biotechnol. Bioeng. 2005, 92, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Mate-Sanchez de Val, J.E.; Calvo-Guirado, J.L.; Gomez Moreno, G.; Perez Albacete-Martinez, C.; Mazón, P.; de Aza, P.N. Influence of hydroxyapatite granule size, porosity and crystallinity on tissue reaction in vivo. Part A: Synthesis, characterization of the materials and SEM analysis. Clin. Oral Implant. Res. 2016. [Google Scholar] [CrossRef] [PubMed]
- Mate-Sanchez de Val, J.E.; Calvo-Guirado, J.L.; Delgado-Ruiz, R.A.; Ramirez-Fernandez, M.P.; Martinez, I.M.; Granero-Marin, J.M.; Negri, B.; Chiva-Garcia, F.; Martinez-Gonzalez, J.M.; de Aza, P.N. New block graft of α-TCP with silicon in critical size defects in rabbits: Chemical characterization, histological, histomorphometric and micro-CT study. Ceram. Int. 2012, 38, 1563–1570. [Google Scholar] [CrossRef]



| Crystalline Size (Sherrer Å) | Shrinkage (%) | Intruded Volume (cc/g) | Total Porosity (%) | Intraparticle Porosity (%) a | Interparticle Porosity (%) b | Real Density (g/cm3) | Apparent Density (g/cm3) | Strength (MPa) |
|---|---|---|---|---|---|---|---|---|
| 213 | 31.99 ± 0.5 | 0.1127 | 20.21 | 15.013 | 5.1969 | 2.13 | 1.72 | 0.60 ± 0.02 |
| (wt %) | O | Ca | P | Si |
|---|---|---|---|---|
| Nurse’ A Material | ||||
| 0 day | 39.21 ± 0.50 (39.21) | 42.50 ± 0.50 (42.50) | 9.70 ± 0.50 (9.70) | 8.54 ± 0.03 (8.54) |
| HA Theoretical | ||||
| 0 day | 41.39 | 39.90 | 18.50 | - |
| Implant | ||||
| 15 days | 38.9 ± 1.58 (38.9) | 42.12 ± 1.66 (42.12) | 10.5 ± 0.57 (10.5) | 8.50 ± 1.05 (8.50) |
| 30 days | 42.10 ± 1.64 (42.10) | 40.30 ± 1.54 (40.30) | 9.7 ± 0.53 (9.7) | 7.9 ± 0.86 (7.9) |
| 60 days | 43.60 ± 1.78 (43.60 ) | 39.7 ± 1.43 (39.7) | 9.21 ± 0.40 (9.21) | 7.5 ± 0.64 (7.5) |
| Interphase | ||||
| 15 days | 51.07 ± 1.97 (51.07) | 31.46 ± 1.46 (31.46) | 15.57 ± 0.96 (15.57) | 1.90 ± 1.1 (1.90) |
| 30 days | 53.37 ± 1.87 (53.37) | 31.27 ± 1.50 (31.27) | 14.89 ± 0.87 (14.90) | 0.71 ± 1.62 (0.71) |
| 60 days | 53.94 ± 1.89 (53.94) | 30.94 ± 1.38 (30.94) | 14.78 ± 0.84 (14.78) | 0.34 ± 0.94 (0.34) |
| New Bone | ||||
| 15 days | 51.82 ± 1.96 (51.82) | 32.56 ± 1.37 (32.56) | 15.36 ± 0.98 (15.36) | 0.26 ± 1.30 (0.26) |
| 30 days | 53.71 ± 1.88 (53.71) | 31.92 ± 0.44 (31.92) | 14.18 ± 0.96 (14.18) | 0.19 ± 1.58 (0.19) |
| 60 days | 54.17 ± 0.91 (54.17) | 31.57 ± 0.42 (31.57) | 14.09 ± 0.87 (14.10) | 0.17 ± 1.01 (0.17) |
| Time of Implantation | Implant | Interphase | New Bone |
|---|---|---|---|
| Ca/P Ratio | Ca/P Ratio | Ca/P Ratio | |
| 15 days | 4.01 ± 0.23 (4.01) | 2.02 ± 0.54 (2.02) | 2.12 ± 0.99 (2.12) |
| 30 days | 4.15 ± 0.16 (4.15) | 2.10 ± 0.43 (2.10) | 2.20 ± 0.67 (2.20) |
| 60 days | 4.31 ± 0.64 (4.34) | 2.16 ± 0.45 (2.16) | 2.24 ± 0.75 (2.24) |
| Time of Implantation | Implant Material | |
|---|---|---|
| Residual Biomaterial (%) | Resorption Rate | |
| 15 days | 73.32 ± 2.04 (73.32) | 26.68 ± 1.05 (26.68) |
| 30 days | 64.21 ± 1.07 (64.21) | 35.79 ± 0.74 (35.80) |
| 60 days | 47.38 ± 1.24 (47.39) | 52.62 ± 1.12 (52.62) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabadan-Ros, R.; Velásquez, P.A.; Meseguer-Olmo, L.; De Aza, P.N. Morphological and Structural Study of a Novel Porous Nurse’s A Ceramic with Osteoconductive Properties for Tissue Engineering. Materials 2016, 9, 474. https://doi.org/10.3390/ma9060474
Rabadan-Ros R, Velásquez PA, Meseguer-Olmo L, De Aza PN. Morphological and Structural Study of a Novel Porous Nurse’s A Ceramic with Osteoconductive Properties for Tissue Engineering. Materials. 2016; 9(6):474. https://doi.org/10.3390/ma9060474
Chicago/Turabian StyleRabadan-Ros, Ruben, Pablo A. Velásquez, Luis Meseguer-Olmo, and Piedad N. De Aza. 2016. "Morphological and Structural Study of a Novel Porous Nurse’s A Ceramic with Osteoconductive Properties for Tissue Engineering" Materials 9, no. 6: 474. https://doi.org/10.3390/ma9060474






