Teriparatide Therapy as an Adjuvant for Tissue Engineering and Integration of Biomaterials
Abstract
:1. Introduction
2. The ‘Need’ in Critical Sized Defects
3. The ‘Need’ in Impaired Fracture Healing
4. PTH Physiology
5. Teriparatide
Continuous vs. Intermittent Debate
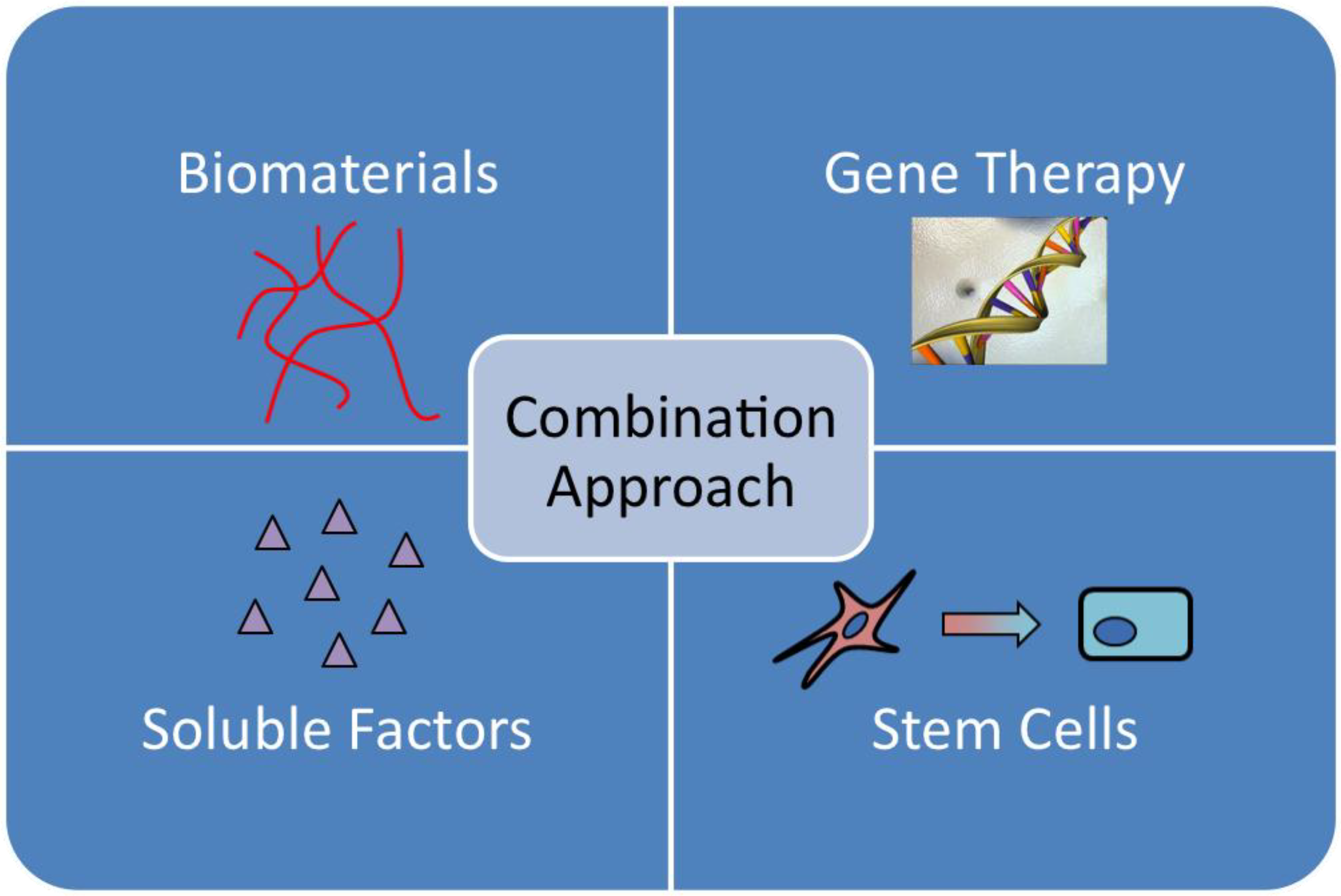
6. Current Approaches to Revitalize Bone Allografts
7. Advantages of Teriparatide Therapy in Treating Problematic Fractures
8. The Basic Science behind Teriparatide
9. The Prospect of PTH Therapy in Osseointegration—Experience from Animal Studies
10. The Prospect of PTH Therapy in Human Skeletal Repair—Evidence So Far
11. Biochemical Markers of PTH1–34 Therapy
12. Unresolved Issues and Future Directions
This Leads Us to Another Set of Questions Such As When to Start, What Dosage to Give, and for How Long Should the PTH1–34 Treatment Be Given?
