Community Capacity Building for Physical Activity Promotion among Older Adults—A Literature Review
Abstract
:1. Introduction
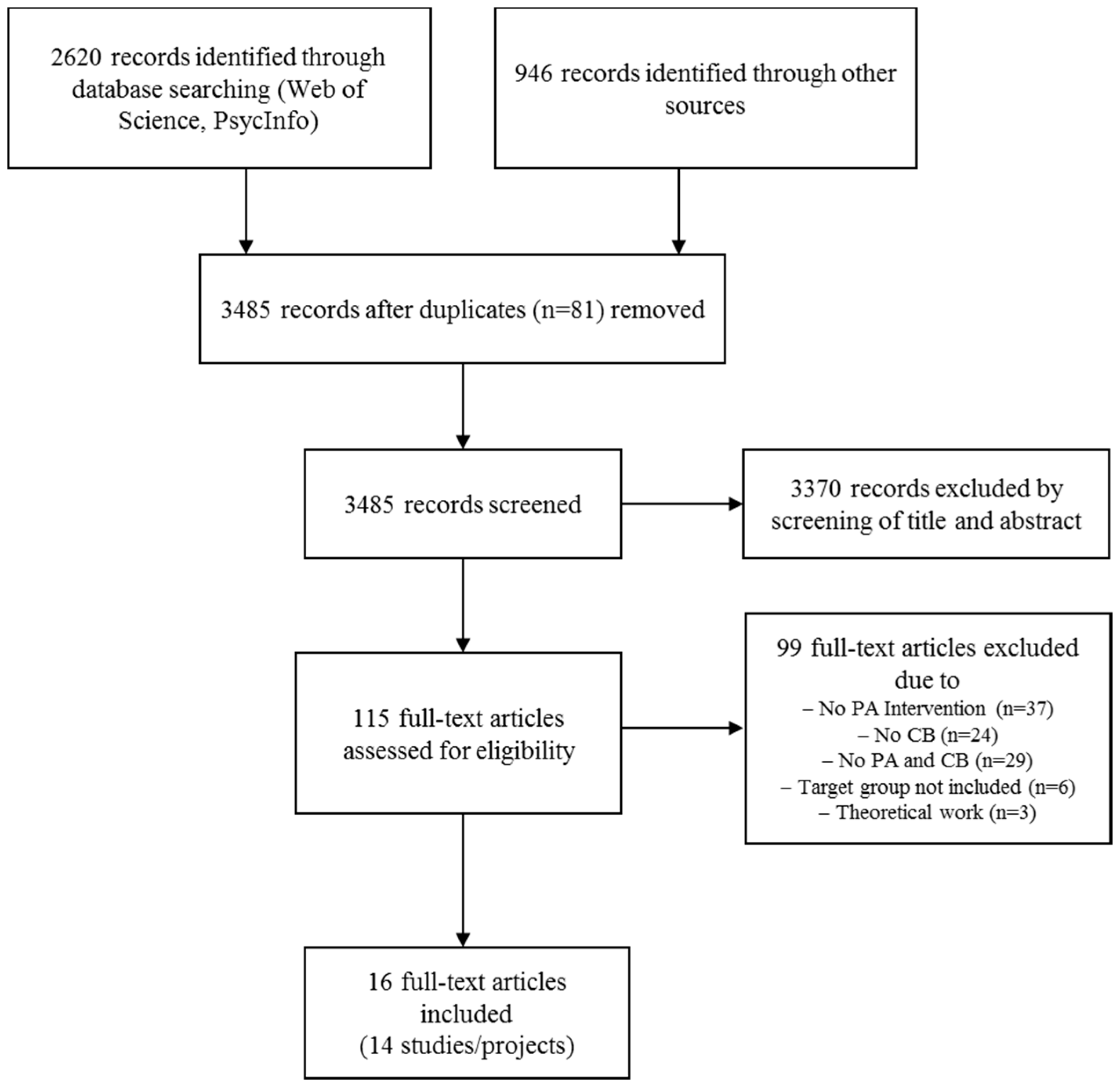
2. Materials and Methods
3. Results
3.1. Capacity Building Strategies
3.1.1. Community-Based Coalition and Network Building
3.1.2. Training of Professionals
3.1.3. Training of Laypersons
3.1.4. Strengthening Competence and Awareness in the Target Population
3.1.5. Allocation of Financial Resources
3.2. Success of the Strategies
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Byberg, L.; Melhus, H.; Gedeborg, R.; Sundstrom, J.; Ahlbom, A.; Zethelius, B.; Berglund, L.G.; Wolk, A.; Michaelsson, K. Total mortality after changes in leisure time physical activity in 50 year old men: 35 year follow-up of population based cohort. Br. Med. J. 2009, 338. [Google Scholar] [CrossRef] [PubMed]
- Fries, J.F.; Bruce, B.; Chakravarty, E. Compression of morbidity 1980–2011: A focused review of paradigms and progress. J. Aging Res. 2011, 2011, 261702. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Chida, Y. Walking and primary prevention: A meta-analysis of prospective cohort studies. Br. J. Sports Med. 2008, 42, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Krug, S.; Jordan, S.; Mensink, G.B.; Muters, S.; Finger, J.; Lampert, T. Physical activity: Results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; von der Lippe, E. Participation in health behaviour change programmes. Results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 878–884. [Google Scholar] [CrossRef] [PubMed]
- Shareck, M.; Frohlich, K.L.; Poland, B. Reducing social inequities in health through settings-related interventions—A conceptual framework. Glob. Health Promot. 2013, 20, 39–52. [Google Scholar] [CrossRef] [PubMed]
- WHO. Physical Activity Promotion in Socially Disadvantaged Groups: Principles for Action; World Health Organization: Copenhagen, Denmark, 2013. [Google Scholar]
- WHO. The Ottawa Charter for Health Promotion; World Health Organization: Geneva, Switzerland, 1986. [Google Scholar]
