Evaluation of a Novel Classification of Heat-Related Illnesses: A Multicentre Observational Study (Heat Stroke STUDY 2012)
Abstract
:1. Introduction
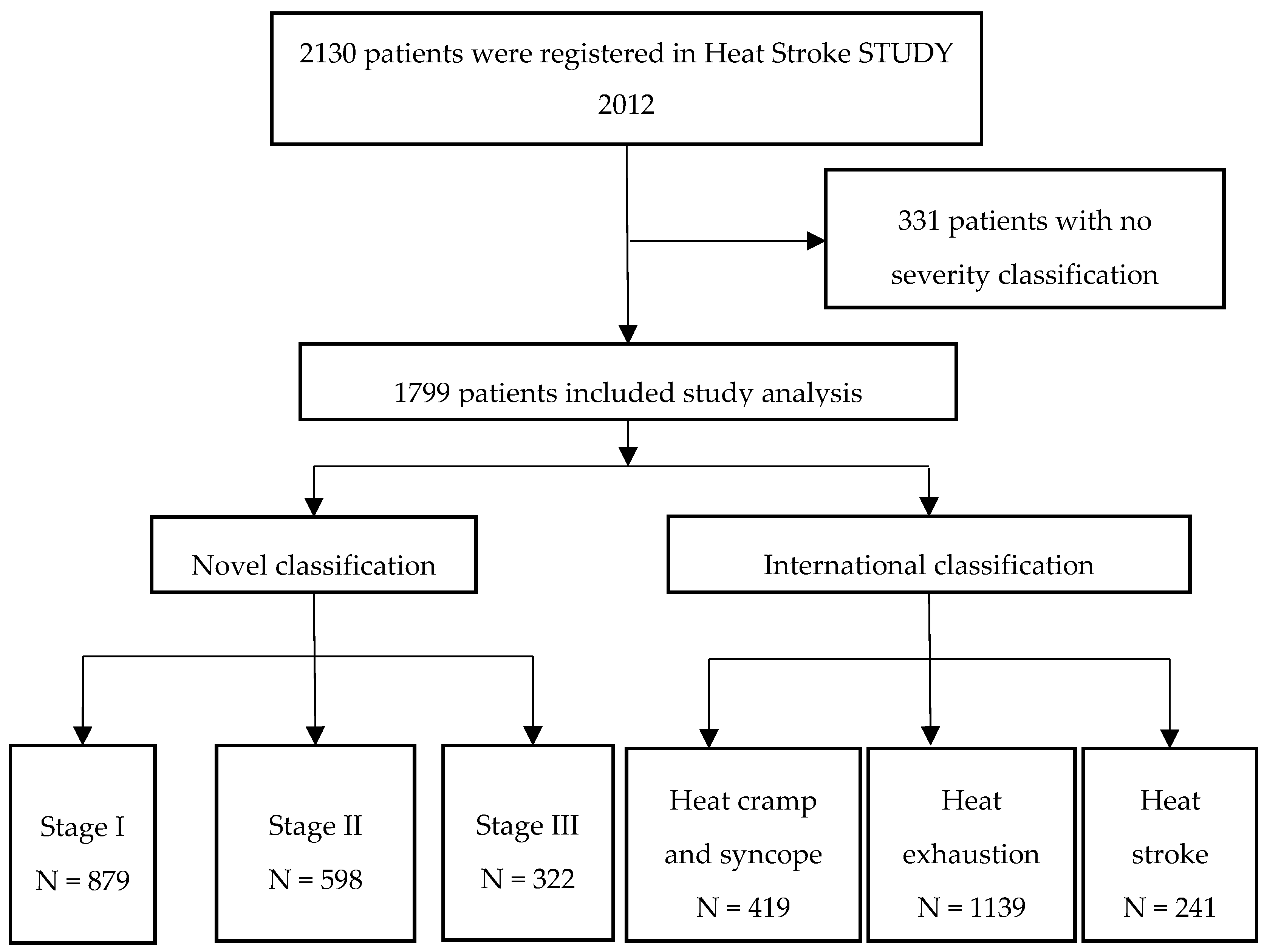
2. Materials and Methods
2.1. Study Overview
2.2. Data Collection
2.3. Statistical Analyses
3. Results
3.1. Changes in Air Temperature During the Study Period
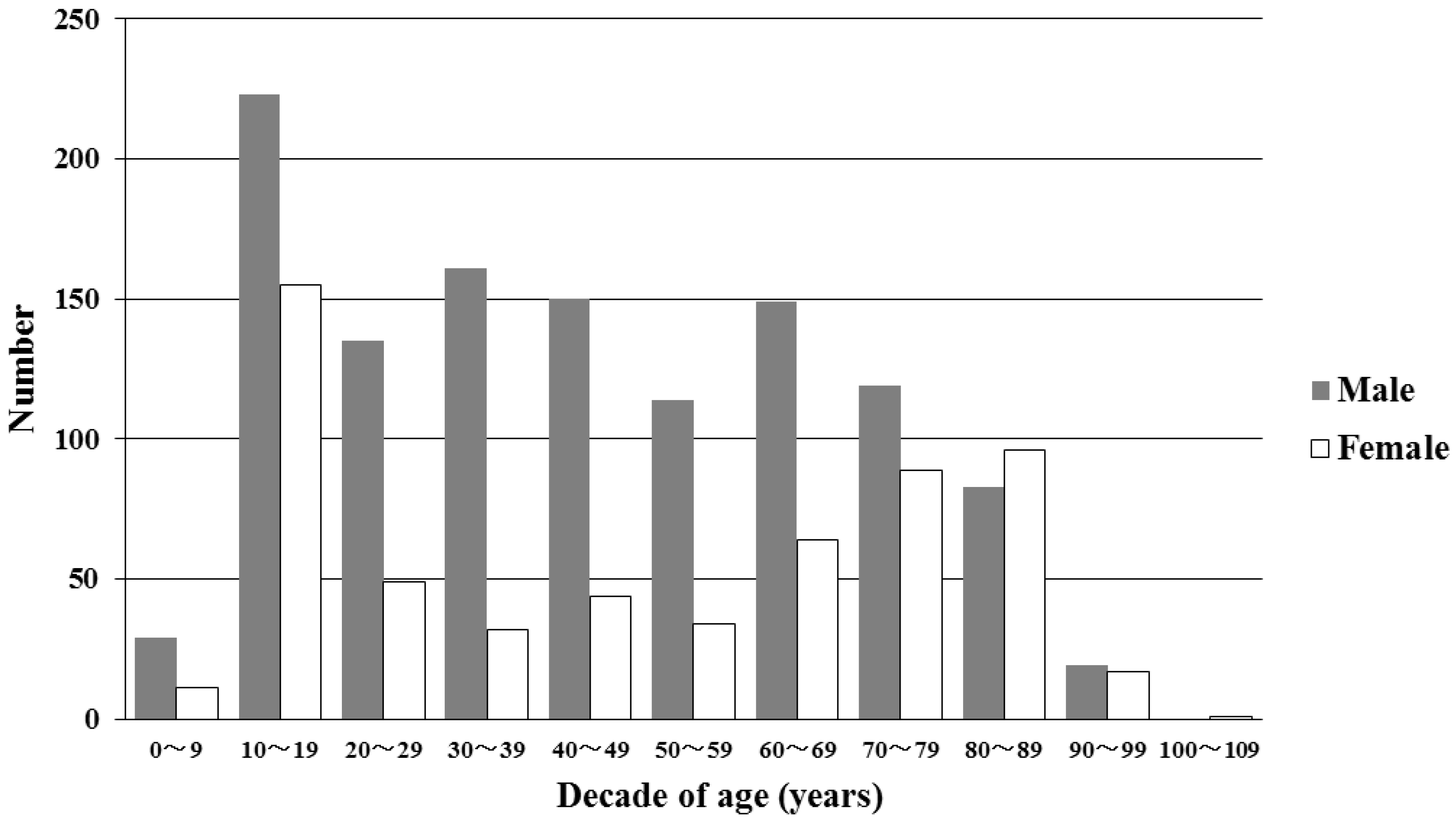
3.2. Demographic Data of Patients with Heat-Related Illness
3.3. Comparison of Heat-Related Illness Severity Diagnosed with the Novel Classification and the International Classification
3.4. Comparisons of Blood Test Data
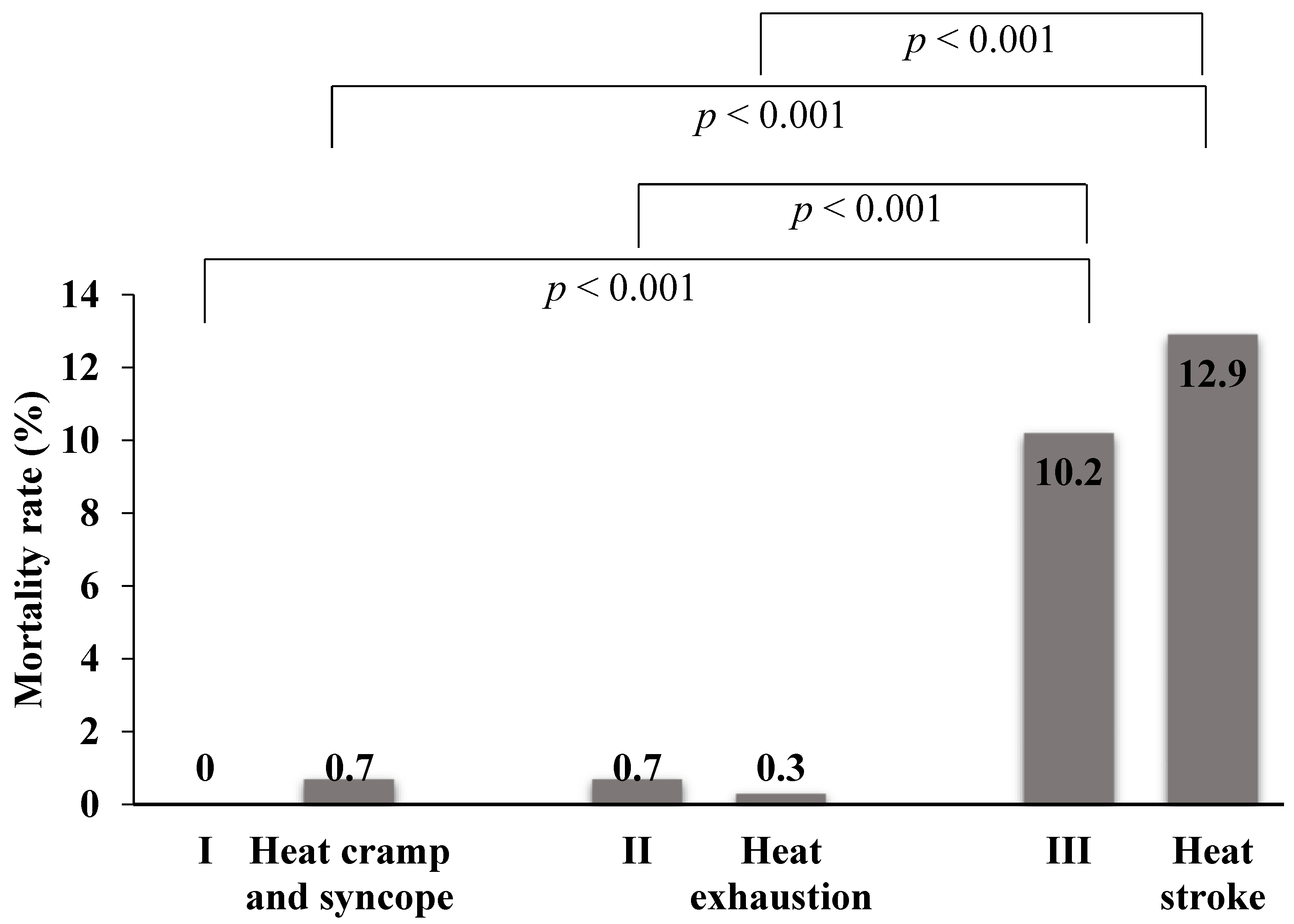
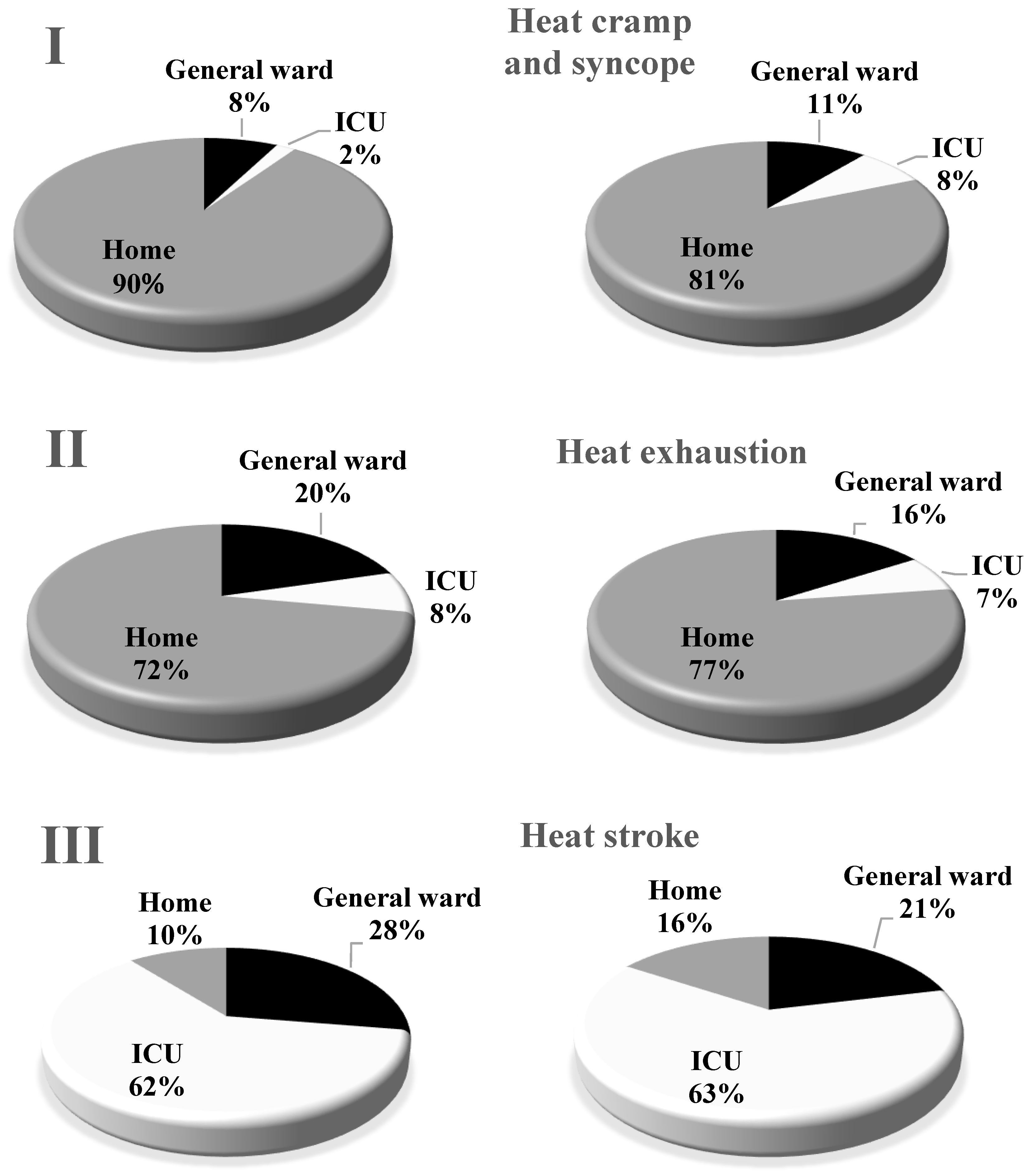
3.5. Outcomes of Patients with Heat-Related Illnesses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
References
- Bouchama, A.; Knochel, J.P. Heat stroke. NeW Eng. J. Med. 2002, 346, 1978–1988. [Google Scholar] [CrossRef] [PubMed]
- Platt, M.; Vicario, S. Heat Illness: Rosen’s Emergency Medicine. Concepts and Clinical Practice; Mosby Elsevier: Philadelphia, PA, USA, 2010. [Google Scholar]
- Shapiro, Y.; Seidman, D.S. Field and clinical observations of exertional heat stroke patients. Med. Sci. Sports Exercise 1990, 22, 6–14. [Google Scholar] [CrossRef]