13. Conclusions
Acknowledgements
References
- Zhang, X.P.; Xie, C.; Lin, A.S.P.; Ito, H.; Awad, H.; Lieberman, J.R.; Rubery, P.T.; Schwarz, E.M.; O'Keefe, R.J.; Guldberg, R.E. Periosteal progenitor cell fate in segmental cortical bone graft transplantations: implications for functional tissue engineering. J. Bone Miner. Res. 2005, 20(12), 2124–2137. [Google Scholar] [CrossRef]
- Foundation, O.C. Oral Cancer Facts. 2010. Available online: http://www.oralcancerfoundation.org/facts/index.htm (accessed on 6 May 2011).
- Stansbury, L.G.; Lalliss, S.J.; Branstetter, J.G.; Bagg, M.R.; Holcomb, J.B. Amputations in U.S. military personnel in the current conflicts in Afghanistan and Iraq. J. Orthop. Trauma 2008, 22(1), 43–46. [Google Scholar]
- Khan, S.N.; Cammisa, F.P., Jr.; Sandhu, H.S.; Diwan, A.D.; Girardi, F.P.; Lane, J.M. The biology of bone grafting. J. Am. Acad. Orthop. Surg. 2005, 13(1), 77–86. [Google Scholar]
- Beaver, R.; Brinker, M.R.; Barrack, R.L. An analysis of the actual cost of tibial nonunions. J. La. State Med. Soc. 1997, 149(6), 200–206. [Google Scholar]
- Xie, C.; Reynolds, D.; Awad, H.; Rubery, P.T.; Pelled, G.; Gazit, D.; Guldberg, R.E.; Schwarz, E.M.; O’Keefe, R.J.; Zhang, X. Structural bone allograft combined with genetically engineered mesenchymal stem cells as a novel platform for bone tissue engineering. Tissue Eng. 2007, 13(3), 435–445. [Google Scholar]
- Harada, S.; Rodan, G.A. Control of osteoblast function and regulation of bone mass. Nature 2003, 423(6937), 349–355. [Google Scholar] [CrossRef]
- Kronenberg, H.M.; Bringhurst, F.R.; Nussbaum, S.; Juppner, H.; Abou-Samra, A.B.; Segre, G.V.; Potts, J.T., Jr. Parathyroid hormone: biosynthesis, secretion, chemistry, and action. In Handbook of Experimental Pharmacology: Physiology and Pharmacology of Bone; Mundy, G.R., Martin, T.J., Heidelberg, M., Eds.; Springer-Verlag KG: Heidelberg, Germany, 1993; pp. 185–201. [Google Scholar]
- Potts, J.T., Jr.; Juppner, H. Parathyroid Hormone and Parathyroid Hormone-Related Peptide in Calcium Homeostasis, Bone Metabolism, and Bone Development: The Proteins, Their Genes, and Receptors. In Metabolic Bone Disease and Clinically Related Disorders; Avioli, L.V., Krane, S.M., Eds.; Academic Press: New York, NY, USA, 1997; pp. 51–94. [Google Scholar]
- Brown, E.M.; Gamba, G.; Riccardi, D.; Lombardi, M.; Butters, R.; Kifor, O.; Sun, A.; Hediger, M.A.; Lytton, J.; Hebert, S.C. Cloning and characterization of an extracellular Ca(2+)-sensing receptor from bovine parathyroid. Nature 1993, 366(6455), 575–580. [Google Scholar]
- Jilka, R.L. Molecular and cellular mechanisms of the anabolic effect of intermittent PTH. Bone 2007, 40(6), 1434–1446. [Google Scholar] [CrossRef]
