The Effect of Taichi Practice on Attenuating Bone Mineral Density Loss: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
2. Methods
2.1. Data Sources and Search Strategy
2.2. Inclusion Criteria
2.3. Data Selection
2.4. Data Extraction
2.5. Methodological Quality of Assessment
2.6. Statistical Analysis
3. Results
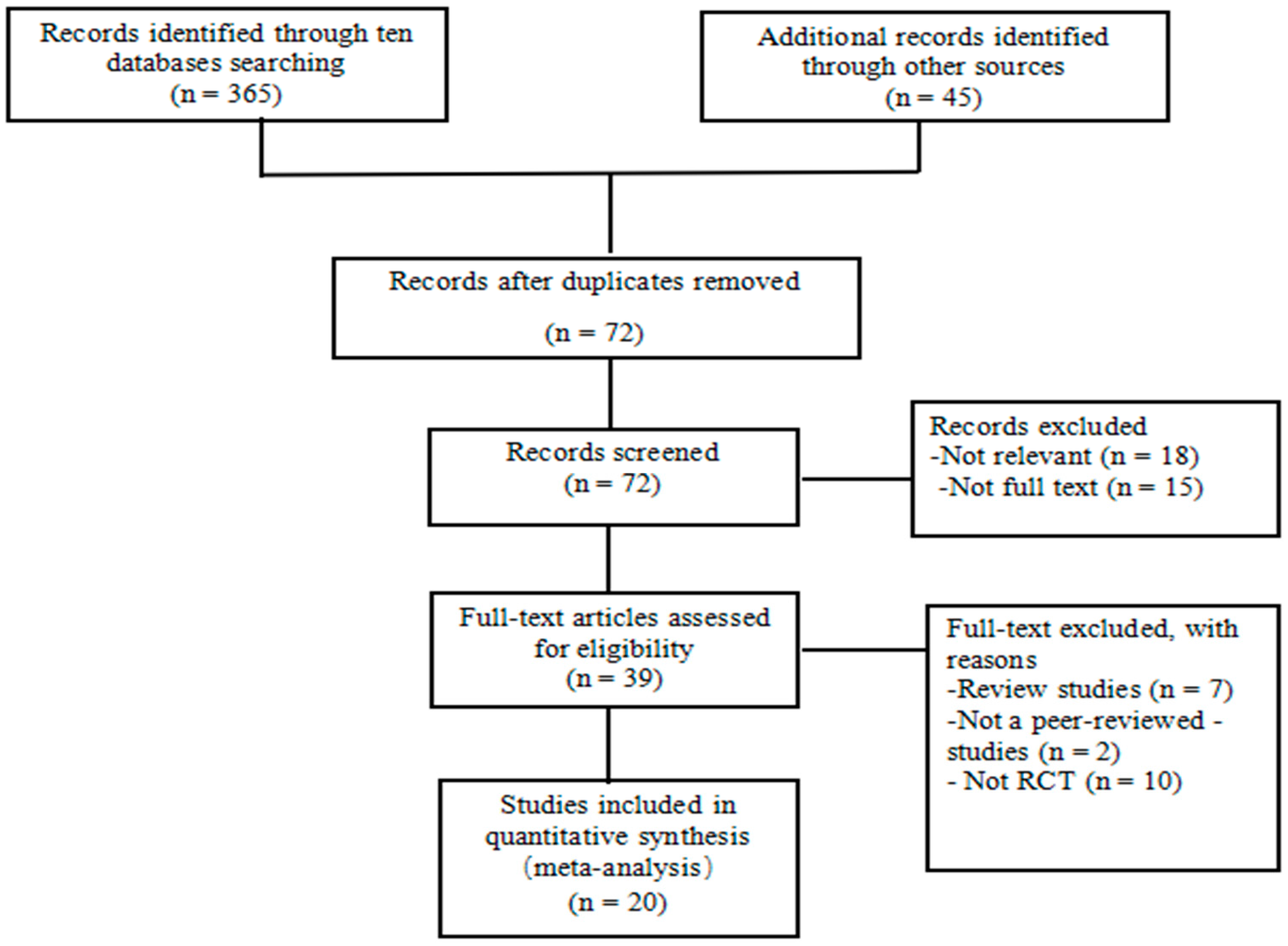
3.1. Literature Search
3.2. Study Characteristics
3.3. Methodological Quality
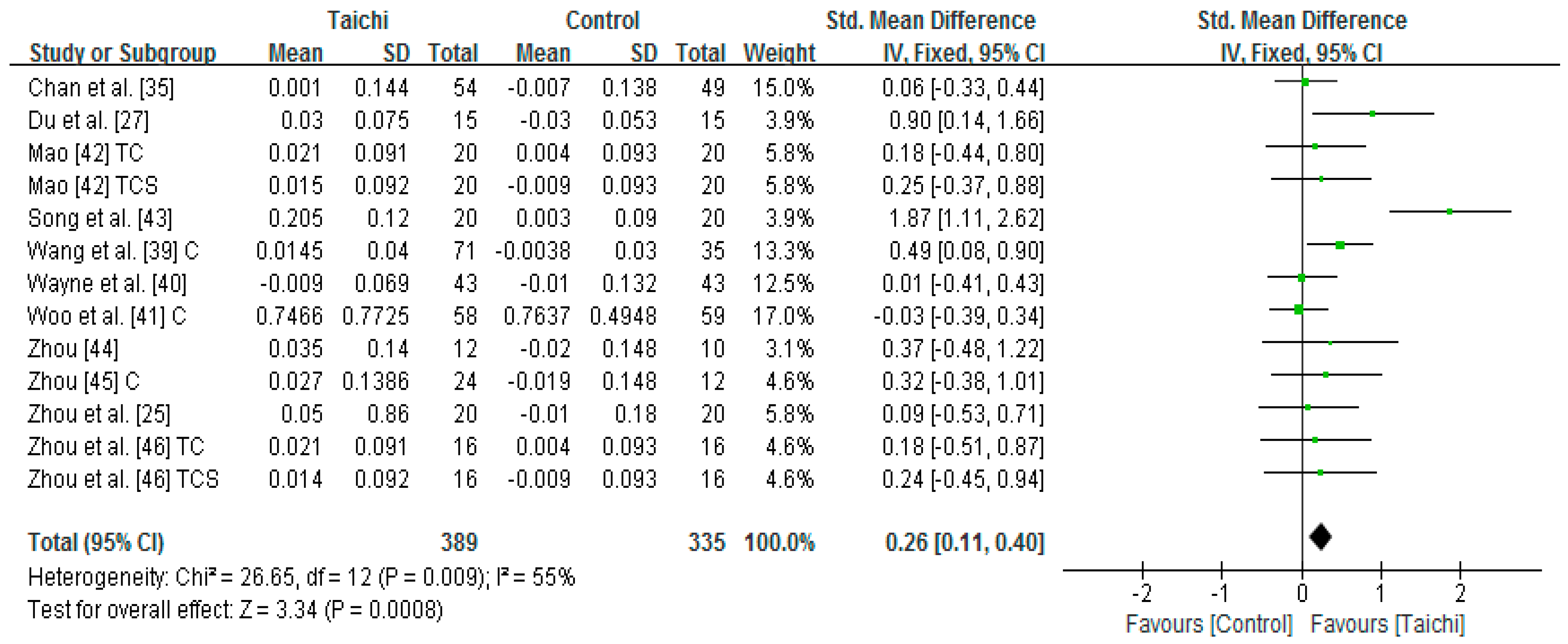
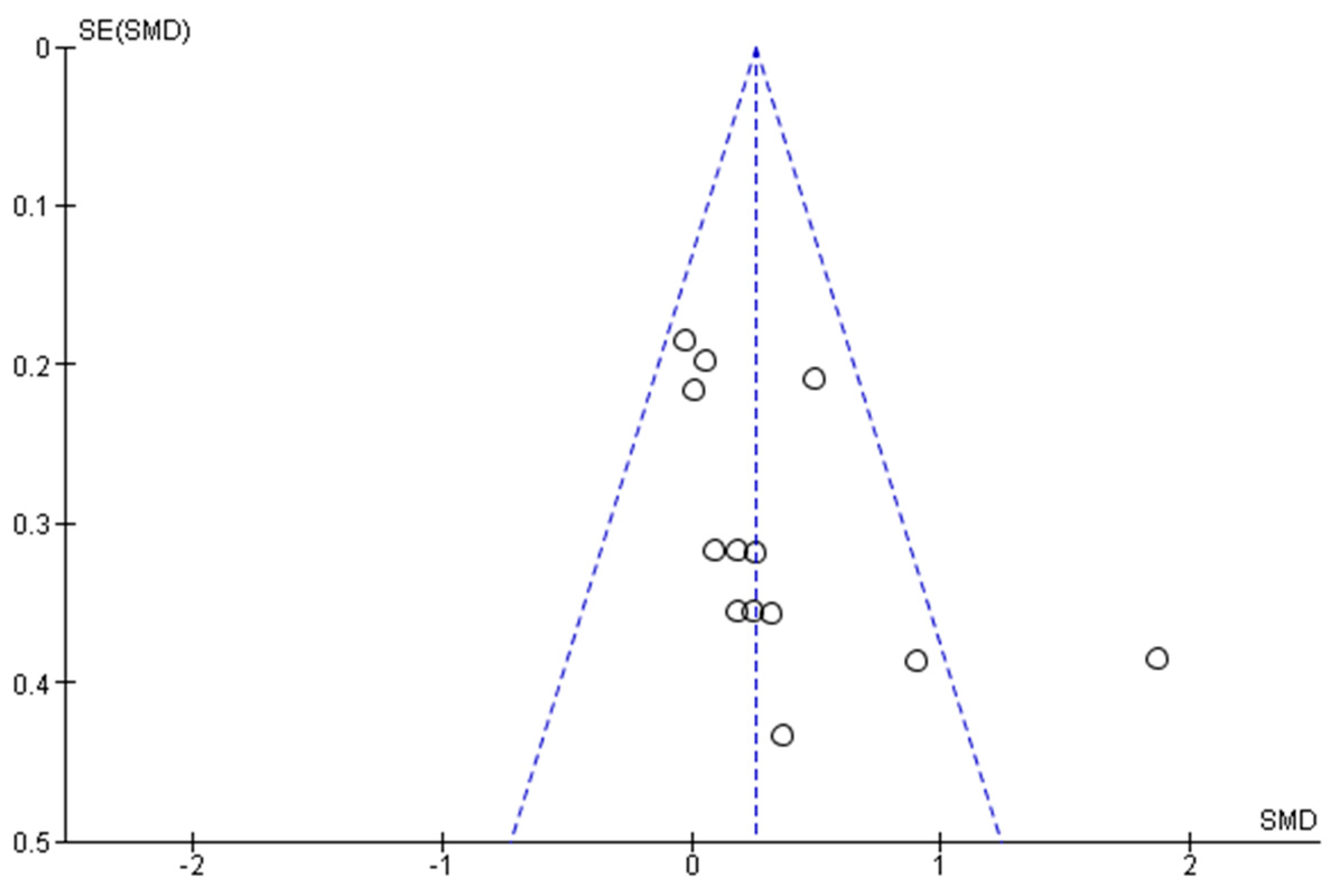
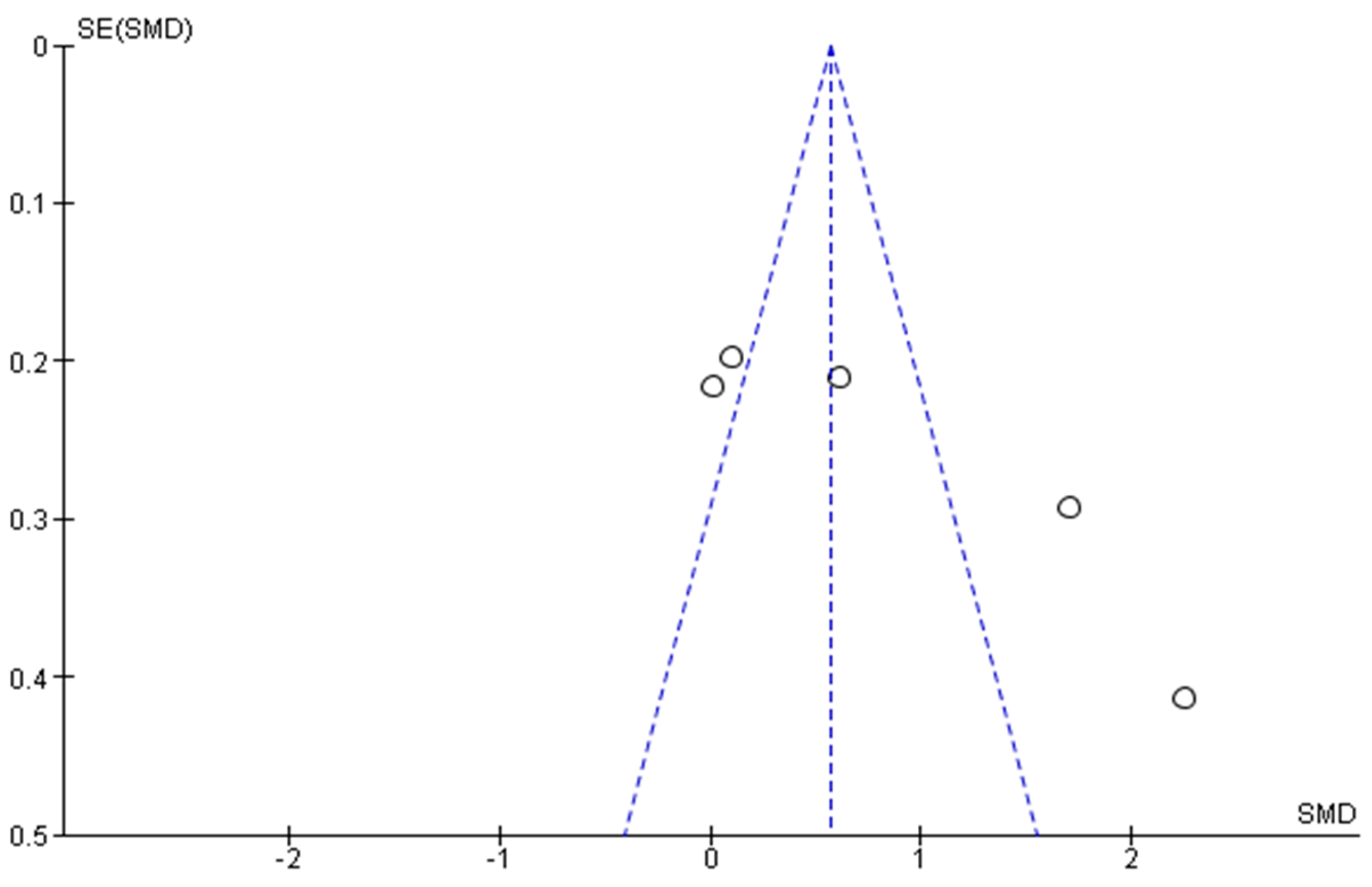
3.4. Meta-Analysis of Outcomes Measured
4. Discussion
4.1. Summary of Evidence
4.2. Bone Mineral Density
4.3. Bone Turnover Markers
4.4. Exercise Intervention
4.5. Study Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lou, L.; Zou, L.; Fang, Q.; Wang, H.; Liu, Y.; Tian, Z.; Han, Y. Effect of Taichi Soft-ball on function-related outcomes in Older Adults: A randomized controlled trial. Evid. Based Complement. Altern. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; SasaKi, J.E.; Wang, H.; Xiao, Z.; Fang, Q.; Zhang, M. A Systematic Review and Meta-Analysis Baduanjin Qigong for Health Benefits: Randomized Controlled Trials. Evid. Based Complement. Altern. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Kachan, D.; Olano, H.; Tannenbaum, S.L.; Annane, D.W.; Mehta, A.; Arheart, K.L.; Fleming, L.E.; Yang, X.; McClure, L.A.; Lee, D.J. Prevalence of Mindfulness Practices in the US Workforce: National Health Interview Survey. Prev. Chronic Dis. 2017, 14, 160034. [Google Scholar] [CrossRef] [PubMed]
