Calcium Phosphate as a Key Material for Socially Responsible Tissue Engineering
Abstract
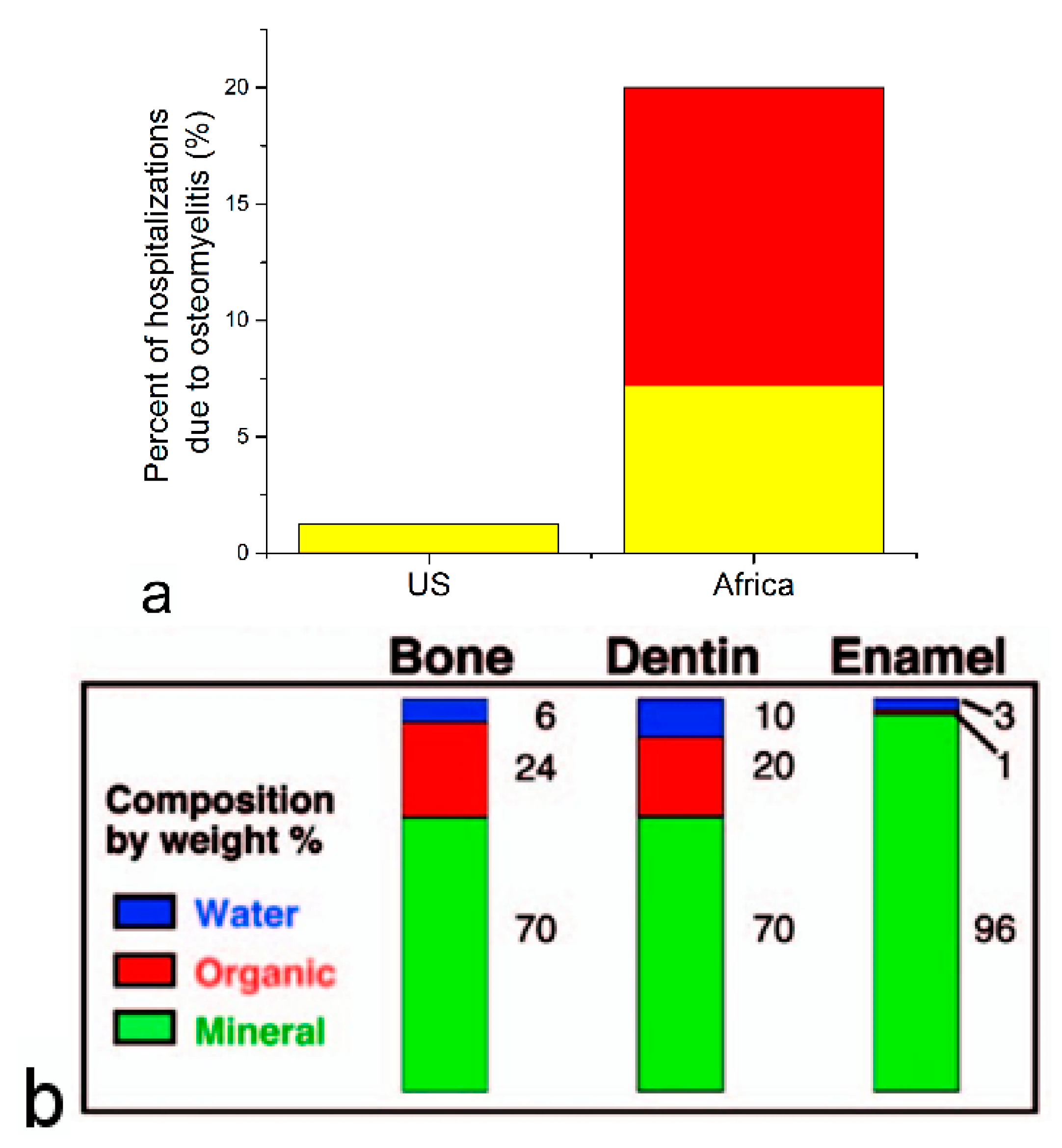
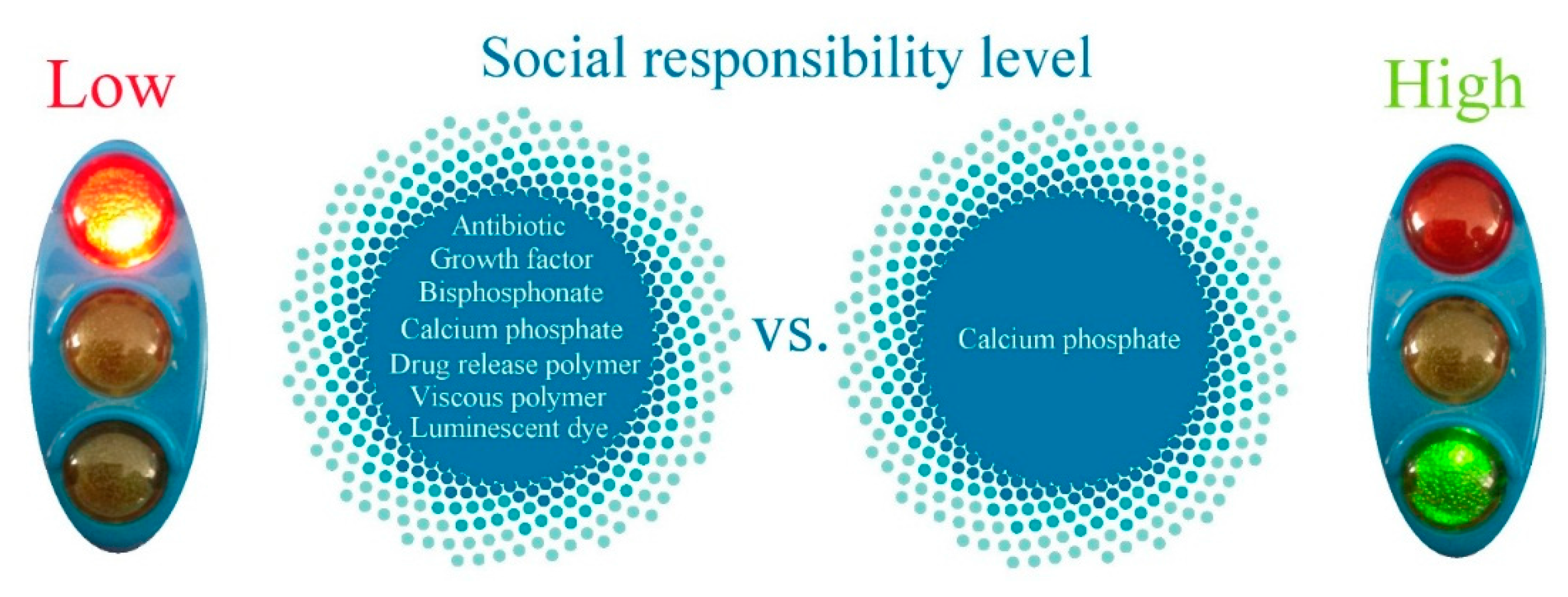
:1. Introduction
“I have to leave the convent and consecrate myself to the poor” [1].Mother Teresa, Calcutta—Darjeeling train, 1946.
