Social Environment of Older People during the First Year in Senior Housing and Its Association with Physical Performance
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Instruments
2.2.1. Perceptions of the Social Environment
2.2.2. Background Variables and Physical Performance Parameters
2.2.3. Statistical Analysis
2.2.4. Ethical Issues
3. Results
3.1. Background Characteristics of the Subjects
3.2. Self-Reported Social Environment and Changes in It 3 and 12 Months after Relocation
3.2.1. Pleasantness of Social Environment and Feeling of Social Restrictiveness
3.2.2 Interpersonal Relationships and Getting Support
3.3. Associations between Participants Perceptions of Their Social Environment and Physical Performance Parameters
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Rossen, E.; Knafl, K. Women’s well-being after relocation to independent living communities. Clin. Nurse Spec. 2007, 21, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Crisp, D.; Windsor, T.; Anstey, K.; Butterworth, P. What are older adults seeking? Factors encouraging or discouraging retirement village living. Aust. J. Ageing 2013, 32, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Granbom, M.; Slaug, B.; Löfqvist, C.; Oswald, F.; Iwarsson, S. Community relocation in very old age: Changes in housing accessibility. Am. J. Occup. Ther. 2016, 70, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bjornsdottir, G.; Arnadottir, S.; Halldorsdottir, S. Facilitators of and barriers to physical activity in retirement communities: Experiences of older women in urban areas. Phys. Ther. 2012, 92, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Phillips, L. Retirement Community residents’ physical activity, depressive symptoms and functional limitations. Clin. Nurs. Res. 2015, 24, 7–28. [Google Scholar] [CrossRef] [PubMed]
- Castle, N. Relocation of the elderly. Med. Care Res. Rev. 2001, 58, 291–333. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.C.; Wilmoth, J.M. The effects of residential mobility on ADL and IADL limitations among the very old living in the community. J. Gerontol.: Soc. Sci. 2004, 59B, 164–172. [Google Scholar] [CrossRef]
- Carroll, S.; Qualls, S. Moving into senior housing: Adapting the old, embracing the new. Generations 2014, 38, 42–47. [Google Scholar]
- Elo, S.; Saarnio, R.; Isola, A. The physical, social and symbolic environment supporting the well-being of home-dwelling elderly people. Int. J. Circumpolar Health 2011, 70, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Portegijs, E.; Keskinen, K.; Tsai, L.T.; Rantanen, T.; Rantakokko, M. Physical limitations, walkability, perceived environmental facilitators and physical activity of older adults in Finland. Int. J. Environ. Res. Public Health 2017, 14, 333. [Google Scholar] [CrossRef] [PubMed]
- Luoma, M.L.; Vaara, M.; Röberg, M.; Mukkila, S.; Mäki, J. Gerontologisen kuntoutuksen vaikuttavuus. In Gerontologisen Kuntouksen Toteutus, Vaikuttavuus Ja Tiedon Välittyminen; Pikkarainen, A., Vaara, M., Salmelainen, U., Eds.; Kelan tutkimusosasto: Helsinki, Finland, 2013; pp. 202–203. [Google Scholar]
- Elo, S. A Theory of an Environment Supporting the Well-Being of Home-Dwelling Elderly from Northern Finland. Ph.D. Thesis, University of Oulu, Oulu, Finland, 2006. [Google Scholar]
- Gramm, J.; Van Dijk, H.; Nieboer, A. The importance of neighbourhood social cohesion and social capital for the wellbeing of older adults in the community. Gerontologist 2012, 53, 142–150. [Google Scholar] [CrossRef] [Green Version]
- Balfour, J.; Kaplan, G. Neighbourhood environment and loss of physical function in older adults: Evidence from the Alameda county study. Am. J. Epidemiol. 2002, 155, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Sakari, R.; Rantakokko, M.; Portegijs, E.; Iwarsson, S.; Sipilä, S.; Viljanen, A.; Rantanen, T. Do associations between perceived environmental and individual characteristics and walking limitations depend on lower extremity performance level? J. Aging Health 2016, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Cress, M.; Orini, S.; Orini, S.; Kinnsler, L. Living environment and mobility of older adults. Gerontology 2011, 57, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Van Holle, V.; Van Cauwenberg, J.; De Bourdeaudhuij, I.; Deforche, B.; Van de Weghe, N.; Van Dyck, D. Interactions between neighbourhood social environment and walkability to explain Belgian older adults’ physical activity and sedentary time. Int. J. Environ. Res. Public Health 2016, 13, 569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Booth, M.; Owen, N.; Bauman, A.; Clavisi, O.; Leslie, E. Social-cognitive perceived environment influences associated with physical activity in older Australians. Prev. Med. 2000, 31, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.; Simonsick, E.; Ferrucci, L.; Robert, J.; Berkman, L.; Blazer, D.; Scherr, P.; Wallace, R. A short physical battery assessing the lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol.: Med. Sci. 1994, 49, 85–94. [Google Scholar] [CrossRef]
- Rikli, R.; Jones, C. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Mullen, S.; McAuley, E.; Satariano, W.; Kealey, M.; Prohaska, T. Physical activity and functional limitations in older adults: The influence of self-efficacy and functonal performance. J. Gerontol. Ser. B 2012, 67, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Moschny, A.; Platen, P.; Klaaben-Mielke, R.; Trampisch, U.; Hinrichs, T. Barriers to physical activity in older adults on Germany: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 121. [Google Scholar] [CrossRef] [PubMed]
- Nordin, S.; Mckee, K.; Wallinder, M.; Von Koch, L.; Wijk, H.; Elf, M. The physical environment and interaction in residential care facilities for older people: A comparative case study. Scand. J. Caring Sci. 2016. [Google Scholar] [CrossRef] [PubMed]
- Tyvimaa, T. Developing and Investing in Senior Houses in Finland—Senior’s Preferences and Investors Insights. Ph.D. Thesis, Tampere University of Technology, Tampere, Finland, 2010. [Google Scholar]