- Yamamoto, T.; Todani, M.; Oda, Y.; Kaneko, T.; Kaneda, K.; Fujita, M.; Miyauchi, T.; Tsuruta, R. Predictive factors for hospitalization of patients with heat illness in Yamaguchi, Japan. Int. J. Environ. Res. Public Health 2015, 12, 11770–11780. [Google Scholar] [CrossRef] [PubMed]
- Hifumi, T.; Kondo, Y.; Shimazaki, J.; Oda, Y.; Shiraishi, S.; Wakasugi, M.; Kanda, J.; Moriya, T.; Yagi, M.; Ono, M.; et al. Prognostic significance of disseminated intravascular coagulation in patients with heat stroke in a nationwide registry. J. Crit. Care 2018, 44, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Past Climate Data and Download. Japan Meteorological Agency. Available online: http://www.data.jma.go.jp/gmd/risk/obsdl/index.php (accessed on 10 July 2018).
- Knaus, W.A.; Draper, E.A.; Wanger, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Past Emergency Transportation Data of Heat Illness Patients and Download. Japan Fire and Disaster Management Agency. Available online: http://www.fdma.go.jp/neuter/topics/fieldList9_2.html (accessed on 10 July 2018).
- Shibolet, S.; Lancaster, M.C.; Danon, Y. Heat stroke: A review. Aviat. Space Environ. Med. 1976, 47, 280–301. [Google Scholar] [PubMed]
- Shibolet, S. The clinical picture of heat stroke. Proc. Tel-Hashomer Hosp. 1962, 1, 80–83. [Google Scholar]