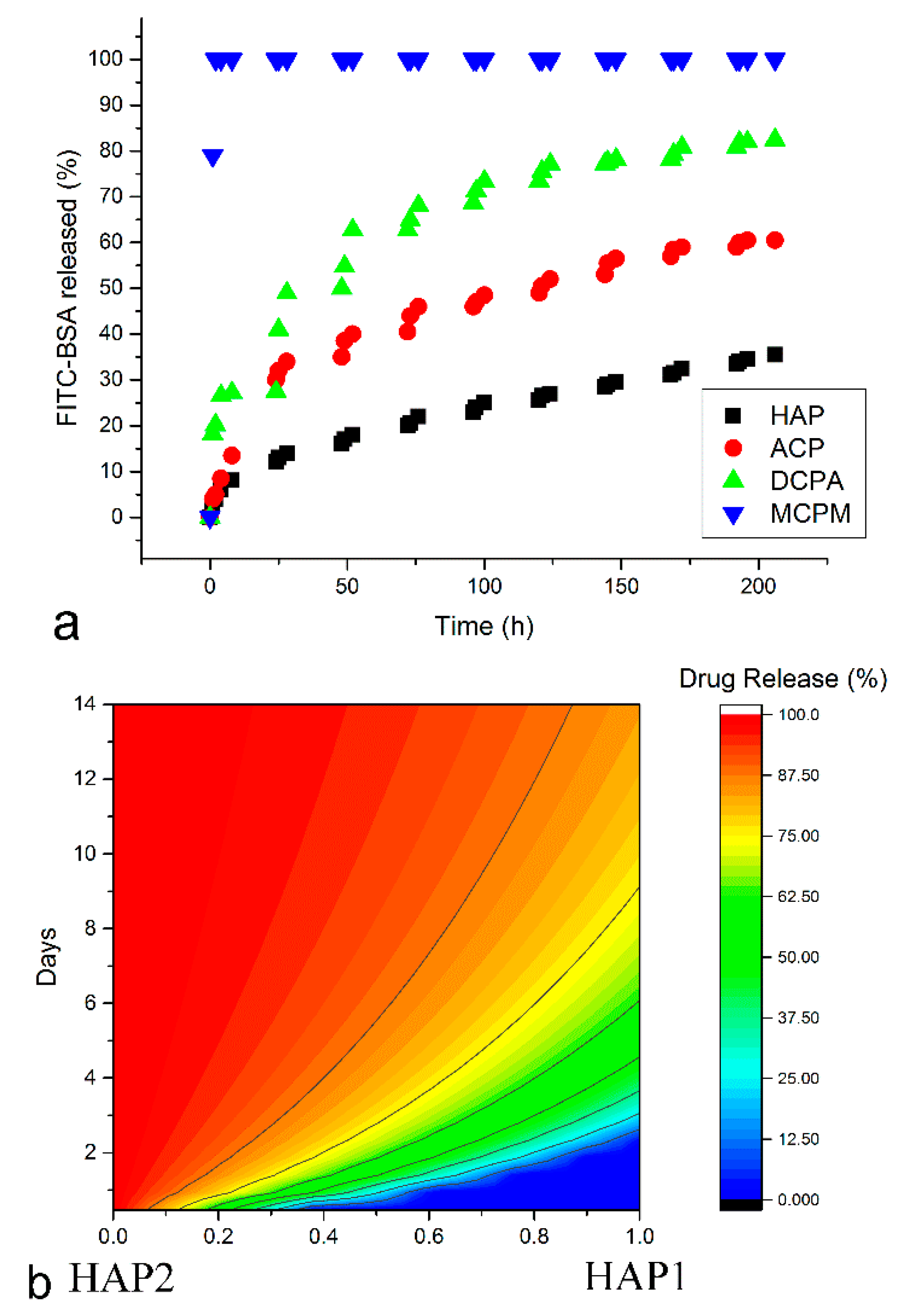
2. CAP as a Tunable Drug Release Carrier and a Viscous, Self-Setting Material for Injectable Bone Grafts
3. CAP as an Intracellular Delivery Carrier
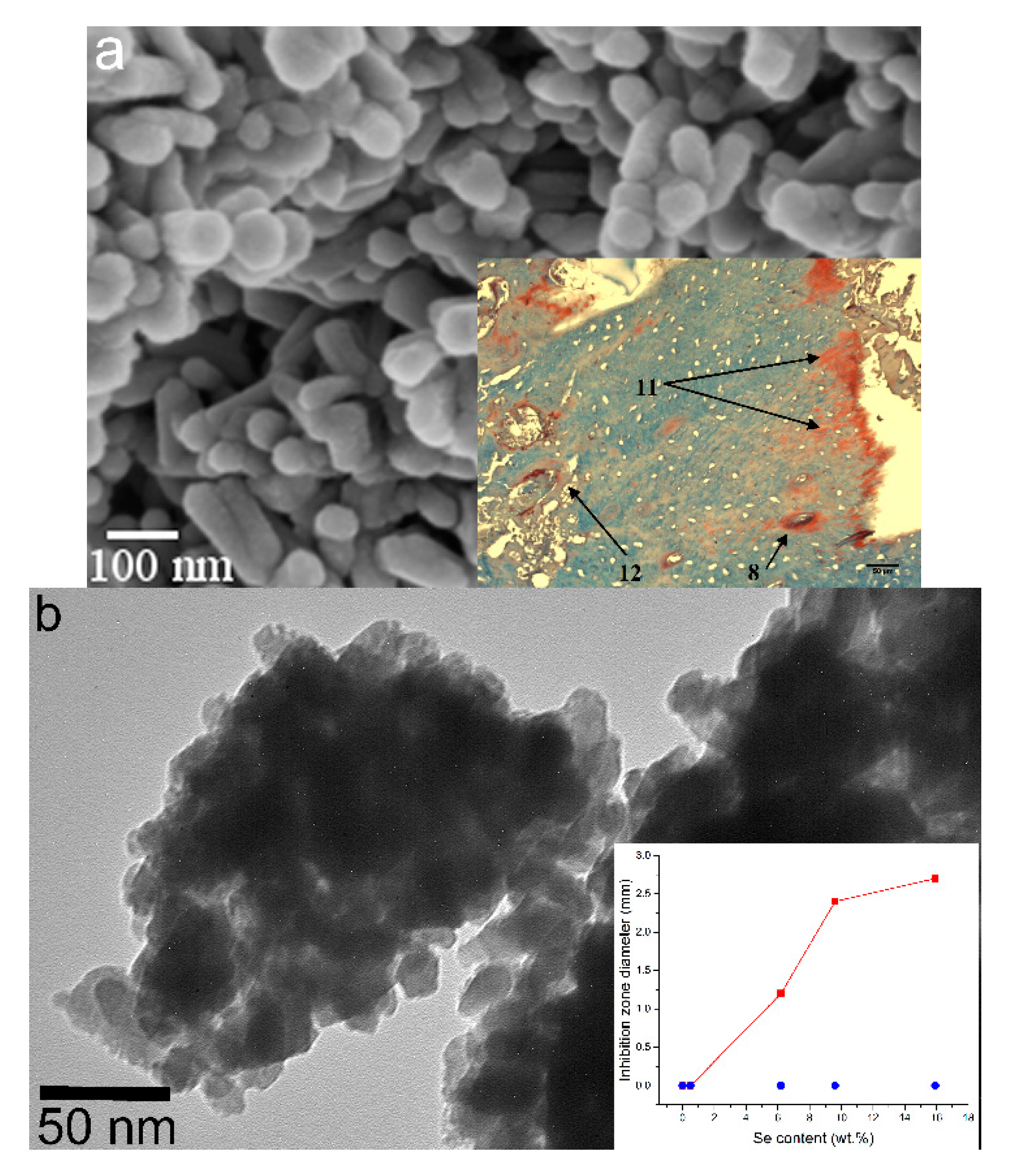
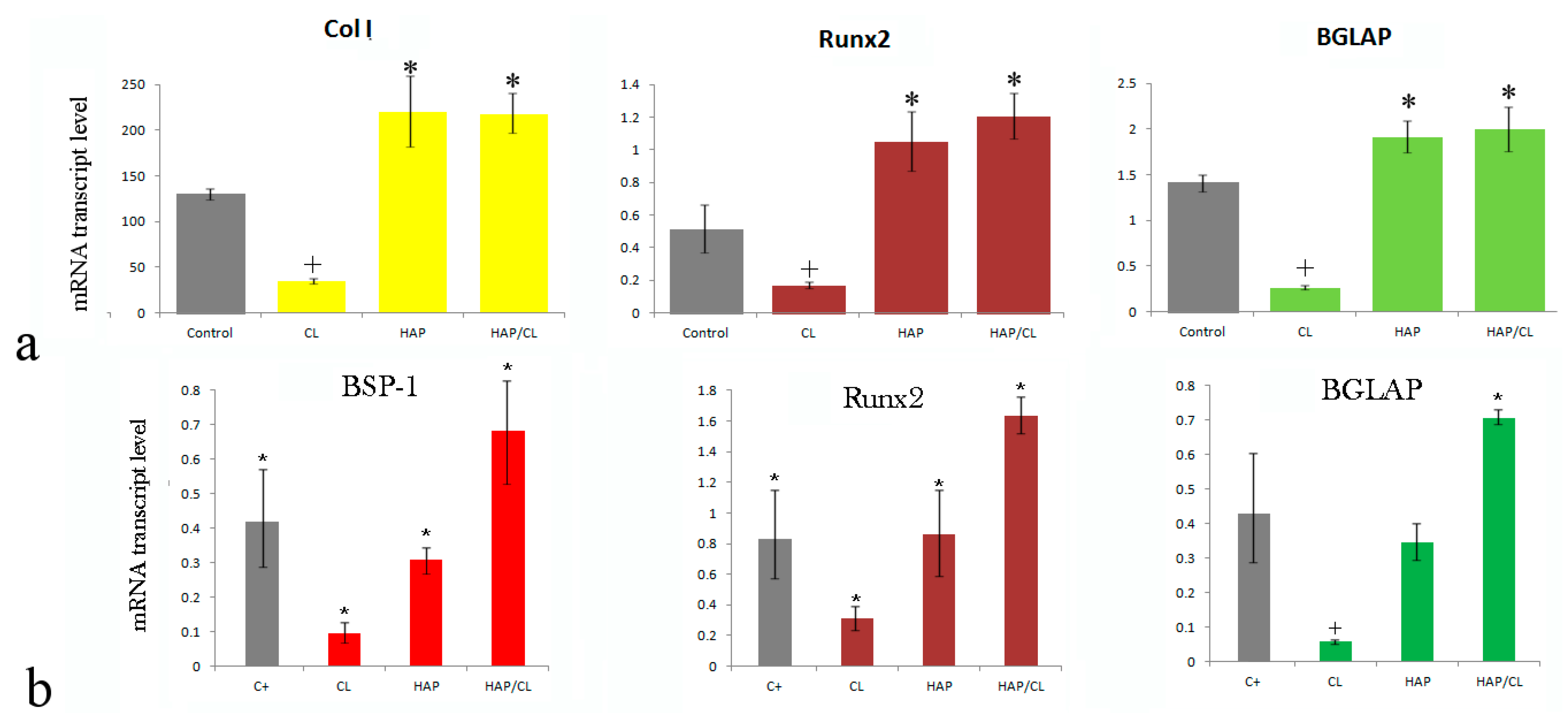
4. CAP as a Foreign Ion Accommodator
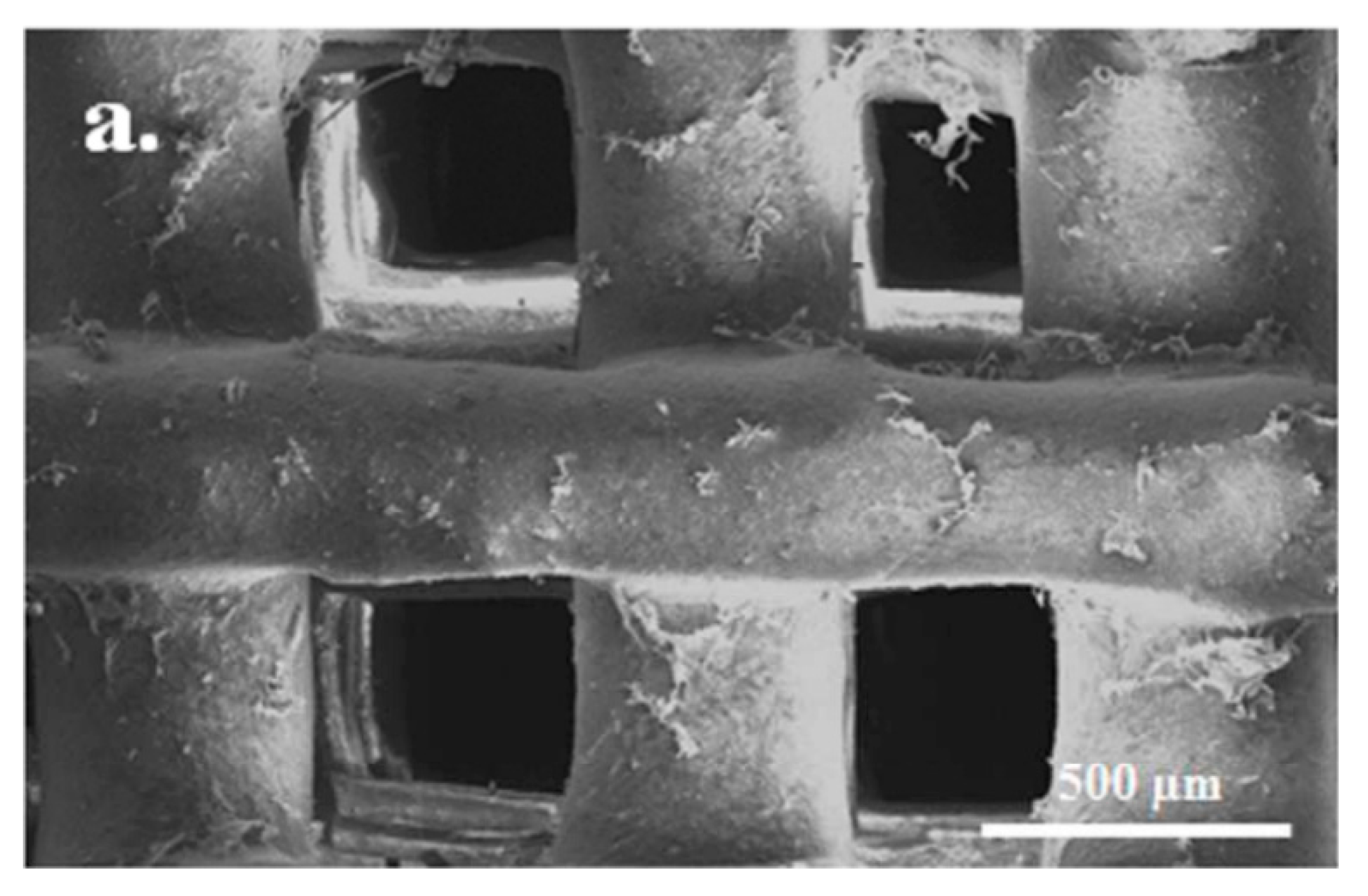
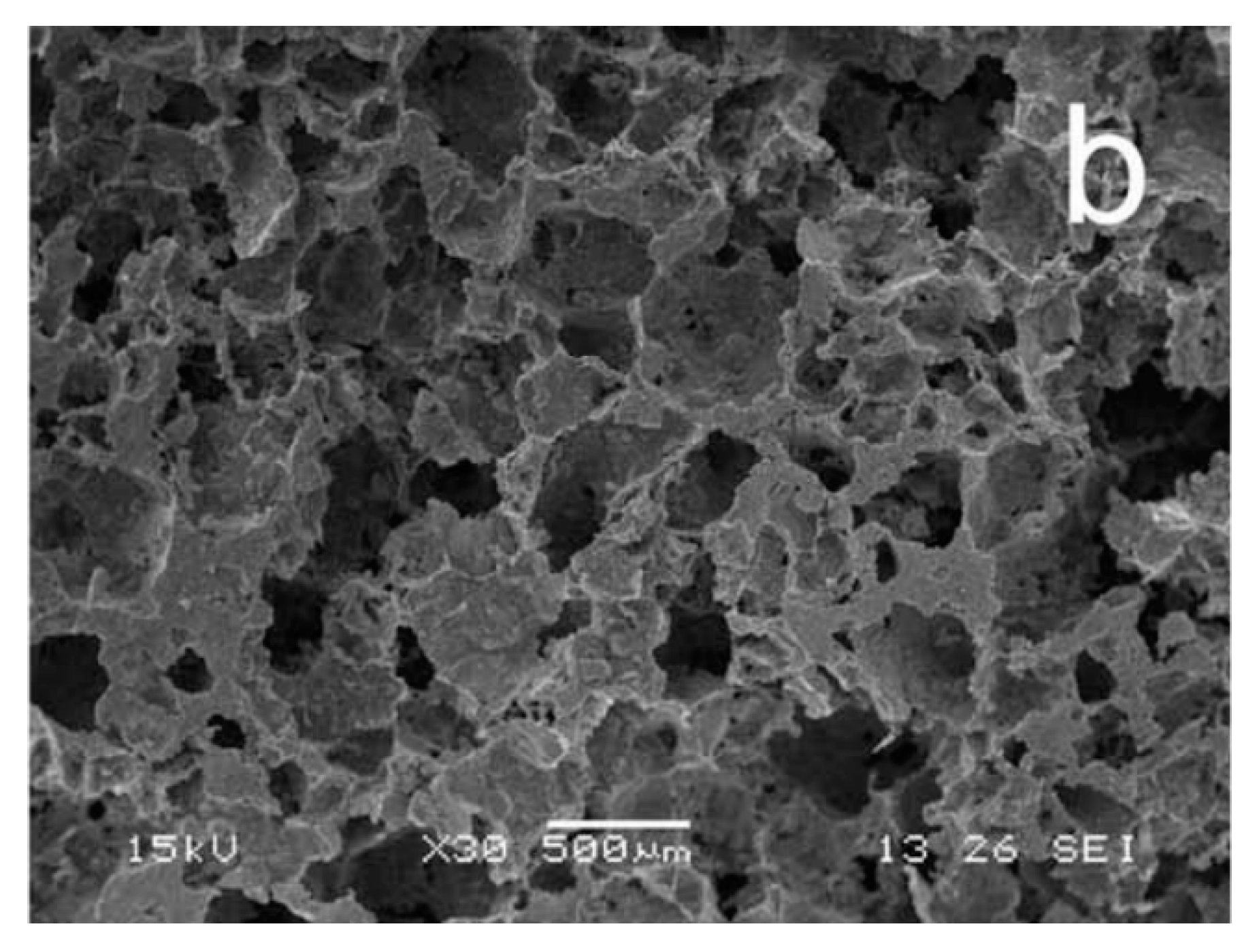
5. CAP as a Material Formable into Macroporous Constructs for Tissue Engineering
6. CAP as a Naturally Osteo-Inductive and Osteogenic Material
7. CAP as a Natural Inhibitor of Osteoclastogenesis
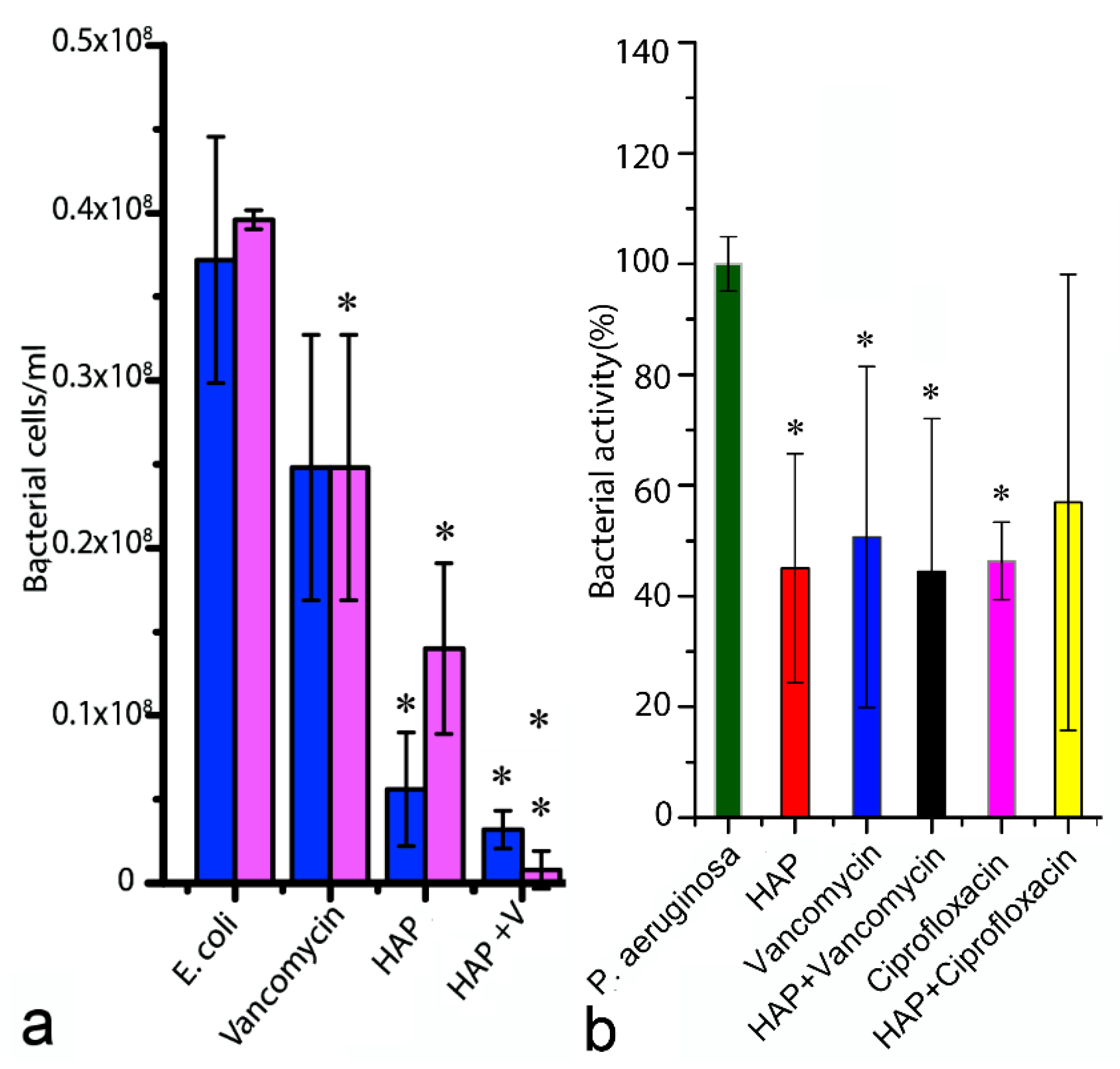
8. CAP as a Natural Antimicrobial
9. CAP as the Ugly Duckling Concealing a Swan Within
10. Conclusions
Acknowledgments
Conflicts of Interest
References
- Gonzalez-Balado, J.L. Mother Teresa: In My Own Words; Gramercy: New York, NY, USA, 1996. [Google Scholar]
- Mao, Y.; Park, T.-J.; Zhang, F.; Zhou, H.; Wong, S.S. Environmentally Friendly Methodologies of Nanostructure Synthesis. Small 2007, 3, 1122–1139. [Google Scholar] [CrossRef] [PubMed]
- Uskoković, V. Nanostructured platforms for the sustained and local delivery of antibiotics in the treatment of osteomyelitis. Crit. Rev. Ther. Drug Carr. Syst. 2015, 32, 1–59. [Google Scholar] [CrossRef]
- Lew, D.P.; Waldvogel, F.A. Osteomyelitis. Lancet 2004, 364, 369–379. [Google Scholar] [CrossRef]
- Del Pozo, J.L.; Patel, R. Clinical practice. Infection associated with prosthetic joints. N. Engl. J. Med. 2009, 361, 787–794. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.C.; Bradley, J.S. Osteoarticular Infections in Children. Infect. Dis. Clin. N. Am. 2015, 29, 557–574. [Google Scholar] [CrossRef] [PubMed]
- Meier, D.E.; Rouma, B.S. Haematogenous Osteomyelitis and Septic Arthritis. In Paediatric Surgery: A Comprehensive Text for Africa; Ameh, E.A., Bickler, S.W., Lakhoo, K., Nwomeh, B.C., Poenaru, D., Eds.; Global Help: Seattle, WA, USA, 2011; pp. 135–140. [Google Scholar]
- Vazquez, M. Osteomyelitis in children. Curr. Opin. Pediatr. 2002, 14, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Christensen, K.L.Y.; Holman, R.C.; Steiner, C.A.; Sejvar, J.J.; Stoll, B.J.; Schonberger, L.B. Infectious disease hospitalizations in the United States. Clin. Infect. Dis. 2009, 49, 1025–1035. [Google Scholar] [CrossRef] [PubMed]
- Pasteris, J.D.; Wopenka, B.; Valsami-Jones, E. Bone and Tooth Mineralization: Why Apatite? Elements 2008, 4, 97–104. [Google Scholar] [CrossRef]
- Yenson, A.; de Fries, H.O.; Deeb, Z.E. Actinomycotic osteomyelitis of the facial bones and mandible. Otolaryngol. Head. Neck. Surg. 1983, 91, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Hatzenbuehler, J.; Pulling, T.J. Diagnosis and management of osteomyelitis. Am. Fam. Phys. 2011, 84, 1027–1033. [Google Scholar]
- Uskoković, V.; Desai, T.A. Nanoparticulate Drug Delivery Platforms for Advancing Bone Infection Therapies. Exp. Opin. Drug Del. 2014, 11, 1899–1912. [Google Scholar] [CrossRef] [PubMed]
- Uskoković, V. The role of hydroxyl channel in defining selected physicochemical peculiarities exhibited by hydroxyapatite. RSC Adv. 2015, 5, 36614–36633. [Google Scholar] [CrossRef] [PubMed]
- Habraken, W.; Habibovic, P.; Epple, M.; Bohner, M. Calcium phosphates in biomedical applications: Materials for the future? Mater. Today 2016, 19, 69–86. [Google Scholar] [CrossRef]
- Uskoković, V.; Desai, T.A. Calcium Phosphate Nanoparticles: A Future Therapeutic Platform for the Treatment of Osteomyelitis. Ther. Deliv. 2013, 4, 643–645. [Google Scholar]
- Uskoković, V.; Uskoković, D.P. Nanosized Hydroxyapatite and Other Calcium Phosphates: Chemistry of Formation and Application as Drug and Gene Delivery Agents. J. Biomed. Mat. Res. B 2011, 96, 152–191. [Google Scholar] [CrossRef] [PubMed]
- Rey, C.; Trombe, J.C.; Montel, G.J. Sur la fixation de la glycine dans le réseau des phosphates à structure d’apatite. J. Chem. Res. 1978, 188, 2401–2416. [Google Scholar]
- Rey, C.; Collins, B.; Shimizu, M.; Glimcher, M.J. Resolution-enhanced Fourier transform infrared spectroscopy study of the environment of phosphate ions in the early deposits of a solid phase of calcium-phosphate in bone and enamel, and their evolution with age. I: Investigations in the upsilon 4 PO4 domain. Calcif. Tissue Int. 1990, 46, 384–394. [Google Scholar] [PubMed]
- Cazalbou, S.; Combes, C.; Eichert, D.; Rey, C.; Glimcher, M.J. Poorly crystalline apatites: Evolution and maturation in vitro and in vivo. J. Bone Miner. Metab. 2004, 22, 310–314. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, M.; Sadaf, S.; Shahid, A. On the Formation of Hydroxyapatite Nano Crystals Prepared Using Cationic Surfactant. Mat. Res. 2015, 18, 468–472. [Google Scholar]
- Kawasaki, T.; Takahashi, S.; Ideda, K. Hydroxyapatite high-performance liquid chromatography: Column performance for proteins. Eur. J. Biochem. 1985, 152, 361–371. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, R.; Freitag, R. Isolation of a recombinant antibody from cell culture supernatant: Continuous annular versus batch and expanded-bed chromatography. Biotechnol. Bioeng. 2001, 73, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Saito, M.; Kurosawa, Y.; Okuyama, T. Scanning Electron Microscopy-Based Approach to Understand the Mechanism Underlying the Adhesion of Dengue Viruses on Ceramic Hydroxyapatite Columns. PLoS ONE 2013, 8, e53893. [Google Scholar] [CrossRef] [PubMed]
- Kazemzadeh-Narbat, M.; Noordin, S.; Masri, B.A.; Garbuz, D.S.; Duncan, C.P.; Hancock, R.E.; Wang, R. Drug release and bone growth studies of antimicrobial peptide-loaded calcium phosphate coating on titanium. J. Biomed. Mat. Res. B 2012, 100, 1344–1352. [Google Scholar] [CrossRef] [PubMed]
- Whitcup, S.M.; Robinson, M.R. Development of a dexamethasone intravitreal implant for the treatment of noninfectious posterior segment uveitis. Ann. N. Y. Acad. Sci. 2015, 1358, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bae, K.H.; Lee, F.; Xu, K.; Keng, C.T.; Tan, S.Y.; Tan, Y.J.; Chen, Q.; Kurisawa, M. Microstructured dextran hydrogels for burst-free sustained release of PEGylated protein drugs. Biomaterials 2015, 63, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Yerragunta, B.; Jogala, S.; Chinnala, K.M.; Aukunuru, J. Development of a novel 3-month drug releasing risperidone microspheres. J. Pharm. Bioallied. Sci. 2015, 7, 37–44. [Google Scholar] [PubMed]