- Tsai, P.F.; Beck, C.; Chang, J.Y.; Hagen, J.; Kuo, Y.F.; Roberson, P.K.; Rosengren, K.; Beuscher, L.; Doan, C.L.; Anand, K.J. The effect of Tai Chi on knee osteoarthritis pain in cognitively impaired elders: Pilot study. Geriatr. Nurs. 2009, 30, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Schmid, C.H.; Hibberd, P.L.; Kalish, R.; Roubenoff, R.; Rones, R.; McAlindon, T. Tai Chi is effective in treating knee osteoarthritis: A randomized controlled trial. Arthritis Care Res. 2009, 61, 1545–1553. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Schmid, C.H.; Rones, R.; Kalish, R.; Yinh, J.; Goldenberg, D.L.; Lee, Y.; McAlindon, T. A randomized trial of Tai Chi for fibromyalgia. N. Engl. J. Med. 2010, 363, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.D.; Sherman, C.A.; Mist, S.D.; Carson, J.W.; Bennett, R.M.; Li, F. A randomized controlled trial of 8-form Tai Chi improves symptoms and functional mobility in fibromyalgia patients. Clin. Rheumatol. 2012, 31, 1205–1214. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.Y.; Jeong, O.Y. The effect of Tai Chi movement in patients with rheumatoid arthritis. J. Korean Acad. Nurs. 2006, 36, 278–285. [Google Scholar] [CrossRef]
- Song, R.; Lee, E.O.; Lam, P.; Bae, S.C. Effects of Tai Chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: A randomized clinical trial. J. Rheumatol. 2003, 30, 2039–2044. [Google Scholar] [PubMed]
- Zou, L.; Wang, H.; Xiao, Z.; Fang, Q.; Zhang, M.; Li, T.; Du, G.; Liu, Y. Tai Chi for health benefits in patients with multiple sclerosis: A systematic review. PLoS ONE 2017, 12, e0170212. [Google Scholar] [CrossRef] [PubMed]
