Current Status of HIV/AIDS in Cameroon: How Effective are Control Strategies?
Abstract
: Nearly three decades after its discovery, HIV infection remains the number one killer disease in Sub-Saharan Africa where up to 67% of the world’s 33 million infected people live. In Cameroon, based on a Demographic Health Survey carried out in 2004, the national HIV prevalence is estimated at 5.5% with women and youths being predominantly infected. Orphans and vulnerable children (OVC) from the HIV and AIDS pandemic have increased steadily over the years; hospital occupancy is estimated at about 30%, hence stretching the health system; co-infections like HIV/tuberculosis have been reported to reach 40–50% of infected cases and 95% of teachers are said not to be productive on several counts. Thus, the impact is multi-sectorial. Furthermore, the HIV epidemic in Cameroon is peculiar because of the wide HIV-1 genetic diversity of HIV-1 Group M observed with several subtypes reported (A, B, C, D, F, G, H, J, K), predominantly subtype A. There are also circulating recombinant forms, mainly CRF02_AG. In addition, HIV-1 Groups O and N have all been noted in Cameroon. These findings have great implications not only for HIV diagnosis, but also for responsiveness to therapy as well as for vaccine development. In 1986, the initial response of the Cameroon government to the increasing trends in the HIV/AIDS infection was to create a National AIDS Control Committee to coordinate a national AIDS programme. By 2000, the first National Strategic Plan was drawn for 2000–2005. The second National Strategic Plan for 2006–2010 is currently being implemented and covers various axes. Some results obtained show that there has been significantly positive outcomes noted in the various arms of intervention by the Cameroon government.Introduction
The Acquired Immuno-deficiency Syndrome (AIDS) is caused by the human immuno-deficiency virus (HIV). Since its first discovery in 1981, the HIV and AIDS pandemic has escalated over the years and today an estimated 33 million people live with the infection worldwide [1]. While HIV/AIDS is a major concern in all countries and all races of the world, it is a bigger problem in developing countries and especially of Sub-Saharan Africa (SSA), where 67% of the world’s infection is harboured. The incidence and prevalence of HIV has been compounded by socio-economic, cultural and religious factors including taboos and war. Furthermore, children have also been gravely affected, with 420,000 new infections in children under 15 years of age in 2007 alone, and 330,000 deaths in the same period, much of which was in SSA [2], with an estimated 25 million orphans projected by 2010.
Research has led to the description of two subfamilies of the HIV, HIV-1 and HIV-2. HIV-1, based on phylogenetic analysis is currently classified into three distinct groups: M (Major), O (Outlier) and N (Non-M, non-O). HIV-1 group M is most prevalent worldwide and has several subtypes (A-D, F-H, J-L) and two subsubtypes (A1 and A2; F1 and F2). Of these, subtypes A,B,C,D,F,G,H,J,K,L are reported to be present in Cameroon, with Subtype A being most prevalent [3, 4, 5]. To date, at least 34 circulating recombinant forms (CRF) of HIV have also been described, and in Cameroon, the CRF 02_AG is predominant [6, 7]. The O subtype which seems to be absent in West and East African countries is most divergent and was first described in 1990 from a Cameroonian patient [8]. Its prevalence in Cameroon has been reported to be approximately 5% [9]. The HIV-1, Subtype N was also first described in Cameroonian samples [10]. The HIV-2 subfamily currently has eight subgroups (A-H) [11] and is predominantly in West Africa [12]. Thus, there is a wide genetic diversity of HIV-1 in Cameroon. This may have great implications for diagnostic issues, vaccine development and responsiveness to therapy as there is a potential to developing natural resistance. Indeed, resistance studies in Cameroon indicate that primary resistant mutations are present in antiretroviral drug-naïve Cameroonians, mainly to Reverse Transcriptase Inhibitors and Protease Inhibitors where up to 9.8% and 7.4% respectively have been reported [6]. This may impact on future therapy with antiretroviral drugs.
