The Association Between Community Stressors and Asthma Prevalence of School Children in Winnipeg, Canada
Abstract
:1. Introduction
2. Experimental Section
2.1. SAGE Survey in Manitoba
2.2. Census Tract and Neighbourhood Profile Selection Criteria
2.3. Measures of Community Socioeconomic Makeup and Community Disorder
2.4. Measures of Community Crime
2.5. Statistical Analysis
3. Results
| Variable | Category | Children of Birth Homes( N = 698) | Birth and Non-Birth Home Children ( N = 1472) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All Children | Children with Asthma | All Children | Children with Asthma | |||||||
| No. | % | No. | % | No. | % | No. | % | |||
| Parent Report of Child Asthma | Yes | 84 | 12.0 | NA | NA | 197 | 13.4 | NA | NA | |
| No | 614 | 88.0 | NA | NA | 1275 | 86.6 | NA | NA | ||
| Father has Asthma | Yes | 51 | 7.3 | 16 | 31.4 | 120 | 8.2 | 31 | 25.8 | |
| No | 630 | 90.3 | 64 | 10.2 | 1302 | 88.5 | 151 | 11.6 | ||
| Not Sure | 17 | 2.4 | 4 | 23.5 | 50 | 3.4 | 15 | 30.0 | ||
| Mother has Asthma | Yes | 57 | 8.2 | 14 | 24.6 | 144 | 9.8 | 52 | 36.1 | |
| No | 624 | 89.4 | 68 | 10.9 | 1283 | 87.2 | 140 | 10.9 | ||
| Not Sure | 17 | 2.4 | 2 | 11.8 | 34 | 2.3 | 5 | 14.7 | ||
| Family History of Asthma (separate variable) | Yes | 162 | 23.2 | 42 | 25.9 | 390 | 26.5 | 112 | 28.7 | |
| No | 536 | 76.8 | 42 | 7.8 | 1082 | 73.5 | 85 | 7.9 | ||
| Hay Fever in Child | Yes | 46 | 6.6 | 24 | 52.2 | 117 | 7.9 | 59 | 50.4 | |
| No | 652 | 93.4 | 60 | 9.2 | 1355 | 92.1 | 138 | 10.2 | ||
| Mold in Household 1995 | Yes | 5 | 0.7 | 2 | 40.0 | 208 | 14.1 | 40 | 19.2 | |
| No | 693 | 99.3 | 82 | 11.8 | 1264 | 85.9 | 157 | 12.4 | ||
| Smoking in Household | Yes | 148 | 21.2 | 24 | 16.2 | 357 | 24.3 | 62 | 17.4 | |
| No | 550 | 78.8 | 60 | 10.9 | 1115 | 75.7 | 135 | 12.1 | ||
| Incidence of Low Income in Households | Quintile 1 | 52 | 7.4 | 10 | 19.2 | 135 | 9.2 | 21 | 15.6 | |
| Quintile 3 | 173 | 24.8 | 16 | 9.2 | 325 | 22.1 | 34 | 10.5 | ||
| Households that are Home Owner Households | Quintile 2 | 164 | 23.5 | 14 | 8.5 | 339 | 23.0 | 36 | 10.6 | |
| Quintile 5 | 47 | 6.7 | 9 | 19.1 | 123 | 8.4 | 24 | 19.5 | ||
| Income Government Transfers Comprise | Quintile 1 | 50 | 7.2 | 10 | 20.0 | 145 | 9.9 | 24 | 16.6 | |
| Quintile 5 | 203 | 29.1 | 21 | 10.3 | 438 | 29.8 | 45 | 10.3 | ||
| Aboriginal Population Composition | Quintile 1 | 53 | 7.6 | 10 | 18.9 | 143 | 9.7 | 22 | 15.4 | |
| Quintile 4 | 128 | 18.3 | 10 | 7.8 | 284 | 19.3 | 29 | 10.2 | ||
| Median 1995 Income | Quintile 1 | 233 | 33.4 | 26 | 11.2 | 467 | 31.7 | 55 | 11.8 | |
| Quintile 5 | 41 | 5.9 | 10 | 24.4 | 121 | 8.2 | 21 | 17.4 | ||
| Male Population Aged 15+ and Unemployed | Quintile 1 | 44 | 6.3 | 12 | 27.3 | 148 | 10.1 | 28 | 18.9 | |