- Koistinen, P.; Elo, S.; Ahlroth, M.; Kokko, J.; Suistio, S.; Kujala, V.; Naarala, M.; Rissanen, T. Oldwellactive—A self-rated wellness profile for the assessment of wellbeing and wellness activity in older people. Eur. Geriatr. Med. 2013, 4, 82–85. [Google Scholar] [CrossRef]
- Lawton, M.; Brody, E. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Jerome, G.; Ko, S.; Kauffman, D.; Studenski, S.; Ferrucci, L.; Simonsick, E. Gait characteristics associated with walking speed decline in older adults: Results from the Baltimore longitudinal study of aging. Arch. Gerontol. Geriatr. 2015, 60, 239–343. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.; Bear-Lehman, J.; Desrosiers, J.; Massy-Westropp, N.; Mathiowetz, V. Average grip strength: A meta-analysis of data obtained with Jamar dynamometer from individuals 75 years or more. J. Geriatr. Phys. Ther. 2007, 30, 28–30. [Google Scholar] [CrossRef] [PubMed]
- Taekema, D.; Gussekloo, J.; Maier, A.; Westendorp, R.; De Craen, A. Handgrip strength as a predictor of functional, psychological and social health: A prospective population-based study among the oldest old. Age Ageing 2010, 39, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.; Syddall, H.; Patel, H.; Martin, H.; Cooper, C.; Sayer, A.A. Is grip strength a good marker of physical performance among community-dwelling older people? J. Nutr. Health Aging 2012, 16, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Laukkanen, P.; Kauppinen, M.; Era, P.; Heikkinen, E. Factors related to coping with physical and instrumental activities of daily living among people born in 1904–1923. Int. J. Geriatr. Psychiatry 1993, 8, 287–296. [Google Scholar] [CrossRef]
- Elo, S.; Isola, A. Interviewing the elderly: Special characteristics of the interview study. J. Nurs. Sci. 2008, 20, 215–225. [Google Scholar]
| Instruments | Assessment Categories and Items | ||||
|---|---|---|---|---|---|
| Environment wellness instrument (self-reported social environment) | Pleasantness of social environment (2 items) | Feeling of social restrictiveness (3 items) | Interpersonal relationships (4 items) | Getting support (3 items) | |
| Oldwellactive questionnaire and SPPB (background characteristics and physical performance) | Background characteristics (10 items) | Do you cope independently with the following IADL tasks? (11 items) | Grip strength, Kg (Jamar dynamometer) | Lower body strength, No. of chair stands in 30 s | Usual walking speed, 4 m (SPPB) |
| Pleasantness of Social Environment and Feelings of Social Restrictiviness | 3 Months | 12 Months | Increased | Decreased | No Change | Significance * | ||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n (%) | n (%) | n (%) | p-Value * | |
| Pleasantness of social environment | ||||||||
| “The community where I live is pleasant” | ||||||||
| Fully agree | 23 | (32) | 41 | (58) | ||||
| Somewhat agree | 44 | (62) | 25 | (35) | ||||
| Somewhat disagree | 4 | (6) | 5 | (7) | ||||
| Fully disagree | 0 | (0) | 0 | (0) | ||||
| 26 (37) | 11 (15) | 37 (53) | 0.010 | |||||
| “I have enough meaningful activities at home” | ||||||||
| Fully agree | 29 | (41) | 29 | (41) | ||||
| Somewhat agree | 17 | (24) | 21 | (30) | ||||
| Somewhat disagree | 20 | (28) | 12 | (17) | ||||
| Totally disagree | 5 | (7) | 9 | (12) | ||||
| 17 (24) | 18 (25) | 36 (51) | 1.000 | |||||
| Feeling of social restrictiveness | ||||||||
| “I feel that at home I have freedom to do whatever I like” | ||||||||
| Fully agree | 58 | (82) | 62 | (87) | ||||
| Somewhat agree | 9 | (13) | 2 | (3) | ||||
| Somewhat disagree | 1 | (1) | 5 | (7) | ||||
| Totally disagree | 3 | (4) | 2 | (3) | ||||
| 10 (14) | 8 (11) | 53 (77) | 0.803 | |||||
| “My life is too limited to the home environment” | ||||||||
| Fully agree | 24 | (34) | 21 | (30) | ||||
| Somewhat agree | 21 | (30) | 28 | (39) | ||||
| Somewhat disagree | 13 | (18) | 15 | (21) | ||||
| Fully disagree | 13 | (18) | 7 | (10) | ||||
| 20 (28) | 23 (32) | 28 (39) | 0.499 | |||||
| “Changes in my physical condition have limited my social interaction” | ||||||||
| Fully agree | 27 | (38) | 27 | (38) | ||||
| Somewhat agree | 18 | (25) | 23 | (32) | ||||
| Somewhat disagree | 5 | (7) | 4 | (6) | ||||
| Fully disagree | 21 | (30) | 17 | (24) | 12(17) | 17 (24) | 42(59) | 0.035 |
| Interpersonal Relationships and Getting Support | 3 Months | 12 Months | Increased | Decreased | No Change | Significance * | ||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n (%) | n (%) | n (%) | p-Value * | |
| Interpersonal relationships | ||||||||
| ´´I meet enough people close to me“ | ||||||||
| Fully agree | 32 | (45) | 38 | (53) | ||||
| Somewhat agree | 12 | (17) | 21 | (30) | ||||
| Somewhat disagree | 23 | (32) | 9 | (13) | ||||
| Fully disagree | 4 | (6) | 3 | (4) | ||||
| 28 (39) | 13 (18) | 30 (42) | 0.023 | |||||
| “I have enough contact with close people (phone, Skype)” | ||||||||
| Fully agree | 46 | (65) | 62 | (87) | ||||
| Somewhat agree | 12 | (17) | 4 | (6) | ||||
| Somewhat disagree | 11 | (16) | 5 | (7) | ||||
| Fully disagree | 2 | (3) | 0 | (0) | ||||
| 21 (30) | 5 (7) | 45 (63) | 0.001 | |||||
| “I feel that people close to me care about me” | ||||||||
| Fully agree | 54 | (76) | 54 | (76) | ||||
| Somewhat agree | 14 | (20) | 13 | (18) | ||||
| Somewhat disagree | 2 | (3) | 1 | (1) | ||||
| Fully disagree | 1 | (1) | 3 | (4) | ||||
| 7 (10) | 7 (10) | 57 (80) | 0.631 | |||||
| “People close to me bring joy into my life” | ||||||||
| Fully agree | 48 | (68) | 45 | (63) | ||||
| Somewhat agree | 20 | (28) | 24 | (34) | ||||
| Somewhat disagree | 3 | (4) | 2 | (3) | ||||
| Fully disagree | 0 | (0) | 0 | (0) | ||||
| 10 (14) | 14 (20) | 47 (66) | 0.715 | |||||
| Getting support | ||||||||
| “I get enough help from people close to me when I need it” | ||||||||
| Fully agree | 51 | (72) | 46 | (65) | ||||
| Somewhat agree | 10 | (14) | 16 | (23) | ||||
| Somewhat disagree | 9 | (13) | 7 | (10) | ||||
| Fully disagree | 1 | (1) | 2 | (3) | ||||
| 13 (18) | 16 (23) | 42 (59) | 0.529 | |||||
| “I get enough support from peers, when I need it” | ||||||||
| Fully agree | 19 | (27) | 19 | (27) | ||||
