In Vitro Analysis of the Fracture Resistance of CAD/CAM Denture Base Resins
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Specimens
2.2. Three-Point Bending Test
2.3. Fracture Surface Roughness Measurements and Fracture Surface Texture
2.4. Statistics
3. Results
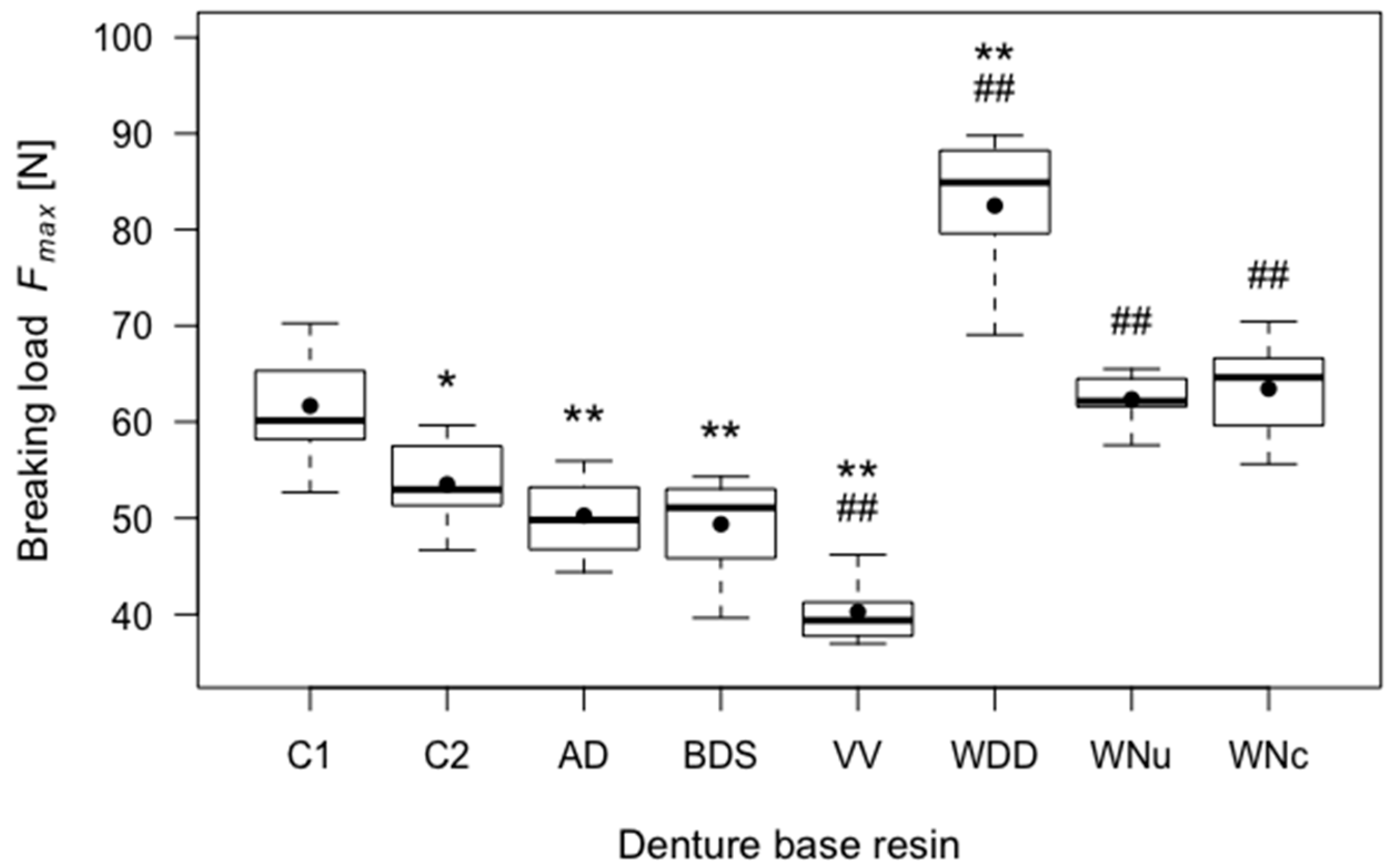
3.1. Breaking Load
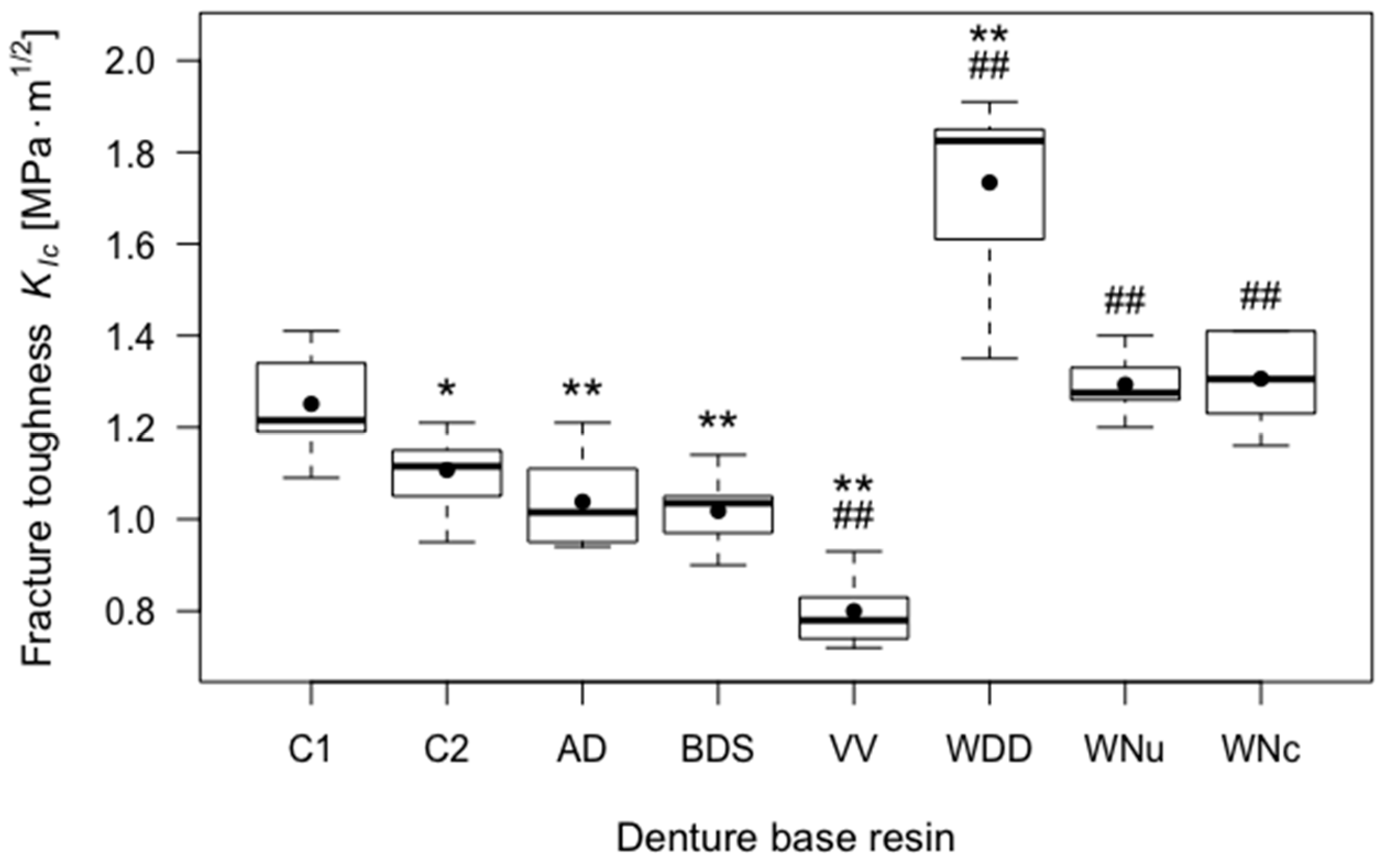
3.2. Fracture Toughness
3.3. Elastic Modulus
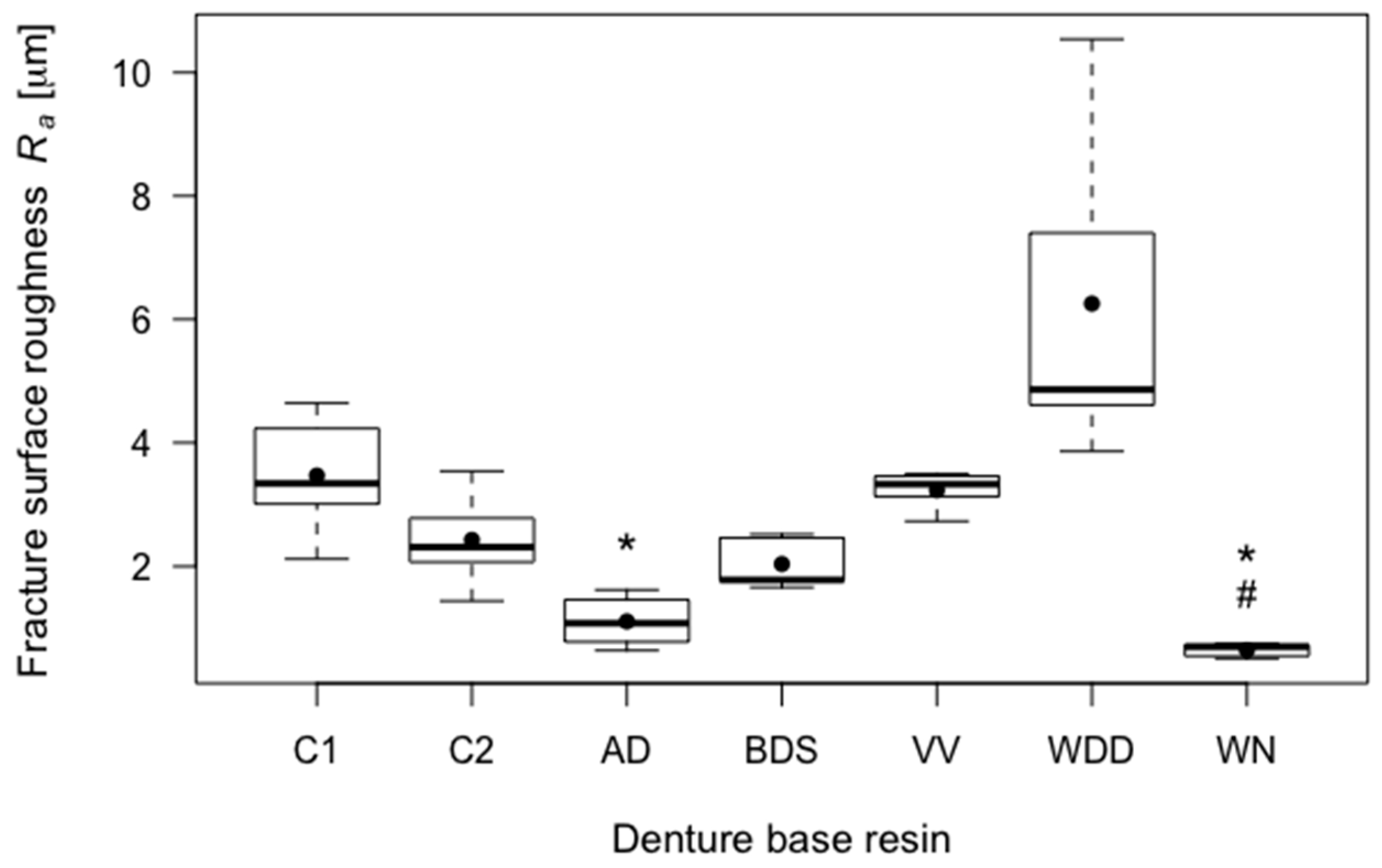
3.4. Fracture Surface Roughness
3.5. Statistical Correlation between Mechanical Behaviour and Fracture Surface Roughness
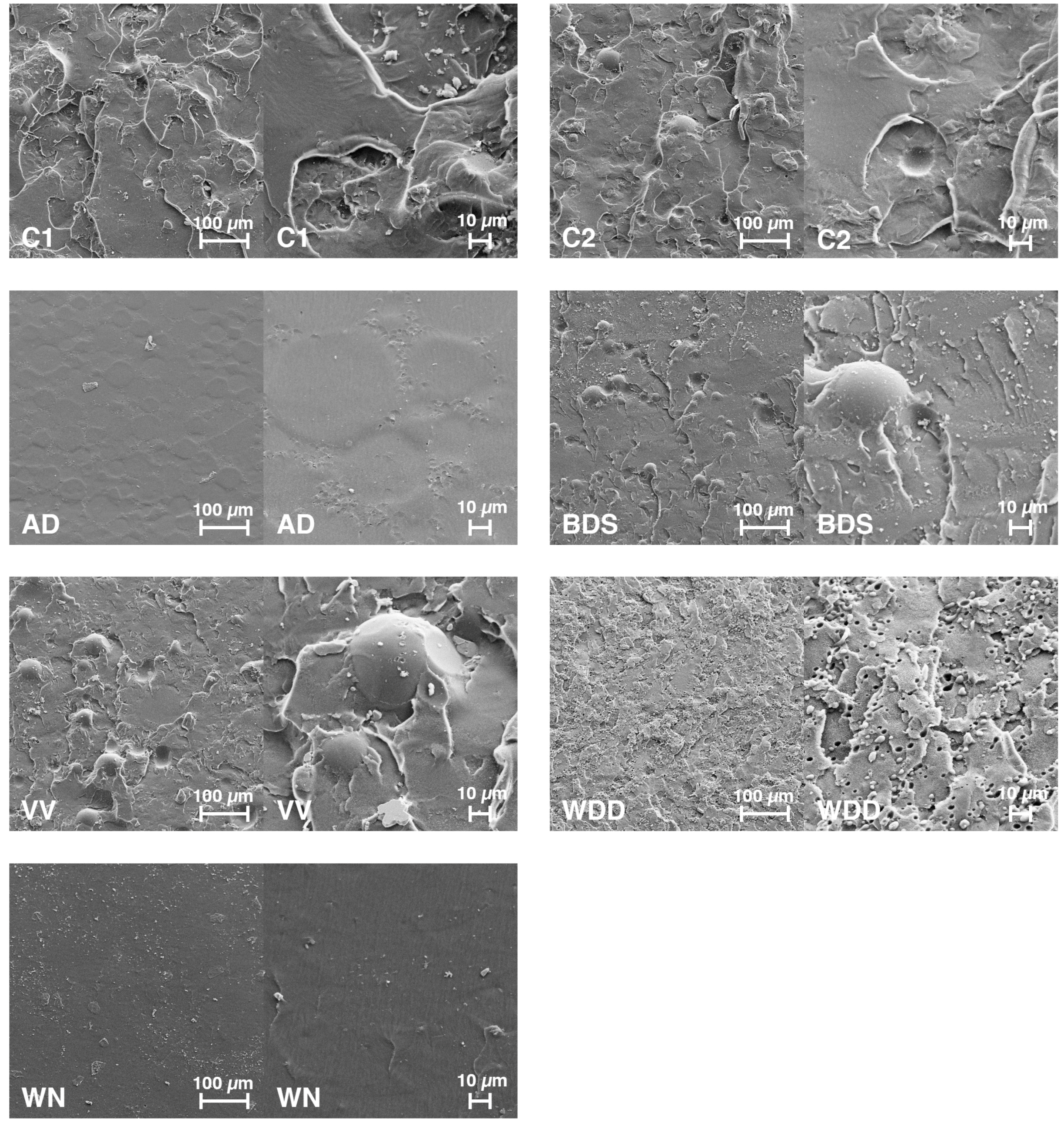
3.6. SEM Imaging of Fracture Surfaces
4. Discussion
4.1. Experimental Setup
4.2. Study Findings
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Darbar, U.R.; Huggett, R.; Harrison, A. Denture fracture—A survey. Br. Dent. J. 1994, 176, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Ates, M.; Cilingir, A.; Sulun, T.; Sunbuloglu, E.; Bozdag, E. The effect of occlusal contact localization on the stress distribution in complete maxillary denture. J. Oral Rehabilit. 2006, 33, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Ali, I.L.; Yunus, N.; Abu-Hassan, M.I. Hardness, flexural strength, and flexural modulus comparisons of three differently cured denture base systems. J. Prosthodont. 