- Neer, R.M.; Arnaud, C.D.; Zanchetta, J.R.; Prince, R.; Gaich, G.A.; Reginster, J.Y.; Hodsman, A.B.; Eriksen, E.F.; Ish-Shalom, S.; Genant, H.K.; et al. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N. Engl. J. Med. 2001, 344(19), 1434–1441. [Google Scholar] [CrossRef]
- Bukata, S.V.; Puzas, J.E. Orthopedic uses of teriparatide. Curr. Osteoporos. Rep. 2010, 8(1), 28–33. [Google Scholar]
- Ryder, K.M.; Tanner, S.B.; Carbone, L.; Williams, J.E.; Taylor, H.M.; Bush, A.; Pintea, V.; Watsky, M.A. Teriparatide is safe and effectively increases bone biomarkers in institutionalized individuals with osteoporosis. J. Bone Miner. Metab. 2010, 28(2), 233–239. [Google Scholar] [CrossRef]
- Saag, K.G.; Zanchetta, J.R.; Devogelaer, J.P.; Adler, R.A.; Eastell, R.; See, K.; Krege, J.H.; Krohn, K.; Warner, M.R. Effects of teriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: Thirty-six-month results of a randomized, double-blind, controlled trial. Arthritis Rheum. 2009, 60(11), 3346–3355. [Google Scholar] [CrossRef]
- Finkelstein, J.S.; Wyland, J.J.; Lee, H.; Neer, R.M. Effects of teriparatide, alendronate, or both in women with postmenopausal osteoporosis. J. Clin. Endocrinol. Metab. 2010, 95(4), 1838–1845. [Google Scholar] [CrossRef]
- Kakar, S.; Einhorn, T.A.; Vora, S.; Miara, L.J.; Hon, G.; Wigner, N.A.; Toben, D.; Jacobsen, K.A.; Al-Sebaei, M.O.; Song, M.; et al. Enhanced chondrogenesis and Wnt signaling in PTH-treated fractures. J. Bone Miner. Res. 2007, 22(12), 1903–1912. [Google Scholar]
- Etoh, M.; Yamaguchi, A. Repetition of continuous PTH treatments followed by periodic withdrawals exerts anabolic effects on rat bone. J. Bone Miner. Metab. 2010, 28(6), 641–649. [Google Scholar] [CrossRef]
- Ito, M. Parathyroid and bone. Effect of parathyroid hormone on bone quality. Clin. Calcium 2007, 17(12), 1858–1864. [Google Scholar]
- Nishida, S.; Yamaguchi, A.; Tanizawa, T.; Endo, N.; Mashiba, T.; Uchiyama, Y.; Suda, T.; Yoshiki, S.; Takahashi, H.E. Increased bone formation by intermittent parathyroid hormone administration is due to the stimulation of proliferation and differentiation of osteoprogenitor cells in bone marrow. Bone 1994, 15(6), 717–723. [Google Scholar] [CrossRef]
- Jilka, R.L.; O’Brien, C.A.; Ali, A.A.; Roberson, P.; Weinstein, R.S.; Manolagas, S.C. Intermittent PTH stimulates periosteal bone formation by actions on post-mitotic preosteoblasts. Bone 2009, 44(2), 275–286. [Google Scholar] [CrossRef]
- Jilka, R.L.; Weinstein, R.S.; Bellido, T.; Roberson, P.; Parfitt, A.M.; Manolagas, S.C. Increased bone formation by prevention of osteoblast apoptosis with parathyroid hormone. J. Clin. Invest. 1999, 104(4), 439–446. [Google Scholar] [CrossRef]
- Bellido, T.; Ali, A.A.; Gubrij, I.; Plotkin, L.I.; Fu, Q.; O’Brien, C.A.; Manolagas, S.C.; Jilka, R.L. Chronic elevation of parathyroid hormone in mice reduces expression of sclerostin by osteocytes: A novel mechanism for hormonal control of osteoblastogenesis. Endocrinology 2005, 146(11), 4577–4583. [Google Scholar]