- Lan, C.; Lai, J.S.; Chen, S.Y.; Wong, M.K. Tai Chi Chuan to improve muscular strength and endurance in elderly individuals: A pilot study. Arch. Phys. Med. Rehabil. 2000, 81, 604–607. [Google Scholar] [CrossRef]
- Qin, L.; Choy, W.; Leung, K.; Leung, P.C.; Au, S.; Hung, W.; Dambacher, M.; Chan, K. Beneficial effects of regular Tai Chi exercise on musculoskeletal system. J. Bone Miner. Metab. 2005, 23, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Maciaszek, J.; Osiński, W.; Szeklicki, R.; Stemplewski, R. Effect of Tai Chi on body balance: Randomized controlled trial in men with osteopenia or osteoporosis. Am. J. Chin. Med. 2007, 35, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Luo, T.; Xie, H.; Huang, M.; Cheng, A.S. Health benefits of qigong or Tai Chi for cancer patients: A systematic review and meta-analyses. Complement. Ther. Med. 2014, 22, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Deyo, R.; Friedly, J.; Skelly, A.; Hashimoto, R.; Weimer, M.; Fu, R.; Dana, T.; Kraegel, P.; Griffin, J.; et al. Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline Nonpharmacologic Therapies for Low Back Pain. Ann. Intern. Med. 2017. [Google Scholar] [CrossRef]
- Ni, X.; Liu, S.; Lu, F.; Shi, X.; Guo, X. Efficacy and safety of Tai Chi for Parkinson’s disease: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2014, 9, e99377. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Pittler, M.H.; Shin, B.C.; Ernst, E. Tai Chi for osteoporosis: A systematic review. Osteoporos. Int. 2008, 19, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Chen, H.; Berger, M.R.; Zhang, L.; Guo, H.; Huang, Y. Effects of Tai Chi exercise on bone health in perimenopausal and postmenopausal women: A systematic review and meta-analysis. Osteoporos. Int. 2016, 27, 2901–2911. [Google Scholar] [CrossRef] [PubMed]