2008, 17, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Ucar, Y.; Akova, T.; Aysan, I. Mechanical properties of polyamide versus different pmma denture base materials. J. Prosthodont. 2012, 21, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Wadachi, J.; Sato, M.; Igarashi, Y. Evaluation of the rigidity of dentures made of injection-molded materials. Dent. Mater. J. 2013, 32, 508–511. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, T.; Lassila, L.V.; Tokue, A.; Takahashi, Y.; Vallittu, P.K. Influence of molecular weight of polymethyl(methacrylate) beads on the properties and structure of cross-linked denture base polymer. J. Mech. Behav. Biomed. Mater. 2011, 4, 1846–1851. [Google Scholar] [CrossRef] [PubMed]
- Huggett, R.; Bates, J.F.; Packham, D.E. The effect of the curing cycle upon the molecular weight and properties of denture base materials. Dent. Mater. 1987, 3, 107–112. [Google Scholar] [CrossRef]
- Murakami, N.; Wakabayashi, N.; Matsushima, R.; Kishida, A.; Igarashi, Y. Effect of high-pressure polymerization on mechanical properties of pmma denture base resin. J. Mech. Behav. Biomed. Mater. 2013, 20, 98–104. [Google Scholar] [CrossRef] [PubMed]
- El Ghazali, S.; Glantz, P.O.; Randow, K. On the clinical deformation of maxillary complete dentures. Influence of the processing techniques of acrylate-based polymers. Acta Odontol. Scand. 1988, 46, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Minoura, M.; Tsutsumi, S.; Okada, M.; Nokubi, T. A cad/cam system for removable denture. Part I: Fabrication of complete dentures. Int. J. Prosthodont. 1994, 7, 17–21. [Google Scholar] [PubMed]