- Bloch, P.; Toft, U.; Reinbach, H.C.; Clausen, L.T.; Mikkelsen, B.E.; Poulsen, K.; Jensen, B.B. Revitalizing the setting approach—Supersettings for sustainable impact in community health promotion. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 118. [Google Scholar] [CrossRef] [PubMed]
- Mummery, W.K.; Brown, W.J. Whole of community physical activity interventions: Easier said than done. Br. J. Sports Med. 2009, 43, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Simmons, A.; Reynolds, R.C.; Swinburn, B. Defining community capacity building: Is it possible? Prev. Med. 2011, 52, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Rutten, A.; Gelius, P. Building policy capacities: An interactive approach for linking knowledge to action in health promotion. Health Promot. Int. 2014, 29, 569–582. [Google Scholar] [CrossRef] [PubMed]
- WHO. Jakarta Declaration on Leading Health Promotion into the 21st Century; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Smith, B.J.; Tang, K.C.; Nutbeam, D. WHO Health Promotion Glossary: New terms. Health Promot. Int. 2006, 21, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Labonte, R.; Woodard, G.B.; Chad, K.; Laverack, G. Community capacity building: A parallel track for health promotion programs. Can. J. Public Health 2002, 93, 181–182. [Google Scholar] [PubMed]
- McLeroy, K.R.; Norton, B.L.; Kegler, M.C.; Burdine, J.N.; Sumaya, C.V. Community-based interventions. Am. J. Public Health 2003, 93, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Stith, S.; Pruitt, I.; Dees, J.E.; Fronce, M.; Green, N.; Som, A.; Linkh, D. Implementing community-based prevention programming: A review of the literature. J. Prim. Prev. 2006, 27, 599–617. [Google Scholar] [CrossRef] [PubMed]
- Stanford School of Medicine. Assessing Scientific Admissibility and Merit of Published Articles. Critical Appraisal Form. Available online: http://peds.stanford.edu/Tools/documents/Critical_Appraisal_Form_CGP.pdf (accessed on 26 June 2015).
- Center for Evidence-Based Management. Critical Appraisal of A Case Study. Available online: http://www.cebma.org/wp-content/uploads/Critical-Appraisal-Questions-for-a-Case-Study.pdf (accessed on 26 June 2015).