| Quintile 2 | 154 | 22.1 | 19 | 12.3 | 271 | 18.4 | 40 | 14.8 | ||
| Quintile 3 | 157 | 22.5 | 13 | 8.3 | 338 | 23.0 | 48 | 14.2 | ||
| Quintile 4 | 172 | 24.6 | 16 | 9.3 | 351 | 23.8 | 36 | 10.3 | ||
| Population that is Male Aged 15 to 24 | Quintile 1 | 186 | 26.6 | 16 | 8.6 | 397 | 27.0 | 42 | 10.6 | |
| Quintile 3 | 147 | 21.1 | 23 | 15.6 | 307 | 20.9 | 55 | 17.9 | ||
| Labour force Participation Aged 15 to 64 | Quintile 1 | 219 | 31.4 | 22 | 10.0 | 457 | 31.0 | 50 | 10.9 | |
| Quintile 4 | 109 | 15.6 | 20 | 18.3 | 242 | 16.4 | 42 | 17.4 | ||
| Homes Needing Major Repairs | Quintile 2 | 107 | 15.3 | 22 | 20.6 | 228 | 15.5 | 39 | 17.1 | |
| Quintile 5 | 195 | 27.9 | 22 | 11.3 | 428 | 29.1 | 51 | 11.9 | ||
| Sexual Assaults per 10,000 Persons | 2.03 | 56 | 8.0 | 5 | 8.9 | 122 | 8.3 | 13 | 10.7 | |
| 9.08 | 52 | 7.4 | 7 | 13.5 | 91 | 6.2 | 10 | 11.0 | ||
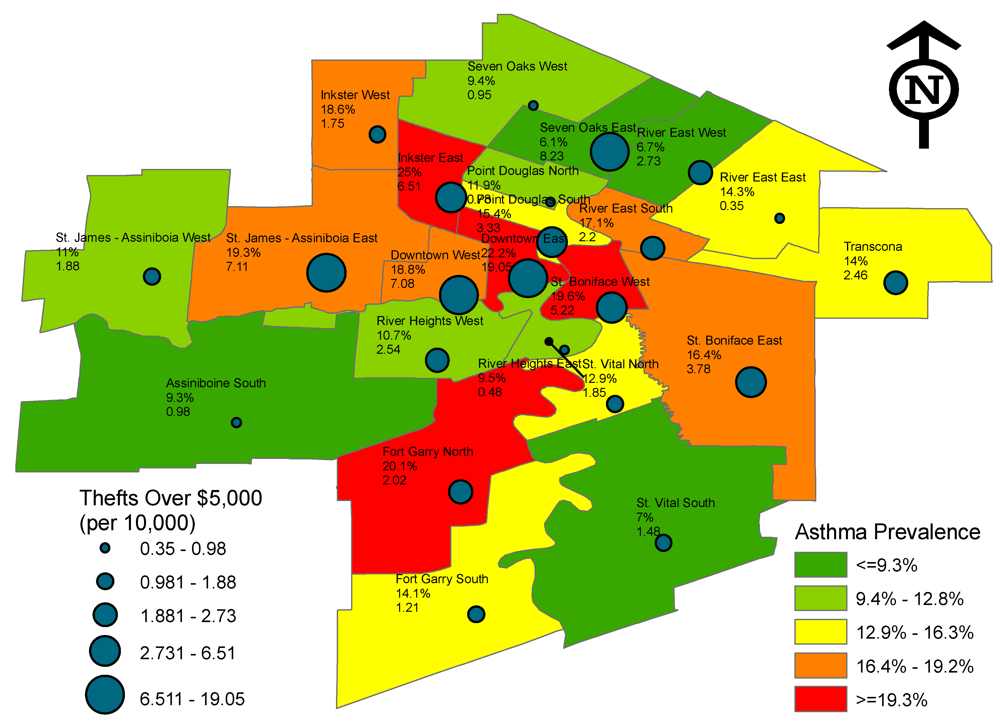
| Thefts Over $5,000 per 10,000 Persons | 0.35 | 49 | 7.0 | 5 | 10.2 | 105 | 7.1 | 15 | 14.3 | |
| 7.11 | 41 | 5.9 | 7 | 17.1 | 83 | 5.6 | 16 | 19.3 | ||
| Variable | Reference Category | Likelihood of Asthma at Age 7 or 8, OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| Children of Birth Homes | Birth and Non-Birth Home Children | |||||
| Quintile or Crime Value | Quintile Proportion, Income or Profile Name | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Community Socioeconomic Makeup Domain | ||||||
| Incidence of Low Income in Households | Quintile 3 to Quintile 1 | [0.17, 0.25) to [0.01, 0.10) | 0.38 (0.15–0.95) a | |||
| Households that are Home Owner Households | Quintile 5 to Quintile 2 | [0.88, 0.99) to [0.46, 0.65) | 2.79 (1.07–7.30) | 3.49 (1.30–9.37) b | 2.05 (1.13–3.72) | 1.87 (1.01–3.46) b |
| Income Government Transfers Comprise | Quintile 5 to Quintile 1 | [0.22, 0.53) to [0.03, 0.09) | 0.36 (0.14–0.96) b | |||
| Aboriginal Population Composition | Quintile 4 to Quintile 1 | [0.06, 0.10) to [0.00 to 0.02) | 0.36 (0.13–0.96) | 0.32 (0.11–0.92) c | ||
| Median 1995 Income | Quintile 5 to Quintile 1 | [$23,233, $34,279) to [$8,710, $15,184) | 2.48 (1.02–6.05) | 3.06 (1.17–8.03) d | ||
| Male Population Aged 15+ and Unemployed | Quintile 4 to Quintile 1 | [0.09, 0.13) to [0.00, 0.04) | 0.27 (0.11–0.66) | 0.24 (0.09–0.66) d | 0.50 (0.28–0.88) | 0.50 (0.27–0.92) d |
| Quintile 3 to Quintile 1 | [0.07, 0.09) to [0.00, 0.04) | 0.25 (0.10–0.61) | 0.23 (0.08–0.63) d | |||
| Quintile 2 to Quintile 1 | [0.04, 0.07) to [0.00, 0.04) | 0.37 (0.16–0.87) | 0.37 (0.14–0.95) d | |||
| Community Disorder Domain | ||||||
| Population that is Male Aged 15 to 24 | Quintile 3 to Quintile 1 | [0.06, 0.07) to [0.03, 0.06) | 2.31 (1.11–4.80 )e | 1.84 (1.18–2.88) | 1.99 (1.24–3.17) e | |