- Uskoković, V.; Desai, T.A. Phase Composition Control of Calcium Phosphate Nanoparticles for Tunable Drug Delivery Kinetics and Treatment of Osteomyelitis. I. Preparation and Drug Release. J. Biomed. Mat. Res. A 2013, 101, 1416–1426. [Google Scholar] [CrossRef] [PubMed]
- Dorozhkin, S.V. Self-setting calcium orthophosphate formulations. J. Funct. Biomater. 2013, 4, 209–311. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Wu, V.M.; Pernal, S.; Uskoković, V. Self-Setting Calcium Phosphate Cements with Tunable Antibiotic Release Rates for Advanced Bone Graft Applications. ACS Appl. Mat. Interfaces 2016, 8, 7691–7708. [Google Scholar] [CrossRef] [PubMed]
- Klein, C.P.; van der Lubbe, H.B.; de Groot, K. A plastic composite of alginate with calcium phosphate granulate as implant material: An in vivo study. Biomaterials 1987, 8, 308–310. [Google Scholar] [PubMed]
- Dupraz, A.; Nguyen, T.P.; Richard, M.; Daculsi, G.; Passuti, N. Influence of a cellulosic ether carrier on the structure of biphasic calcium phosphate ceramic particles in an injectable composite material. Biomaterials 1999, 20, 663–673. [Google Scholar] [CrossRef]
- Sa, Y.; Yang, F.; Leeuwenburgh, S.C.; Wolke, J.G.; Ye, G.; de Wijn, J.R.; Jansen, J.A.; Wang, Y. Physicochemical properties and in vitro mineralization of porous polymethylmethacrylate cement loaded with calcium phosphate particles. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Verma, A.; Teja, B.V.; Pandey, G.; Mittapelly, N.; Trivedi, R.; Mishra, P.R. An insight into functionalized calcium based inorganic nanomaterials in biomedicine: Trends and transitions. Colloids Surf. B Biointerfaces 2015, 133, 120–139. [Google Scholar] [CrossRef] [PubMed]
- Maitra, A. Calcium phosphate nanoparticles: Second-generation nonviral vectors in gene therapy. Expert Rev Mol Diagn. 2005, 5, 893–905. [Google Scholar] [CrossRef] [PubMed]
- Jun, W.; Lin, L.; Cai, Y.; Yao, J. Recent advances of calcium phosphate nanoparticles for controlled drug delivery. Min. Rev. Med. Chem. 2013, 13, 1501–1507. [Google Scholar] [CrossRef]
- Mostaghaci, B.; Loretz, B.; Lehr, C.-M. Calcium phosphate system for gene delivery: Historical background and emerging opportunities. Curr. Pharm. Des. 2016, 22, 1529–1533. [Google Scholar] [CrossRef] [PubMed]
- Nichols, B.J.; Lippincott-Schwartz, J. Endocytosis without clathrin coats. Trends Cell Biol. 2011, 11, 406–412. [Google Scholar] [CrossRef]
- Olton, D.Y.E.; Close, J.M.; Sfeir, C.S.; Kumta, P.N. Intracellular trafficking pathways involved in the gene transfer of nano-structured calcium phosphate-DNA particles. Biomaterials 2011, 32, 7662–7670. [Google Scholar] [CrossRef] [PubMed]
- Loyter, A.; Scangos, G.; Juricek, D.; Keene, D.; Ruddle, F.H. Mechanisms of DNA entry into mammalian cells. II. Phagocytosis of calcium phosphate DNA co-precipitate visualized by electron microscopy. Exp. Cell Res. 1982, 139, 223–234. [Google Scholar] [CrossRef]
- Gopalakrishnan, B.; Wolff, J. siRNA and DNA Transfer to Cultured Cells. Methods Mol. Biol. 2009, 480, 31–52. [Google Scholar] [PubMed]
- Orrantia, E.; Chang, P.L. Intracellular distribution of DNA internalized through calcium phosphate precipitation. Exp. Cell. Res. 1990, 190, 170–174. [Google Scholar] [CrossRef]
- O’Neill, W.C. The fallacy of the calcium-phosphorus product. Kidney Int. 2007, 72, 792–796. [Google Scholar] [CrossRef] [PubMed]
- Sokolova, V.; Epple, M. Inorganic Nanoparticles as Carriers of Nucleic Acids into Cells. Angew. Chem. Int. Ed. 2008, 47, 1382–1395. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Wu, V.M.; Ghosh, S.; Uskoković, V. Gene Delivery Using Calcium Phosphate Nanoparticles: Optimization of the Transfection Process and the Effects of Citrate and Poly(l-Lysine) as Additives. J. Colloid Interface Sci. 2016, 471, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Upadhye, K.; Kumta, P.N. Nano-Sized Calcium Phosphate (CaP) Carriers for Non-Viral Gene Deilvery. Mater. Sci. Eng. B Adv. Funct. Solid State Mater. 2012, 177, 289–302. [Google Scholar] [CrossRef]
- Lee, M.S.; Lee, J.E.; Byun, E.; Kim, N.W.; Lee, K.; Lee, H.; Sim, S.J.; Lee, D.S.; Jeong, J.H. Target-specific delivery of siRNA by stabilized calcium phosphate nanoparticles using dopa-hyaluronic acid conjugate. J. Control. Release 2014, 192, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Khameneh, B.; Diab, R.; Ghazvini, K.; Bazzaz, B. Breakthroughs in bacterial resistance mechanisms and the potential ways to combat them. Microb. Pathogen. 2016, 95, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Bayles, K.W.; Wesson, C.A.; Liou, L.W.; Fox, L.K.; Bohach, G.A.; Trumble, W.R. Intracellular Staphylococcus aureus escapes the endosome and induces apoptosis in epithelial cells. Infect. Immun. 1998, 66, 336–342. [Google Scholar] [PubMed]
- Ellington, J.K.; Harris, M.; Webb, L.; Smith, B.; Smith, T.; Tan, K.; Hudson, M. Intracellular Staphylococcus aureus: A Mechanism for the Indolence of Osteomyelitis. J. Bone Jt. Surg. 2003, 85B, 918–921. [Google Scholar]
- Bost, K.L.; Ramp, W.K.; Nicholson, N.C.; Bento, J.L.; Marriott, I.; Hudson, M.C. Staphylococcus aureus Infection of Mouse or Human Osteoblasts Induces High Levels of Interleukin-6 and Interleukin-12 Production. J. Infect. Dis. 1999, 180, 1912–1920. [Google Scholar] [CrossRef] [PubMed]
- Lemaire, S.; van Bambeke, F.; Pierard, D.; Appelbaum, P.C.; Tulkens, P.M. Activity of Fusidic Acid against Extracellular and Intracellular Staphylococcus aureus: Influence of pH and Comparison with Linezolid and Clindamycin. Clin. Infect. Dis. 2011, 52, S493–S503. [Google Scholar] [CrossRef] [PubMed]