- Sotomayor, M.; Dominguez, A.; Pawlik, F. Building community capacity for health promotion in a Hispanic community. Prev. Chronic Dis. 2007, 4, A16. [Google Scholar] [PubMed]
- Kolb, M.; Diketmüller, R.; Steininger, C. Building Policy Capacities for Health Promotion through Physical Activity among Sedentary Older People—Endbericht Institut für Sportwissenschaft; Universität Wien: Wien, Austria, 2011. [Google Scholar]
- Abuzahra, M.; Hinterberger, M. Reifer Lebensgenuss—Endbericht; FH Joanneum: Bad Gleichenberg, Austria, 2012. [Google Scholar]
- Sundermeier, A. Bewegt Leben—Mehr Vom Leben; Kivi e.V.: Siegburg, Germany, 2011. [Google Scholar]
- Jitramontree, N.; Chatchaisucha, S.; Thaweeboon, T.; Kutintara, B.; Intanasak, S. Action research development of a fall prevention program for thai community-dwelling older persons. Pac. Rim Int. J. Nurs. Res. 2015, 19, 11. [Google Scholar]
- Zgibor, J.C.; Schlenk, E.A.; Vater, L.; Kola, S.; Vander Bilt, J.; Woody, S.; Jacob, M.E.; Lo-Ciganic, W.H.; Brenckle, A.; Brandenstein, J.; et al. Partnership Building and Implementation of an Integrated Healthy-Aging Program. Prog. Community Health Partnersh. 2016, 10, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Nunez, D.E.; Armbruster, C.; Phillips, W.T.; Gale, B.J. Community-based senior health promotion program using a collaborative practice model: The Escalante Health Partnerships. Public Health Nurs. 2003, 20, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Forschungsgesellschaft für Gerontologie (FFG). Aktionsbündnis “Gesund Älter Werden in EVING”; Forschungsgesellschaft für Gerontologie e.V.: Dortmund, Germany, 2012. [Google Scholar]
- Layne, J.E.; Sampson, S.E.; Mallio, C.J.; Hibberd, P.L.; Griffith, J.L.; Das, S.K.; Flanagan, W.J.; Castaneda-Sceppa, C. Successful dissemination of a community-based strength training program for older adults by peer and professional leaders: The people exercising program. J. Am. Geriatr. Soc. 2008, 56, 2323–2329. [Google Scholar] [CrossRef] [PubMed]
- Hooker, S.P.; Cirill, L.A. Evaluation of community coalitions ability to create safe, effective exercise classes for older adults. Eval. Program Plan. 2006, 29, 242–250. [Google Scholar] [CrossRef]
- Luten, K.A.; Reijneveld, S.A.; Dijkstra, A.; de Winter, A.F. Reach and effectiveness of an integrated community-based intervention on physical activity and healthy eating of older adults in a socioeconomically disadvantaged community. Health Educ. Res. 2016, 31, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Neuhold, C. Evaluationsbericht: Modellprojekt Lebenswerte Lebenswelten für Ältere; Medizinische Universität Graz: Graz, Austria, 2008. [Google Scholar]
- Reis-Klingspiegl, K. Endbericht: Lebenswerte Lebenswelten für Ältere; Medizinische Universität Graz: Graz, Austria, 2008. [Google Scholar]
- Guse, C.E.; Peterson, D.J.; Christiansen, A.L.; Mahoney, J.; Laud, P.; Layde, P.M. Translating a fall prevention intervention into practice: A randomized community trial. Am. J. Public Health 2015, 105, 1475–1481. [Google Scholar] [CrossRef] [PubMed]
- Peterson, D.J.; Christiansen, A.L.; Guse, C.E.; Layde, P.M. Community translation of fall prevention interventions: The methods and process of a randomized trial. J. Community Psychol. 2015, 43, 1005–1018. [Google Scholar] [CrossRef]
- West, D.S.; Bursac, Z.; Cornell, C.E.; Felix, H.C.; Fausett, J.K.; Krukowski, R.A.; Lensing, S.; Love, S.J.; Prewitt, T.E.; Beck, C. Lay health educators translate a weight-loss intervention in senior centers: A randomized controlled trial. Am. J. Prev. Med. 2011, 41, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Hawe, P.; Noort, M.; King, L.; Jordens, C. Multiplying health gains: The critical role of capacity-building within health promotion programs. Health Policy 1997, 39, 29–42. [Google Scholar] [CrossRef]
- McAuley, L.; Pham, B.; Tugwell, P.; Moher, D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? Lancet 2000, 356, 1228–1231. [Google Scholar] [CrossRef]
- Marlier, M.; Cardon, G.; De Bourdeaudhuij, I.; Willem, A. A capacity building approach to increase sports participation in disadvantaged urban communities: A multilevel analysis. J. Urban Health 2014, 91, 1114–1128. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.M.; Adeney, K.L.; Shinn, C.; Safranek, S.; Buckner-Brown, J.; Krause, L.K. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst. Rev. 2015, 6, CD009905. [Google Scholar]
- O’Mara-Eves, A.; Brunton, G.; Oliver, S.; Kavanagh, J.; Jamal, F.; Thomas, J. The effectiveness of community engagement in public health interventions for disadvantaged groups: A meta-analysis. BMC Public Health 2015, 15, 129. [Google Scholar] [CrossRef] [PubMed]
| Authors | Study Design | Setting | Target Group Sample Size | Quality Appraisal (Number of ‘Yes’) |