- Uzawa, T.; Hori, M.; Ejiri, S.; Ozawa, H. Comparison of the effects of intermittent and continuous administration of human parathyroid hormone(1–34) on rat bone. Bone 1995, 16(4), 477–484. [Google Scholar]
- Horwitz, M.J.; Tedesco, M.B.; Sereika, S.M.; Syed, M.A.; Garcia‐Ocaña, A.; Bisello, A.; Hollis, B.W.; Rosen, C.J.; Wysolmerski, J.J.; Dann, P.; et al. Continuous PTH and PTHrP infusion causes suppression of bone formation and discordant effects on 1,25(OH)2 vitamin D. J. Bone Miner. Res. 2005, 20(10), 1792–1803. [Google Scholar] [CrossRef]
- Fu, Q.; Jilka, R.L.; Manolagas, S.C.; O’Brien, C.A. Parathyroid hormone stimulates receptor activator of NFkappa B ligand and inhibits osteoprotegerin expression via protein kinase A activation of cAMP-response element-binding protein. J. Biol. Chem. 2002, 277(50), 48868–48875. [Google Scholar]
- Tiyapatanaputi, P.; Rubery, P.T.; Carmouche, J.; Schwarz, E.M.; O’keefe, R.J.; Zhang, X. A novel murine segmental femoral graft model. J. Orthop. Res. 2004, 22(6), 1254–1260. [Google Scholar] [CrossRef]
- Einhorn, T.A.; Majeska, R.J.; Mohaideen, A.; Kagel, E.M.; Bouxsein, M.L.; Turek, T.J.; Wozney, J.M. A single percutaneous injection of recombinant human bone morphogenetic protein-2 accelerates fracture repair. J. Bone Jt. Surg. Am. Vol. 2003, 85-A(8), 1425–1435. [Google Scholar]
- Einhorn, T.A. Clinical applications of recombinant human BMPs: early experience and future development. J. Bone Jt. Surg. Am. Vol. 2003, 85-A Suppl. 3, 82–88. [Google Scholar]
- Bruder, S.P.; Kurth, A.A.; Shea, M.; Hayes, W.C.; Jaiswal, N.; Kadiyala, S. Bone regeneration by implantation of purified, culture-expanded human mesenchymal stem cells. J. Orthop. Res. 1998, 16(2), 155–162. [Google Scholar] [CrossRef]
- Yoon, S.T.; Boden, S.D. Osteoinductive molecules in orthopaedics: Basic science and preclinical studies. Clin. Orthop. Relat. Res. 2002, 395(2), 33–43. [Google Scholar] [CrossRef]
- Valentin-Opran, A.; Wozney, J.; Csimma, C.; Lilly, L.; Riedel, G.E. Clinical evaluation of recombinant human bone morphogenetic protein-2. Clin. Orthop. Relat. Res. 2002, 395(2), 110–120. [Google Scholar] [CrossRef]
- Rickard, D.J.; Wang, F.L.; Rodriguez-Rojas, A.M.; Wu, Z.; Trice, W.J.; Hoffman, S.J.; Votta, B.; Stroup, G.B.; Kumar, S.; Nuttall, M.E. Intermittent treatment with parathyroid hormone (PTH) as well as a non-peptide small molecule agonist of the PTH1 receptor inhibits adipocyte differentiation in human bone marrow stromal cells. Bone 2006, 39(6), 1361–1372. [Google Scholar] [CrossRef]
- Kaback, L.A.; Soung do, Y.; Naik, A.; Geneau, G.; Schwarz, E.M.; Rosier, R.N.; O’Keefe, R.J.; Drissi, H. Teriparatide (1–34 human PTH) regulation of osterix during fracture repair. J. Cell. Biochem. 2008, 105(1), 219–226. [Google Scholar] [CrossRef]