| Labour Force Participation Aged 15 to 64 | Quintile 4 to Quintile 1 | [0.69, 0.75) to [0.42, 0.57) | 2.14 (1.03–4.43) | 2.28 (1.02–5.10) d | 1.70 (1.05–2.74) | |
| Homes Needing Major Repairs | Quintile 5 to Quintile 2 | [0.13, 0.21) to [0.05, 0.07) | 0.49 (0.24–0.99) | 0.47 (0.23–0.98) e | ||
| Community Crime and Violence Domain | ||||||
| Sexual Assaults per 10,000 Persons | 9.08 to 2.03 | St. James-Assiniboia West to River Heights West | 1.21 (0.99–1.47) † | 1.25 (1.01–1.55) d | 1.12 (0.99–1.27) ‡ | 1.16 (1.02–1.32) d |
| Thefts Over $5,000 per 10,000 Persons | 7.11 to 0.35 | St. James-Assiniboia East to River East East | 1.85 (1.06–3.21) | 2.10 (1.14–3.86) d | 1.42 (0.99–2.02) † | 1.47 (1.00–2.16) d |
| Children of Birth Homes at Age 7 or 8 | ||||||
|---|---|---|---|---|---|---|
| Variable | Reference Category | Model I: null model | OR (95% CI) | |||
| Model II: addition of crime | Model III: addition of participant data | Model IV: addition of community social makeup to Model III | Model V: addition of community disorder to Model III | |||
| Homes Needing Major Repairs | Quintile 5 to Quintile 2 | 0.67 (0.30–1.50) | ||||
| Male Population Aged 15+ and Unemployed | Quintile 4 to Quintile 1 | 0.32 (0.12–0.91) | ||||
| Quintile 3 to Quintile 1 | 0.32 (0.11–0.92) | |||||
| Quintile 2 to Quintile 1 | ||||||
| Father has Asthma | Yes to No | 4.14 (2.06–8.33) | 4.22 (2.04–8.72) | 3.93 (1.90–8.11) | ||
| Not Sure to No | ||||||
| Hay Fever in Child | Yes to No | 11.36 (5.85–21.74) | 10.71 (5.37–21.35) | 11.49 (5.75–22.73) | ||
| Mold in Household 1995 | Yes to No | 7.52 (1.22–45.45) | 9.43 (1.46–62.5) | 6.45 (1.00–41.67) | ||
| Smoking in Household | Yes to No | 1.61 (0.93–1.61) † | 1.65 (0.94–2.90) † | |||
| Thefts Over $5,000 per 10,000 Persons | 7.11 to 0.35 | 1.85 (1.06–3.21) | 2.05 (1.11–3.81) | 1.82 (0.96–3.46) ‡ | 1.94 (1.00–3.71) | |
| Neighbourhood Variance (SE) | 0.12 (0.13) | 0.05 (0.11) | 0.14 (0.16) | 0.07 (0.15) | 0.11 (0.15) | |
| Median OR | 1.13 | 1.05 | 1.15 | 1.07 | 1.12 | |
| Birth and Non-Birth Home Children at Age 7 or 8 | ||||||
| Homes Needing Major Repairs | Quintile 5 to Quintile 2 | 0.75 (0.44–1.29) | ||||
| Male Population Aged 15+ and Unemployed | Quintile 4 to Quintile 1 | 0.61 (0.32–1.16) | ||||
| Quintile 3 to Quintile 1 | 0.93 (0.50–1.73) | |||||
| Quintile 2 to Quintile 1 | ||||||
| Father has Asthma | Yes to No | 2.58 (1.60–4.18) | 2.63 (1.62–4.28) | 2.50 (1.54–4.07) | ||
| Not Sure to No | 3.41 (1.75–6.65) | 3.62 (1.84–7.12) | 3.46 (1.77–6.76) | |||
| Hay Fever in Child | Yes to No | 8.70 (5.71–13.16) | 8.80 (5.76–13.45) | |||
| Mold in Household 1995 | Yes to No | |||||
