Household Preparedness and Preferred Communication Channels in Public Health Emergencies: A Cross-Sectional Survey of Residents in an Asian Developed Urban City
Abstract
:1. Introduction
2. Materials and Methods
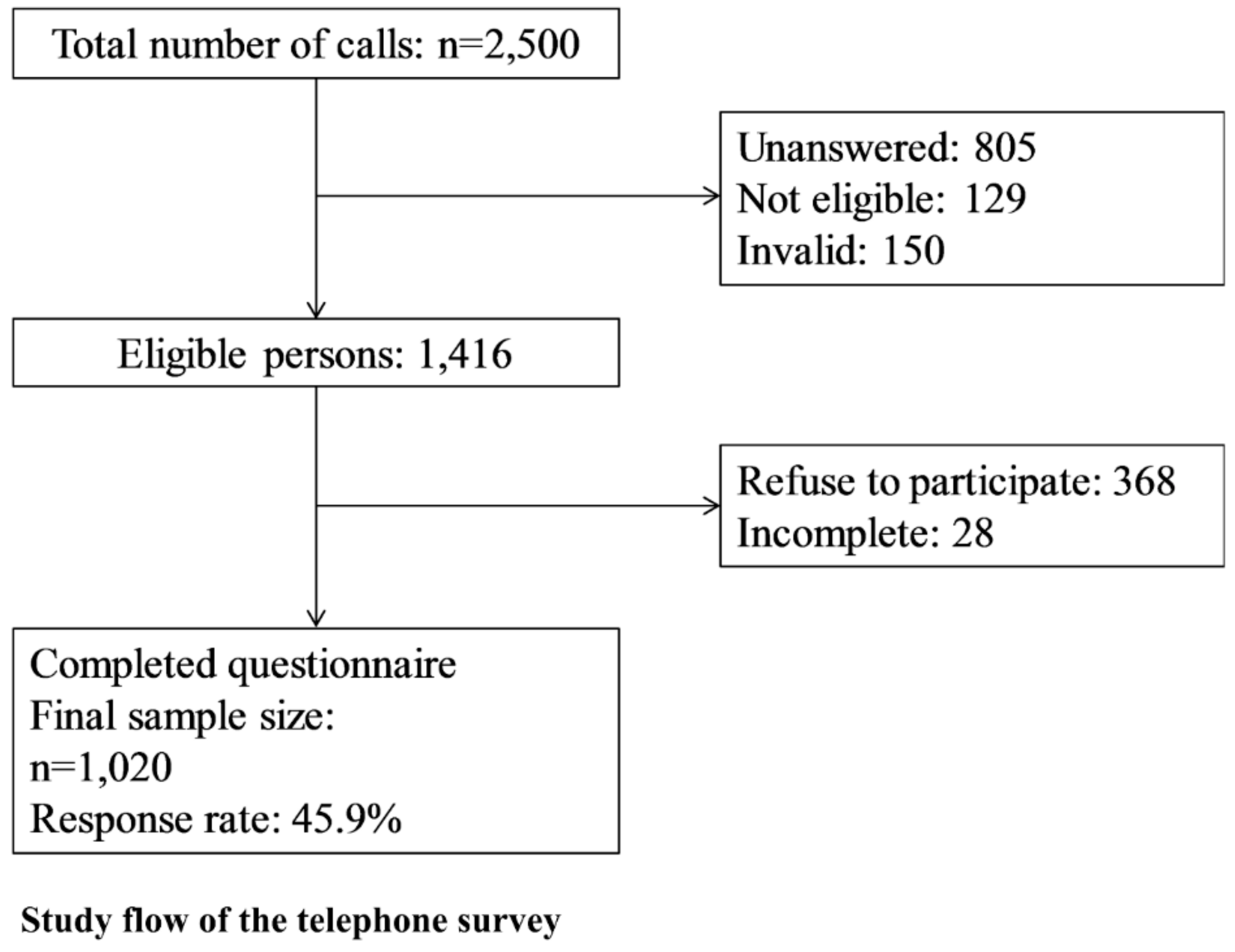
2.1. Study Design and Study Population
2.2. Instrument
- Socio-demographic and background information, including age, gender, district of residence, occupation and employment status, educational attainment, type and size of housing, and household income (21 questions). Vulnerable population referred to the elderly (>60 years old), those with respiratory or chronic diseases including asthma and hypertension and those who had flu in the past 2 weeks from the day of the interview.