- Uskoković, V.; Desai, T.A. Simultaneous Bactericidal and Osteogenic Effect of Nanoparticulate Calcium Phosphate Powders Loaded with Clindamycin on Osteoblasts Infected with Staphylococcus Aureus. Mater. Sci. Eng. C 2014, 37, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, R.; Patra, M.; Dutta, D.; Banik, M.; Basu, T. Tetracycline-Entrapped Calcium Phosphate Nanoparticle (Tet-CPNP): Rejuvenation of an Obsolete Antibiotic to Further Action. Biochim. Biophys. Acta 2016, in press. [Google Scholar]
- Sommerfeldt, D.W.; Rubin, C.T. Biology of bone and how it orchestrates the form and function of the skeleton. Eur. Spine J. 2001, 10, S86–S95. [Google Scholar] [PubMed]
- Rey, C.; Combes, C.; Drouet, C.; Sfihi, H. Chemical diversity of apatites. Adv. Sci. Technol. 2006, 49, 27–36. [Google Scholar] [CrossRef]
- Cummings, L.J.; Snyder, M.A.; Brisack, K. Protein chromatography on hydroxyapatite columns. Methods Enzymol. 2009, 463, 387–404. [Google Scholar] [PubMed]
- Giovannini, R.; Freitag, R. Comparison of different types of ceramic hydroxyapatite for the chromatographic separation of plasmid DNA and a recombinant anti-Rhesus D antibody. Bioseparation 2001, 9, 359–368. [Google Scholar] [CrossRef]
- Oliva, J.; De Pablo, J.; Cortina, J.-L.; Cama, J.; Ayora, C. Removal of cadmium, copper, nickel, cobalt and mercury from water by Apatite IITM: Column experiments. J. Hazard. Mater. 2011, 194, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Smičiklas, I.; Dimović, S.; Plećaš, I.; Mitrić, M. Removal of Co2+ from aqueous solutions by hydroxyapatite. Water Res. 2006, 40, 2267–2274. [Google Scholar] [CrossRef] [PubMed]
- Wopenka, B.; Pasteris, J.D. A mineralogical perspective on the apatite in bone. Mater. Sci. Eng. C 2005, 25, 131–143. [Google Scholar] [CrossRef]
- Leventouri, T. Synthetic and biological hydroxyapatites: Crystal structure questions. Biomaterials 2006, 27, 3339–3342. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Valencia, C.; López-Álvarez, M.; Cochón-Cores, B.; Pereiro, I.; Serra, J.; González, P. Novel selenium-doped hydroxyapatite coatings for biomedical applications. J. Biomed. Mater. Res. A 2013, 101, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Pizzala, H.; Caldarelli, S.; Eon, J.G.; Rossi, A.M.; San Gil, R.A.; Laurencin, D.; Smith, M.E. A solid-state NMR study of lead and vanadium substitution into hydroxyapatite. J. Am. Chem. Soc. 2009, 131, 5145–5152. [Google Scholar] [CrossRef] [PubMed]
- Morgan, T.T.; Goff, T.M.; Adair, J.H. The colloidal stability of fluorescent calcium phosphosilicate nanoparticles: The effects of evaporation and redispersion on particle size distribution. Nanoscale 2011, 3, 2044–2053. [Google Scholar] [CrossRef] [PubMed]
- Mayer, I.; Berger, U.; Markitziu, A.; Gedalia, I. The uptake of lithium ions by synthetic carbonated hydroxyapatite. Calcif. Tissue Int. 1986, 38, 293–295. [Google Scholar] [CrossRef] [PubMed]
- Selvakumar, M.; Srivastava, P.; Pawar, H.S.; Francis, N.K.; Das, B.; Sathishkumar, G.; Subramanian, B.; Jaganathan, S.K.; George, G.; Anandhan, S.; et al. On-Demand Guided Bone Regeneration with Microbial Protection of Ornamented SPU Scaffold with Bismuth-doped Single Crystalline Hydroxyapatite: Augmentation and Cartilage Formation. ACS Appl. Mater. Interfaces 2016, 8, 4086–4100. [Google Scholar] [CrossRef] [PubMed]
- Bulanov, E.N.; Wang, J.; Knyazev, A.V.; White, T.; Manyakina, M.E.; Baikie, T.; Lapshin, A.N.; Dong, Z. Structure and Thermal Expansion of Calcium-Thorium Apatite, [Ca4]F[Ca2Th4]T[(SiO4)6]O2. Inorg. Chem. 2015, 54, 11356–11361. [Google Scholar] [CrossRef] [PubMed]
- Chatelain, G.; Bourgeois, D.; Ravaux, J.; Averseng, O.; Vidaud, C.; Meyer, D. Incorporation of uranium into a biomimetic apatite: Physicochemical and biological aspects. J. Biol. Inorg. Chem. 2015, 20, 497–507. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Lorenzo, L.M.; Hart, J.N.; Gross, K.A. Influence of fluorine in the synthesis of apatites. Synthesis of solid solutions of hydroxy-fluorapatite. Biomaterials 2003, 24, 3777–3785. [Google Scholar] [CrossRef]
- Kubota, T.; Nakamura, A.; Toyoura, K.; Matsunaga, K. The effect of chemical potential on the thermodynamic stability of carbonate ions in hydroxyapatite. Acta Biomater. 2014, 10, 3716–3722. [Google Scholar] [CrossRef] [PubMed]
- Hasna, K.; Kumar, S.S.; Komath, M.; Varma, M.R.; Jayaraj, M.K.; Kumar, K.R. Synthesis of chemically pure, luminescent Eu3+ doped HAp nanoparticles: A promising fluorescent probe for in vivo imaging applications. Phys. Hem. Chem. Phys. 2013, 15, 8106–8111. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Liu, M.; Hui, J.; Fan, D.; Ma, H.; Zhang, X.; Wang, Y.; Wei, Y. Ln3+-doped hydroxyapatite nanocrystals: Controllable synthesis and cell imaging. Phys. Chem. Chem. Phys. 2015, 17, 20301–20307. [Google Scholar] [CrossRef] [PubMed]
- Wiglusz, R.J.; Drulis-Kawa, Z.; Pazik, R.; Zawisza, K.; Dorotkiewicz-Jach, A.; Roszkowiak, J.; Nedelec, J.M. Multifunctional Lanthanide and Silver Ion Co-Doped Nano-Chlorapatites with Combined Spectroscopic and Antimicrobial Properties. Dalton Trans. 2015, 44, 6918–6925. [Google Scholar] [CrossRef] [PubMed]
- Ahmadzadeh, E.; Talebnia, F.; Tabatabaei, M.; Ahmadzadeh, H.; Mostaghaci, B. Osteoconductive composite graft based on bacterial synthesized hydroxyapatite nanoparticles doped with different ions: From synthesis to in vivo studies. Nanomed. Nanotechnol. Biol. Med. 2016. [Google Scholar] [CrossRef] [PubMed]
- Kolmas, J.; Groszyk, E.; Piotrowska, U. Nanocrystalline hydroxyapatite enriched in selenite and manganese ions: Physicochemical and antibacterial properties. Nanoscale Res. Lett. 2015, 10, 989. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; He, W.; Li, F.; Perera, T.S.; Gan, L.; Han, Y.; Wang, X.; Li, S.; Dai, H. Luminescence Enhanced Eu3+/Gd3+ Co-Doped Hydroxyapatite Nanocrystals as Imaging Agents in Vitro and in Vivo. ACS Appl. Mater. Interfaces 2016, in press. [Google Scholar] [CrossRef] [PubMed]