| Smoking in Household | Yes to No | 1.45 (1.02–2.06) | 1.41 (0.98–2.02) ‡ | 1.43 (1.00–2.04) | ||
| Thefts Over $5,000 per 10,000 Persons | 7.11 to 0.35 | 1.42 (0.99–2.02) † | 1.46 (0.99–2.14) † | 1.46 (0.97–2.20) ‡ | 1.38 (0.91–2.11) | |
| Neighbourhood Variance (SE) | 0.05 (0.05) | 0.02 (0.04) | 0.03 (0.05) | 0.01 (0.05) | 0.04 (0.06) | |
| Median OR | 1.05 | 1.02 | 1.03 | 1.01 | 1.04 | |
4. Discussion
5. Limitations
6. Conclusions
Acknowledgments
Conflict of Interest
References
- Lee, J.T.; Son, J.Y.; Kim, H.; Kim, S.Y. Effect of air pollution on asthma-related hospital admissions for children by socioeconomic status associated with area of residence. Arch. Environ. Occup. Health 2006, 61, 123–130. [Google Scholar]
- Persky, V.W.; Slezak, J.; Contreras, A.; Becker, L.; Hernandez, E.; Ramakrishnan, V.; Piorkowski, J. Relationships of race and socioeconomic status with prevalence, severity, and symptoms of asthma in Chicago school children. Ann. Allergy Asthma Immunol. 1998, 81, 266–271. [Google Scholar] [CrossRef]
- Gupta, R.S.; Zhang, X.; Sharp, L.K.; Shannon, J.J.; Weiss, K.B. Geographic variability in childhood asthma prevalence in Chicago. J. Allergy Clin. Immunol. 2008, 121, 639–645. [Google Scholar]
- Sternthal, M.J.; Coull, B.A.; Chiu, Y.H.M.; Cohen, S.; Wright, R.J. Associations among maternal childhood socioeconomic status, cord blood IgE levels, and repeated wheeze in urban children. J. Allergy Clin. Immunol. 2011, 128, 337–345. [Google Scholar] [CrossRef]
- Bacon, S.L.; Bouchard, A.; Loucks, E.B.; Lavoie, K.L. Individual-level socioeconomic status is associated with worse asthma morbidity in patients with asthma. Respir. Res. 2009, 10, 125. [Google Scholar]
- Subbarao, P.; Becker, A.; Brook, J.R.; Daley, D.; Mandhane, P.J.; Miller, G.E.; Turvey, S.W.; Sears, M.R. Epidemiology of asthma: Risk factors for development. Expert Rev. Clin. Immunol. 2009, 5, 777–795. [Google Scholar]
- Szreter, S.; Woolcock, M. Health by association? Social capital, social theory, and the political economy of public health. Int. J. Epidemiol. 2004, 33, 650–667. [Google Scholar] [CrossRef]
- Sampson, R.J. Disparity and diversity in the contemporary city: Social (dis)order revisited. Br. J. Sociol. 2009, 60, 1–31. [Google Scholar]
- Foster, H.; Brooks-Gunn, J. Toward a stress process model of children’s exposure to physical family and community violence. Clin. Child Fam. Psychol. Rev. 2009, 12, 71–94. [Google Scholar]
- Gee, G.C.; Payne-Sturges, D. Environmental Health disparities: A framework integrating psychosocial and environmental concepts. Environ. Health Perspect. 2004, 112, 1645–1653. [Google Scholar]
- Matheson, F.I.; Moineddin, R.; Dunn, J.R.; Creatore, M.I.; Gozdyra, P.; Glazier, R.H. Urban neighborhoods, chronic stress, gender and depression. Soc. Sci. Med. 2006, 63, 2604–2616. [Google Scholar] [CrossRef]