- Wayne, P.M.; Kiel, D.P.; Krebs, D.E.; Davis, R.B.; Savetsky-German, J.; Connelly, M.; Buring, J.E. The effects of Tai Chi on bone mineral density in postmenopausal women: A systematic review. Arch. Phys. Med. Rehabil. 2007, 88, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Li, S. Effects of Taiji and fast-walking on the bone mineral density and metabolism in older adults. J. Jilin Inst. Phys. Educ. 2011, 27, 87–88. [Google Scholar]
- Shen, C.L.; Williams, J.S.; Chyu, M.C.; Paige, R.L.; Stephens, A.L.; Chauncey, K.B.; Prabhu, F.R.; Ferris, L.T.; Yeh, J.K. Comparison of the effects of Tai Chi and resistance training on bone metabolism in the elderly: A feasibility study. Am. J. Chin. Med. 2007, 35, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.H.; Zhang, Q.H.; Xu, R.M.; Ma, M.; Zhao, X.P.; Shen, G.Q.; Guo, Y.H.; Wang, Y. Effect of Tai-chi exercise on lower limb muscle strength, bone mineral density and balance function of elderly women. Int. J. Clin. Exp. Med. 2014, 7, 1569–1576. [Google Scholar] [PubMed]
- Sufinowicz, M.O.; Sleboda, R.; Nowak, A.L.; Maciaszek, J.A.; Osinski, W.; Stemplewski, R.A.; Szeklicki, R.O.; Salamon, A.R. Effects of Tai Chi on Changes in Concentration of Markers of Bone Turnover in Elderly Men. 2006. Available online: http://wbc1.wbc.poznan.pl/Content/61424/Sufinowicz_REV.pdf (accessed on 4 August 2017).