- Ignjatović, N.; Ajduković, Z.; Savić, V.; Najman, S.; Mihailović, D.; Vasiljević, P.; Stojanović, Z.; Uskoković, V.; Uskoković, D. Nanoparticles of cobalt-substituted hydroxyapatite in regeneration of mandibular osteoporotic bones. J. Mater. Sci. Mater. Med. 2013, 24, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Tampieri, A.; D’Alessandro, T.; Sandri, M.; Sprio, S.; Landi, E.; Bertinetti, L.; Panseri, S.; Pepponi, G.; Goettlicher, J.; Bañobre-López, M.; et al. Intrinsic magnetism and hyperthermia in bioactive Fe-doped hydroxyapatite. Acta Biomater. 2012, 8, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.; Bianchi, M.; Sartori, M.; Parrilli, A.; Panseri, S.; Ortolani, A.; Sandri, M.; Boi, M.; Salter, D.M.; Maltarello, M.C.; et al. Magnetic forces and magnetized biomaterials provide dynamic flux information during bone regeneration. J. Mater. Sci. Mater. Med. 2016, 27, 51. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.J.; Summers, N.J.; Cook, E.A. Healing in the new millennium: Bone stimulators: An overview of where we’ve been and where we may be heading. Clin. Pediatr. Med. Surg. 2015, 32, 45–59. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Xiao, B.; Zhang, Y.; Liu, J.; Xue, H.; Lei, J.; Kong, H.; Huang, Y.; Jin, Z.; Gu, N.; et al. Super-paramagnetic responsive nanofibrous scaffolds under static magnetic field enhance osteogenesis for bone repair in vivo. Sci. Rep. 2013, 3, 2655. [Google Scholar] [CrossRef] [PubMed]
- Tran, P.L.; Hammond, A.A.; Mosley, T.; Cortez, J.; Gray, T.; Colmer-Hamood, J.A.; Shashtri, M.; Spallholz, J.E.; Hamood, A.N.; Reid, T.W. Organoselenium coating on cellulose inhibits the formation of biofilms by Pseudomonas aeruginosa and Staphylococcus aureus. Appl. Environ. Microbiol. 2009, 75, 3586–3592. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Hao, H.; Li, Y.; Zhang, S. Selenium-substituted hydroxyapatite nanoparticles and their in vivo antitumor effect on hepatocellular carcinoma. Colloids Surf. B Biointerfaces 2016, 140, 297–306. [Google Scholar]
- Tran, A.; Sarin, L.; Hurt, R.H.; Webster, T.J. Differential effects of nanoselenium doping on healthy and cancerous osteoblasts in coculture on titanium. Int. J. Nanomed. 2010, 5, 351–358. [Google Scholar]
- Chen, X.; Cai, K.; Fang, J.; Lai, M.; Hou, Y.; Li, J.; Luo, Z.; Hu, Y.; Tang, L. Fabrication of selenium-deposited and chitosan-coated titania nanotubes with anticancer and antibacterial properties. Colloids Surf B Biointerfaces 2013, 103, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Perez, R.A.; Mestres, G. Role of pore size and morphology in musculo-skeletal tissue regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 61, 922–939. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Fernandes, H.; Habibovic, P.; de Boer, J.; Barradas, A.M.C.; de Ruiter, A.; Walsh, W.R.; van Blitterswijk, C.A.; de Brujin, J.D. Osteoinductive ceramics as a synthetic alternative to autologous bone grafting. Proc. Natl. Acad. Sci. USA 2010, 107, 13614–13619. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.H.K.; Burguera, E.F.; Carey, L.E. Strong, macroporous, and in situ-setting calcium phosphate cement-layered structures. Biomaterials 2007, 28, 3786–3796. [Google Scholar] [CrossRef] [PubMed]
- Garagiola, U.; Grigolato, R.; Soldo, R.; Bacchini, M.; Bassi, G.; Roncucci, R.; de Nardi, S. Computer-aided design/computer-aided manufacturing of hydroxyapatite scaffolds for bone reconstruction in jawbone atrophy: A systematic review and case report. Maxillofac. Plast. Reconstr. Surg. 2016, 38, 2. [Google Scholar] [CrossRef] [PubMed]
- Rosa, A.L.; de Oliveira, P.T.; Beloti, M.M. Macroporous scaffolds associated with cells to construct a hybrid biomaterial for bone tissue engineering. Expert Rev. Med. Devices 2008, 5, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Pilliar, R.M.; Filiaggi, M.J.; Wells, J.D.; Grynpas, M.D.; Kandel, R.A. Porous calcium polyphosphate scaffolds for bone substitute applications—In vitro characterization. Biomaterials 2001, 22, 963–972. [Google Scholar] [CrossRef]
- Deville, S.; Saiz, E.; Tomsia, A.P. Freeze casting of hydroxyapatite scaffolds for bone tissue engineering. Biomaterials 2006, 27, 5480–5489. [Google Scholar] [CrossRef] [PubMed]
- Uskoković, V. Amelogenin in Enamel Tissue Engineering. Adv. Exp. Med. Biol. 2015, 881, 237–254. [Google Scholar] [PubMed]
- Yao, H.-B.; Ge, J.; Mao, L.-B.; Yan, Y.-X.; Yu, S.-H. 25th Anniversary Article: Artificial Carbonate Nanocrystals and Layered Structural Nanocomposites Inspired by Nacre: Synthesis, Fabrication and Applications. Adv. Mater. 2014, 26, 163–188. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, H.; Tamai, N.; Murase, T.; Myoui, A. Interconnected porous hydroxyapatite ceramics for bone tissue engineering. J. R. Soc. Interface 2009, 6, S341–S348. [Google Scholar] [CrossRef] [PubMed]
- Almirall, A.; Larrecq, G.; Delgado, J.; Martınez, S.; Planell, J.; Ginebra, M.P. Fabrication of low temperature macroporous hydroxyapatite scaffolds by foaming and hydrolysis of an α-TCP paste. Biomaterials 2004, 25, 3671–3680. [Google Scholar] [CrossRef] [PubMed]
- Warnke, P.H.; Seitz, H.; Warnke, F.; Becker, S.T.; Sivananthan, S.; Sherry, E.; Liu, Q.; Wiltfang, J.; Douglas, T. Ceramic scaffolds produced by computer-assisted 3D printing and sintering: Characterization and biocompatibility investigations. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 93, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Miguel, C.; Claus, M.; Andrea, E.; Uwe, G.; Jürgen, G.; Inês, P.; Jörg, T.; Elke, V. Direct 3D powder printing of biphasic calcium phosphate scaffolds for substitution of complex bone defects. Biofabrication 2014, 6, 015006. [Google Scholar]
- Seitz, H.; Rieder, W.; Irsen, S.; Leukers, B.; Tille, C. Three-dimensional printing of porous ceramic scaffolds for bone tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 74, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Uskoković, V.; Lee, K.; Lee, P.P.; Fischer, K.E.; Desai, T.A. Shape effect in the design of nanowire-coated microparticles as transepithelial drug delivery devices. ACS Nano 2012, 6, 7832–7841. [Google Scholar] [CrossRef] [PubMed]
- Dalby, M.J.; Gadegaard, N.; Tare, R.; Andar, A.; Riehle, M.O.; Herzyk, P.; Wilkinson, C.D.W.; Oreffo, R.O.C. The Control of Human Mesenchymal Cell Differentiation Using Nanoscale Symmetry and Disorder. Nat. Mater. 2007, 6, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Kirkham, J.; Brookes, S.J.; Shore, R.C.; Wood, S.R.; Smith, D.A.; Zhang, J.; Chen, H.; Robinson, C. Physico-chemical properties of crystal surfaces in matrix-mineral interactions during mammalian biomineralisation. Curr. Opin. Coll. Interface Sci. 2002, 7, 124–132. [Google Scholar] [CrossRef]
- Covani, U.; Giacomelli, L.; Krajewski, A.; Ravaglioli, A.; Spotorno, L.; Loria, P.; Das, S.; Nicolini, C. Biomaterials for orthopedics: A roughness analysis by atomic force microscopy. J. Biomed. Mater. Res. A 2007, 82, 723–730. [Google Scholar] [CrossRef] [PubMed]
- Gross, K.A.; Muller, D.; Lucas, H.; Haynes, D.R. Osteoclast resorption of thermal spray hydoxyapatite coatings is influenced by surface topography. Acta Biomater. 2012, 8, 1948–1956. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Kurashina, K.; de Bruijn, J.D.; Li, Y.; de Groot, K.; Zhang, X. A preliminary study on osteoinduction of two kinds of calcium phosphate ceramics. Biomaterials 1999, 20, 1799–1806. [Google Scholar] [CrossRef]
- Klein, C.P.; de Groot, K.; Driessen, A.A.; van der Lubbe, H.B. Interaction of biodegradable beta-whitlockite ceramics with bone tissue: An in vivo study. Biomaterials 1985, 6, 189–192. [Google Scholar] [CrossRef]
- Kumar, A.; Nune, K.C.; Misra, R.D.K. Biological functionality of extracellular matrix-ornamented three-dimensional printed hydroxyapatite scaffolds. J. Biomed. Mater. Res. A 2016. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Su, J.; Wei, J.; Kong, H.; Liu, C. Biocompatibility and osteogenicity of degradable Ca-deficient hydroxyapatite scaffolds from calcium phosphate cement for bone tissue engineering. Acta Biomater. 2009, 5, 268–278. [Google Scholar] [CrossRef] [PubMed]
- LeGeros, R.Z. Properties of osteoconductive biomaterials: Calcium phosphates. Clin. Orthop. 2002, 395, 81–98. [Google Scholar] [CrossRef] [PubMed]
- Mistry, A.S.; Mikos, A.G. Tissue Engineering Strategies for Bone Regeneration. Adv. Biochem. Eng. Biotechnol. 2005, 94, 1–22. [Google Scholar] [PubMed]
- Uskoković, V.; Desai, T.A. Phase Composition Control of Calcium Phosphate Nanoparticles for Tunable Drug Delivery Kinetics and Treatment of Osteomyelitis. II. Antibacterial and Osteoblastic Response. J. Biomed. Mater. Res. A 2013, 101, 1427–1436. [Google Scholar] [PubMed]
- Teti, G.; Salvatore, V.; Focaroli, S.; Durante, S.; Mazzotti, A.; Dicarlo, M.; Mattioli-Belmonte, M.; Orsini, G. In vitro osteogenic and odontogenic differentiation of human dental pulp stem cells seeded on carboxymethyl cellulose-hydroxyapatite hybrid hydrogel. Front. Physiol. 2015, 6, 297. [Google Scholar] [PubMed]
- Niu, C.C.; Lin, S.S.; Chen, W.J.; Liu, S.J.; Chen, L.H.; Yang, C.Y.; Wang, C.J.; Yuan, L.J.; Chen, P.H.; Cheng, H.Y. Benefits of biphasic calcium phosphate hybrid scaffold-driven osteogenic differentiation of mesenchymal stem cells through upregulated leptin receptor expression. J. Orthop. Surg. Res. 2015, 10, 111. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Wang, G.; Fan, H.; Wang, X.; Lu, J.; Zhang, X. Expression of core binding factor 1 and osteoblastic markers in C2C12 cells induced by calcium phosphate ceramics in vitro. J. Biomed. Mater. Res. A 2007, 82, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Rupani, A.; Hidalgo-Bastida, L.A.; Rutten, F.; Dent, A.; Turner, I.; Cartmell, S. Osteoblast activity on carbonated hydroxyapatite. J. Biomed. Mater. Res. A 2012, 100, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Song, J.H.; Kim, J.H.; Park, S.; Kang, W.; Kim, H.W.; Kim, H.E.; Jang, J.H. Signaling responses of osteoblast cells to hydroxyapatite: The activation of ERK and SOX9. J. Bone Miner. Metabol. 2008, 26, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Lock, J.; Liu, H. Nanomaterials enhance osteogenic differentiation of human mesenchymal stem cells similar to a short peptide of BMP-7. Int. J. Nanomed. 2011, 6, 2769–2777. [Google Scholar]
- Tazi, N.; Zhang, Z.; Messaddeq, Y.; Almeida-Lopes, L.; Zanardi, L.M.; Levinson, D.; Rouabhia, M. Hydroxyapatite bioactivated bacterial cellulose promotes osteoblast growth and the formation of bone nodules. AMB Express 2012, 2, 61. [Google Scholar] [CrossRef] [PubMed]
- Johansson, P.; Jimbo, R.; Naito, Y.; Kjellin, P.; Currie, F.; Wennerberg, A. Polyether ether ketone implants achieve increased bone fusion when coated with nano-sized hydroxyapatite: A histomorphometric study in rabbit bone. Int. J. Nanomed. 2016, 11, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhang, D.; Hu, Z.; Cheng, J.; Zhuo, C.; Fang, X.; Xing, Y. MicroRNA-26a-modified adipose-derived stem cells incorporated with a porous hydroxyapatite scaffold improve the repair of bone defects. Mol. Med. Rep. 2015, 12, 3345–3350. [Google Scholar] [CrossRef] [PubMed]
- Guarino, V.; Veronesi, F.; Marrese, M.; Giavaresi, G.; Ronca, A.; Sandri, M.; Tampieri, A.; Fini, M.; Ambrosio, L. Needle-like ion-doped hydroxyapatite crystals influence osteogenic properties of PCL composite scaffolds. Biomed. Mater. 2016, 11, 015018. [Google Scholar] [CrossRef] [PubMed]
- Hatakeyama, W.; Taira, M.; Chosa, N.; Kihara, H.; Ishisaki, A.; Kondo, H. Effects of apatite particle size in two apatite/collagen composites on the osteogenic differentiation profile of osteoblastic cells. Int. J. Mol. Med. 2013, 32, 1255–1261. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhou, G.; Zheng, L.; Liu, H.; Niu, X.; Fan, Y. Micro-/nano- sized hydroxyapatite directs differentiation of rat bone marrow derived mesenchymal stem cells towards an osteoblast lineage. Nanoscale 2012, 4, 2484–2490. [Google Scholar] [CrossRef] [PubMed]
- Liang, L.H.; Liu, D.; Jiang, Q. Size-dependent continuous binary solution phase diagram. Nanotechnology 2003, 14, 438–442. [Google Scholar] [CrossRef]
- Fan, Q.; Wang, Y.E.; Zhao, X.; Loo, J.S.; Zuo, Y.Y. Adverse biophysical effects of hydroxyapatite nanoparticles on natural pulmonary surfactant. ACS Nano 2011, 5, 6410–6416. [Google Scholar] [CrossRef] [PubMed]