- Steptoe, A.; Feldman, P.J. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann. Behav. Med. 2001, 23, 177. [Google Scholar]
- Myers, T.; Tomasio, L. Asthma: 2015 and Beyond. Respir. Care 2011, 56, 1389–1410. [Google Scholar]
- Hwang, B.F.; Lee, Y.L.; Lin, Y.C.; Jaakkola, J.J.K.; Guo, Y.L. Traffic related air pollution as a determinant of asthma among Taiwanese school children. Thorax 2005, 60, 467–473. [Google Scholar]
- Shankardass, K.; McConnell, R.S.; Milam, J.; Berhane, K.; Tatalovich, Z.; Wilson, J.P.; Jerrett, M. The association between contextual socioeconomic factors and prevalent asthma in a cohort of Southern California school children. Soc. Sci. Med. 2007, 65, 1792. [Google Scholar]
- Burra, T.A.; Moineddin, R.; Agha, M.M.; Glazier, R.H. Social disadvantage, air pollution, and asthma physician visits in Toronto, Canada. Environ. Res. 2009, 109, 567–574. [Google Scholar] [CrossRef]
- Finkelstein, M.M.; Jerrett, M.; DeLuca, P.; Finkelstein, N.; Verma, D.K.; Chapman, K.; Sears, M.R. Relation between income, air pollution and mortality: A cohort study. Can. Med. Assoc. J. 2003, 169, 397–402. [Google Scholar]
- Smargiassi, A.; Kosatsky, T.; Hicks, J.; Plante, C.; Armstrong, B.; Villeneuve, P.J.; Goudreau, S. Risk of asthmatic episodes in children exposed to sulfur dioxide stack emissions from a refinery point source in Montreal, Canada. Environ. Health Perspect. 2009, 117, 653–659. [Google Scholar]
- Henderson, C.; Roux, A.V.; David, R.J.; Kiefe, C.I.; West, D.; Williams, D.R. Neighbourhood characteristics, individual level socioeconomic factors, and depressive symptoms in young adults: The CARDIA study. J. Epidemiol. Community Health 2005, 59, 322–328. [Google Scholar] [CrossRef]
- Laraia, B.; Messer, L.; Kaufman, J.; Dole, N.; Caughy, M.; O’Campo, P.; Savitz, D. Direct observation of neighborhood attributes in an urban area of the US south: characterizing the social context of pregnancy. Int. J. Health Geogr. 2006, 5, 11. [Google Scholar]
- O’Campo, P.; Salmon, C.; Burke, J. Neighbourhoods and mental well-being: What are the pathways? Health Place 2009, 15, 56–68. [Google Scholar] [CrossRef]
- Sampson, R.J.; Morenoff, J.D.; Felton, E. Beyond social capital: spatial dynamics of collective efficacy for children. Am. Sociol. Rev. 1999, 64, 633–660. [Google Scholar]
- Wright, R.J. Health effects of socially toxic neighborhoods: The violence and urban asthma paradigm. Clin. Chest Med. 2006, 27, 413–421. [Google Scholar]
- Sternthal, M.J.; Jun, H.J.; Earls, F.; Wright, R.J. Community violence and urban childhood asthma: A multilevel analysis. Eur. Respir. J. 2010, 36, 1400–1409. [Google Scholar]