Cameroon
Cameroon is situated in Central West Africa, north of the Equator. Cameroon is bounded on the North by Tchad, on the South by Gabon and Congo, on the West by Nigeria and on the East by the Central African Republic. Cameroon has a surface area of about 475,000 km2 and a population of about 16 million people and an annual growth rate of about 2.8%. Cameroon is undergoing a demographic transition and about 50% of the population now lives in urban areas. Administratively, the country is divided into 10 provinces headed by governors. Each province is divided into divisions, divisions into subdivisions and subdivisions into districts. Yaoundé is the administrative capital of Cameroon and is in the Central Province of the country. Its economic capital is situated in Douala and the average income per capita over the last five years ranges from US$ 600–650.
The Ministry of Public Health co-ordinates all health services in the country. According to a Ministry of Health report in 2002, the health system is organised at three levels: central, intermediate and peripheral. The Central level has three reference health institutions of Category I and three of Category II institutions. Of the Intermediary level are nine provincial hospitals and affiliated health structures. Peripheral institutions are health districts. In Cameroon, in 2002, there were 150 such health districts and 1,388 health centers [13]. Currently there is an estimated 174 health districts in Cameroon. Among the rest, some are under the auspices of private institutions and religious missions.
There is a national public health emphasis on preventive medicine and preventive health services are available throughout the country to complete this national health structure. The national social insurance scheme in Cameroon does not cover the health service; patients have to pay for every aspect of services rendered.
HIV Situation in Cameroon
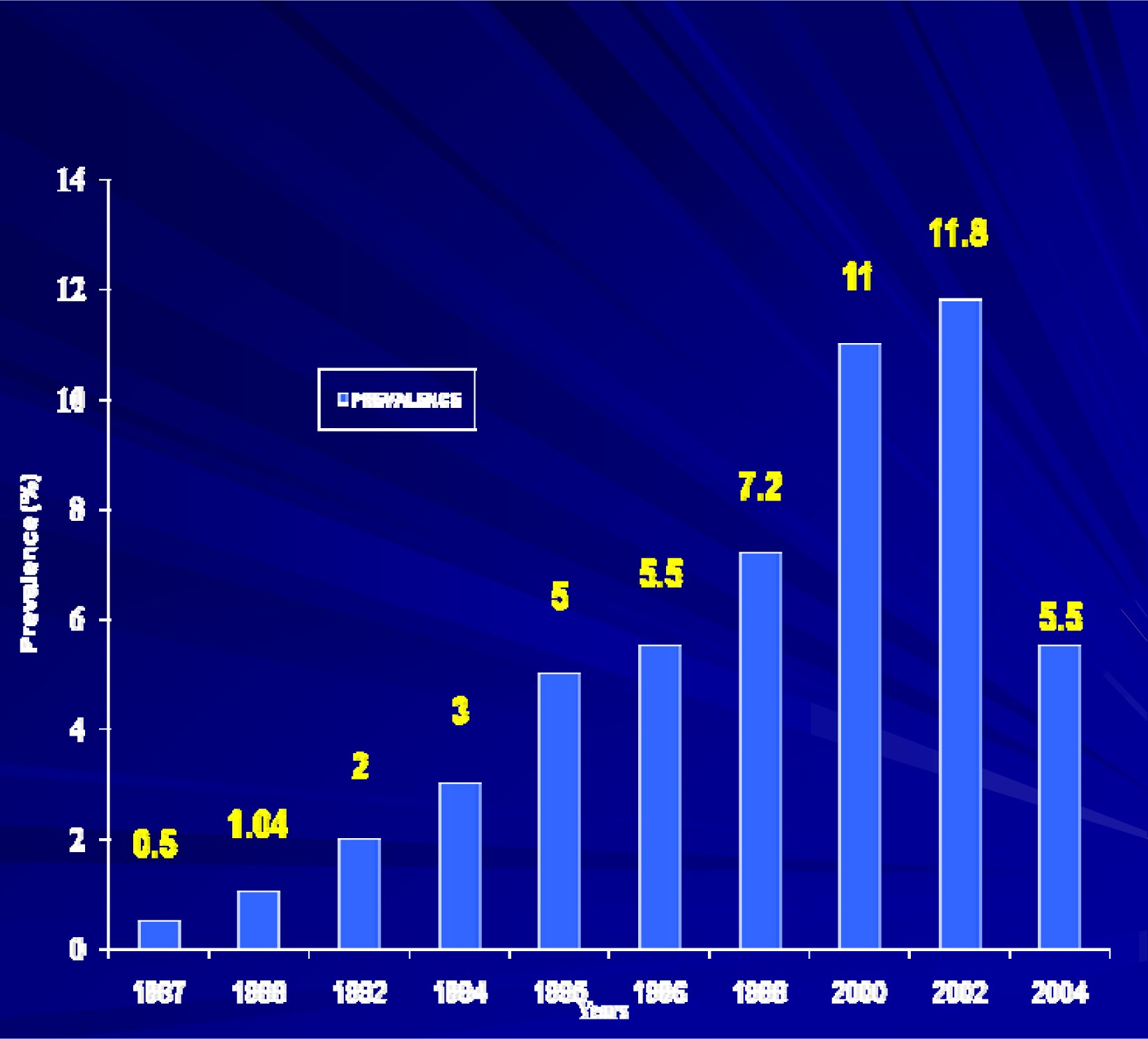
The first AIDS cases were reported in Cameroon in 1985 and ten years later, in 1995, an official total of 2766 had been notified with a cumulative number of 8,141 [14]. Similarly the prevalence of the HIV infection in Cameroon has progressively risen from 0.4% in 1987 to 1.2% in 1990 [15] and from 4% in 1992 [16] to about 7% in 1997, to 11% in 2000 [17] and today, the national prevalence stands at 5.5% based on a Demographic and Health Survey carried out in 2004 [18] - Figure 1. This figure shows a steady rise in the HIV prevalence from 0.5% in 1987 to 11.8% in 2002. In 2004, there is a huge drop observed, to 5.5%. This is explained by the fact that the data from 1987 to 2002 was obtained from sentinel surveillance in antenatal clinics throughout the nation, whereas in 2004 it was a demographic and health survey of various strata of the general population, including university students, commercial sex workers, long distance drivers and others. Transmission is mainly heterosexual (90%) with the blood and vertical routes being 5% respectively.
