Forecasting the Incidence of Mumps in Zibo City Based on a SARIMA Model
Abstract
:1. Introduction
2. Materials and Methods
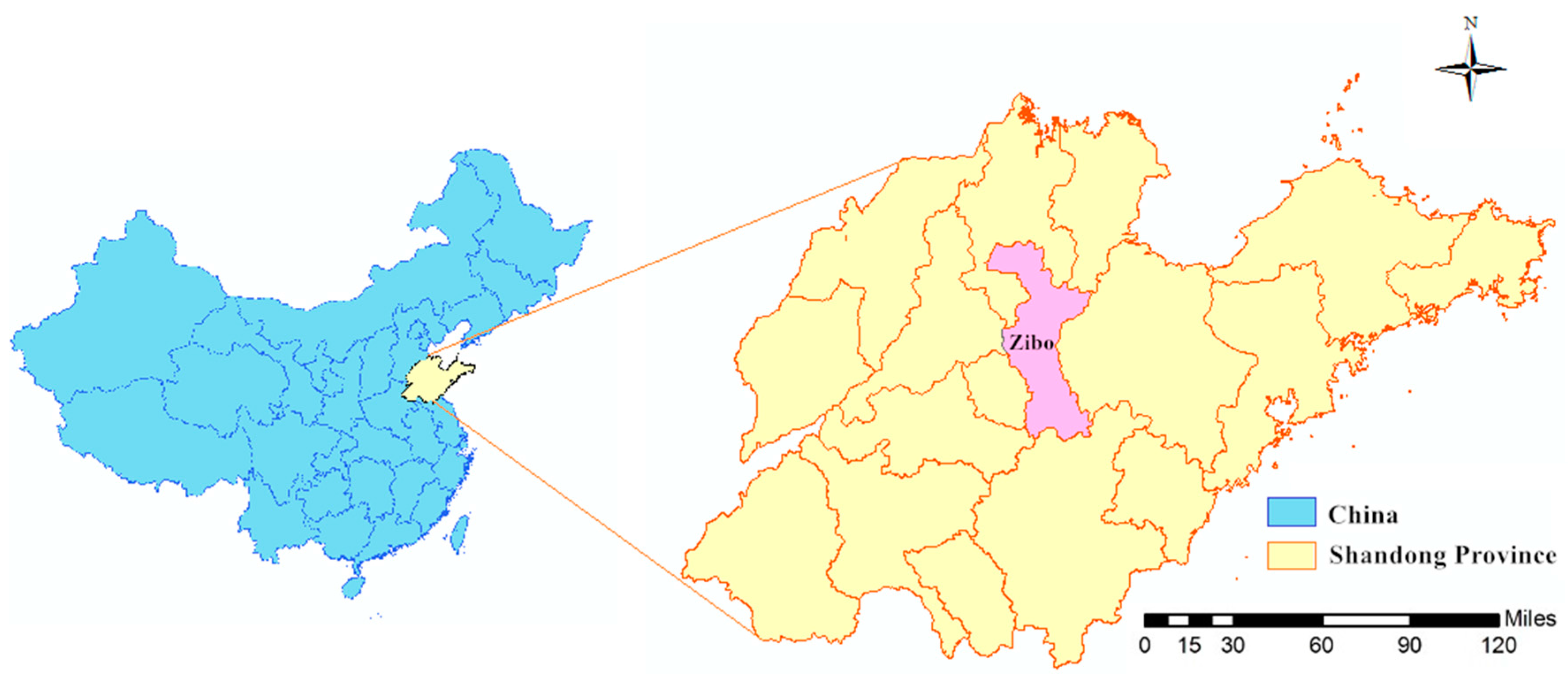
2.1. Study Area and Data Collection
2.2. Statistical Analysis
3. Results
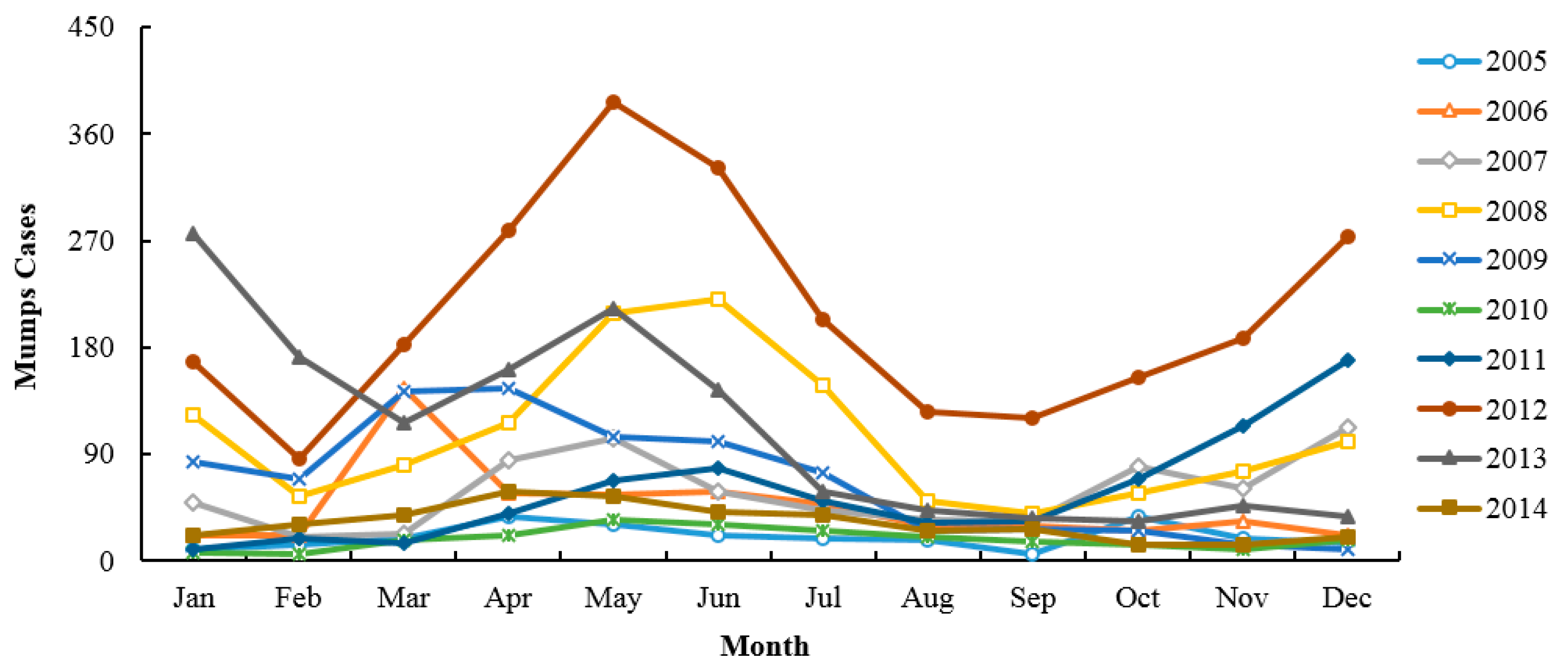
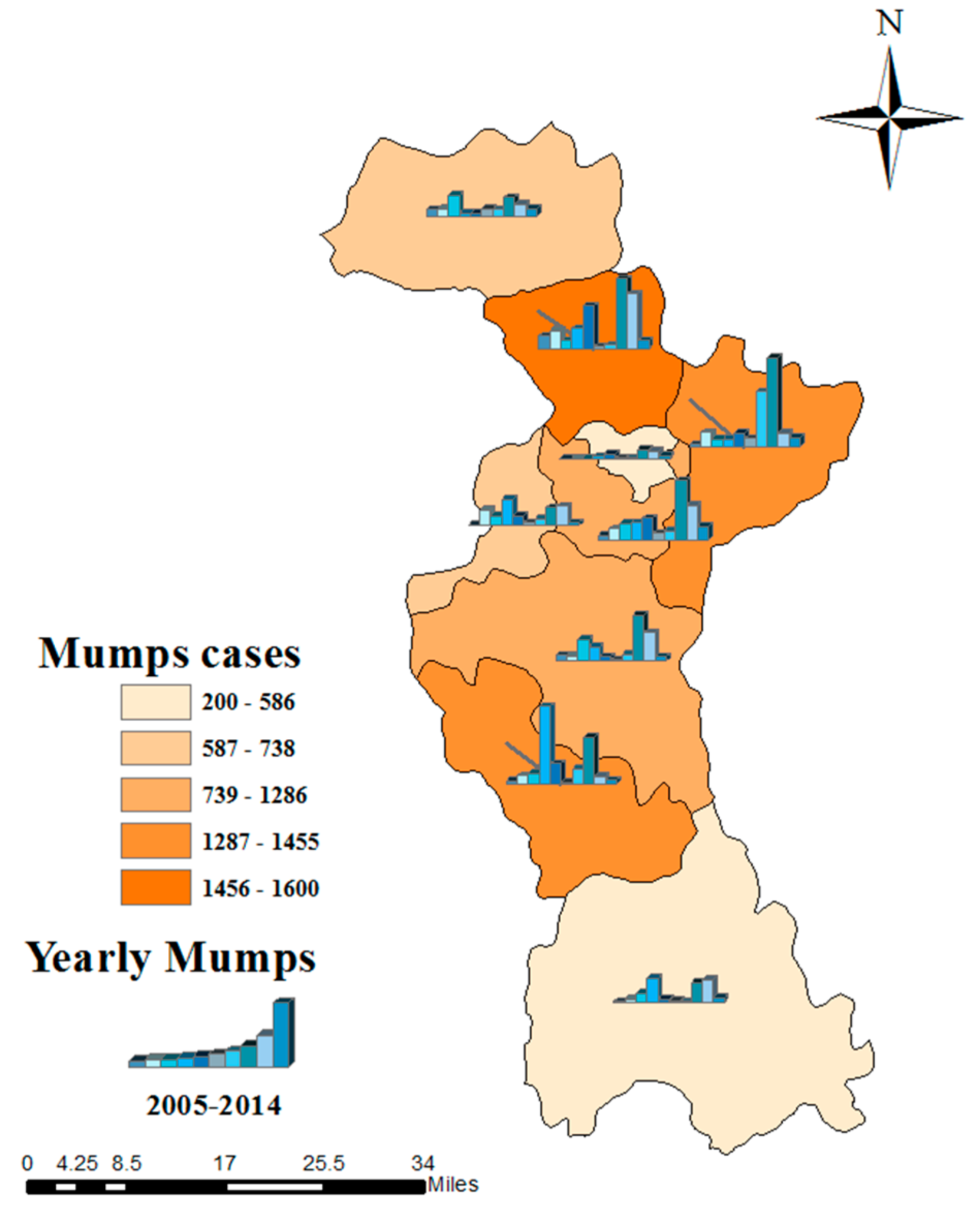
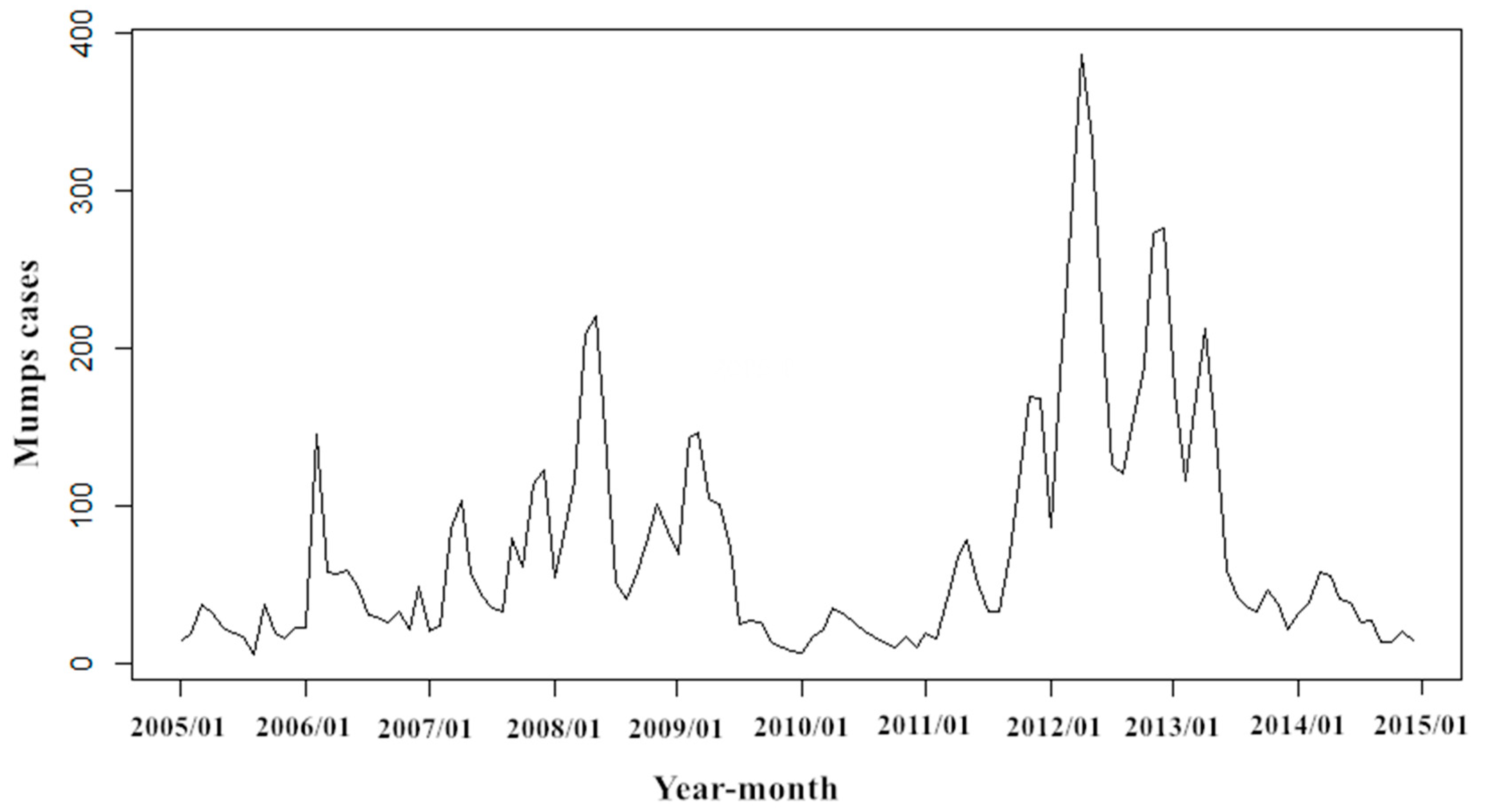
3.1. Descriptive Analyses
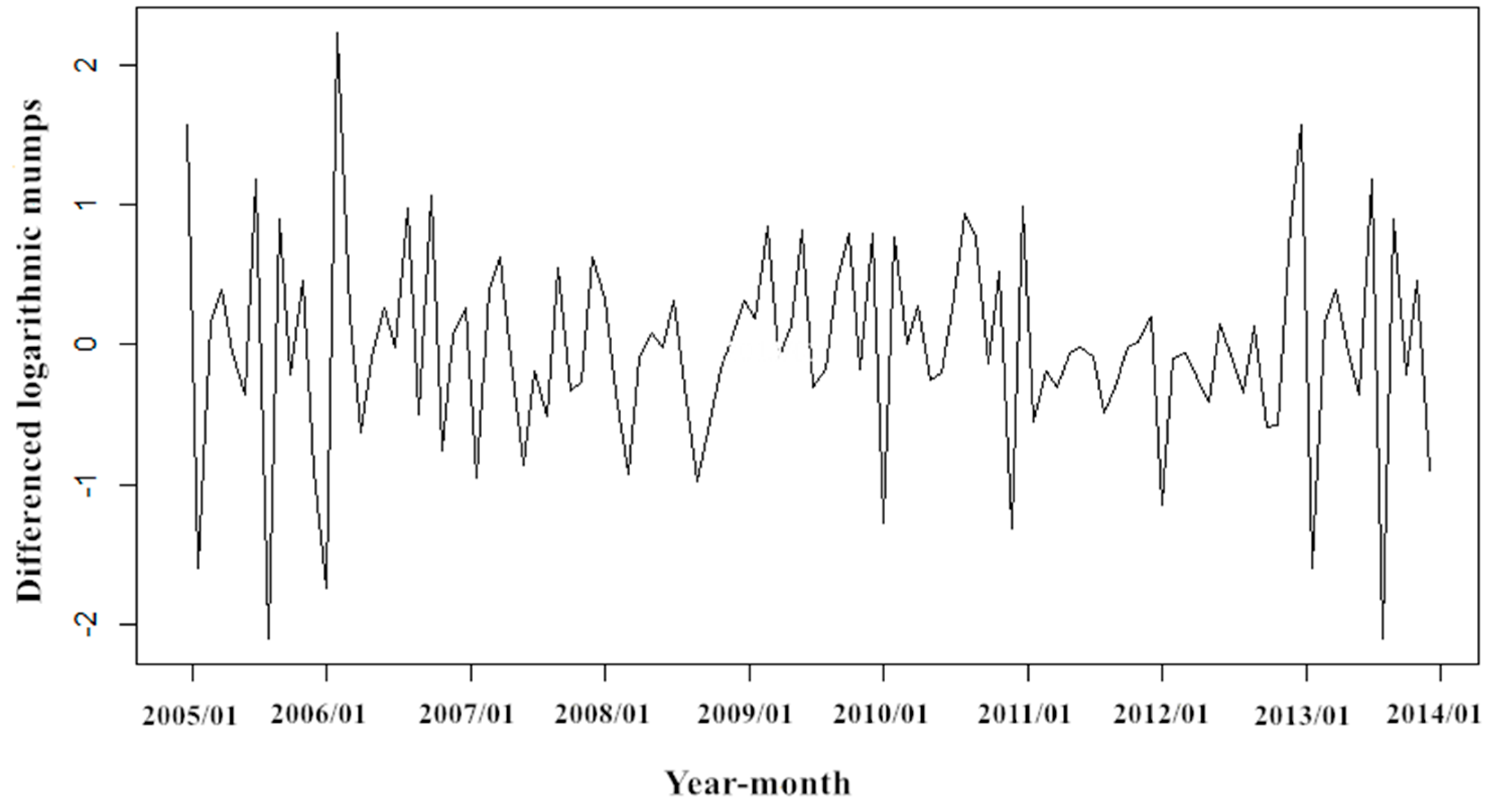
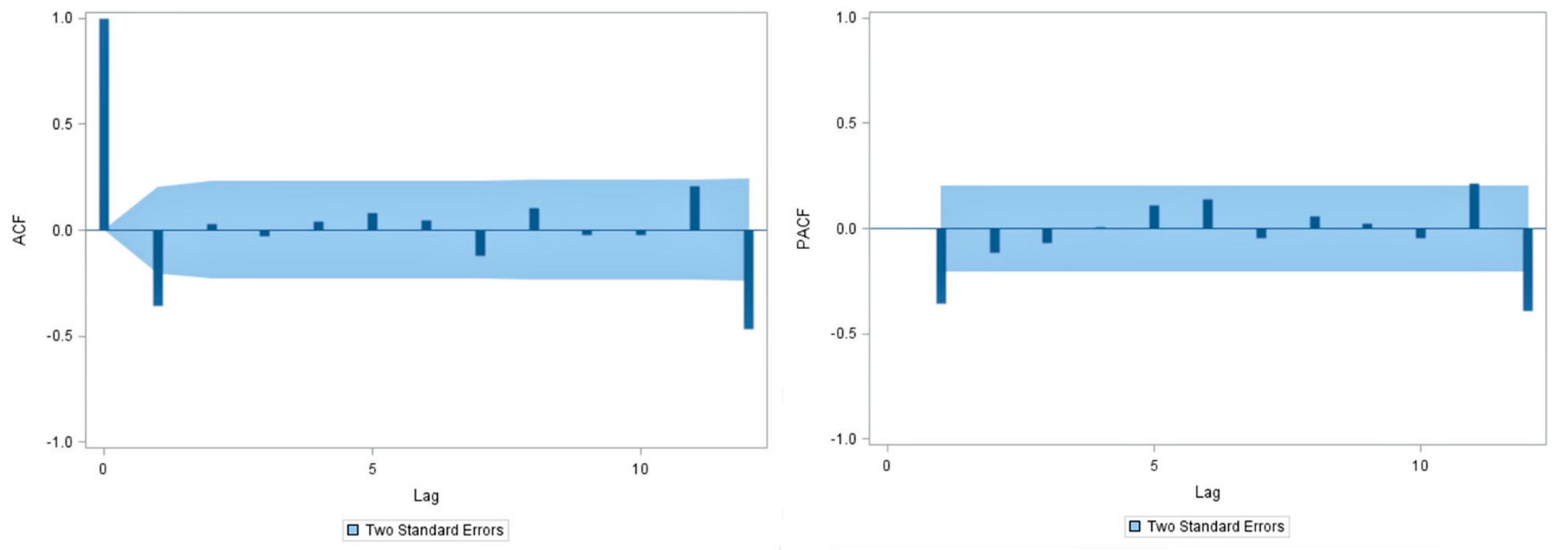
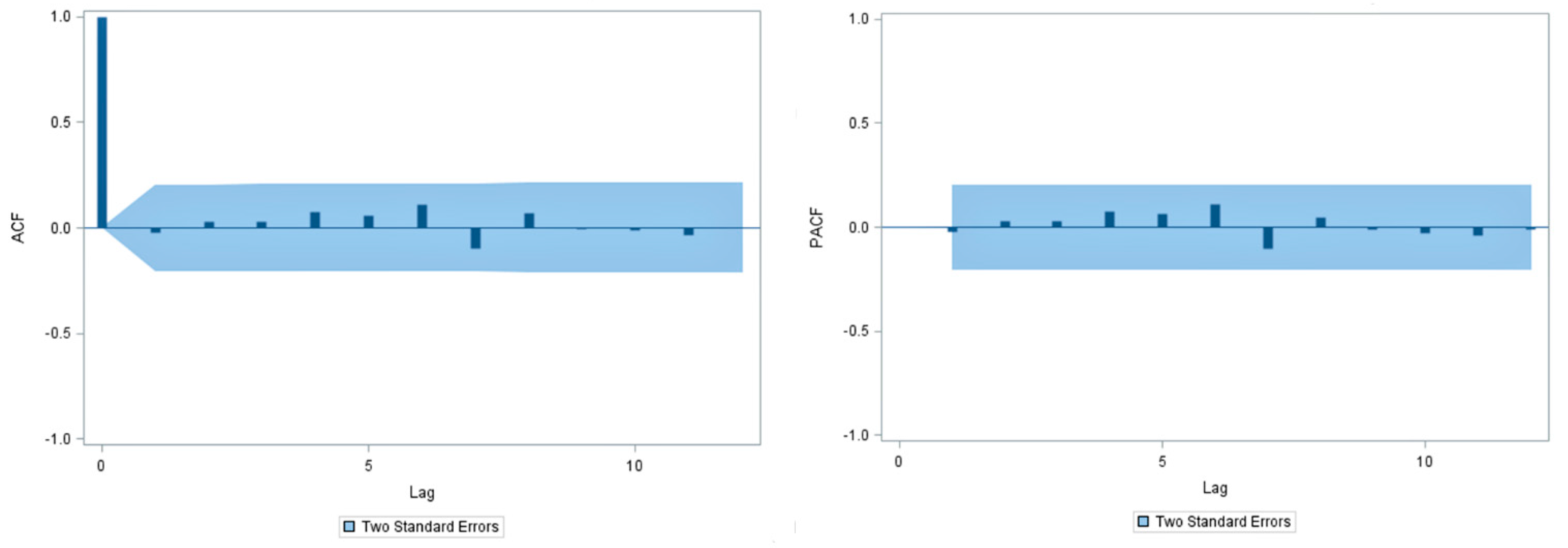
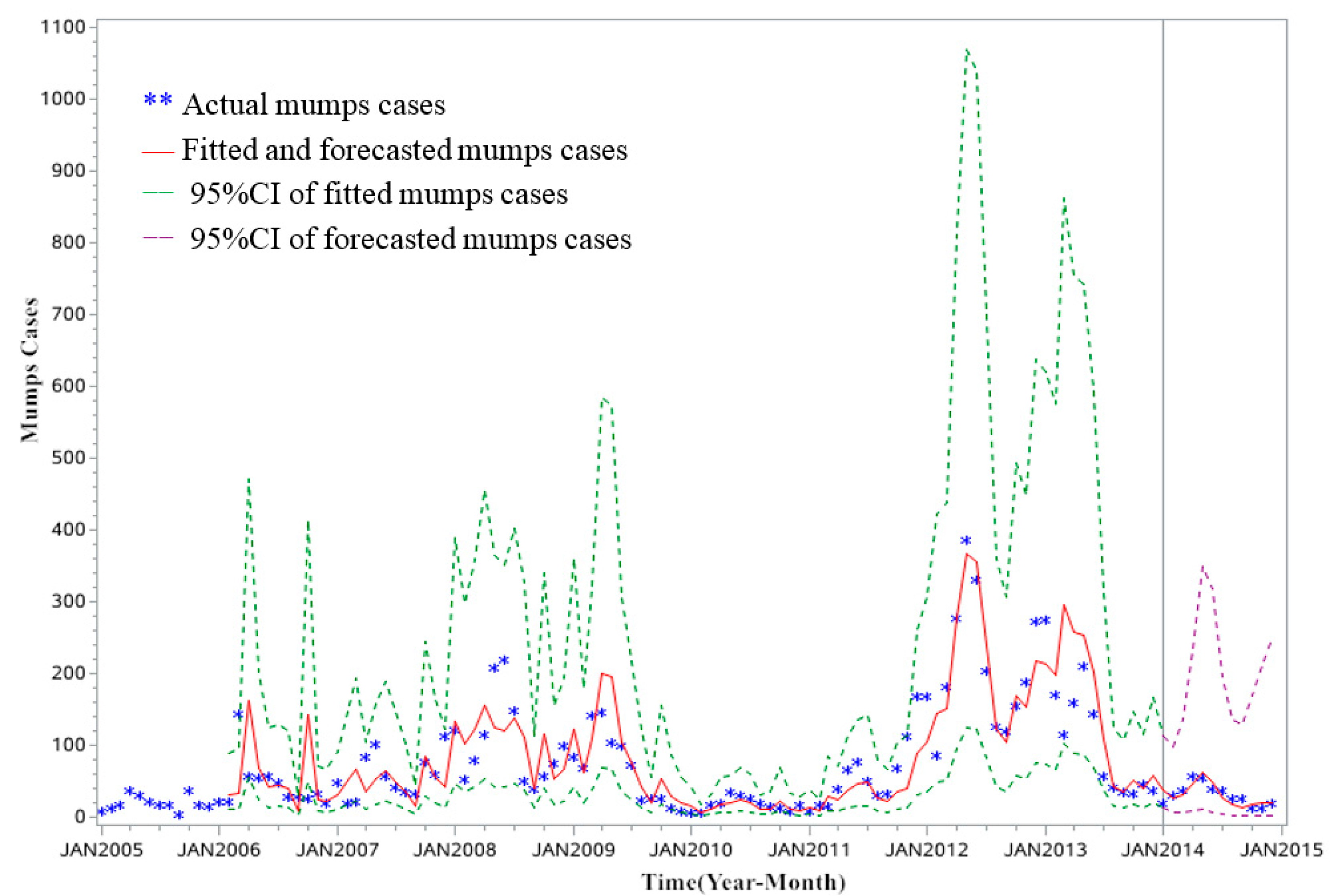
3.2. SARIMA Model
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Anders, H.; Steven, R.; Kathrin, M. Mumps. Lancet 2008, 371, 32–44. [Google Scholar]