- Morello-Frosch, R.; Shenassa, E.D. The Environmental riskscape and social inequality: Implications for explaining maternal and child health disparities. Environ. Health Perspect. 2006, 114, 1150. [Google Scholar]
- Cutrona, C.E.; Wallace, G.; Wesner, K.A. Neighborhood characteristics and depression: An examination of stress processes. Curr. Dir. Psychol. Sci. 2006, 15, 188–192. [Google Scholar]
- Mulvaney, C.; Kendrick, D. Depressive symptoms in mothers of pre-school children. Soc. Psychiatry Psychiatr. Epidemiol. 2005, 40, 202–208. [Google Scholar]
- Kozyrskyj, A.L.; Mai, X.M.; McGrath, P.; HayGlass, K.T.; Becker, A.B.; MacNeil, B. Continued exposure to maternal distress in early life is associated with an increased risk of childhood asthma. Am. J. Respir. Crit. Care Med. 2008, 177, 142–147. [Google Scholar]
- Kozyrskyj, A.L.; Hayglass, K.T.; Sandford, A.J.; Parq, P.D.; Chan-Yeung, M.; Becker, A.B. A novel study design to investigate the early-life origins of asthma in children (SAGE study). Allergy 2009, 64, 1185–1193. [Google Scholar]
- Kozyrskyj, A.L.; Kendall, G.E.; Jacoby, P.; Sly, P.D.; Zubrick, S.R. Association between socioeconomic status and the development of asthma: analyses of income trajectories. Am. J. Public Health 2010, 100, 540–546. [Google Scholar]
- Farfel, A.; Tirosh, A.; Derazne, E.; Garty, B.Z.; Afek, A. Association between socioeconomic status and the prevalence of asthma. Ann. Allergy Asthma Immunol. 2010, 104, 490–495. [Google Scholar]
- Garner, R.; Kohen, D. Changes in the prevalence of asthma among Canadian children. Health Rep. 2008, 19, 45–50. [Google Scholar]
- Kozyrskyj, A.L.; Becker, A.B. Rural-urban differences in asthma prevalence: Possible explanations. J. Allergy Clin. Immunol. 2004, 113, S306. [Google Scholar]
- Gupta, R.S.; Zhang, X.; Springston, E.E.; Sharp, L.K.; Curtis, L.M.; Shalowitz, M.; Shannon, J.J.; Weiss, K.B. The association between community crime and childhood asthma prevalence in Chicago. Ann. Allergy Asthma Immunol. 2010, 104, 299–306. [Google Scholar]
- Wilkins, R. PCCF+ Version 5D User’s Guide. Automated geographic coding based on the statistics Canada postal code Conversion files, including postal codes through September 2008 (Statistics Canada, Catalogue 82F0086-XDB); Statistics Canada: Ottawa, Canada, 2009. [Google Scholar]
- City of Winnipeg Community Area Profiles. 2009. Available online: http://www.winnipeg.ca/census/2001/Community%20Area/ (accessed on 18 November 2011).
- Statistics Canada, 1996 Census of Population: All Tables, Winnipeg (157 areas) (table), 1996 Census of Population (43 Large Urban Centres, Census Tracts (neighbourhoods)) (database), Using E-STAT (distributor). Statistics Canada: Ottawa, Canada, 2009.