In the earlier years, more than 70% of the infected people were aged between 20 and 39 years [15], the work force of the country. Today, youths are still the most infected and those in the 15–24 year age group are hard hit, with the girls infected constituting 10–15%, compared to 4–6.5% of boys of the same age. There is no doubt that the socio-economic impact on this society is profound with growing numbers of sectors being affected, and high hospital bed occupancy rampant, resulting in an over-stretched medical personnel and an extra burden to the health system. School teachers are reported to be unproductive on several counts and morbidity is high from opportunistic such as tuberculosis. Furthermore, there is a rising number of orphans from the HIV pandemic, with 122,670 cases reported in 2005 [19].
Trends in General Population
Gender
As is the tendency in SSA, the Cameroonian woman is more infected than the man, constituting about 55% of cases. According to the DHS in 2004 [18], HIV infection was detected in 6.8% females, compared to 4.1% males. This trend in women is also observed when other variables are examined including marital and educational status. Several factors contribute to the Cameroonian woman and the African woman on the whole, being more vulnerable to the infection. These may include socio-cultural factors and gender-related norms, poor educational and healthcare access, especially for treatment of sexually transmitted infections (STI) as well as the lack of reproductive and sexual rights, with women being mostly economically dependent on men, and hence with little negotiating power. In fact, it has been suggested that gender may be a single most important determinant of the HIV and AIDS epidemic. Figure 2 shows the prevalence of HIV among women in the various provinces of Cameroon. There is no data published in Cameroon on men having sex with men, but anecdotal evidence suggests that the practice is now existent in Cameroon.
Children
There were about 45,000 children reported to be living with HIV and AIDS in Cameroon in 2001, and a drop was noted in 2005 to 35,000 children. The numbers of AIDS orphans was 122,670 in 2005. Most children are believed to acquire the infection during pregnancy and breastfeeding. Indeed several studies have confirmed that mother-to-child transmission of HIV is a primary route of infection in SSA, accounting for up to 90–95% transmissions. An estimated 1,600 children are infected daily by their mothers and without any intervention, 30–40% of breastfeeding mothers transmit to their babies [20]. This can be explained by the high rate of infection in the women and the efficiency of mother-to-child transmission of the infection. In a study in Cameroon by Kouam et al.[21], mother-to-child transmission was estimated at 11.1% in mothers who had been put on the recommended single dose of Nevirapine at the onset of labour, as well as for their neonates within 72 hours of delivery. Transmission in these children may also occur through the sexual route, mainly through sexual abuse, rampant amongst orphans and through the blood route (unsterile injections, unsafe transfusions and scarifications).