- Song, R.; Roberts, B.L.; Lee, E.O.; Lam, P.; Bae, S.C. A randomized study of the effects of Tai Chi on muscle strength, bone mineral density, and fear of falling in women with osteoarthritis. J. Altern. Complement. Med. 2010, 16, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Liu, C.; Li, J. Effect of Taichi on bone mineral density in people with hyperlipidemia. Fujian Sports Sci. Technol. 2014, 33, 39–42. [Google Scholar]
- Peppone, L.J.; Mustian, K.M.; Janelsins, M.C.; Palesh, O.G.; Rosier, R.N.; Piazza, K.M.; Purnell, J.Q.; Darling, T.V.; Morrow, G.R. Effects of a structured weight-bearing exercise program on bone metabolism among breast cancer survivors: A feasibility trial. Clin. Breast Cancer 2010, 10, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Zhang, M.; Gou, B.; Lv, Y.; Zhou, X.; Liu, H. Influence of Taiji softball on estrogen and bone metabolism index in perimenopausal women. J. Xi’an Phys. Educ. 2014, 31, 459–463. [Google Scholar]
- Uman, L.S. Systematic reviews and meta-analyses. J. Can. Acad. Child Adolesc. Psychiatry 2011, 20, 57. [Google Scholar] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. (Zagreb) 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2; The Cochrane Collaboration: London, UK, 2009. [Google Scholar]
- Jadad, A.R.; Carroll, D.; Moore, A.; McQuay, H. Developing a database of published reports of randomised clinical trials in pain research. Pain 1996, 66, 239–246. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.; Qin, L.; Lau, M.; Woo, J.; Au, S.; Choy, W.; Lee, K.; Lee, S. A randomized, prospective study of the effects of Tai Chi Chun exercise on bone mineral density in postmenopausal women. Arch. Phys. Med. Rehabil. 2004, 85, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Hui, S.S.; Xie, Y.J.; Woo, J.; Kwok, T.C. Effects of Tai Chi and walking exercises on weight loss, metabolic syndrome parameters, and bone mineral density: A cluster randomized controlled trial. Evid. Based Complement. Altern. Med. 2015. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.L.; Chyu, M.C.; Pence, B.C.; Yeh, J.K.; Zhang, Y.; Felton, C.K.; Doctolero, S.; Wang, J.S. Green tea polyphenols supplementation and Tai Chi exercise for postmenopausal osteopenic women: Safety and quality of life report. BMC Complement. Altern. Med. 2010, 10, 76. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.L.; Chyu, M.C.; Yeh, J.K.; Zhang, Y.; Pence, B.C.; Felton, C.K.; Brismée, J.M.; Arjmandi, B.H.; Doctolero, S.; Wang, J.S. Effect of green tea and Tai Chi on bone health in postmenopausal osteopenic women: A 6-month randomized placebo-controlled trial. Osteoporos. Int. 2012, 23, 1541–1552. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Yu, B.; Chen, W.; Lu, Y.; Yu, D. Simplified Tai Chi resistance training versus traditional Tai Chi in slowing bone loss in postmenopausal women. Evid. Based Complement. Altern. Med. 2015. [Google Scholar] [CrossRef] [PubMed]
- Wayne, P.M.; Kiel, D.P.; Buring, J.E.; Connors, E.M.; Bonato, P.; Yeh, G.Y.; Cohen, C.J.; Mancinelli, C.; Davis, R.B. Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: A pilot pragmatic, randomized trial. BMC Complement. Altern. Med. 2012, 12, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woo, J.; Hong, A.; Lau, E.; Lynn, H. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing 2007, 36, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Mao, H. Effect of Taichi combined with calcium supplements on bone mineral density in postmenopausal women. Chin. J. Rehabil. Med. 2009, 24, 814–816. [Google Scholar]
- Song, H. Effect of Taijiquan exercise on bone density and bone metabolism of primary osteoporosis sufferers. J. Phys. Educ. 2008, 15, 106–108. [Google Scholar]
- Zhou, Y. Effect of sport exercise on prevention lumbar L2-4 osteoporosis on postmenopausal women. Chin. J. Sports Med. 2003, 22, 72–74. [Google Scholar]
- Zhou, Y. Effect of traditional sports on bone density in postmenopausal women. J. Beijing Sport Univ. 2004, 27, 354–360. [Google Scholar]
- Zhou, Y.; Lee, J.; Chen, Z.; Gu, J. Effect of Taichi pushing hand exercise and calcium supplement on bone mineral density in menopausal women. Chin. J. Sports Med. 2005, 24, 106–108. [Google Scholar]
- Wu, G.; Hitt, J. Ground contact characteristics of Tai Chi gait. Gait Posture 2005, 22, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.T.; Chang, J.H.; Huang, C.F. Ground reaction force characteristics of Tai Chi push hand. J. Sports Sci. 2014, 32, 1698–1703. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Osteoporosis Prevention, Diagnosis, and Therapy. 2000. Available online: https://consensus.nih.gov/2000/2000osteoporosis111html.htm (accessed on 4 August 2017).