- Yasuoka, S.; Aruga, T.; Toyota, I.; Kitahara, T.; Sakamoto, T.; Okudera, T.; Tomita, H.; Ueda, M.; Inoue, T.; Kimura, Y.; et al. Heat illness grade III syndrome: New diagnostic criteria of heat stroke (heat illness grade III). J. Jpn. Congr. Neurol. Emerg. 2003, 16, 5–9. (In Japanese) [Google Scholar]
- Glazer, J.L. Management of heatstroke and heat exhaustion. Am. Fam. Physician 2005, 71, 2133–2140. [Google Scholar] [PubMed]
- Leon, L.R.; Helwig, B.G. Heat stroke: Role of the systemic inflammatory response. J. Appl. Physiol. 2010, 109, 1980–1988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lambert, G.P. Intestinal barrier dysfunction, endotoxemia, and gastrointestinal symptoms: The ‘canary in the coal mine’ during exercise-heat stress? Med. Sports Sci. 2008, 53, 61–73. [Google Scholar]
- Krau, S.D. Heat-related illness: A hot topic in critical care. Crit. Care Nurs. Clin. N. Am. 2013, 25, 251–262. [Google Scholar] [CrossRef] [PubMed]
- Junglee, N.A.; Di Felice, U.; Dolci, A.; Fortes, M.B.; Jibani, M.M.; Lemmey, A.B.; Walsh, N.P.; Macdonald, J.H. Exercising in a hot environment with muscle damage: Effects on acute kidney injury biomarkers and kidney function. Am. J. Physiol. Renal Physiol. 2013, 305, F813–F820. [Google Scholar] [CrossRef] [PubMed]