| Somewhat agree | 16 | (23) | 17 | (24) | ||||
| Somewhat disagree | 20 | (28) | 18 | (25) | ||||
| Fully disagree | 16 | (23) | 17 | (24) | ||||
| 18 (25) | 24 (34) | 39 (55) | 1.000 | |||||
| “I have no problems when moving outside home” | ||||||||
| Fully agree | 26 | (37) | 20 | (28) | ||||
| Somewhat agree | 11 | (16) | 9 | (13) | ||||
| Somewhat disagree | 18 | (25) | 14 | (20) | ||||
| Fully disagree | 16 | (22) | 28 | (39) | ||||
| 11 (15) | 25 (35) | 35 (49) | 0.019 | |||||
| Background Characteristics | n | % |
|---|---|---|
| Age (years) | ||
| 55–64 | 4 | 5 |
| 65–74 | 9 | 11 |
| 75–84 | 42 | 52 |
| 85–94 | 26 | 32 |
| Gender | ||
| Female | 57 | 70 |
| Male | 24 | 30 |
| Marital status | ||
| Married | 27 | 33 |
| Unmarried | 7 | 9 |
| Widowed | 30 | 37 |
| Divorced | 17 | 21 |
| Housing | ||
| Lived alone | 61 | 75 |
| Lived with someone (cohabited) | 20 | 25 |
| Children | ||
| Has children | 68 | 84 |
| No children | 13 | 16 |
| Service use | ||
| No services | 23 | 28 |
| Services | 58 | 72 |
| Financial situation | ||
| Very good | 2 | 3 |
| Good | 23 | 28 |
| Moderate | 53 | 65 |
| Poor or very poor | 3 | 4 |
| Mood at the moment | ||
| Very good | 1 | 1 |
| Good | 22 | 31 |
| Average | 44 | 62 |
| Bad | 4 | 6 |
| Worried about being depressed or hopeless in the last month | ||
| Yes | 24 | 34 |
| No | 47 | 66 |
| Diseases | ||
| Coronary heart disease | 72 | 88 |
| Musculoskeletal disease | 59 | 73 |
| Neurological disease | 21 | 26 |
| Diabetes | 14 | 17 |
| Respiratory organ disease | 13 | 16 |
| Cancer | 4 | 5 |
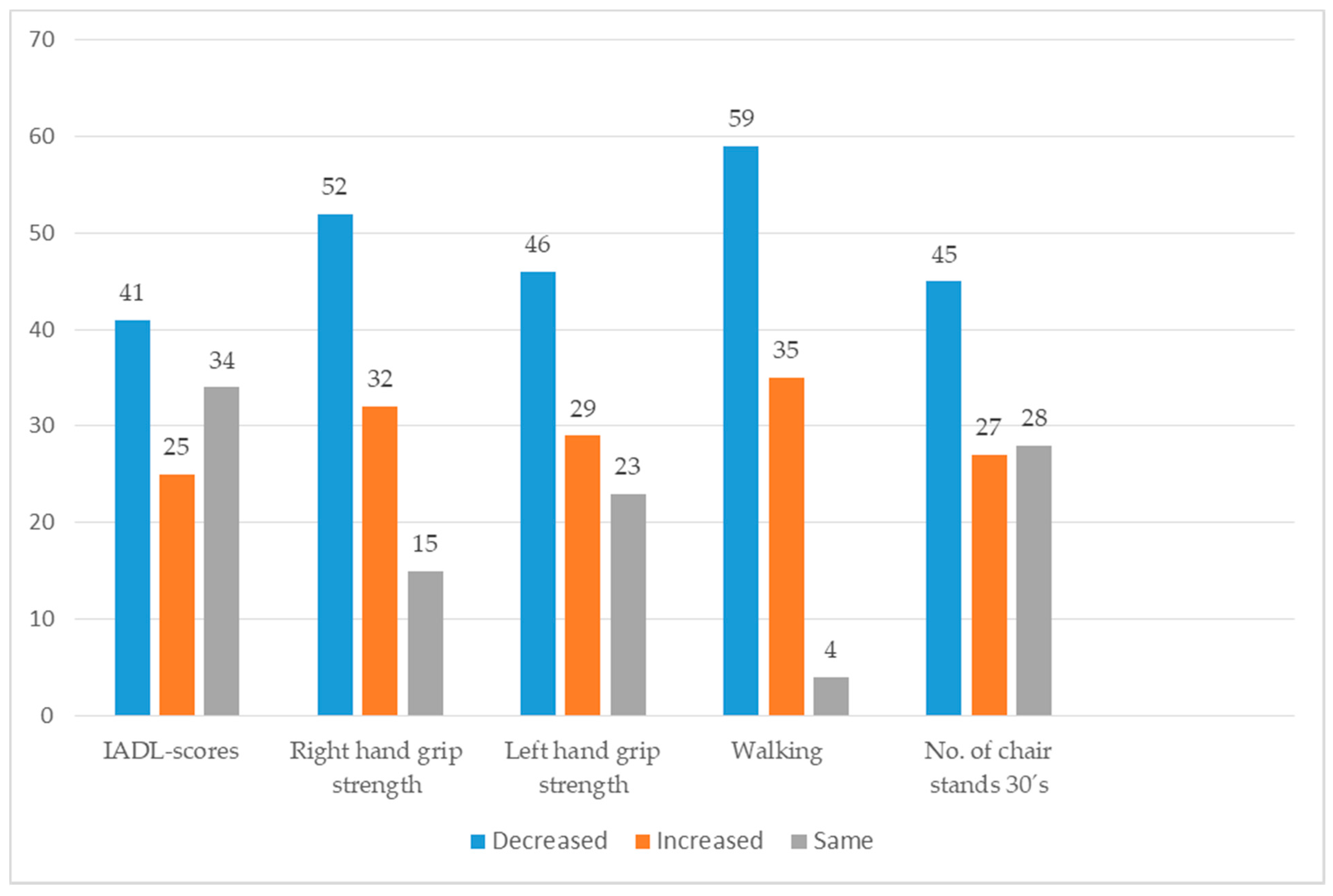
| Measured Physical Performance | 3 Months | 12 Months | 3–12 Months | Significance * |
|---|---|---|---|---|
| Mean | Mean | Change | p-Value | |
| Usual walking 4 m (s) (Walking speed m/s) | 6.27 | 7.64 | +1.37 | 0.002 |
| 0.63 | 0.52 | –0.11 | ||
| Grip strength, right hand (kg) | 22.94 | 21.20 | –1.74 | 0.033 |
| Grip strength, left hand (kg) | 20.80 | 20.28 | –0.52 | 0.410 |
| IADL scores | 14.65 | 13.82 | –0.83 | 0.002 |
| No. of Chair stands in 30 s’ | 6.58 | 6.13 | –0.45 | 0.150 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lotvonen, S.; Kyngäs, H.; Koistinen, P.; Bloigu, R.; Elo, S. Social Environment of Older People during the First Year in Senior Housing and Its Association with Physical Performance. Int. J. Environ. Res. Public Health 2017, 14, 960. https://doi.org/10.3390/ijerph14090960
Lotvonen S, Kyngäs H, Koistinen P, Bloigu R, Elo S. Social Environment of Older People during the First Year in Senior Housing and Its Association with Physical Performance. International Journal of Environmental Research and Public Health. 2017; 14(9):960. https://doi.org/10.3390/ijerph14090960
Chicago/Turabian StyleLotvonen, Sinikka, Helvi Kyngäs, Pentti Koistinen, Risto Bloigu, and Satu Elo. 2017. "Social Environment of Older People during the First Year in Senior Housing and Its Association with Physical Performance" International Journal of Environmental Research and Public Health 14, no. 9: 960. https://doi.org/10.3390/ijerph14090960