- Yang, C.; Frei, H.; Burt, H.M.; Rossi, F. Effects of continuous and pulsatile PTH treatments on rat bone marrow stromal cells. Biochem. Biophys. Res. Commun. 2009, 380(4), 791–796. [Google Scholar]
- Moutsatsos, I.K.; Turgeman, G.; Zhou, S.; Kurkalli, B.G.; Pelled, G.; Tzur, L.; Kelley, P.; Stumm, N.; Mi, S.; Müller, R.; et al. Exogenously regulated stem cell-mediated gene therapy for bone regeneration. Mol. Ther. 2001, 3(4), 449–461. [Google Scholar] [CrossRef]
- Gazit, D.; Turgeman, G.; Kelley, P.; Wang, E.; Jalenak, M.; Zilberman, Y.; Moutsatsos, I. Engineered pluripotent mesenchymal cells integrate and differentiate in regenerating bone: A novel cell-mediated gene therapy. J. Gene Med. 1999, 1(2), 121–133. [Google Scholar]
- Turgeman, G.; Pittman, D.D.; Müller, R.; Kurkalli, B.G.; Zhou, S.; Pelled, G.; Peyser, A.; Zilberman, Y.; Moutsatsos, I.K.; Gazit, D. Engineered human mesenchymal stem cells: A novel platform for skeletal cell mediated gene therapy. J. Gene Med. 2001, 3(3), 240–251. [Google Scholar]
- Dayoub, H.; Dumont, R.J.; Li, J.Z.; Dumont, A.S.; Hankins, G.R.; Kallmes, D.F.; Helm, G.A. Human mesenchymal stem cells transduced with recombinant bone morphogenetic protein-9 adenovirus promote osteogenesis in rodents. Tissue Eng. 2003, 9(2), 347–356. [Google Scholar] [CrossRef]
- Virk, M.S.; Sugiyama, O.; Park, S.H.; Gambhir, S.S.; Adams, D.J.; Drissi, H.; Lieberman, J.R. “Same Day” ex-vivo regional gene therapy: A novel strategy to enhance bone repair. Mol. Ther. 2011, 19(5), 960–968. [Google Scholar] [CrossRef]
- Aslan, H.; Zilberman, Y.; Kandel, L.; Liebergall, M.; Oskouian, R.J.; Gazit, D.; Gazit, Z. Osteogenic differentiation of noncultured immunoisolated bone marrow-derived CD105+ cells. Stem Cells 2006, 24(7), 1728–1737. [Google Scholar] [CrossRef]
- Aslan, H.; Zilberman, Y.; Arbeli, V.; Sheyn, D.; Matan, Y.; Liebergall, M.; Li, J.Z.; Helm, G.A.; Gazit, D.; Gazit, Z. Nucleofection-based ex vivo nonviral gene delivery to human stem cells as a platform for tissue regeneration. Tissue Eng. 2006, 12(4), 877–889. [Google Scholar] [CrossRef] [PubMed]
- Boden, S.D.; Kang, J.; Sandhu, H.; Heller, J.G. Use of recombinant human bone morphogenetic protein-2 to achieve posterolateral lumbar spine fusion in humans: A prospective, randomized clinical pilot trial: 2002 Volvo Award in clinical studies. Spine 2002, 27(23), 2662–2673. [Google Scholar] [CrossRef]
- Jilka, R.L.; Almeida, M.; Ambrogini, E.; Han, L.; Roberson, P.K.; Weinstein, R.S.; Manolagas, S.C. Decreased oxidative stress and greater bone anabolism in the aged, when compared to the young, murine skeleton with parathyroid hormone administration. Aging Cell 2010, 9(5), 851–867. [Google Scholar] [CrossRef]