|---|---|---|---|---|
| Sotomayor et al. 2007 [23] | Case study | Nueces County, South Texas, USA | Middle-aged and elderly Latinos N = not specified | 5/10 |
| Kolb et al. 2011 [24] | Case study | Area of Vienna, Austria | Inactive, older adults N = 12 (focus group) | 7/10 |
| Abuzahra & Hinterberger 2012 [25] | Case study | 5 communities in Steiermark, Austria | Older adults (≥50 years) N = not specified | 4/10 |
| Sundermeier 2011 [26] | Case study | 8 communities in the Rhein-Sieg area, Germany | Older adults (≥60 years)/ N = not specified | 6/10 |
| Jitramontree et al. 2015 [27] | Case study | Community in West Bangkok, Thailand | Older adults (≥60years), family members, PHNs, health volunteers, community leader N = 80 | 5/10 |
| Zgibor et al. 2016 [28] | Survey | 54 communities in Allegheny County, PA, USA | Older adults (≥50 years) N = 462 | 6/10 |
| Nunez et al. 2003 [29] | Survey | Escalante, UT, USA | Older adults (≥50 years) N = 135 | 4/10 |
| FGG 2012 [30] | Survey | Urban district Dortmund-Eving, Germany | Older adults, low SES, migrant background, or limited mobility N = 55 | 4/10 |
| Layne et al. 2008 [31] | Survey | Senior centers, community centers, and churches in New England, USA | Older adults (≥50 years) N = 244 trainers N = 2217 participants | 3/10 |
| Hooker & Cirill 2006 [32] | Cohort study | 28 counties in California, USA | Older adults (≥50 years) N = 167 (PA class participants) N = 90 (coalition members) | 4/10 |
| Luten et al. 2016 [33] | Cohort study (CBA) | Disadvantaged community in Groningen, The Netherlands | Older adults (≥50 years) N = 641 | 8/10 |
| Neuhold 2008, Reis-Kling-spiegl 2008 [34,35] | Cohort study (BA) | 13 communities in Graz and Voitsberg, Austria | Older adults (≥60 years)/ N = 908 | 5/10 |
| Guse et al. 2015/ Peterson et al. 2015 [36,37] | CRCT | 20 Counties in Wisconsin, USA | Older adults (≥65 years)/ N = 817 | 6/11 |
| West et al. 2011 [38] | CRCT | 15 senior centers in Arkansas, USA | Older adults (≥60 years), obese (BMI ≥ 30) N = 228 | 6/11 |
| Authors | Intervention Components | Outcome Measures | Results |
|---|---|---|---|
| Case studies | |||
| Sotomayor et al. 2007 [23] | Community coalitions and networks: Community-wide health forums and coalitions consisting of elected officials, older adults, representatives of community groups and agencies Training of laypersons: Training of lay health educators Strengthening competence and awareness in the population: Local media campaigns; Group sessions for residents providing health-related knowledge and social support | None | Anecdotal evidence that the activities improved the health of the target group by encouraging use of appropriate health services |
| Kolb et al. 2011 [24] | Community coalitions and networks: Building inter-sectoral alliance for PA; Quality standards for PA programs for older adults Strengthening competence and awareness in the population: Launch of a website for PA for older adults |
|
|
| Abuzahra & Hinterberger 2012 [25] | Community coalitions and networks: Community group formation in five municipalities including representatives of regional development and tourism agencies Strengthening competence and awareness in the population: Lectures and classes on PA, nutrition, sexuality and vitality Allocation of financial resources: Local projects applied for funding |
|
|
| Sundermeier 2011 [26] | Community coalitions and networks: Community-based working groups were formed during meetings with local key persons in four pilot municipalities Training of professionals: Training of management skills and public relations issues for network members; Training of PA class instructors Strengthening competence and awareness in the population: Information events and special days for mapping existing exercise/PA programs |
|
|
| Jitramontree et al. 2015 [27] | Community coalitions and networks: Community participatory planning process with community leader, public health nurses, public health volunteers, older adults, family members Strengthening competence and awareness in the population: Risk assessment among older adults; Dissemination of results via community broadcast system; Development and dissemination of a fall prevention handbook; Exercise and cane use training program; Home visits; Reminder calls | Perceived benefits of the program |
|
| Cross-sectional surveys | |||
| Zgibor et al. 2016 [28] | Community coalitions and networks: Formation of research-funding agency partnership; Formalized site selection process Training of professionals: Training for instructors Strengthening competence and awareness in the population: PA and health education group sessions |
|
|