- De Meijer, A.R.; Fikkers, B.G.; De Keijzer, M.H.; Van Engelen, B.G.; Drenth, J.P. Serum creatine kinase as predictor of clinical course in rhabdomyolysis: A 5-year intensive care survey. Intens. Care Med. 2003, 29, 1121–1125. [Google Scholar] [CrossRef] [PubMed]
- Kahanov, L.; Eberman, L.E.; Wasik, M.; Alvey, T. Exertional rhabdomyolysis in a collegiate American football player after preventive coldwater immersion: A case report. J. Athl. Train. 2012, 47, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Wappler, F.; Fiege, M.; Steinfath, M.; Agarwal, K.; Scholz, J.; Singh, S.; Matschke, J.; Schulte, J.; am Esch, J. Evidence for susceptibility to malignant hyperthermia in patients with exercise-induced rhabdomyolysis. Anesthesiology 2001, 94, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Hausfater, P.; Hurtado, M.; Pease, S.; Juillien, G.; Lvovschi, V.E.; Salehabadi, S.; Lidove, O.; Wolff, M.; Bernard, M.; Chollet-Martin, S.; et al. Is procalcitonin a marker of critical illness in heatstroke? Intens. Care Med. 2008, 34, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Nylén, E.S.; Al Arifi, A.; Becker, K.L.; Snider, R.H., Jr.; Alzeer, A. Effect of classic heatstroke on serum procalcitonin. Crit. Care Med. 1997, 25, 1362–1365. [Google Scholar]