- Andreassen, T.T.; Ejersted, C.; Oxlund, H. Intermittent parathyroid hormone (1–34) treatment increases callus formation and mechanical strength of healing rat fractures. J. Bone Miner. Res. 1999, 14(6), 960–968. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, A.; Shimoji, N.; Shiomi, K.; Shimizu, S.; Moriya, H.; Einhorn, T.A.; Yamazaki, M. Mechanisms for the enhancement of fracture healing in rats treated with intermittent low-dose human parathyroid hormone (1–34). J. Bone Miner. Res. 2002, 17(11), 2038–2047. [Google Scholar] [CrossRef] [PubMed]
- Nakazawa, T.; Nakajima, A.; Shiomi, K.; Moriya, H.; Einhorn, T.A.; Yamazaki, M. Effects of low-dose, intermittent treatment with recombinant human parathyroid hormone (1–34) on chondrogenesis in a model of experimental fracture healing. Bone 2005, 37(5), 711–719. [Google Scholar] [CrossRef]
- Kaback, L.A.; Soung do, Y.; Naik, A.; Geneau, G.; Schwarz, E.M.; Rosier, R.N.; O’Keefe, R.J.; Drissi, H. Teriparatide (1–34 human PTH) regulation of osterix during fracture repair. J. Cell Biochem. 2008, 105(1), 219–226. [Google Scholar] [CrossRef] [PubMed]
- Kaback, L.A.; Soung do, Y.; Naik, A.; Smith, N.; Schwarz, E.M.; O’Keefe, R.J.; Drissi, H. Osterix/Sp7 regulates mesenchymal stem cell mediated endochondral ossification. J. Cell. Physiol. 2008, 214(1), 173–182. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, K.; Jingushi, S.; Ikenoue, T.; Urabe, K.; Sakai, H.; Iwamoto, Y. Expression of parathyroid hormone-related peptide and insulin-like growth factor I during rat fracture healing. J. Orthop. Res. 2003, 21(3), 511–520. [Google Scholar] [CrossRef]
- Kakar, S.; Einhorn, T.A.; Vora, S.; Miara, L.J.; Hon, G.; Wigner, N.A.; Toben, D.; Jacobsen, K.A.; Al-Sebaei, M.O.; Song, M.; et al. Enhanced chondrogenesis and Wnt signaling in PTH-treated fractures. J. Bone Miner. Res. 2007, 22(12), 1903–1912. [Google Scholar] [CrossRef]
- Komatsu, D.E.; Brune, K.A.; Liu, H.; Schmidt, A.L.; Han, B.; Zeng, Q.Q.; Yang, X.H.; Nunes, J.S.; Lu, Y.F.; Geiser, A.G.; et al. Longitudinal in vivo analysis of the region-specific efficacy of parathyroid hormone in a rat cortical defect model. Endocrinology 2009, 150(4), 1570–1579. [Google Scholar] [CrossRef]
- Skripitz, R.; Andreassen, T.T.; Aspenberg, P. Parathyroid hormone (1–34) increases the density of rat cancellous bone in a bone chamber. A dose-response study. J. Bone Jt. Surg. Br. Vol. 2000, 82(1), 138–141. [Google Scholar]
- Andreassen, T.T.; Willick, G.E.; Morley, P.; Whitfield, J.F. Treatment with parathyroid hormone hPTH(1–34), hPTH(1–31), and monocyclic hPTH(1–31) enhances fracture strength and callus amount after withdrawal fracture strength and callus mechanical quality continue to increase. Calcif. Tissue Int. 2004, 74(4), 351–356. [Google Scholar] [CrossRef]
- Komatsubara, S.; Mori, S.; Mashiba, T.; Nonaka, K.; Seki, A.; Akiyama, T.; Miyamoto, K.; Cao, Y.; Manabe, T.; Norimatsu, H. Human parathyroid hormone (1–34) accelerates the fracture healing process of woven to lamellar bone replacement and new cortical shell formation in rat femora. Bone 2005, 36(4), 678–687. [Google Scholar] [CrossRef]
- Manabe, T.; Mori, S.; Mashiba, T.; Kaji, Y.; Iwata, K.; Komatsubara, S.; Seki, A.; Sun, Y.X.; Yamamoto, Y. Human parathyroid hormone (1–34) accelerates natural fracture healing process in the femoral osteotomy model of cynomolgus monkeys. Bone 2007, 40(6), 1475–1482. [Google Scholar]
- Quinn, J.M.; Elliott, J.; Gillespie, M.T.; Martin, T.J. A combination of osteoclast differentiation factor and macrophage-colony stimulating factor is sufficient for both human and mouse osteoclast formation in vitro. Endocrinology 1998, 139(10), 4424–4427. [Google Scholar] [CrossRef]
- Yasuda, H.; Shima, N.; Nakagawa, N.; Yamaguchi, K.; Kinosaki, M.; Mochizuki, S.; Tomoyasu, A.; Yano, K.; Goto, M.; Murakami, A.; et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc. Natl. Acad. Sci. USA 1998, 95(7), 3597–3602. [Google Scholar] [CrossRef] [PubMed]
- Alkhiary, Y.M.; Gerstenfeld, L.C.; Krall, E.; Westmore, M.; Sato, M.; Mitlak, B.H.; Einhorn, T.A. Enhancement of experimental fracture-healing by systemic administration of recombinant human parathyroid hormone (PTH 1–34). J. Bone Jt. Surg. Am. Vol. 2005, 87(4), 731–741. [Google Scholar] [CrossRef]
- Pierroz, D.D.; Bonnet, N.; Baldock, P.A.; Ominsky, M.S.; Stolina, M.; Kostenuik, P.J.; Ferrari, S.L. Are osteoclasts needed for the bone anabolic response to parathyroid hormone? A study of intermittent parathyroid hormone with denosumab or alendronate in knock-in mice expressing humanized RANKL. J. Biol. Chem. 2010, 285(36), 28164–28173. [Google Scholar]
- Chavassieux, P.; Karsdal, M.A.; Segovia‐Silvestre, T.; Neutzsky‐Wulff, A.V.; Chapurlat, R.; Boivin, G.; Delmas, P.D. Mechanisms of the anabolic effects of teriparatide on bone: insight from the treatment of a patient with pycnodysostosis. J. Bone Miner. Res. 2008, 23(7), 1076–1083. [Google Scholar] [CrossRef]
- Martin, T.J. Does bone resorption inhibition affect the anabolic response to parathyroid hormone? Trends Endocrinol. Metab. 2004, 15(2), 49–50. [Google Scholar]
- Reynolds, D.G.; Shaikh, S.; Papuga, M.O.; Lerner, A.L.; O’Keefe, R.J.; Schwarz, E.M.; Awad, H.A. muCT-based measurement of cortical bone graft-to-host union. J. Bone Miner. Res. 2009, 24(5), 899–907. [Google Scholar] [CrossRef]
- Oteo-Alvaro, A.; Moreno, E. Atrophic humeral shaft nonunion treated with teriparatide (rh PTH 1–34): A case report. J. Shoulder Elbow Surg. 2010, 19(7), e22–e28. [Google Scholar] [CrossRef]
- Rubery, P.T.; Bukata, S.V. Teriparatide may accelerate healing in delayed unions of type III odontoid fractures: A report of 3 cases. J. Spinal Disord. Tech. 2010, 23(2), 151–155. [Google Scholar] [CrossRef]
- Chintamaneni, S.; Finzel, K.; Gruber, B.L. Successful treatment of sternal fracture nonunion with teriparatide. Osteoporos. Int. 2010, 21(6), 1059–1063. [Google Scholar] [CrossRef]
- Puzas, J.E.; Houck, J.; Bukata, S.V. Accelerated fracture healing. J. Am. Acad. Orthop. Surg. 2006, 14(10), S145–S151. [Google Scholar]
- Resmini, G.; Iolascon, G. 79-year-old post-menopausal woman with humerus fracture during teriparatide treatment. Aging Clin. Exp. Res. 2007, 19 Suppl. 4, 30–31. [Google Scholar]
- Peichl, P.; Holzer, G. Parathyroid Hormone 1-84 Accelerates Fracture Healing in Pubic Bones of Elderly Osteoporotic Women. In Proceedings of ASBMR 31st Annual Meeting, Colorado, CO, USA, 11–15 September 2009.
- Zati, A.; Sarti, D.; Malaguti, M.C.; Pratelli, L. Teriparatide in the treatment of a loose hip prosthesis. J. Rheumatol. 2011, 38(4), 778–780. [Google Scholar] [CrossRef] [PubMed]
- Aspenberg, P.; Genant, H.K.; Johansson, T.; Nino, A.J.; See, K.; Krohn, K.; García-Hernández, P.A.; Recknor, C.P.; Einhorn, T.A.; Dalsky, G.P.; et al. Teriparatide for acceleration of fracture repair in humans: A prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J. Bone Miner. Res. 2010, 25(2), 404–414. [Google Scholar] [CrossRef]
- Aspenberg, P.; Johansson, T. Teriparatide improves early callus formation in distal radial fractures. Acta Orthop. 2010, 81(2), 234–236. [Google Scholar]
- Tsujimoto, M.; Chen, P.; Miyauchi, A.; Sowa, H.; Krege, J.H. PINP as an aid for monitoring patients treated with teriparatide. Bone 2011, 48(4), 798–803. [Google Scholar] [CrossRef]
- Yu, E.W.; Neer, R.M.; Lee, H.; Wyland, J.J.; de la Paz, A.V.; Davis, M.C.; Okazaki, M.; Finkelstein, J.S. Time-dependent changes in skeletal response to teriparatide: Escalating vs. constant dose teriparatide (PTH 1–34) in osteoporotic women. Bone 2011, 48(4), 713–719. [Google Scholar]
- Aleksyniene, R.; Thomsen, J.S.; Eckardt, H.; Bundgaard, K.G.; Lind, M.; Hvid, I. Parathyroid hormone PTH(1–34) increases the volume, mineral content, and mechanical properties of regenerated mineralizing tissue after distraction osteogenesis in rabbits. Acta Orthop. 2009, 80(6), 716–723. [Google Scholar]
© 2011 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Dhillon, R.S.; Schwarz, E.M. Teriparatide Therapy as an Adjuvant for Tissue Engineering and Integration of Biomaterials. Materials 2011, 4, 1117-1131. https://doi.org/10.3390/ma4061117
Dhillon RS, Schwarz EM. Teriparatide Therapy as an Adjuvant for Tissue Engineering and Integration of Biomaterials. Materials. 2011; 4(6):1117-1131. https://doi.org/10.3390/ma4061117
Chicago/Turabian StyleDhillon, Robinder S., and Edward M. Schwarz. 2011. "Teriparatide Therapy as an Adjuvant for Tissue Engineering and Integration of Biomaterials" Materials 4, no. 6: 1117-1131. https://doi.org/10.3390/ma4061117