- Beard, J.R.; Cerda, M.; Blaney, S.; Ahern, J.; Vlahov, D.; Galea, S. Neighborhood characteristics and change in depressive symptoms among older residents of New York City. Am. J. Public Health 2009, 99, 1308–1314. [Google Scholar]
- Franzini, L.; Caughy, M.; Spears, W.; Eugenia Fernandez Esquer, M. Neighborhood economic conditions, social processes, and self-rated health in low-income neighborhoods in Texas: A multilevel latent variables model. Soc. Sci. Med. 2005, 61, 1135–1150. [Google Scholar] [CrossRef]
- Mair, C.; Diez Roux, A.V.; Morenoff, J.D. Neighborhood stressors and social support as predictors of depressive symptoms in the Chicago Community Adult Health Study. Health Place 2010, 16, 811–819. [Google Scholar]
- To, T.; Gershon, A.; Wang, C.; Dell, S.; Cicutto, L. Persistence and remission in childhood asthma: A population-based asthma birth cohort study. Arch. Pediatr. Adolesc. Med. 2007, 161, 1197–1204. [Google Scholar]
- MacLeod, K.E.; Gee, G.C.; Crawford, P.; Wang, M.C. Neighbourhood environment as a predictor of television watching among girls. J. Epidemiol. Community Health 2008, 62, 288–292. [Google Scholar]
- Lightbody, J. The reform of a metropolitan government: The case of Winnipeg, 1971. Can. Public Policy/Anal. Politiques. 1978, 4, 489–504. [Google Scholar] [CrossRef]
- Dear, M. Los Angeles and the Chicago School: Invitation to a Debate. City Community 2002, 1, 5. [Google Scholar]
- Wright, R.J.; Fisher, E.B. Putting Asthma into Context: Community Influences on Risk, Behavior, and Intervention. In Neighborhoods and Health; Ichiro, K., Lisa, F.B., Eds.; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- Wright, R.J.; Steinbach, S.F. Violence: An unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environ. Health Perspect. 2001, 109, 1085–1089. [Google Scholar]
- Wright, R.J.; Cohen, S.; Carey, V.; Weiss, S.T.; Gold, D.R. Parental stress as a predictor of wheezing in infancy. A Prospective birth-cohort study. Am. J. Respir. Crit. Care Med. 2002, 165, 358–365. [Google Scholar]
- Haczku, A.; Panettieri, R.A., Jr. Social stress and asthma: The role of corticosteroid insensitivity. J. Allergy Clin. Immunol. 2010, 125, 550–558. [Google Scholar]
- Curry, A.; Latkin, C.; Davey-Rothwell, M. Pathways to depression: The impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland, USA. Soc. Sci. Med. 2008, 67, 23–30. [Google Scholar] [CrossRef]
- Pittman, T. The Association Between Neigbourhood Stressors and Asthma Prevalence of School Children in Winnipeg. April 2011. [Google Scholar]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Pittman, T.P.; Nykiforuk, C.I.J.; Mignone, J.; Mandhane, P.J.; Becker, A.B.; Kozyrskyj, A.L. The Association Between Community Stressors and Asthma Prevalence of School Children in Winnipeg, Canada. Int. J. Environ. Res. Public Health 2012, 9, 579-595. https://doi.org/10.3390/ijerph9020579
Pittman TP, Nykiforuk CIJ, Mignone J, Mandhane PJ, Becker AB, Kozyrskyj AL. The Association Between Community Stressors and Asthma Prevalence of School Children in Winnipeg, Canada. International Journal of Environmental Research and Public Health. 2012; 9(2):579-595. https://doi.org/10.3390/ijerph9020579
Chicago/Turabian StylePittman, Tyler P., Candace I. J. Nykiforuk, Javier Mignone, Piush J. Mandhane, Allan B. Becker, and Anita L. Kozyrskyj. 2012. "The Association Between Community Stressors and Asthma Prevalence of School Children in Winnipeg, Canada" International Journal of Environmental Research and Public Health 9, no. 2: 579-595. https://doi.org/10.3390/ijerph9020579