| Nunez et al. 2003 [29] | Community coalitions and networks: University-community partnership (university college of nursing, local health department, and a community action agency) Strengthening competence and awareness in the population: PA courses for older adults; Health education (e.g., healthy nutrition); Screening for hypertension, diabetes and high cholesterol |
|
|
| FGG 2012 [30] | Community coalitions and networks: University-led community coalition including the local senior office, (intercultural) community centers, peers and other stakeholders Strengthening competence and awareness in the population: Public lectures on health promotion; Provision of PA and healthy eating classes |
|
|
| Layne et al. 2008 [31] | Training of professionals: Train-the-trainer workshops for PA class instructors (‘leadership training’) Training of laypersons: Same training as for the professionals Strengthening competence and awareness in the population: PA classes for older adults |
|
|
| Cohort studies | |||
| Hooker & Cirill 2006 [32] | Community coalitions and networks: Coalition led by administrative and program personnel from local health departments and area agency on aging Training of professionals: Training of PA class instructors Strengthening competence and awareness in the population: PA classes for older adults Allocation of financial resources: Funding for local implementation |
|
|
| Luten et al. 2016 [33] | Community coalitions and networks: Local healthcare professionals and peers were involved in the intervention development and implementation Strengthening competence and awareness in the population: Local media campaign (posters, radio spots, radio interviews, advertorials and press reports, newsletters, flyers, Goud Leven guide, website) |
|
|
| Neuhold 2008/Reis-Klingspiegl 2008 [34,35] | Community coalitions and networks: Senior networks and platforms in 13 municipalities Training for professionals: Management skills training for project leaders Allocation of financial resources: Local projects applied for funding |
|
|
| Cluster randomized controlled | |||
| Guse et al. 2015/Peterson et al. 2015 [36,37] | Community coalitions and networks: Research-led coalition with aging units and local health offices; Provision of technical assistance Training of professionals: Fall prevention instructor training, group facilitation skills, marketing and recruitment techniques Strengthening competence and awareness in the population: Local events (Fall Prevention Awareness Days); Dissemination of local survey results; Fall prevention classes for older adults Allocation of financial resources: Funding for local implementation |
|
|
| West et al. 2011 [38] | Training of laypersons: Training of lay health educators Strengthening competence and awareness in the population: 12-week group-based standardized lifestyle intervention |
|
|
| Facilitating Factors | Barriers |
|---|---|
| Early involvement of a constant local cooperation partner that takes over responsibility | Reliance (e.g., financial) on a single project partner |
| Written agreements with project partners to improve engagement and collaboration | Administrative and political interlocking between network partners |
| Conscientious choice of project partners and stakeholders (e.g., build a group that is able to take decisions, inclusion of stakeholders from all community sectors) | Conflicts of interest inside the network |
| Strong integration of local politics | Competitive thinking among the network partners |
| Target group involvement during planning phase | Change of persons in charge within the project team |
| Using synergies from existing networks | A narrow project schedule |
| Allocation of financial resources by the municipality | Difficulties in understanding the workshop content among laypersons |
| Transparent information flow to keep the partners informed | Unclear allocation of roles by local authorities and other organizations involved |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ubert, T.; Forberger, S.; Gansefort, D.; Zeeb, H.; Brand, T. Community Capacity Building for Physical Activity Promotion among Older Adults—A Literature Review. Int. J. Environ. Res. Public Health 2017, 14, 1058. https://doi.org/10.3390/ijerph14091058
Ubert T, Forberger S, Gansefort D, Zeeb H, Brand T. Community Capacity Building for Physical Activity Promotion among Older Adults—A Literature Review. International Journal of Environmental Research and Public Health. 2017; 14(9):1058. https://doi.org/10.3390/ijerph14091058
Chicago/Turabian StyleUbert, Tobias, Sarah Forberger, Dirk Gansefort, Hajo Zeeb, and Tilman Brand. 2017. "Community Capacity Building for Physical Activity Promotion among Older Adults—A Literature Review" International Journal of Environmental Research and Public Health 14, no. 9: 1058. https://doi.org/10.3390/ijerph14091058