Risk Groups
The trends of the infection have also been reported in various target groups of the population including commercial sex workers, long distance lorry drivers, uniformed officers and tuberculosis patients. In some of these groups, the HIV prevalence has been as high as 40–50%. In one study looking at HIV infection in specific subpopulations of Cameroon [22], a prevalence of 26.4%, 19.9% and 16.3% was respectively observed in female commercial sex workers, residents along the Chad-Cameroon petroleum pipeline and long distance truck drivers. In the same analysis, lower prevalences were noted in health care personnel (5.2%) and university students (3.8%). These findings confirm the need for expanded prevention and care programmes for high risk groups of the community.
Government Interventions and Outcomes
The first important government intervention against the HIV epidemic in Cameroon was the creation of the National AIDS Control Committee (NACC) in 1986, to coordinate AIDS programmes nationally. The World Health Organisation/Global Programme on AIDS (WHO/GPA) plan was first introduced in Cameroon in 1987, and in 1991 the NACC was made a branch of Preventive Medicine in the Ministry of Public Health.
The first Strategic Plan for Cameroon covered 2000–2005. This plan included the strategies for the prevention of the transmission of STI/AIDS with emphasis on women of childbearing ages, prevention of mother-to-child transmission and the prevention of HIV transmission through blood (enhancing blood safety). The management of already infected cases was enabled through the enhancing of access to treatment and care (referrals to certified treatment centres) and programmes to protect and promote the rights of PLWHA were some of the strategies. Furthermore, the promotion of research as well as strategies for the coordination of the programme throughout the national territory were established and implemented.
The second national Strategic Plan for 2006–2010 focused on six aspects: Universal access to HIV prevention in targeted groups; Universal access to treatment for adults and children living with HIV; Protection and support to AIDS orphans and vulnerable children (OVC); Involvement of all stakeholders in the fight against HIV and AIDS; Epidemiological surveillance and research promotion as well as the Reinforcement and coordination and management of the programme, partnerships and the monitoring and evaluation of its implementation.
Effectiveness of Current Strategic Plan
Universal Access to HIV prevention
The strategies employed to promote access to prevention for all included the increase in the number of fixed & mobile voluntary counseling and testing (VCT) units, prevention and treatment of STI and the promotion of the use of both male and female condoms. With reference to the increasing numbers of people being tested for HIV infection, it is of interest to note that there is also a high percentage of those returning to collect their results in all the provinces where testing has occurred, with an overall rate of those not returning of about 4.2% [23]. In addition the prevention of mother-to-child transmission of HIV, the promotion of blood safety as well as of youth programmes, has also all been employed. Table 1 shows the details of progress made in achieving this plan.
Universal Access to Treatment and Care
One useful strategy implemented by the Cameroonian government has been the decentralisation of HIV and AIDS management units through the creation of certified treatment centers (CTC) throughout the national territory. In 2005 40 CTC existed, covering 14 of the 174 existing health districts, and by 2007 there were 113 CTC, covering 82 districts, thus enhancing access to care for the population.
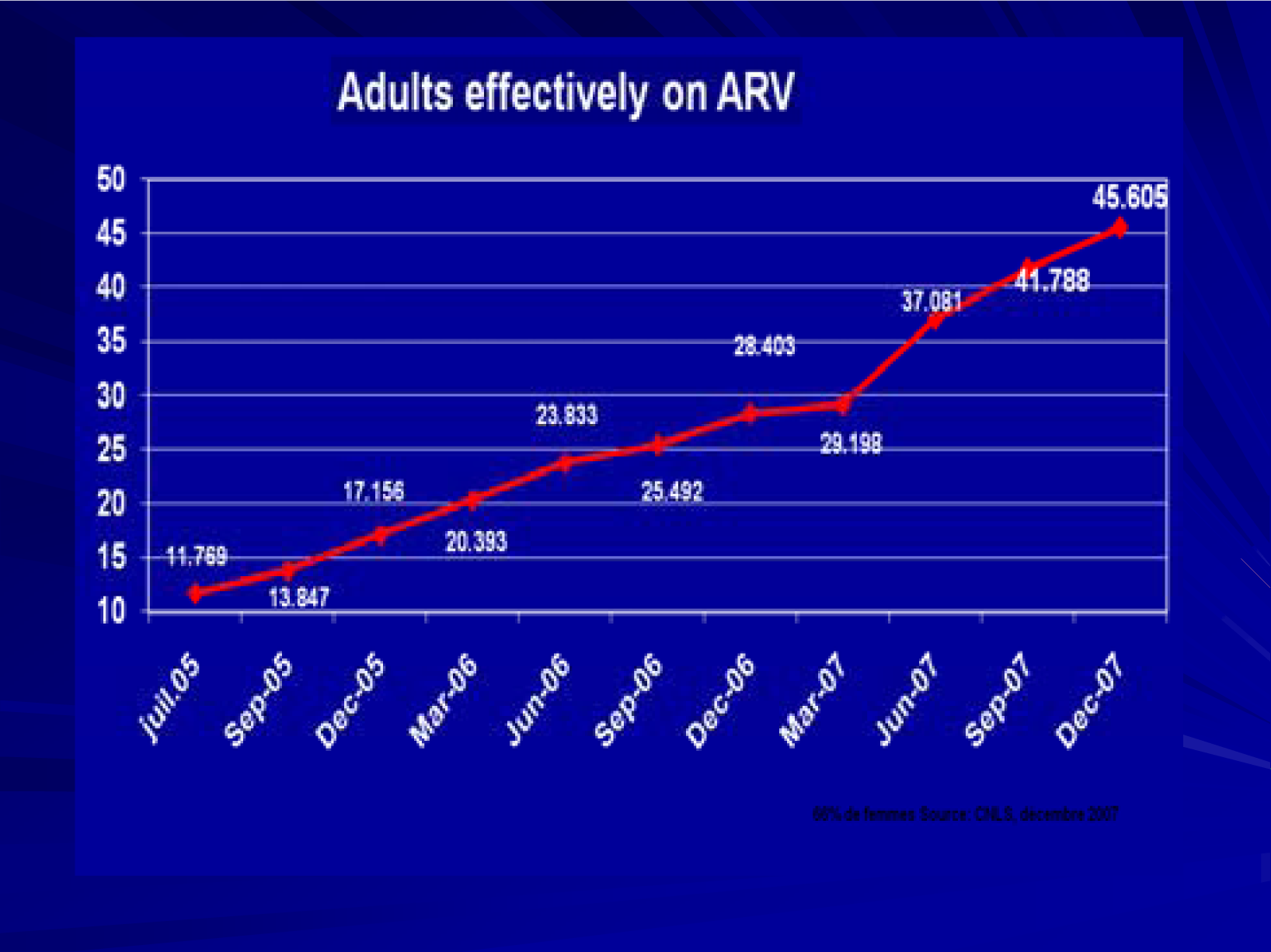
The access to treatment and care has been mostly supported by the Cameroon Government, Global Funds for AIDS, Tuberculosis and Malaria (GFATM) and to some extent by other agencies. According to the Report by the National AIDS Control Committee in 2008 [23], the GFATM has supported this since 1st January 2005, renewed in February, 2007 for a period of three years. The Clinton Foundation also supports second line ARV for adults and first and second line ARV for children. The National AIDS Control Committee also estimates that 510,000 people are currently living with HIV and AIDS in Cameroon, of which 91,453 are said to be eligible for treatment with antiretroviral (ARV) drugs. In December 2006, there were 28,403 patients on ARV and by December 2007 the number effectively on treatment had reached 45,605 (49.9%), an increase by 61%. About 6.2% had been lost either through death (2.2%) or totally lost to follow up (4.0%) - See Figure 3. A similar trend has also been observed in paediatric cases with 1001 on ARV in December 2006 and 1700 by December 2007, an increase by approximately 70%.
Concerning opportunistic infections there has been a steady rise in the numbers with access to free cotrimoxazole (16,534 in 2006 compared to 57,550 in 2007) and in those on free treatment for Cryptococcus and cerebral toxoplasmosis (119 in 2006 and 454 in 2007).