- Tong, H.S.; Liu, Y.S.; Wen, Q.; Tang, Y.Q.; Yuan, F.F.; Su, L. Serum procalcitonin predicting mortality in exertional heatstroke. Emerg. Med. J. 2012, 29, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Miyake, Y.; Aruga, T.; Inoue, K.; Okudera, H.; Kitahara, T.; Shimazaki, S.; Tsuruta, R.; Maekawa, T.; Yokota, H. Heat stroke STUDY 2006 in Japan. J. Jpn Assoc. Acute Med. 2008, 19, 309–321. (In Japanese) [Google Scholar]
- Miyake, Y.; Aruga, T.; Inoue, K.; Okudera, H.; Kitahara, T.; Shimazaki, S.; Tsuruta, R.; Yokota, H. Heat stroke STUDY 2008 in Japan. J. Jpn Assoc. Acute Med. 2010, 21, 230–244. (In Japanese) [Google Scholar]
- Miyake, Y.; Aruga, T.; Inoue, K.; Okudera, H.; Kitahara, T.; Shimazaki, S.; Tsuruta, R.; Yokota, H.; Nakamura, S.; Tsubokura, M. Heat stroke STUDY 2010 in Japan. J. Jpn Assoc. Acute Med. 2012, 23, 211–230. (In Japanese) [Google Scholar]
- Hayashida, K.; Kondo, Y.; Hifumi, T.; Shimazaki, J.; Oda, Y.; Shiraishi, S.; Fukuda, T.; Sasaki, J.; Shimizu, K. A novel early risk assessment tool for detecting clinical outcomes in patients with heat-related illness (J-ERATO score): Development and validation in independent cohorts in Japan. PLoS ONE 2018. [Google Scholar] [CrossRef] [PubMed]


| Variable | n = 1799 |
|---|---|
| Age, years | 44 (21–68) |
| Males | 1184 (66) |
| Exertional heat illness | 1121 (62) |
| APACHE II score | 13 (8–22) |
| Laboratory data | |
| ALT (IU/L) | 19.0 (14.0–32.0) |
| Creatinine (mg/dL) | 0.90 (0.70–1.40) |
| BUN (mg/dL) | 17.0 (12.7–23.0) |
| Platelet count (104/μL) | 23.0 (18.3–28.5) |
| Outcome | |
| Home | 1259 (70) |
| General ward | 278 (15) |
| ICU | 262 (15) |
| Death | 37 (2) |
| International Classification | Novel Classification | |
|---|---|---|
| ALT | 0.147 * | 0.214 * |
| Creatinine | 0.183 * | 0.306 * |
| BUN | 0.147 * | 0.256 * |
| Platelet count | −0.101 * | −0.165 * |
| Stage I and II | Stage III | p Value * | |
|---|---|---|---|
| ALT (IU/L) | 18.0 (13.0–29.0) | 22.0 (15.0–43.0) | 0.001 |
| Creatinine (mg/dL) | 0.83 (0.66–1.19) | 1.25 (0.82–2.07) | <0.001 |
| BUN (mg/dL) | 16.0 (12.0–21.9) | 20.0 (14.9–26.5) | <0.001 |
| Platelet count (104/μL) | 23.6 (19.0–29.3) | 21.5 (17.5–27.3) | 0.003 |
| Heat Cramp and Syncope or Heat Exhaustion | Heat Stroke | p Value * | |
|---|---|---|---|
| ALT (IU/L) | 18.0 (13.0–29.0) | 17.0 (13.0–24.0) | 0.420 |
| Creatinine (mg/dL) | 0.83 (0.66–1.19) | 0.88 (0.67–1.29) | 0.487 |
| BUN (mg/dL) | 16.0 (12.0–21.9) | 17.0 (14.3–22.9) | 0.135 |
| Platelet count (104/μL) | 23.6 (19.0–29.3) | 23.2 (15.9–27.5) | 0.122 |
| III | Heat Stroke | |
|---|---|---|
| Mortality, number (%) | 33/322 (10.2) | 31/241 (12.9) |
| Sensitivity for death (95% CI) | 0.892 (0.755–0.957) | 0.838 (0.692–0.923) |
| Specificity for death (95% CI) | 0.836 (0.833–0.837) | 0.881 (0.878–0.883) |