- Kawahata, N.; Ono, H.; Nishi, Y.; Hamano, T.; Nagaoka, E. Trial of duplication procedure for complete dentures by cad/cam. J. Oral Rehabilit. 1997, 24, 540–548. [Google Scholar] [CrossRef]
- Sun, Y.; Lu, P.; Wang, Y. Study on cad&rp for removable complete denture. Comput. Methods Programs Biomed. 2009, 93, 266–272. [Google Scholar] [PubMed]
- Kanazawa, M.; Inokoshi, M.; Minakuchi, S.; Ohbayashi, N. Trial of a cad/cam system for fabricating complete dentures. Dent. Mater. J. 2011, 30, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Inokoshi, M.; Kanazawa, M.; Minakuchi, S. Evaluation of a complete denture trial method applying rapid prototyping. Dent. Mater. J. 2012, 31, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Steinmassl, P.A.; Klaunzer, F.; Steinmassl, O.; Dumfahrt, H.; Grunert, I. Evaluation of currently available cad/cam denture systems. Int. J. Prosthodont. 2017, 30, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, C.J.; Garbacea, A.; Naylor, W.P.; Daher, T.; Marchack, C.B.; Lowry, J. Cad/cam fabricated complete dentures: Concepts and clinical methods of obtaining required morphological data. J. Prosthet. Dent. 2012, 107, 34–46. [Google Scholar] [CrossRef]