- Knowledge, attitudes, and practices of preventive measures against A/H7N9 influenza infections (26 questions), reported elsewhere [21].
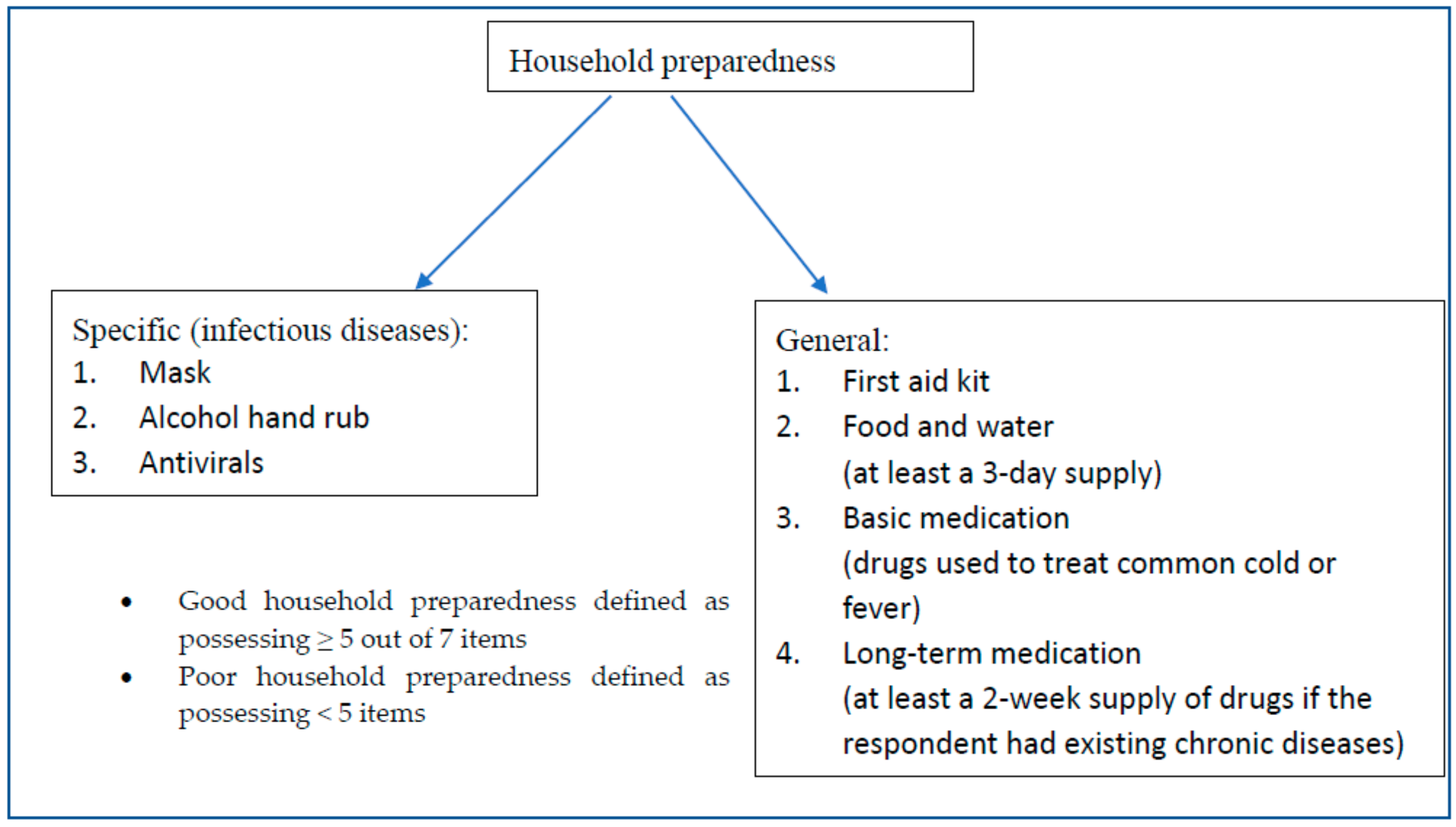
- Figure 2 summarizes the categories of household preparedness, the items for each category and the definition of household preparedness levels.
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Preparedness Level in General Disasters and Infectious Diseases Outbreaks
3.2. Characteristics of Respondents Lacking Household Preparedness
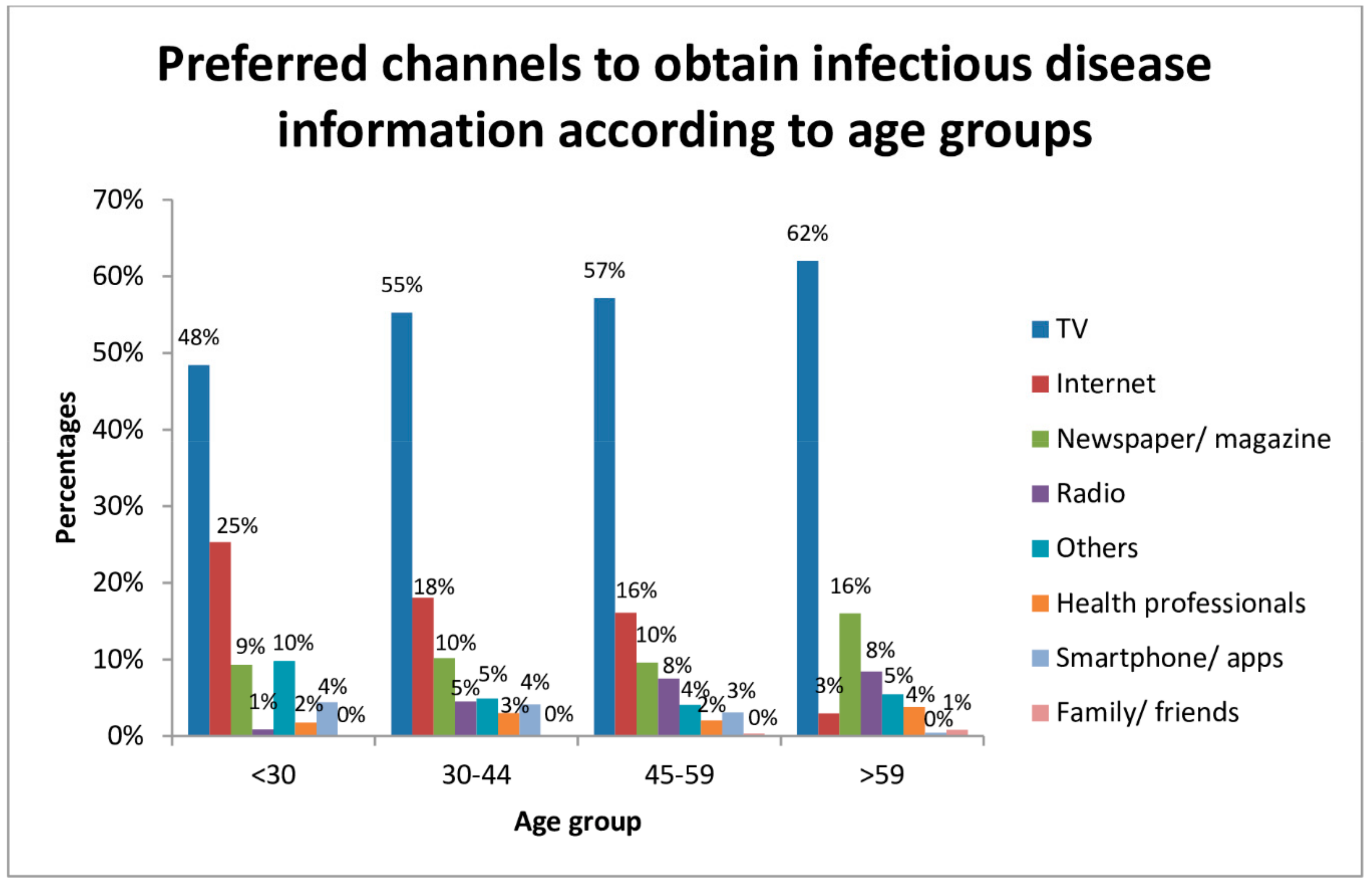
3.3. Suitable Channels for Community Disease Surveillance and Risk Communication
4. Discussion
4.1. Household Preparedness Level
4.2. Preferred Channels in Different Countries
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Landesman, L.Y. Public Health Management of Disasters: The Practice Guide; American Public Health Association: Washington, DC, USA, 2005. [Google Scholar]
- Thomas, T.N.; Leander-Griffith, M.; Harp, V.; Cioffi, J.P. Influences of preparedness knowledge and beliefs on household disaster preparedness. MMWR Morb Mortal Wkly. Rep. 2015, 64, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Australian Government. Department of Health. Health Emergency Preparedness and Response. Available online: www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-bio-index.htm (accessed on 13 July 2016).
- The Alabama Department of Public Health. Get 10—The Campaign. Available online: http://adph.org/get10/Default.asp?id=2290 (accessed on 9 July 2016).
- Emergency Preparedness Week Toolkit. Available online: http://www.getprepared.gc.ca/cnt/rsrcs/ep-wk/tlkt-en.aspx (accessed on 13 July 2016).
- Get Prepared. Emergency Kits. Available online: http://www.getprepared.gc.ca/cnt/kts/index-en.aspx (accessed on 9 July 2016).
- National Society for Earthquake Technology. Prepare Earthquake Emergency Kit. Available online: http://www.nset.org.np/nset2012/index.php/menus/menuid-62/submenuid-115 (accessed on 10 July 2016).
- National Society for Earthquake Technology. Nepal Earthquake Risk Management Program II (NERMP 2). Available online: http://www.nset.org.np/nset2012/index.php/programs/programdetail/programid-80 (accessed on 13 July 2016).
- Prevention Web. Hong Kong has the Highest Natural Disasters Risk in Asia—Study. Available online: https://www.preventionweb.net/news/view/44503 (accessed on 13 July 2016).
- Chan, E.Y.; Yue, J.; Lee, P.; Wang, S.S. Socio-demographic Predictors for Urban Community Disaster Health Risk Perception and Household Based Preparedness in a Chinese Urban City. PLoS Curr. Disasters 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Hong Kong SAR Census and Statistics Department. Population—Overview|Census and Statistics Department. Available online: http://www.censtatd.gov.hk/hkstat/sub/so20.jsp (accessed on 13 July 2016).
- Hong Kong SAR Information Services Department. Avian Flu: Frequently Asked Questions. Available online: http://www.info.gov.hk/info/flu/chi/faq.htm (accessed on 14 July 2016).
- World Health Organization. Avian Influenza. Available online: http://www.who.int/mediacentre/factsheets/avian_influenza/en/ (accessed on 14 July 2016).
- Hung, L.S. The SARS epidemic in Hong Kong: What lessons have we learned? J. R. Soc. Med. 2003, 96, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Hong Kong SAR Centre for Health Protection—Number of Notifiable Infectious Diseases by Month in 2009. Available online: http://www.chp.gov.hk/en/data/1/10/26/43/375.html (accessed on 13 July 2016).
- Bao, C.-J.; Cui, L.-B.; Zhou, M.-H.; Hong, L.; Gao, G.F.; Wang, H. Live-animal markets and influenza A (H7N9) virus infection. N. Engl. J. Med. 2013, 368, 2337–2339. [Google Scholar] [CrossRef] [PubMed]
- Hong Kong Observatory. Tropical Cyclone Warning System for Hong Kong. Available online: http://www.weather.gov.hk/informtc/tcService.htm (accessed on 5 December 2016).
- Hong Kong Jockey Club Disaster Preparedness and Response Institute. Hong Kong’s Emergency and Disaster Response System. Available online: http://www.hkjcdpri.org.hk/policy-brief-hong-kong’s-emergency-and-disaster-response-system (accessed on 14 July 2016).
- Hong Kong SAR Security Bureau. Simple Guidelines in the Event of Major Mishaps. Available online: http://www.sb.gov.hk/eng/emergency/mishaps/guidelines_mishaps.pdf (accessed on 4 November 2016).
- Hong Kong SAR Centre for Health Protection. E-resources-Avian Influenza. Available online: http://www.chp.gov.hk/en/her_list/463/24/13.html (accessed on 14 July 2016).
- Chan, E.Y.; Cheng, C.K.; Tam, G.; Huang, Z.; Lee, P. Knowledge, attitudes, and practices of Hong Kong population towards human A/H7N9 influenza pandemic preparedness, China, 2014. BMC Public Health 2015, 15, 1. [Google Scholar] [CrossRef] [PubMed]
- Hong Kong SAR Centre for Health Protection—Frequently Asked Questions on Influenza (Flu). Available online: http://www.chp.gov.hk/en/view_content/38225.html (accessed on 21 July 2016).
- Hong Kong SAR Centre for Health Protection. Seasonal Influenza. Available online: https://www.chp.gov.hk/en/features/14843.html (accessed on 26 July 2018).
- Yu, H.; Cowling, B.J.; Feng, L.; Lau, E.H.; Liao, Q.; Tsang, T.K.; Peng, Z.; Wu, P.; Liu, F.; Fang, V.J.; et al. Human infection with avian influenza A H7N9 virus: An assessment of clinical severity. Lancet 2013, 382, 138–145. [Google Scholar] [CrossRef]
- Wu, P.; Fang, V.J.; Liao, Q.; Ng, D.M.; Wu, J.T.; Leung, G.M.; Fielding, R.; Cowling, B.J. Responses to threat of influenza A (H7N9) and support for live poultry markets, Hong Kong, 2013. Emerg. Infect. Dis. 2014, 20, 882. [Google Scholar] [CrossRef] [PubMed]
- Tamiflu. Fever, Aches, Chills. Check Your Symptoms and Learn More about a Prescription Flu Treatment. Available online: http://www.tamiflu.com/ (accessed on 8 August 2016).
- Centers for Disease Control and Prevention. Emergency Preparedness and Response. Available online: https://emergency.cdc.gov/preparedness/kit/disasters/index.asp (accessed on 14 January 2016).
- Fung, O.W.M.; Loke, A.Y. Disaster preparedness of families with young children in Hong Kong. Scand. J. Public Health 2010, 38, 880–888. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.; Kim, J.H.; Griffiths, S.M.; Lau, J.T.; Yu, I. Does living density matter for nonfatal unintentional home injury in Asian urban settings? Evidence from Hong Kong. J. Urban Health 2009, 86, 872–886. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.; Kim, J.H.; Ng, Q.; Griffiths, S.; Lau, J. A descriptive study of nonfatal, unintentional home-based injury in urban settings: Evidence from Hong Kong. Asia-Pac. J. Public Health 2008, 20, 39–48. [Google Scholar] [PubMed]
- Nicolopoulos, N.; Hansen, E. How well prepared are Australian communities for natural disasters and fire emergencies? Aust. J. Emerg. Manag. 2009, 24, 60. [Google Scholar]
- Kapucu, N. Culture of preparedness: Household disaster preparedness. Disaster Prev. Manag. 2008, 17, 526–535. [Google Scholar] [CrossRef]
- Phillips, B.D.; Metz, W.C.; Nieves, L.A. Disaster threat: Preparedness and potential response of the lowest income quartile. Glob. Environ. Chang. Part B Environ. Hazards 2005, 6, 123–133. [Google Scholar] [CrossRef]
- Ferguson, N.M.; Cummings, D.A.; Cauchemez, S.; Fraser, C.; Riley, S.; Meeyai, A.; Iamsirithaworn, S.; Burke, D.S. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature 2005, 437, 209–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. WHO Guidelines on the Use of Vaccines and Antivirals during Influenza Pandemics. 2004. Available online: http://www.who.int/csr/resources/publications/influenza/11_29_01_A.pdf (accessed on 14 July 2016).
- Black, A.J.; House, T.; Keeling, M.J.; Ross, J.V. Epidemiological consequences of household-based antiviral prophylaxis for pandemic influenza. J. R. Soc. Interface 2013, 10, 20121019. [Google Scholar] [CrossRef] [PubMed]
- Marshall, H.; Ryan, P.; Roberton, D.; Street, J.; Watson, M. Pandemic influenza and community preparedness. Am. J. Public Health 2009, 99, S365–S371. [Google Scholar] [CrossRef] [PubMed]
- Hong Kong SAR Information Services Department. Concern over Sale of Antiviral Drug Tamiflu. Available online: http://archive.news.gov.hk/isd/ebulletin/en/category/healthandcommunity/041228/html/041228en05003.htm (accessed on 14 July 2016).
- Rosenthal, E. Healthy Public Is Hoarding a Drug to Fight a Distant Threat. The New York Times. Available online: http://www.nytimes.com/2005/10/28/world/europe/healthy-public-is-hoarding-a-drug-to-fight-a-distant-threat.html (accessed on 28 October 2005).
- Davis, A.; Moore-Bridger, B. Flu Drug Distribution in Chaos as Patients Ignore Rules. Evening Standard. Available online: http://www.standard.co.uk/news/flu-drug-distribution-in-chaos-as-patients-ignore-rules-6745719.html (accessed on 12 April 2015).
- Hong Kong SAR Information Services Department. LCQ 17: Stockpiling of Antiviral Drugs. Available online: http://www.info.gov.hk/gia/general/200901/14/P200901140138.htm (accessed on 4 November 2016).
- Tomio, J.; Sato, H.; Matsuda, Y.; Koga, T.; Mizumura, H. Household and Community Disaster Preparedness in Japanese Provincial City: A Population-Based Household Survey. Adv. Anthropol. 2014, 4, 68. [Google Scholar] [CrossRef]
- DeBastiani, S.D.; Strine, T.W.; Vagi, S.J.; Barnett, D.J.; Kahn, E.B. Preparedness Perceptions, Sociodemographic Characteristics, and Level of Household Preparedness for Public Health Emergencies: Behavioral Risk Factor Surveillance System, 2006–2010. Health Secur. 2015, 13, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Mohammad-pajooh, E.; Ab Aziz, K. Investigating factors for disaster preparedness among residents of Kuala Lumpur. Nat. Hazards Earth Syst. Sci. Discuss. 2014, 2, 3683–3709. [Google Scholar] [CrossRef] [Green Version]
- Botzen, W.; Aerts, J.; Van Den Bergh, J. Dependence of flood risk perceptions on socioeconomic and objective risk factors. Water Resour. Res. 2009, 45. [Google Scholar] [CrossRef] [Green Version]
- Smith, D.L.; Notaro, S.J. Personal emergency preparedness for people with disabilities from the 2006–2007 Behavioral Risk Factor Surveillance System. Disabil. Health J. 2009, 2, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Becker, J.S.; Paton, D.; Johnston, D.M.; Ronan, K.R. Salient beliefs about earthquake hazards and household preparedness. Risk Anal. 2013, 33, 1710–1727. [Google Scholar] [CrossRef] [PubMed]
- Ofcom. News Consumption in the UK—2014 Reportjuly 13, 2016. Available online: http://stakeholders.ofcom.org.uk/binaries/research/media-literacy/media-lit-10years/2015_Adults_media_use_and_attitudes_report.pdf (accessed on 14 July 2016).
- Manganello, J.A.; Gerstner, G.; Pergolino, K.; Graham, Y.; Strogatz, D. Understanding Digital Technology Access and Use Among New York State Residents to Enhance Dissemination of Health Information. JMIR Public Health Surveill. 2016, 2. [Google Scholar] [CrossRef] [PubMed]
- Eastwood, K.; Durrheim, D.; Francis, J.L.; d’Espaignet, E.T.; Duncan, S.; Islam, F.; Speare, R. Knowledge about pandemic influenza and compliance with containment measures among Australians. Bull. World Health Organ. 2009, 87, 588–594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Deursen, A.J.; van Dijk, J.A. Internet skill levels increase, but gaps widen: A longitudinal cross-sectional analysis (2010–2013) among the Dutch population. Inf. Commun. Soc. 2015, 18, 782–797. [Google Scholar] [CrossRef]
- Chan, E.Y.; Huang, Z.; Mark, C.K.; Guo, C. Weather information acquisition and health significance during extreme cold weather in a subtropical city: A cross-sectional survey in Hong Kong. Int. J.Disaster Risk Sci. 2017, 8, 134–144. [Google Scholar] [CrossRef]
- Hill, J.H.; Burge, S.; Haring, A.; Young, R.A. Communication technology access, use, and preferences among primary care patients: From the Residency Research Network of Texas (RRNeT). J. Am. Board Fam. Med. 2012, 25, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Glass, D.C.; Kelsall, H.L.; Slegers, C.; Forbes, A.B.; Loff, B.; Zion, D.; Fritschi, L. A telephone survey of factors affecting willingness to participate in health research surveys. BMC Public Health 2015, 15, 1017. [Google Scholar] [CrossRef] [PubMed]
- Bradley, D.T.; McFarland, M.; Clarke, M. The Effectiveness of Disaster Risk Communication: A Systematic Review of Intervention Studies. PLoS Curr. Disasters 2014, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Demographics | Sample Population | Hong Kong Population 2011 | Sample vs. Census p-Value a | |
|---|---|---|---|---|
| n | % | % | ||
| Age (n = 1020) | ||||
| 15–24 | 143 | 14.0 | 14.0 | 0.99 |
| 25–44 | 348 | 34.1 | 35.5 | |
| 45–64 | 363 | 35.6 | 35.4 | |
| ≥65 | 166 | 16.3 | 15.1 | |
| Gender (n = 1020) | ||||
| Male | 461 | 45.2 | 46.0 | 1.00 |
| Female | 559 | 54.8 | 54.0 | |
| Education (n = 1019) | ||||
| Primary education or below | 138 | 13.5 | 22.7 | 0.18 |
| Secondary education | 517 | 50.7 | 50.0 | |
| Post-secondary education (including diploma and certificate) | 364 | 35.7 | 27.3 | |
| Occupation (n = 1006) | ||||
| White collar | 411 | 40.9 | NA | |
| Blue collar | 96 | 9.5 | NA | |
| Housewife, retired or unemployed | 393 | 39.1 | NA | |
| Students | 106 | 10.5 | NA | |
| Area of residence (n = 1020) | ||||
| Hong Kong Island | 185 | 18.1 | 18.0 | 1.00 |
| Kowloon | 308 | 30.2 | 29.8 | |
| New Territories | 527 | 51.7 | 52.2 | |
| Marital status (n = 1018) | ||||
| Single | 355 | 34.9 | 42.2 | 0.36 |
| Married | 663 | 65.1 | 57.8 | |
| Household income (n = 969) | ||||
| <$10,000 | 135 | 13.9 | 23.8 | 0.30 |
| $10,000–19,999 | 220 | 22.7 | 23.8 | |
| $20,000–39,999 | 346 | 35.7 | 29.0 | |
| ≥$40,000 | 268 | 27.7 | 23.5 | |
| Type of housing (n = 1017) | ||||