- Wheater, G.; Elshahaly, M.; Tuck, S.P.; Datta, H.K.; van Laar, J.M. The clinical utility of bone marker measurements in osteoporosis. J. Transl. Med. 2013, 11, 201. [Google Scholar] [CrossRef] [PubMed]
- Woitge, H.W.; Oberwittler, H.; Heichel, S.; Grauer, A.; Ziegler, R.; Seibel, M.J. Short-and long-term effects of ibandronate treatment on bone turnover in Paget disease of bone. Clin. Chem. 2000, 46, 684–690. [Google Scholar] [PubMed]
- Woitge, H.W.; Scheidt-Nave, C.; Kissling, C.; Leidig-Bruckner, G.; Meyer, K.; Grauer, A.; Scharla, S.H.; Ziegler, R.; Seibel, M.J. Seasonal Variation of Biochemical Indexes of Bone Turnover: Results of a Population-Based Study. J. Clin. Endocrinol. Metab. 1998, 83, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Lelard, T.; Doutrellot, P.L.; David, P.; Ahmaidi, S. Effects of a 12-week Tai Chi Chuan program versus a balance training program on postural control and walking ability in older people. Arch. Phys. Med. Rehabil. 2010, 91, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Wang, C.; Tian, Z.; Wang, H.; Shu, Y. Effect of Yang-Style Tai Chi on Gait Parameters and Musculoskeletal Flexibility in Healthy Chinese Older Women. Sports 2017, 5. [Google Scholar] [CrossRef]
- Yeh, G.Y.; Wood, M.J.; Lorell, B.H.; Stevenson, L.W.; Eisenberg, D.M.; Wayne, P.M.; Goldberger, A.L.; Davis, R.B. Effects of Tai Chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: A randomized controlled trial. Am. J. Med. 2004, 117, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.C.; Wang, W.H.; Chan, P.; Lin, L.J.; Wang, C.H.; Tomlinson, B.; Hsieh, M.H.; Yang, H.Y.; Liu, J.C. The beneficial effects of Tai Chi Chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J. Altern. Complement. Med. 2003, 9, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.J.; Garber, C.E.; Jun, T.W.; Jin, Y.S.; Chung, S.J.; Kang, H.J. Therapeutic effects of Tai Chi in patients with Parkinson’s disease. ISRN Neurol. 2013. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, E.F. Cellular mechanisms of bone remodeling. Rev. Endocr. Metab. Disord. 2010, 11, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Jou, T.H. The Tao of TCC Chuan: Way to Rejuvenation. Available online: https://www.amazon.com/Dao-Taijiquan-Way-Rejuvenation-Tai/dp/0804813574 (accessed on 4 August 2017).
- Wang, H.R.; Wei, A.K.; Lu, Y.Z.; Yu, B.; Chen, W.H.; Lu, Y.; Liu, Y.; Yu, D.H.; Zou, L.Y. Simplified Tai Chi Program Training versus Traditional Tai Chi on the Functional Movement Screening in Older Adults. Evid. Based Complement. Altern. Med. 2016. [Google Scholar] [CrossRef] [PubMed]


| Author [Reference] | Study Design | Study Location (Language) | Study Participants | Sample Size (Participants/Analyzed) and Intervention | Outcomes Measured | Study Results |
|---|---|---|---|---|---|---|
| Chen et al. [20] | RCT | Shanghai, China (Chinese) | 40 female and older adults, aged 55 to 65 | TC (20/20): 55 to 65 min, 3 to 4 times weekly for 20 weeks (Yang-style) CG: sedentary lifestyle | Calcaneus ultrasound BMD (BQI, BUA, and SOS) Biomarkers (ALP) | Mean change (Sig) for TC vs. CG: BQI (−3.53 vs. −8.32), SOS (−14.11 vs. −15.57), and BUA (−1.58 vs. −9.21). Mean change (Sig) for TC vs. CG:ALP (−13 vs. −12.69) |
| Chan et al. [35] | RCT | Hongkong, China (English) | 132 postmenopausal women (54.0 ± 3.5 years) | TC (67/54): five 50-min sessions weekly for 12 months (Yang style) CG (65/54): sedentary lifestyle | BMD (Lumbar spine – L2-4, proximal femur [neck and trochanter], and ultral distal tibia [tBMD, iBMD, CTD]) | TC vs. CG (NS): lumbar spine (0.10 vs. −0.89%), proximal femur neck (−0.94 vs. −1.80%), proximal femur trochanter (−1.19 vs. −0.56%), tBMD (−0.53 vs. −1.46), iBMD (−0.61 vs. −1.58), and CTD (−0.39 vs. −1.40). |
| Du et al. [27] | RCT | Shanxi, China (Chinese) | 30 perimenopausal women, aged 45 to 55 | TCSB (15/15): 90 min, 4 to 5 times weekly for 24 weeks. CG: original lifestyle | BMD (Total body, lumbar spine [L1-4], and trunk) Biomarker (ALP) | Mean BMD change (Sig) for TC vs. CG: lumbar spine (0.03 vs. −0.003), total body (0.01 vs. −0.02), and trunk (0 vs. −0.05) Mean change for TC vs. CG: ALP (−1.1 vs. 0.2) |
| Hui et al. [36] | RCT | Hongkong, China (English) | 253 middle-aged participants (45.8 ± 5.3 years) | TC (129/129): five 45-min sessions weekly for 12 weeks (Yang-style) CT (124/124): original lifestyle | BMC (total body) | Mean BMD change (NS) for TC and CG: total body (−0.39 vs. −0.33) |
| Mao [42] | RCT | Shangxi, China (Chinese) | 80 postmenopausal women (56.78 ± 2.91 years) | TC (20/20) and TCS (20/20): 45 to 50 min, 7 times weekly for 20 weeks. CS (20/20): standard care (calcium supplement) CG (20/20): original lifestyle | BMD (Lumbar spine [L2-4]) | TC vs. CG and TCCS vs. CS (Sig): Lumbar spine (1.361 vs. −0.874) and (2.036 vs. 0.378), respectively. |