- Infante, L.; Yilmaz, B.; McGlumphy, E.; Finger, I. Fabricating complete dentures with cad/cam technology. J. Prosthet. Dent. 2014, 111, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Steinmassl, P.A.; Wiedemair, V.; Huck, C.; Klaunzer, F.; Steinmassl, O.; Grunert, I.; Dumfahrt, H. Do cad/cam dentures really release less monomer than conventional dentures? Clin. Oral Investig. 2017, 21, 1697–1705. [Google Scholar] [CrossRef] [PubMed]
- Steinmassl, P.A.; Steinmassl, O.; Dumfahrt, H.; Grunert, I. Total digital—Materialkundliche aspekte cad/cam-gefertigter prothesen. Teamwork 2016, 19, 206–209. [Google Scholar]
- Dentistry—Base Polymers—Part 1: Denture Base Polymers; ISO 20795-1:2013; International Organization for Standardization: Geneva, Switzerland, 2013.
- Geometrische Produktspezifikationen (GPS)–Oberflächenbeschaffenheit: Tastschnittverfahren–Nenneigenschaften von Tastschnittgeräten (ISO 3274: 1996); DIN EN ISO 3274:1998-04; Beuth Verlag: Berlin, Germany, 1998.
- Vallittu, P.K. Glass fiber reinforcement in repaired acrylic resin removable dentures: Preliminary results of a clinical study. Quintessence Int. 1997, 28, 39–44. [Google Scholar] [PubMed]
- Narva, K.K.; Vallittu, P.K.; Helenius, H.; Yli-Urpo, A. Clinical survey of acrylic resin removable denture repairs with glass-fiber reinforcement. Int. J. Prosthodont. 2001, 14, 219–224. [Google Scholar] [PubMed]
- Fontijn-Tekamp, F.A.; Slagter, A.P.; Van Der Bilt, A.; Van Hof, T.M.A.; Witter, D.J.; Kalk, W.; Jansen, J.A. Biting and chewing in overdentures, full dentures, and natural dentitions. J. Dent. Res. 2000, 79, 1519–1524. [Google Scholar] [CrossRef] [PubMed]
- Massachusetts Institute of Technology (MIT). 6.777j/2.751j Material Properties Database-PMMA. Available online: http://www.mit.edu/~6.777/matprops/pmma.htm (accessed on 20 November 2017).
- Ayman, A.D. The residual monomer content and mechanical properties of cad\cam resins used in the fabrication of complete dentures as compared to heat cured resins. Electron. Physician 2017, 9, 4766–4772. [Google Scholar] [CrossRef] [PubMed]
- Ruyter, I.E.; Espevik, S. Compressive creep of denture base polymers. Acta Odontol. Scand. 1980, 38, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Jagger, D.C.; Harrison, A.; Jandt, K.D. The reinforcement of dentures. J. Oral Rehabilit. 1999, 26, 185–194. [Google Scholar] [CrossRef]


| Group | Abbreviation | Product Name | Manufacturer | Head Office |
|---|---|---|---|---|
| 1 | AD | AvaDent Digital Dentures | Global Dental Science Europe BV | Tilburg, Netherlands |
| 2 | BDS | Baltic Denture System | Merz Dental GmbH | Lütjenburg, Germany |
| 3 | VV | Vita VIONIC | Vita Zahnfabrik | Bad Säckingen, Germany |
| 4 | WDD | Wieland Digital Dentures | Wieland Dental + Technik GmbH & Co. KG Ivocar Vivadent AG | Pforzheim, Germany/Schaan, Liechtenstein |
| 5 | WNu | Whole You Nexteeth (uncoated) | Whole You Inc. | San Jose, US |
| 6 | WNc | Whole You Nexteeth (coated) | Whole You Inc. | San Jose, US |
| 7 | C1 (control group 1) | Candulor Aesthetic Red (heat-curing resin) | Candulor AG | Glattpark, Germany |
| 8 | C2 (control group 2) | Candulor Aesthetic Blue (self-curing resin) | Candulor AG | Glattpark, Germany |
| Parameter | Group | Mean | SD a | p (Compared to C1) | p (Compared to C2) |
|---|---|---|---|---|---|
| Breaking load Fmax (N) | C1 | 61.66 | 5.60 | - | 0.030 |
| C2 | 53.51 | 4.07 | 0.030 | - | |
| AD | 50.26 | 4.02 | 0.002 | 0.629 | |
| BDS | 49.37 | 4.91 | 0.001 | 0.448 | |
| VV | 40.27 | 3.40 | 0.000 | 0.000 | |
| WDD | 82.49 | 7.47 | 0.000 | 0.000 | |
| WNu | 62.35 | 2.44 | 1.000 | 0.001 | |
| WNc | 63.44 | 4.91 | 0.993 | 0.002 | |
| Fracture toughness KIc (MPa·m1/2) | C1 | 1.25 | 0.11 | - | 0.049 |
| C2 | 1.11 | 0.08 | 0.049 | - | |
| AD | 1.04 | 0.10 | 0.004 | 0.644 | |
| BDS | 1.02 | 0.07 | 0.001 | 0.170 | |
| VV | 0.80 | 0.07 | 0.000 | 0.000 | |
| WDD | 1.73 | 0.19 | 0.000 | 0.000 | |
| WNu | 1.29 | 0.6 | 0.947 | 0.000 | |
| WNc | 1.31 | 0.09 | 0.913 | 0.001 | |
| Elastic modulus E (MPa) | C1 | 3570.24 | 450.75 | - | 0.950 |
| C2 | 3405.01 | 178.52 | 0.950 | - | |
| AD | 4649.15 | 1110.93 | 0.171 | 0.077 | |
| BDS | 4606.38 | 325.93 | 0.000 | 0.000 | |
| VV | 4569.16 | 267.40 | 0.001 | 0.000 | |
| WDD | 4009.95 | 200.00 | 0.175 | 0.000 | |
| WNu | 4921.05 | 87.85 | 0.000 | 0.000 | |
| WNc | 4777.01 | 110.72 | 0.000 | 0.000 | |
| Fracture surface roughness Ra (µm) | C1 | 3.47 | 0.10 | - | 0.568 |
| C2 | 2.42 | 0.79 | 0.568 | - | |
| AD | 1.11 | 0.38 | 0.032 | 0.118 | |
| BDS | 2.04 | 0.42 | 0.197 | 0.942 | |
| VV | 3.23 | 0.31 | 1.000 | 0.405 | |
| WDD | 6.25 | 2.74 | 0.447 | 0.205 | |
| WN | 0.65 | 0.11 | 0.019 | 0.050 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steinmassl, O.; Offermanns, V.; Stöckl, W.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.-A. In Vitro Analysis of the Fracture Resistance of CAD/CAM Denture Base Resins. Materials 2018, 11, 401. https://doi.org/10.3390/ma11030401
Steinmassl O, Offermanns V, Stöckl W, Dumfahrt H, Grunert I, Steinmassl P-A. In Vitro Analysis of the Fracture Resistance of CAD/CAM Denture Base Resins. Materials. 2018; 11(3):401. https://doi.org/10.3390/ma11030401
Chicago/Turabian StyleSteinmassl, Otto, Vincent Offermanns, Wolfgang Stöckl, Herbert Dumfahrt, Ingrid Grunert, and Patricia-Anca Steinmassl. 2018. "In Vitro Analysis of the Fracture Resistance of CAD/CAM Denture Base Resins" Materials 11, no. 3: 401. https://doi.org/10.3390/ma11030401