- Tannoury, C.A.; An, H.S. Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J. 2014, 14, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Wang, Y.P.; Liu, F.X.; Zeng, K.; Qian, M.Q.; Chen, G.; Shi, L.; Zhu, G.X. Increased invasiveness of osteosarcoma mesenchymal stem cells induced by bone-morphogenetic protein-2. In Vitro Cell Dev. Biol. Anim. 2013, 49, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Eguchi, Y.; Wakitani, S.; Imai, Y.; Naka, Y.; Hashimoto, Y.; Nakamura, H.; Takaoka, K. Antitumor necrotic factor agent promotes BMP-2-induced ectopic bone formation. J. Bone Miner. Metab. 2010, 28, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Francis, M.D.; Russell, R.G.; Fleisch, H. Diphosphonates inhibit hydroxyapatite dissolution in vitro and bone resorption in tissue culture and in vivo. Science 1969, 165, 1262–1264. [Google Scholar]
- Leu, C.T.; Luegmayr, E.; Freedman, L.P.; Rodan, G.A.; Reszka, A.A. Relative binding affinities of bisphosphonates for human bone and relationship to antiresorptive efficacy. Bone 2006, 38, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Stražić-Geljić, I.; Melis, N.; Boukhechba, F.; Schaub, S.; Mellier, C.; Janvier, P.; Laugier, J.-P.; Bouler, J.-M.; Verron, E.; Scimeca, J.-C. Incorporation of gallium enhances reconstructive properties of a calcium phosphate bone substitute. Acta Biomater. 2016, in press. [Google Scholar]
- Davison, N.L.; Su, J.; Yuan, H.; van den Beucken, J.J.; de Bruijn, J.D.; Barrère-de Groot, F. Influence of surface microstructure and chemistry on osteoinduction and osteoclastogenesis by biphasic calcium phosphate discs. Eur. Cell. Mater. 2015, 29, 314–329. [Google Scholar] [PubMed]
- Jiao, K.; Niu, L.N.; Li, Q.H.; Chen, F.M.; Zhao, W.; Li, J.J.; Chen, J.H.; Cutler, C.W.; Pashley, D.H.; Tay, F.R. Biphasic silica/apatite co-mineralized collagen scaffolds stimulate osteogenesis and inhibit RANKL-mediated osteoclastogenesis. Acta Biomater. 2015, 19, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Costa-Rodrigues, J.; Silva, A.; Santos, C.; Almeida, M.M.; Costa, M.E.; Fernandes, M.H. Complex effect of hydroxyapatite nanoparticles on the differentiation and functional activity of human pre-osteoclastic cells. J. Biomed. Nanotechnol. 2014, 10, 3590–3600. [Google Scholar] [CrossRef] [PubMed]
- Shiwaku, Y.; Neff, L.; Nagano, K.; Takeyama, K.; de Bruijn, J.; Dard, M.; Gori, F.; Baron, R. The Crosstalk between Osteoclasts and Osteoblasts Is Dependent upon the Composition and Structure of Biphasic Calcium Phosphates. PLoS ONE 2015, 10, e0132903. [Google Scholar] [CrossRef] [PubMed]
- Theuretzbacher, U. Accelerating resistance, inadequate antibacterial drug pipelines and international responses. Int. J. Antimicrob. Agents 2012, 39, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Oktar, F.N.; Yetmez, M.L.; Ficai, D.; Ficai, A.; Dumitru, F.; Pica, A. Molecular mechanism and targets of the antimicrobial activity of metal nanoparticles. Curr. Top. Med. Chem. 2015, 15, 1583–1588. [Google Scholar] [CrossRef] [PubMed]
- Domingo-Calap, P.; Georgel, P.; Bahram, S. Back to the future: Bacteriophages as promising therapeutic tools. HLA 2016, 87, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Mojsoska, B.; Jenssen, H. Peptides and Peptidomimetics for Antimicrobial Drug Design. Pharmaceuticals 2015, 8, 366–415. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Zheng, J.; Tang, X.; Goering, P.L. Silver Nanoparticle-Induced Autophagic-Lysosomal Disruption and NLRP3-Inflammasome Activation in HepG2 Cells is Size-Dependent. Toxicol. Sci. 2016, in press. [Google Scholar] [CrossRef] [PubMed]
- Gliga, A.R.; Skoglund, S.; Wallinder, I.O.; Fadeel, B.; Karlsson, H.L. Size-dependent cytotoxicity of silver nanoparticles in human lung cells: The role of cellular uptake, agglomeration and Ag release. Part. Fibre Toxicol. 2014, 11, 11. [Google Scholar] [CrossRef] [PubMed]
- Avalos, A.; Haza, A.I.; Mateo, D.; Morales, P. Cytotoxicity and ROS production of manufactured silver nanoparticles of different sizes in hepatoma and leukemia cells. J. Appl. Toxicol. 2014, 34, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, A.S. Phage therapy—Constraints and possibilities. Ups. J. Med. Sci. 2014, 119, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Lohan, S.; Bisht, G.S. Recent approaches in design of peptidomimetics for antimicrobial drug discovery research. Min. Rev. Med. Chem. 2013, 13, 1073–1088. [Google Scholar] [CrossRef]
- Gupta, P.; Sarkar, S.; Das, B.; Bhattacharjee, S.; Tribedi, P. Biofilm, pathogenesis and prevention—A journey to break the wall: A review. Arch. Microbiol. 2016, 198, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Richards, J.J.; Melander, C. Small Molecule Approaches toward the Non-Microbicidal Modulation of Bacterial Biofilm Growth and Maintenance. Anti-Inf. Agents Med. Chem. 2009, 8, 295–314. [Google Scholar] [CrossRef]
- Wu, H.; Moser, C.; Wang, H.Z.; Høiby, N.; Song, Z.J. Strategies for combating bacterial biofilm infections. Int. J. Oral Sci. 2015, 7, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Goyal, A.K.; Khatri, K.; Mishra, N.; Mehta, A.; Vaidya, B.; Tiwari, S.; Paliwal, R.; Paliwal, S.; Vyas, S.P. Development of self-assembled nanoceramic carrier construct(s) for vaccine delivery. J. Biomater. Appl. 2009, 24, 65–84. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Moguche, A.O.; Chiu, D.; Murali-Krishna, K.; Baneyx, F. Just-in-time vaccines: Biomineralized calcium phosphate core-immunogen shell nanoparticles induce long-lasting CD8(+) T cell responses in mice. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Kozlova, D.; Sokolova, V.; Zhong, M.; Zhang, E.; Yang, J.; Li, W.; Yang, Y.; Buer, J.; Westendorf, A.M.; Epple, M.; et al. Calcium phosphate nanoparticles show an effective activation of the innate immune response in vitro and in vivo after functionalization with flagellin. Virol. Sin. 2014, 29, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kim, W.Y.; Huang, L. Systemic delivery of gemcitabine triphosphate via LCP nanoparticles for NSCLC and pancreatic cancer therapy. Biomaterials 2013, 34, 3447–3458. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Wu, X.; Nakanishi, H.; Yamamoto, Y.; Uemura, M.; Hata, T.; Nishimura, J.; Takemasa, I.; Mizushima, T.; Sasaki, J.; et al. A glucose carbonate apatite complex exhibits in vitro and in vivo anti-tumour effects. Sci. Rep. 2015, 5, 7742. [Google Scholar] [CrossRef] [PubMed]