| Peppone et al. [26] | RCT | USA (English) | 16 breast cancer survivors, median age of 53 years | TC (7/7): three 60-min sessions weekly for 12 weeks (Yang-style) CG (9/9): standard care | Biomarkers (NTx, BAP, and BRI) | BAP (NS): TC (8.3 to 10.2; 22.4%) vs. ST (7.6 to 8.1; 6.3%). NTx (Sig): TC (17.6 to 11.1; −36.6%) vs. ST (20.8 to 18.8; –9.6%) BRI (Sig, p = 0.05): TC (1.6) vs. ST (0.23) |
| Shen et al. [21] | RCT | Texas, USA (English) | 28 sedentary, older adults. TC (78.8 ± 1.3) RT (79.4 ± 2.2) | TC (14/14) three 40-min sessions weekly for 24 weeks (Yang-style) RT (14/14): three 40-min sessions weekly for 24 weeks (bench press, leg press, leg curl, leg extension, and seated row on a resistance exercise machine, as well as shoulder press and arm curl) | Biomarkers (BAP, PYD, PTH, and BAP/PYD ratio), but mean score and standard deviation were not reported. | After 6 weeks, both TC and RT exhibited higher level of serum BAP, as compared to the baseline and the TC group exhibited a greater increase in serum BAP than the RT group. BAP/PYD ratio was higher than baseline only in the TC group, and the increase of the ratio in the TC was greater than that in the RT group. |
| Shen et al [37] | RCT | Texas, USA (English) | 171 postmenopausal women TC + placebo (58.3 ± 7.7); TC + GTP (57.6 ± 6.7); GTP (56.5 ± 5.5); Placebo (57.6 ± 7.5) | Placebo + TC (42/37): medicinal starch 500 mg daily and 24-move simplified Yang-style TC training (three 60-min sessions weekly for 24 weeks. TC + GPT (38/37): same as TC group + GTP 500 mg daily. GPT (47/39): GTP 500 mg daily Placebo (44/37): same as medicinal starch 500 mg daily. | Biomarker (ALP). | No significant change in the ALP was observed |
| Shen et al. [38] | RCT | Texas, USA (English) | Same as Shen et al. [37] | Same as Shen et al. [37] Yang-style | Biomarkers (BAP and TRAP) | A significant main effect of TC on serum BAP at 3 months (p = 0.04). No significant main effect of TC on TRAP was found. |
| Song [43] | RCT | Jiangsu, China (Chinese) | 40 people with osteoporosis. TC (62.67 ± 11.23) CG (63.81 ± 13.07) | TC (20/20): six 60-min sessions weekly (yang-style, but not report the length of intervention) + standard care CG (20/20): standard care | BMD (lumbar spine [L2-4] and femoral neck) Biomarkers (BGP and ALP) | Mean change (Sig) for TC and CG: lumbar spine (0.205 vs. 0.003) and femoral neck (0.228 vs. 0.005). Mean change (Sig) for TC and CG: and BGP (−2.04 vs. −0.61) and ALP (−17.31 vs. −11.58) |
| Song et al. [24] | RCT | South Korea (English) | 82 women with osteoarthritis TC (mean age = 63 years) CG (mean age = 61 years) | TC (41/30): 60 to 65 min, 7 times weekly for six months (Sun style) CG (41/35): 60-min self-help education session, once monthly for six months | BMD (DXA): Femoral neck and trochanter. | Mean change (Sig) for TC vs. CG: Femur neck (0.09 vs. −0.10), (0.04 vs. −0.04), and trochanter (0.07 vs. −0.05). |
| Song et al. [22] | RCT | Henan, China (English) | 105 community living elderly women, aged 55 to 65. | TC (35/31): Chen Style CG1 (35/33): Dance CG2 (35/30): Walking six 40-min sessions weekly for 12 months in three selected groups | BMD (BQI) | Mean Change (Sig) for TC vs. CG1 vs. CG2: BQI (10.51 vs. 7.65 vs. 7.69) |
| Sufinowicz et al. [23] | RCT | Poland (English) | 90 men aged over 60 (68.83 ± 5.84 years) | TC (35/35): 45-min, twice per week for four months CG (55/55): original lifestyle | Biomarkers (OSC and CTX) | Mean change (Sig) for TC vs. CG: CTX (−0.31 vs. −0.065) and OSC (−0.949 vs. −0.751) |
| Wang et al. [39] | RCT | Shanghai, China (English) | 119 postmenopausal women, aged 52 to 65 | TC (40/34): four 60-min sessions weekly for 12 months TCRT (40/37): four 60-min sessions weekly for 12 months CG (39/35): original lifestyle | BMD (lumbar spine [L2-4] and femoral neck) | Mean change (Sig) for TCRT vs. TC vs. CG: Lumbar spine (0.0182 vs. 0.0105 vs. −0.0038), femur neck (0.0004 vs. 0.0045 vs. −0.03), and (−0.0047 vs. −0.0171 vs. −0.0397) |
| Wayne et al. [40] | RCT | Boston, MA, USA (English) | 86 post-menopausal osteopenic women, aged 45 to 70 | TC (43/42): 99.5 h during 9-month intervention plus standard care. Of the TC group, 26 completed 75% training requirements or above as TCAG CG (43/42): standard care (daily calcium, vitamin D, and regular exercise) | BMD (femoral neck, total hip, and lumbar spine [L1-4]). Biomarkers (CTX and OSC) | Femoral neck BMD: Significant positive change (+0.04%) was only observed in TCAG compared to the baseline, whereas CG group experienced a loss (−0.98%) (p = 0.05) Biomarker: significant positive change (−5.1%) in OSC was only observed in TCAG group (p = 0.03) compared to the baseline. |