- Martina, H.; Radomíra, L.; Dita, S.; Kristýna, H.; Helena, J.; Ludmila, N.; Pavla, L.; Jan, K.; Simona, A.; Vilma, M. Mumps in the Czech Republic in 2013: Clinical characteristics, mumps virus genotyping, and epidemiological links. Cent. Eur. J. Public Health 2016, 24, 22–28. [Google Scholar]
- Hana, O.; Marek, M.; Pavla, L.; Helena, Š.; Radomíra, L.; Lucie, J.; Jan, K. Protective effect of vaccination against mumps complications, Czech Republic, 2007–2012. BMC Public Health 2016, 16, 293. [Google Scholar] [CrossRef]
- Xu, Q.; Xu, A.; Song, L.; Zhang, L.; Xiao, Z.; Li, R.; Liu, Y.; Wang, C.; Li, M. Epidemiological survey on clinical diagnosed mumps from 2001 to 2003 in Shandong. Chin. J. Vaccines Immun. 2006, 6, 497–499. [Google Scholar]
- Fei, F.; Feng, L.; Xu, Z.; Feng, Z. Epidemiology of mumps in China, 2008–2010. Dis. Surveill. 2011, 26, 691–693. [Google Scholar]
- Galazka, A.M.; Robertson, S.E.; Kraigher, A. Mumps and mumps vaccine: A global review. Bull. World Health Organ. 1999, 77, 3–14. [Google Scholar] [PubMed]
- Cui, A.; Zhu, Z.; Hu, Y.; Deng, X.; Sun, Z.; Zhang, Y.; Mao, N.; Xu, S.; Fang, X.; Gao, H.; et al. Mumps epidemiology and mumps virus genotypes circulating in Mainland China during 2013–2015. PLoS ONE 2017, 12, e0169561. [Google Scholar] [CrossRef] [PubMed]
- Monika, R.K.; Justyna, R. Mumps in Poland in 2014. Epidemiol. Chron. 2016, 70, 183–187. [Google Scholar]
- Park, S.H. Resurgence of mumps in Korea. Infect. Chemother. 2015, 47, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gustavo, D.; Patricia, Q.; Amy, P.; Albert, E.B.; Meghan, L.H.; Jennifer, S.; Kae, H.; Carol, F.; Dennis, L.; Anne, O.; et al. Recent resurgence of mumps in the United States. N. Engl. J. Med. 2008, 358, 1580–1589. [Google Scholar]
- Sabbe, M.; Vandermeulen, C. The resurgence of mumps and pertussis. Hum. Vaccines Immunother. 2016, 12, 955–959. [Google Scholar] [CrossRef] [PubMed]
- Bi, X. Study on Eco-Geographical Regionalization of Major Infections Diseases in Shandong Province; Shandong University: Jinan, China, 2009. [Google Scholar]
- Yin, A.; Cao, J.; Wang, K.; Xu, J.; Yuan, Q.; Lei, J. Analysis on epidemic characteristics of mumps, Shandong Province. Prev. Med. Trib. 2013, 19, 943–945. [Google Scholar] [CrossRef]
- Wu, J.; Ye, L.; You, E. Prediction of incidence of notifiable contagious diseases by appalication of time series model. J. Math. Med. 2007, 20, 90–93. [Google Scholar]
- Martinez, E.Z.; Silva, E.A.S.; Da Fabbro, A.L.D. A SARIMA forecasting model to predict the number of cases of dengue in Campinas, State of São Paulo, Brazil. Rev. Soc. Bras. Med. Trop. 2011, 44, 436–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahmood, M.; Mahshid, N.; Abbas, B.; Narges, K.; Saeed, S.; Shanaz, A. Forecasting tuberculosis incidence in Iran using Box-Jenkins Models. Iran. Red Crescent Med. J. 2014, 16, e11779. [Google Scholar] [CrossRef]
- Cao, S.; Wang, F.; Wilson, T.; Lap, A.T.; Jean, H.K.; Liu, J.; Lu, Z. A hybrid seasonal prediction model for tuberculosis incidence in China. BMC Med. Inform. Decis. Mak. 2013, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Varun, K.; Abha, M.; Sanjeet, P.; Geeta, Y.; Richa, T.; Deepak, R.; Saudan, S. Forecasting malaria cases using climatic factors in delhi, India: a time series analysis. Malar. Res. Treat. 2014, 482851. [Google Scholar] [CrossRef]
- Yang, L.; Liang, S.; Wang, X.; Li, X.; Wu, Y.; Ma, W. Burden of disease measured by disability-adjusted life years and a disease Forecasting Time Series Model of Scrub Typhus in Laiwu, China. PLoS Negl. Trop. Dis. 2015, 9, e3420. [Google Scholar] [CrossRef] [PubMed]
- Shahrokh, Y.C.; Fatemeh, R.T.; Reza, M.; Alireza, R. A time series model for assessing the trend and forecasting the road traffic accident mortality. Arch. Trauma Res. 2016, 5, e36570. [Google Scholar] [CrossRef]
- Lin, Y.; Chen, M.; Chen, G.; Wu, X.; Lin, T. Application of an autoregressive integrated moving average model for predicting injury mortality in Xiamen, China. BMJ Open 2015, 5, e008491. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Bao, C.; Zhao, Y.; Yi, H.; Tang, S.; Yu, H.; Chen, F. ARIMA product season model and its application on forecasting in incidence of infectious disease. Appl. Stat. Manag. 2008, 27, 362–368. [Google Scholar]
- Zhang, X.; Pang, Y.; Cui, M.; Lorann, S.; Xiang, H. Forecasting mortality of road traffic injuries in China using seasonal autoregressive integrated moving average model. Ann. Epidemiol. 2015, 25, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Su, Q.; Liu, J.; Ma, C.; Fan, C.; Wen, N.; Luo, H.; Wang, H.; Li, L.; Hao, L. Epidemic profile of mumps in China during 2004–2013. Chin. J. Prev. Med. 2016, 50, 611–614. [Google Scholar]
- Han, Z.; Huang, Z. Analysis on epidemiological characteristics of mumps, Zibo City, 2007–2013. Prev. Med. Trib. 2014, 20, 622–625. [Google Scholar]
- Zhang, B.; Li, D.; Teng, H.; Xu, A. Analysis on Epidemiological Characteristics of mumps, Zhangdian District, Zibo City, 2008–2013. