The Impact of Ambient Air Pollution on Daily Hospital Visits for Various Respiratory Diseases and the Relevant Medical Expenditures in Shanghai, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analyses
3. Results
3.1. Descriptive Statistics
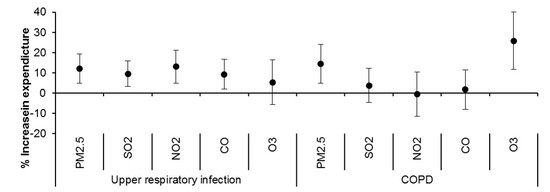
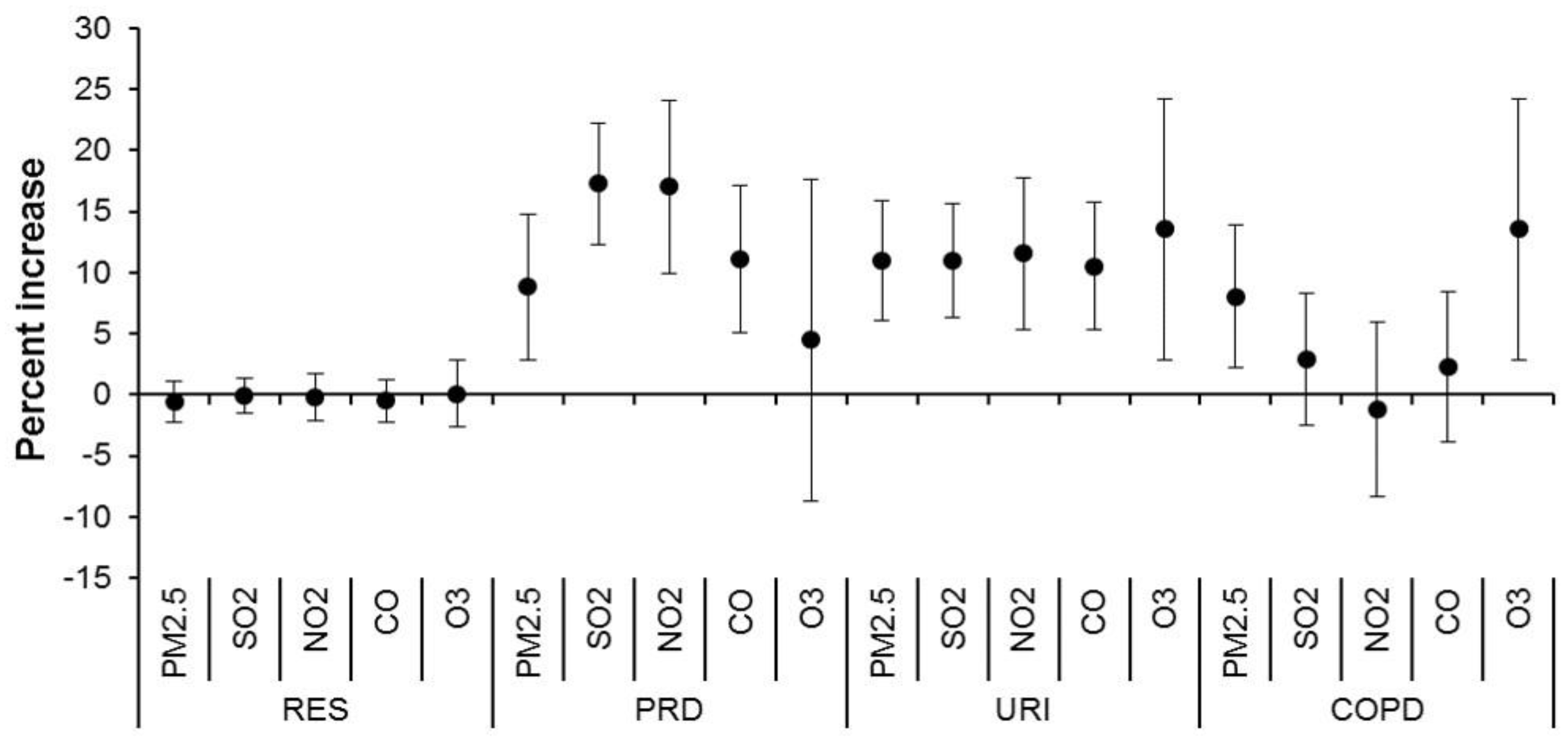
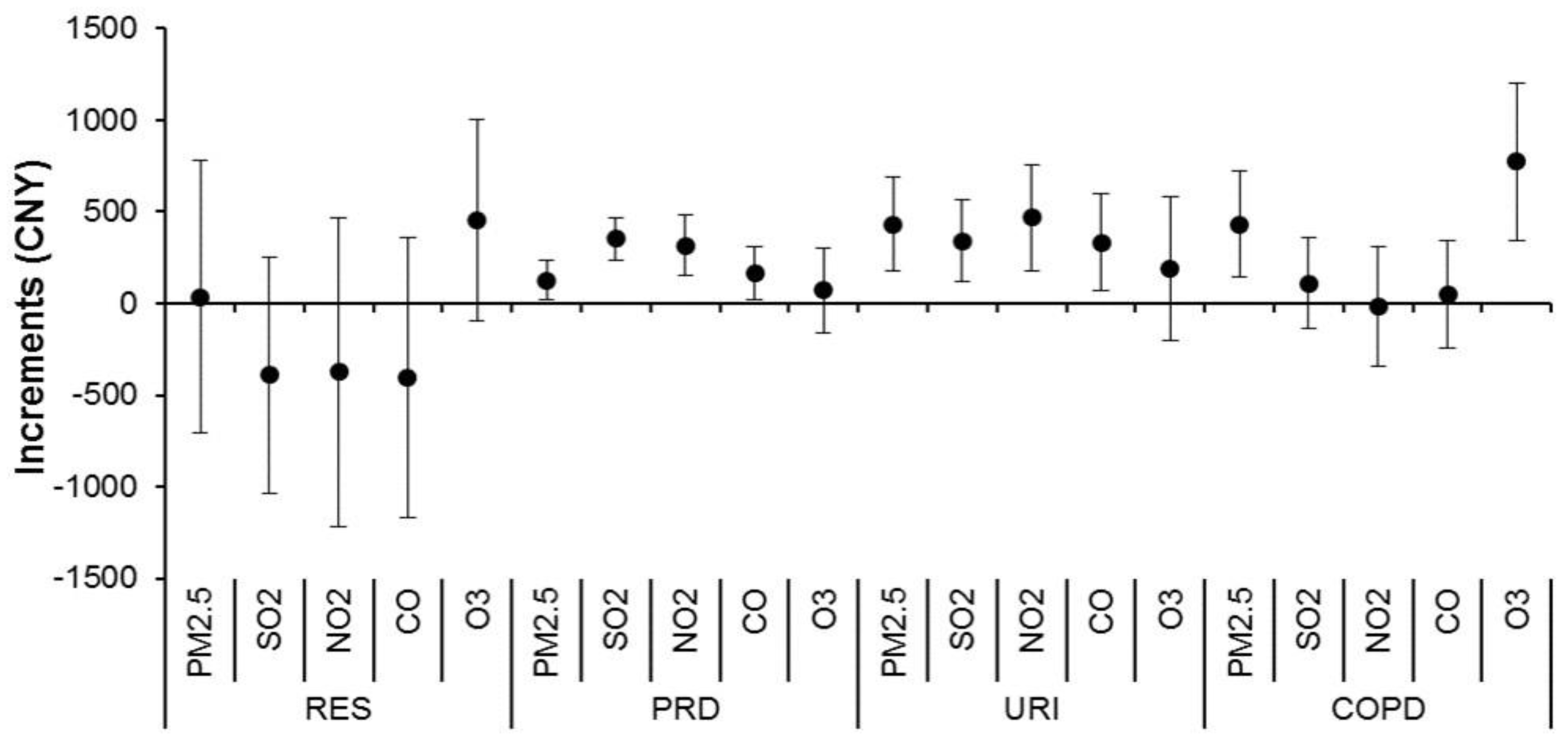
3.2. Regression Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Chen, R.; Yin, P.; Meng, X.; Liu, C.; Wang, L.; Xu, X.; Ross, J.A.; Tse, L.A.; Zhao, Z.; Kan, H.; et al. Fine Particulate Air Pollution and Daily Mortality. A Nationwide Analysis in 272 Chinese Cities. Am. J. Respir. Crit. Care Med. 2017, 196, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Sun, Z.; Cao, J.; Wang, X.; Zhong, L.; Bi, X.; Li, H.; Liu, W.; Zhu, T.; Huang, W. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ. Int. 2013, 54, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Xu, D.; Cheng, Y.; Dong, S.; Guo, C.; Jiang, X.; Zheng, X. Systematic review and meta-analysis of the adverse health effects of ambient PM2.5 and PM10 pollution in the Chinese population. Environ. Res. 2015, 136, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Capraz, O.; Deniz, A.; Dogan, N. Effects of air pollution on respiratory hospital admissions in Istanbul, Turkey, 2013 to 2015. Chemosphere 2017, 181, 544–550. [Google Scholar] [CrossRef] [PubMed]
- Phung, D.; Hien, T.T.; Linh, H.N.; Luong, L.M.; Morawska, L.; Chu, C.; Binh, N.D.; Thai, P.K. Air pollution and risk of respiratory and cardiovascular hospitalizations in the most populous city in Vietnam. Sci. Total Environ. 2016, 557–558, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Li, W.; Tan, J.; Song, W.; Xu, X.; Jiang, C.; Chen, G.; Chen, R.; Ma, W.; Chen, B.; et al. Association of ambient air pollution with hospital outpatient and emergency room visits in Shanghai, China. Sci. Total Environ. 2009, 407, 5531–5536. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Song, Y.; Cai, X.; Zhou, J. Economic assessment of the health effects related to particulate matter pollution in 111 Chinese cities by using economic burden of disease analysis. J. Environ. Manag. 2008, 88, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Bank, W. Cost of Pollution in China; World Bank: Washington, DC, USA, 2007. [Google Scholar]
- Dominici, F.; Peng, R.D.; Bell, M.L.; Pham, L.; McDermott, A.; Zeger, S.L.; Samet, J.M. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006, 295, 1127–1134. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A. Distributed Lag Linear and Non-Linear Models in R: The Package dlnm. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Peng, R.D.; Dominici, F.; Louis, T.A. Model choice in time series studies of air pollution and mortality. J. Roy. Stat. Soc. A Stat. 2006, 169, 179–198. [Google Scholar] [CrossRef]
- Chen, R.; Chu, C.; Tan, J.; Cao, J.; Song, W.; Xu, X.; Jiang, C.; Ma, W.; Yang, C.; Chen, B.; et al. Ambient air pollution and hospital admission in Shanghai, China. J. Hazard. Mater. 2010, 181, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Li, X.; Wang, S.; Wang, C.; Huang, F.; Gao, Q.; Wu, L.; Tao, L.; Guo, J.; Wang, W.; et al. Fine Particulate Air Pollution and Hospital Emergency Room Visits for Respiratory Disease in Urban Areas in Beijing, China, in 2013. PLoS ONE 2016, 11, e0153099. [Google Scholar] [CrossRef] [PubMed]
- DeVries, R.; Kriebel, D.; Sama, S. Outdoor Air Pollution and COPD-Related Emergency Department Visits, Hospital Admissions, and Mortality: A Meta-Analysis. COPD 2017, 14, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Xie, S.; Yu, Q.; Huo, X.; Ming, X.; Wang, J.; Zhou, Y.; Peng, Z.; Zhang, H.; Cui, X.; et al. Short-term effects of ambient air pollution on pediatric outpatient visits for respiratory diseases in Yichang city, China. Environ. Pollut. 2017, 227, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Sioutas, C.; Cho, A.; Schmitz, D.; Misra, C.; Sempf, J.; Wang, M.; Oberley, T.; Froines, J.; Nel, A. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ. Health Perspect. 2003, 111, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Qiao, L.; Li, H.; Zhao, Y.; Zhang, Y.; Xu, W.; Wang, C.; Wang, H.; Zhao, Z.; Xu, X.; et al. Fine Particulate Matter Constituents, Nitric Oxide Synthase DNA Methylation and Exhaled Nitric Oxide. Environ. Sci. Technol. 2015, 49, 11859–11865. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, R.W.; Anderson, H.R.; Sunyer, J.; Ayres, J.; Baccini, M.; Vonk, J.M.; Boumghar, A.; Forastiere, F.; Forsberg, B.; Touloumi, G.; et al. Acute effects of particulate air pollution on respiratory admissions: Results from APHEA 2 project. Air Pollution and Health: A European Approach. Am. J. Respir. Crit. Care Med. 2001, 164, 1860–1866. [Google Scholar] [CrossRef] [PubMed]
- Sunyer, J.; Atkinson, R.; Ballester, F.; Le Tertre, A.; Ayres, J.G.; Forastiere, F.; Forsberg, B.; Vonk, J.M.; Bisanti, L.; Anderson, R.H.; et al. Respiratory effects of sulphur dioxide: A hierarchical multicity analysis in the APHEA 2 study. Occup. Environ. Med. 2003, 60, e2. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Ebisu, K.; Peng, R.D.; Walker, J.; Samet, J.M.; Zeger, S.L.; Dominici, F. Seasonal and regional short-term effects of fine particles on hospital admissions in 202 US counties, 1999–2005. Am. J. Epidemiol. 2008, 168, 1301–1310. [Google Scholar] [CrossRef] [PubMed]
- Zeger, S.L.; Thomas, D.; Dominici, F.; Samet, J.M.; Schwartz, J.; Dockery, D.; Cohen, A. Exposure measurement error in time-series studies of air pollution: Concepts and consequences. Environ. Health Perspect. 2000, 108, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Goldman, G.T.; Mulholland, J.A.; Russell, A.G.; Strickland, M.J.; Klein, M.; Waller, L.A.; Tolbert, P.E. Impact of exposure measurement error in air pollution epidemiology: Effect of error type in time-series studies. Environ. Health 2011, 10, 61. [Google Scholar] [CrossRef] [PubMed]


| Mean | SD | Min | P25 | P50 | P75 | Max | |
|---|---|---|---|---|---|---|---|
| Pollutants (μg/m3) | |||||||
| PM2.5 | 56 | 37 | 7 | 30 | 45 | 70 | 255 |
| SO2 | 19 | 13 | 6 | 11 | 15 | 22 | 103 |
| NO2 | 46 | 21 | 5 | 31 | 42 | 57 | 143 |
| CO | 821 | 311 | 364 | 606 | 735 | 951 | 2281 |
| O3 | 100 | 44 | 11 | 69 | 96 | 124 | 266 |
| Weather conditions | |||||||
| Temperature (°C) | 17 | 9 | −1 | 10 | 18 | 24 | 35 |
| Humidity (%) | 72 | 13 | 31 | 63 | 73 | 81 | 98 |
| Diseases | Emergency Department | Outpatient Department | ||
|---|---|---|---|---|
| Visits | Expenditures | Visits | Expenditures | |
| Total RES | 230 ± 85 | 73 ± 27 | 2100 ± 510 | 488 ± 153 |
| PRD | 14 ± 67 | 39 ± 18 | 1560 ± 340 | 364 ± 103 |
| URI | 17 ± 21 | 4 ± 5 | 170 ± 54 | 35 ± 13 |
| COPD | 5 ± 5 | 3 ± 3 | 50 ± 32 | 15 ± 12 |
| Asthma | 6 ± 3 | 2 ± 1 | 160 ± 74 | 55 ± 32 |
| LRI | 58 ± 18 | 25 ± 18 | 230 ± 85 | 56 ± 22 |
| Total RES | ||||
| January | 340 ± 99 | 113 ± 37 | 2520 ± 650 | 573 ± 197 |
| February | 280 ± 73 | 92 ± 24 | 1600 ± 510 | 347 ± 143 |
| March | 230 ± 46 | 75 ± 14 | 1830 ± 340 | 404 ± 99 |
| April | 260 ± 100 | 74 ± 22 | 1990 ± 310 | 447 ± 93 |
| May | 190 ± 60 | 58 ± 19 | 1990 ± 330 | 455 ± 100 |
| June | 170 ± 39 | 53 ± 13 | 2000 ± 290 | 458 ± 91 |
| July | 250 ± 88 | 77 ± 25 | 1960 ± 320 | 447 ± 102 |
| August | 240 ± 70 | 74 ± 22 | 1770 ± 320 | 403 ± 103 |
| September | 180 ± 46 | 57 ± 17 | 2050 ± 410 | 476 ± 125 |
| October | 180 ± 49 | 58 ± 14 | 2270 ± 430 | 541 ± 127 |
| November | 180 ± 39 | 58 ± 12 | 2440 ± 340 | 601 ± 109 |
| December | 270 ± 78 | 85 ± 21 | 2740 ± 410 | 686 ± 131 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, H.; Niu, Y.; Yao, Y.; Chen, R.; Zhou, X.; Kan, H. The Impact of Ambient Air Pollution on Daily Hospital Visits for Various Respiratory Diseases and the Relevant Medical Expenditures in Shanghai, China. Int. J. Environ. Res. Public Health 2018, 15, 425. https://doi.org/10.3390/ijerph15030425
Zhang H, Niu Y, Yao Y, Chen R, Zhou X, Kan H. The Impact of Ambient Air Pollution on Daily Hospital Visits for Various Respiratory Diseases and the Relevant Medical Expenditures in Shanghai, China. International Journal of Environmental Research and Public Health. 2018; 15(3):425. https://doi.org/10.3390/ijerph15030425
Chicago/Turabian StyleZhang, Hao, Yue Niu, Yili Yao, Renjie Chen, Xianghong Zhou, and Haidong Kan. 2018. "The Impact of Ambient Air Pollution on Daily Hospital Visits for Various Respiratory Diseases and the Relevant Medical Expenditures in Shanghai, China" International Journal of Environmental Research and Public Health 15, no. 3: 425. https://doi.org/10.3390/ijerph15030425