| LR+ (95% CI) | 5.438 (4.526–5.884) | 7.030 (5.662–7.863) |
| LR− (95% CI) | 0.129 (0.051–0.294) | 0.184 (0.087–0.351) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, T.; Fujita, M.; Oda, Y.; Todani, M.; Hifumi, T.; Kondo, Y.; Shimazaki, J.; Shiraishi, S.; Hayashida, K.; Yokobori, S.; et al. Evaluation of a Novel Classification of Heat-Related Illnesses: A Multicentre Observational Study (Heat Stroke STUDY 2012). Int. J. Environ. Res. Public Health 2018, 15, 1962. https://doi.org/10.3390/ijerph15091962
Yamamoto T, Fujita M, Oda Y, Todani M, Hifumi T, Kondo Y, Shimazaki J, Shiraishi S, Hayashida K, Yokobori S, et al. Evaluation of a Novel Classification of Heat-Related Illnesses: A Multicentre Observational Study (Heat Stroke STUDY 2012). International Journal of Environmental Research and Public Health. 2018; 15(9):1962. https://doi.org/10.3390/ijerph15091962
Chicago/Turabian StyleYamamoto, Takahiro, Motoki Fujita, Yasutaka Oda, Masaki Todani, Toru Hifumi, Yutaka Kondo, Junya Shimazaki, Shinichiro Shiraishi, Kei Hayashida, Shoji Yokobori, and et al. 2018. "Evaluation of a Novel Classification of Heat-Related Illnesses: A Multicentre Observational Study (Heat Stroke STUDY 2012)" International Journal of Environmental Research and Public Health 15, no. 9: 1962. https://doi.org/10.3390/ijerph15091962