| Woo et al. [41] | RCT | Hongkong, China (English) | 120 community-living elderly people, aged 65 to 74 | TC (60/58): Three sessions weekly for 12 months CG (60/59): original lifestyle | BMD (the total hip and spine [L1-4]) | For female participants, TC vs. CG: total hip (Sig) (0.07 vs. −2.25%), spine (NS) (0.10 vs. 0.98%) For female participants, TC vs. CG: total hip (NS) (−0.48 vs. −0.15%), and spine (1.35 vs. 0.54%) |
| Zhou [44] | RCT | Shangxi, China (Chinese) | 48 postmenopausal women (55.94 ± 2.83 years) | TCPH (12/12), Fan dancing (12/12), and walking (12/12): 45 to 60 min, 5 to 7 times weekly for 10 months. CG (12/12): original lifestyle | BMD (Lumbar spine [L2-4] | Lumbar spine (Sig) for TC vs. CG: (3.4 vs. −1.83%) and for TCPH vs. CG (1.84 vs. −1.83%) |
| Zhou [45] | RCT | Shanxi, China (Chinese) | 60 postmenopausal women, aged 55.9 | TC (12/12), TCPH (12/12), rope jumping (12/12), Mulan boxing (12/12): Five-to-seven sessions (45 to 60 min) for 10 months (Yang Style). CG (12/12): original lifestyle | BMD (Lumbar spine [L2-4], distal radius and ulna of wrist) | Mean change (Sig) for TCPH vs. CG: lumbar spine (0.035 vs. −0.019), distal radius (0.031 vs. −0.017), and distal ulna (0.033 vs. −0.016). Mean change (Sig) for TC vs. CG: lumbar spine (0.019 vs. −0.019), distal radius (0.017 vs. −0.017), and distal ulna (0.016 vs. −0.016) |
| Zhou et al. [46] | RCT | Shan Xi, China, (Chinese) | 64 postmenopausal women, with a mean age of 57.21 ± 3.41 | TCPH (16/16): 45 to 60 min, 5 to 7 times weekly for 6 months. CS (16/16): calcium carbonate 750 mg + calcium, 300 mg + Vitamin D, 100 IU, 1 tablet, 2 times daily for 6 months. TCPH + CSG: same as above CG: original lifestyle | BMD (Lumbar spine [L2-4] | TCPH + CSG vs. CSG: lumbar spine (Sig) (2.037 vs. 0.378%) TCPH vs. CG: lumbar spine (NS) (1.361 vs. −0.874%) |
| Zhou et al. [25] | RCT | Guizhou, China (Chinese) | 40 older adults with hyperlipidemia (60 ± 5.6 years) | TC (20/20): four 90-min sessions for 6 months. CG (20/20): original lifestyle | BMD (Distal radius, Lumbar spine [L2-4] and trochanter) Biomarker (BGP) | Mean change (Sig) for TC vs. CG: distal radius (0.08 vs. −0.04), lumbar spine (0.05 vs. −0.05), trochanter (0.22 vs. −0.01) Biomarker: mean change (Sig) for TC (5.44) vs. CG (−0.11) |
| Author | RE | RM | EC | OAB | WDR | SSE | ADA | TCID | QTCI | Study Quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Chen et al. [20] | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Fair |
| Chan et al. [35] | Yes | No | Yes | No | Yes | Yes | Yes | Yes | No | Fair |
| Du et al. [27] | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Fair |
| Hui et al. [36] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Good |
| Mao [42] | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Fair |
| Peppone et al. [26] | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Good |
| Shen et al. [21] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Good |
| Shen et al. [37] | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Good |
| Shen et al. [38] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Good |
| Song et al. [43] | Yes | No | Yes | No | Yes | No | No | No | Yes | Fair |
| Song et al [24] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Good |
| Song et al. [22] | Yes | No | Yes | No | Yes | No | No | Yes | No | Fair |
| Sufinowicz et al. [23] | Yes | No | No | No | Yes | No | No | Yes | No | Poor |
| Wang et al. [39] | Yes | No | Yes | No | Yes | No | Yes | Yes | Yes | Fair |
| Wayne et al. [40] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Good |
| Woo et al. [41] | Yes | Yes | Yes | No | Yes | Yes | Yes | No | No | Fair |
| Zhou [44] | Yes | No | Yes | No | Yes | No | No | Yes | No | Fair |
| Zhou [45] | Yes | No | Yes | No | Yes | No | No | Yes | No | Fair |
| Zhou et al [46] | Yes | No | Yes | No | Yes | No | No | Yes | No | Fair |
| Zhou et al. [25] | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Fair |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zou, L.; Wang, C.; Chen, K.; Shu, Y.; Chen, X.; Luo, L.; Zhao, X. The Effect of Taichi Practice on Attenuating Bone Mineral Density Loss: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2017, 14, 1000. https://doi.org/10.3390/ijerph14091000
Zou L, Wang C, Chen K, Shu Y, Chen X, Luo L, Zhao X. The Effect of Taichi Practice on Attenuating Bone Mineral Density Loss: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health. 2017; 14(9):1000. https://doi.org/10.3390/ijerph14091000
Chicago/Turabian StyleZou, Liye, Chaoyi Wang, Kevin Chen, Yankai Shu, Xiaoan Chen, Lin Luo, and Xitang Zhao. 2017. "The Effect of Taichi Practice on Attenuating Bone Mineral Density Loss: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" International Journal of Environmental Research and Public Health 14, no. 9: 1000. https://doi.org/10.3390/ijerph14091000