- Venkatasubbu, G.D.; Ramasamy, S.; Reddy, G.P.; Kumar, J. In vitro and in vivo anticancer activity of surface modified paclitaxel attached hydroxyapatite and titanium dioxide nanoparticles. Biomed. Microdevices 2013, 15, 711–726. [Google Scholar] [CrossRef] [PubMed]
- Kawai, K.; Larson, B.J.; Ishise, H.; Carre, A.L.; Nishimoto, S.; Longaker, M.; Lorenz, H.P. Calcium-based nanoparticles accelerate skin wound healing. PLoS ONE 2011, 6, e27106. [Google Scholar] [CrossRef] [PubMed]
- Pouget, E.M.; Bomans, P.H.H.; Goos, J.A.C.M.; Frederik, P.M.; de With, G.; Sommerdijk, N.A.J.M. The initial stages of template-controlled CaCO3 formation revealed by cryo-TEM. Science 2009, 323, 1455–1458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Onuma, K. Recent research on pseudobiological hydroxyapatite crystal growth and phase transition mechanisms. Prog. Cryst. Growth Charact. Mat. 2006, 52, 223–245. [Google Scholar] [CrossRef]
- Wu, V.M.; Uskoković, V. Is There a Relationship between Solubility and Resorbability of Different Calcium Phosphate Phases in vitro? Biochim. Biophys. Acta Gen. Subj. 2016, in press. [Google Scholar] [CrossRef] [PubMed]
- Uskoković, V.; Odsinada, R.; Djordjevic, S.; Habelitz, S. Dynamic Light Scattering and Zeta Potential of Colloidal Mixtures of Amelogenin and Hydroxyapatite in Calcium and Phosphate Rich Ionic Milieus. Arch. Oral Biol. 2011, 56, 521–532. [Google Scholar] [CrossRef] [PubMed]
- Pitek, A.S.; Wen, A.M.; Shukla, S.; Steinmetz, N.F. Nanomedicine: The Protein Corona of Plant Virus Nanoparticles Influences their Dispersion Properties, Cellular Interactions, and in Vivo Fates. Small 2016, 12, 1682. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Jiao, B.; Shi, X.; Valle, R.P.; Fan, Q.; Zuo, Y.Y. Physicochemical Properties of Nanoparticles Regulate Translocation across Pulmonary Surfactant Monolayer and Formation of Lipoprotein Corona. ACS Nano 2013, 7, 10525–10533. [Google Scholar] [CrossRef] [PubMed]
- Gamble, W. Atherosclerosis: The carbonic anhydrase, carbon dioxide, calcium concerted theory. J. Theor. Biol. 2006, 239, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Dorozhkin, S.V.; Epple, M. Biological and Medical Significance of Calcium Phosphates. Angew. Chem. Int. Ed. 2002, 41, 3130–3146. [Google Scholar] [CrossRef]
- Uskoković, V. Surface Charge Effects Involved in the Control of Stability of Sols Comprising Uniform Cholesterol Particles. Mat. Manuf. Process. 2008, 23, 620–623. [Google Scholar] [CrossRef]
- Liu, L.; Xiao, Z.; Xiao, Y.; Wang, Z.; Li, F.; Li, M.; Peng, X. Potential enhancement of intravenous nano-hydroxyapatite in high-intensity focused ultrasound ablation for treating hepatocellular carcinoma in a rabbit model. Oncol. Lett. 2014, 7, 1485–1492. [Google Scholar] [CrossRef] [PubMed]
- Barth, B.M.; Sharma, R.; Altinoğlu, E.I.; Morgan, T.T.; Shanmugavelandy, S.S.; Kaiser, J.M.; McGovern, C.; Matters, G.L.; Smith, J.P.; Kester, M.; et al. Bioconjugation of calcium phosphosilicate composite nanoparticles for selective targeting of human breast and pancreatic cancers in vivo. ACS Nano 2010, 4, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Bohner, M.; Baroud, G. Injectability of calcium phosphate pastes. Biomaterials 2005, 26, 1553–1563. [Google Scholar] [CrossRef] [PubMed]
- Orlovskii, V.P.; Komlev, V.S.; Barinov, S.M. Hydroxyapatite and Hydroxyapatite-Based Ceramics. Inorg. Mat. 2002, 38, 973–984. [Google Scholar] [CrossRef]
- Uskoković, V. Prospects and Pits on the Path of Biomimetics: The Case of Tooth Enamel. J. Biomimet. Biomat. Tissue Eng. 2010, 8, 45–78. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, E.F. Small Is Beautiful, 25th Anniversary Edition: Economics as If People Mattered: 25 Years Later with Commentaries; Hartley and Marks Publishers: Vancouver, BC, Canada, 2000. [Google Scholar]
- Liao, N. Combining Instrumental and Contextual Approaches: Nanotechnology and Sustainable Development. J. Law Med. Ethics 2009, 37, 781–789. [Google Scholar] [CrossRef] [PubMed]


| Class of Chemical | Chemical | Company | Price per Gram |
|---|---|---|---|
| Antibiotic | Gentamycin | Thermo Fisher | $110 |
| Vancomycin | Sigma Aldrich | $51.50 | |
| Ciprofloxacin | Alfa Aesar | $11.10 | |
| Growth factor | IGF-1 | Sigma Aldrich | $4,540,000 |
| TGF-β 1 | Alfa Aesar | $204,000,000 | |
| BMP-2 | Thermo Fisher | $12,000,000 | |
| BMP-4 | Thermo Fisher | $19,000,000 | |
| BMP-7 | Thermo Fisher | $19,000,000 | |
| Bisphosphonate | Alendronic acid | Sigma Aldrich | $1,690 |
| Zoledronic acid | Sigma Aldrich | $466.70 | |
| Pamidronic acid | Sigma Aldrich | $4812 | |
| Mineral compound | Calcium phosphate | Sigma Aldrich | $0.12 |
| Calcium phosphate | Alfa Aesar | $0.06 | |
| Drug release polymer | PLGA | Sigma Aldrich | $67.40 |
| PEO | Alfa Aesar | $0.71 | |
| PLLA | Sigma Aldrich | $45.00 | |
| Viscous polymer | Polyurethane injectables | Sigma Aldrich | $23.50 |
| PCL | Sigma Aldrich | $8.74 | |
| Chitosan | Alfa Aesar | $0.84 | |
| Hyaluronic acid | Sigma Aldrich | $26,700 | |
| Luminescent dye | Oxytetracycline | Sigma Aldrich | $1,632 |
| Calcein green | Thermo Fisher | $313,000 | |
| Alizarin red | Sigma Aldrich | $2.40 | |
| Xylenol orange | Sigma Aldrich | $41.00 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uskoković, V.; Wu, V.M. Calcium Phosphate as a Key Material for Socially Responsible Tissue Engineering. Materials 2016, 9, 434. https://doi.org/10.3390/ma9060434
Uskoković V, Wu VM. Calcium Phosphate as a Key Material for Socially Responsible Tissue Engineering. Materials. 2016; 9(6):434. https://doi.org/10.3390/ma9060434
Chicago/Turabian StyleUskoković, Vuk, and Victoria M. Wu. 2016. "Calcium Phosphate as a Key Material for Socially Responsible Tissue Engineering" Materials 9, no. 6: 434. https://doi.org/10.3390/ma9060434