In order to ease patient monitoring and treatment, there has been marked capacity building and recruitment of psychosocial staff (184 in 2005 and total of 508 by 2007); subsidized laboratory testing packages (for CD4 counts, full blood counts, fasting blood sugar and liver enzymes is one package that costs 3000Frs CFA -approximately $7 USD) and health systems reinforcement through the provision of equipment to the health institutions (spectrophotometers, flow cytometres, electronic counters etc.). Furthermore, in 2007, a nutritional support programme was implemented for which 120 personnel has already been trained.
Protection and Support to OVC
In 2006, taking into consideration all categories of OVC, there were 183, 523 identified for assistance by the NACC, of which assistance was provided to 25,643 (14%). In 2007, assistance was given to 43,505 of them, an increase by 69.6%. However, when AIDS orphans were examined, 12,776 and 28,319 (121.7% rise) were respectively catered for in 2006 and 2007.
Involvement of all Stakeholders
The program has involved various categories of stakeholders, assisting them technically and financially in anti-AIDS activities. For example in 2006, 130 associations of PLWHA were sponsored and in 2007 there were 101 sponsored. Religious organizations, believed to promote moral education also received financial support in 2007. Opinion leaders including political leaders, traditional chiefs, administrative authorities have been implicated, and the public sector (Government and private structures, firms, NGOs, International partners including WHO, UNICEF,UNAIDS, World Bank, CDC, French Cooperation, UNESCO, UNDP, CARE, GTZ, PLAN International etc.) have all collaborated in the achievement of success in the implementation of this plan. The role of the media cannot be overemphasized.
Epidemiological Surveillance and Research Promotion
Epidemiological surveillance has mainly consisted in the notification of new cases. For example in 2006 there were 8,569 new cases notified, compared to 10,625 new cases in 2007.
The major research projects have covered: Virological studies including resistance studies; mother-to-child transmission of HIV; Clinical & epidemiological research; Social science aspects as well as Public health research. Some of the major institutions involved in the various arms of research include the National AIDS Control Committee, the Faculty of Medicine and Biomedical Sciences and other Faculties of Cameroonian Universities, the Institute Pasteur in Cameroon, the French National Agency for AIDS Research, CRESAR, CDC Atlanta, the Chantal Biya International Research Centre, and others. A lot of data is being generated & disseminated in various ways both nationally and internationally, some of which has been used to implement policy. For example, in studies demonstrating that there was no correlation between total lymphocyte counts and CD4 counts in HIV infected persons in our community, equipment for CD4 counts have been made available in most major health institutions of the country. The results of several studies on the genetic diversity of HIV in Cameroon as well as on primary and secondary drug resistance to ARV have all contributed significantly to policies and access to second line therapy in the country. Furthermore, several HIV prevention and care programmes have targeted specific groups based on the high prevalence of the infection reported from research and surveillance carried out in such groups.
Conclusions
The Cameroon government in its effort to curb the HIV and AIDS pandemic has achieved a lot barely midway into the implementation of the second national strategic plan. Since 2006, there has been a lot of scaling up of institutions both in equipment and human resources as well as in minimum packages for various services.
There has been systematic proposals of free HIV testing to all pregnant women and children less than 15 years; early diagnosis in neonates less than 18 months is performed by molecular biology techniques while the rest of the population pay 500 Frs CFA (∼$1.1 USD) for HIV testing. In addition, it is now possible to refer all patients to appropriate treatment centers after CD4 and total; lymphocyte counts have been measured.
Furthermore, family planning for any unwanted pregnancies is provided in many centers as well as nutritional counseling for parents of neonates.
Stepwise progress has been made over the years, from a pilot phase through an initial extension phase and then a scaling up phase, with the implication of international organisms and communities. Although the overall negative impact of HIV/AIDS has been devastating, there is a lot of government commitment, a key determinant to success.
References
- 2008 Report on the global HIV/AIDS epidemic; UNAIDS/WHO: Geneva, Switzerland, 2008.
- 2007 Report on the global HIV/AIDS epidemic; UNAIDS/WHO: Geneva, Switzerland, 2007.
- Fonjungo, P; Mpoudi, EN; Torimiro, JN; Alemnji, GA; Eno, T; Lyonga, J; Nkengasong, JN; Lal, RB; Rayfield, M; Kalish, L; Folks, TM; Pieniazek, D. Human immunodeficiency virus type 1 group M protease in Cameroon: genetic diversity and protease inhibitor mutational features. J. Clin. Microbiol. 2002, 40, 837–845. [Google Scholar]
- Ndembi, N; Takehisa, J; Zekeng, L; Kobayashi, E; Ngansop, C; Songok, EM; Kageyama, S; Takemura, T; Ido, E; Hayami, M; Kaptue, L; Ichimura, H. Genetic diversity of HIV type 1 in rural eastern Cameroon. J. Acquir. Immune. Defic. Syndr. 2004, 37, 1641–1650. [Google Scholar]
- Ndongmo, CB; Pieniazek, D; Holberg-Petersen, M; Holm-Hansen, C; Zekeng, L; Jeansson, L; Kaptue, L; Kalish, ML. HIV genetic diversity in Cameroon: possible public health importance. AIDS Res. Hum. Retrovir. 2006, 22, 812–816. [Google Scholar]
- Koizumi, Y; Ndembi, N; Miyashita, M; Lwembe, R; Kageyama, S; Mbanya, D; Kaptue, L; Numazaki, K; Fujiyama, Y; Ichimura, H. Emergence of antiretroviral therapy resistance-associated primary mutations among drug-naive HIV-1-infected individuals in rural Western Cameroon. J. Acquir. Immune. Defic. Syndr. 2006, 43, 15–22. [Google Scholar]
- Ndembi, N; Abraha, A; Pilch, H; Ichimura, H; Mbanya, D; Kaptue, L; Salata, R; Arts, EJ. Molecular characterization of HIV-1 and HIV-2 in Yaoundé, Cameroon: Evidence of major drug resistance mutations in newly diagnosed patients infected with subtypes other than subtype B. J. Clin. Microbiol. 2008, 46, 177–184. [Google Scholar]
- Vanden Haesevelde, M; Decourt, JL; De Leys, RJ; Vanderborght, B; van der Groen, G; van Heuverswijn, H; Saman, E. Genomic cloning and complete sequence analysis of a highly divergent African human immunodeficiency isolate. J. Virol. 1994, 68, 1586–1596. [Google Scholar]
- Nkengasong, JN; Peeters, M; vanden Haesevelde, M; Musi, SS; Willems, B; Ndumbe, PM; Delaporte, E; Perret, JL; Piot, P; van den Groen, G. Antigenic evidence of the presence of the abberant HIV-1 ANT 70 virus in Cameroon and Gabon. AIDS 1993, 7, 1536–1538. [Google Scholar]
- Simon, F; Mauclère, P; Roques, P; Loussert-Ajaka, I; Müller-Trutwin, MC; Saragosti, S; Georges-Courbot, MC; Barré-Sinoussi, F; Brun-Vézinet, F. Identification of a new Human Immunodeficiency Virus type 1 Distinct from Group and Group O. Nature Med. 1998, 4, 1032–1037. [Google Scholar]
- Damond, F; Worobey, M; Campa, P; Farfara, I; Colin, G; Matheron, S; Brun-Vezinet, F; Robertson, RI; Simon, F. Identification of a highly divergent HIV-2 and proposal for a change in HIV-2 classification. AIDS Res. Human. Retrovir. 2004, 20, 666–672. [Google Scholar]
- DeCock, KM; Adjorlolo, G; Ekpini, E; Sibailly, T; Kouado, J; Maran, M; Brattegaard, K; Vetter, KM; Doorly, R; Gayle, HD. Epidemiology and transmission of HIV-2: Why there is no HIV-2 pandemic. JAMA 1993, 270, 2083–2086. [Google Scholar]
- 2002.
- Mbopi Kéou, FX; Mpoudi-Ngollé, E; Nkengasong, J; Zekeng, L; Mbanya, D; Affana, G; Mauclère, P; Monny Lobé, M; Tapko, JB; Ndumbe, P. Trends of AIDS epidemic in Cameroon, 1986 through 1995. J. Acq. Immuno. Defic. Syndr. Hum. Retrovir. 1998, 18, 89–91. [Google Scholar]
- Garcia-Calleja, JM; Mvondo, JL; Sam Abbenyi, S; Zekeng, L; Loius, JP; Trebucq, A; Kaptue, L. Profil de l’épidémie VIH/SIDA au Cameroun. Bull. Liais. Doc. OCEAC 1992, 99, 31–33. [Google Scholar]
- Garcia-Calleja, JM; Abbenyi, S. Review of HIV prevalence studies in Cameroon. AIDS Inform. Bull. 1993, 1, 5–6. [Google Scholar]
- Sentinel Surveillance of the Ministry of Public Health; Cameroon, 2000.
- Institut National de la Statistique Enquête Demographique et de Santé Cameroun 2004. http://www.measuredhs.com/countries/, accessed April 15, 2008.
- National AIDS Control Committee’s Annual Reports; Cameroon, 2005.
- Iliff, PJ; Piwoz, EG; Tavengwa, NV; Zunguza, CD; Marinda, ET; Nathoo, KJ; Moulton, LH; Ward, BJ; Humphrey, JH; ZVITAMBO study group. Early exclusive breastfeeding reduces the risk of postnatal HIV-1 transmission and increases HIV-free survival. AIDS 2005, 19, 699–708. [Google Scholar]
- Kouam, L; Nsangou, I; Mbanya, D; Nkam, M; Kongnyuy, EJ; Ngassa, P; Tebeu, PM; Elobe, N; Kamgaing, NG; Zekeng, L; Doh, AS. Prevention of mother-to-child transmission of HIV in Cameroon: experiences from the University Teaching Hospital in Yaounde (Cameroon). Zentralbl. Gynakol. 2006, 128, 82–86. [Google Scholar]
- Musoko, JJ; Macauley, IB; Zoungkanyi, AB; Assumpta, Bella; Koulla-Shiro, S. Human Immunodeficiency Virus infection and associated factors among specific population subgroups in Cameroon. AIDS Behav 2007, 9294–9298. [Google Scholar] [CrossRef]
- Comité National de Lutte contre le SIDA (Groupe Technique Central): Rapport annuel d’activités du Programme National de Lutte contre le SIDA, 2007. Yaoundé, Mars 2008..

| Activity | Outcome in 2006 | Outcome in 2007 |
|---|---|---|
| Fixed and Mobile VCT units | 179, 266 tested | 573,875 tested |
| % not collecting results | Not available | 4.2 |
| 22,789 STI treated | ||
| Prevention and treatment of STI | Not available | 254 counselors trained |
| 30 nurses recruited to STI sites | ||
| Condom distribution | ||
| Male | 33,242,888 | 29,752,819 |
| Female | 130,264 | 80,730 |
| Blood safety (units collected) | 26,079 | 61,388 |
| PMTCT (antenatal testing) | 90,238 | 209,037 |
| Youth (15 – 24 years) | UNESCO, UNICEF National programme on Adolescent Reproductive Health; Interventions of various ministries (Basic Education, Health, Communication…) | |
| Preventing new infections in women (outreach programmes) | Capacity building/reinforcement of women in various capacities, groups and levels (CSW, NGO, cultural groups…) | |
© 2008 MDPI All rights reserved.
Share and Cite
Mbanya, D.; Sama, M.; Tchounwou, P.B. Current Status of HIV/AIDS in Cameroon: How Effective are Control Strategies? Int. J. Environ. Res. Public Health 2008, 5, 378-383. https://doi.org/10.3390/ijerph5050378
Mbanya D, Sama M, Tchounwou PB. Current Status of HIV/AIDS in Cameroon: How Effective are Control Strategies? International Journal of Environmental Research and Public Health. 2008; 5(5):378-383. https://doi.org/10.3390/ijerph5050378
Chicago/Turabian StyleMbanya, Dora, Martyn Sama, and Paul B. Tchounwou. 2008. "Current Status of HIV/AIDS in Cameroon: How Effective are Control Strategies?" International Journal of Environmental Research and Public Health 5, no. 5: 378-383. https://doi.org/10.3390/ijerph5050378