| Public housing | 387 | 38.1 | 30.3 | 0.61 b |
| Subsidized homeownership housing | 160 | 15.7 | 15.9 | |
| Private permanent housing | 455 | 44.7 | 52.3 | |
| Others | 15 | 1.5 | 1.4 | |
| Characteristics | Household Preparedness | a COR (95% CI) | bp-Value | c AOR (95% CI) | bp-Value | |
|---|---|---|---|---|---|---|
| Poor | Good | |||||
| N (%) | N (%) | |||||
| Respondents | ||||||
| Gender | ||||||
| Male | 214 (46.4) | 247 (53.6) | 1 | 1 | ||
| Female | 202 (36.1) | 357 (63.9) | 1.53 (1.19, 1.97) | <0.01 | 1.63 (1.25, 2.21) | <0.01 |
| Occupation | ||||||
| White collar | 156 (38.0) | 255 (62.0) | 1 | |||
| Blue collar | 56 (58.3) | 40 (41.7) | 0.44 (0.28, 0.69) | <0.01 | ||
| Unemployed | 162 (41.2) | 231 (58.8) | 0.87 (0.66, 1.16) | 0.34 | ||
| Student | 38 (35.8) | 68 (64.2) | 1.09 (0.70, 1.71) | 0.69 | ||
| Education | ||||||
| Primary education or below | 75 (54.3) | 63 (45.6) | 1 | 1 | ||
| Secondary education | 213 (41.2) | 304 (58.8) | 1.70 (1.16, 2.48) | 0.01 | 1.68 (1.12, 2.53) | 0.01 |
| Post-secondary education (including diploma and certificate) | 127 (34.9) | 237 (65.1) | 2.22 (1.49, 3.31) | <0.01 | 1.92 (1.21, 3.02) | 0.01 |
| Household characteristics: Type of housing | ||||||
| Public housing | 176 (45.5) | 211 (54.5) | 1 | |||
| Subsidized home ownership housing | 71 (44.4) | 89 (55.6) | 1.05 (0.72, 1.51) | 0.81 | ||
| Private permanent housing | 164 (36.0) | 291 (64.0) | 1.48 (1.12, 1.95) | 0.01 | ||
| Household income | ||||||
| <$10,000 | 70 (51.9) | 65 (48.1) | 1 | 1 | ||
| $10,000–19,999 | 104 (47.3) | 116 (52.7) | 1.20 (0.78, 1.84) | 0.40 | 1.12 (0.78, 1.73) | 0.60 |
| $20,000–39,999 | 140 (40.5) | 206 (59.5) | 1.58 (1.06, 2.36) | 0.02 | 1.40 (0.93, 2.11) | 0.11 |
| ≥$40,000 | 83 (31.0) | 185 (69.0) | 2.40 (1.57, 3.67) | <0.01 | 2.01 (1.27, 3.17) | <0.01 |
| Family size | ||||||
| 1 | 38 (61.3) | 24 (38.7) | 1 | |||
| 2 | 80 (40.8) | 116 (59.2) | 2.30 (1.28, 4.12) | 0.01 | ||
| 3–4 | 233 (39.9) | 351 (60.1) | 2.39 (1.39, 4.08) | <0.01 | ||
| ≥5 | 65 (36.5) | 113 (63.5) | 2.75 (1.52, 4.99) | <0.01 | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tam, G.; Huang, Z.; Chan, E.Y.Y. Household Preparedness and Preferred Communication Channels in Public Health Emergencies: A Cross-Sectional Survey of Residents in an Asian Developed Urban City. Int. J. Environ. Res. Public Health 2018, 15, 1598. https://doi.org/10.3390/ijerph15081598
Tam G, Huang Z, Chan EYY. Household Preparedness and Preferred Communication Channels in Public Health Emergencies: A Cross-Sectional Survey of Residents in an Asian Developed Urban City. International Journal of Environmental Research and Public Health. 2018; 15(8):1598. https://doi.org/10.3390/ijerph15081598
Chicago/Turabian StyleTam, Greta, Zhe Huang, and Emily Ying Yang Chan. 2018. "Household Preparedness and Preferred Communication Channels in Public Health Emergencies: A Cross-Sectional Survey of Residents in an Asian Developed Urban City" International Journal of Environmental Research and Public Health 15, no. 8: 1598. https://doi.org/10.3390/ijerph15081598





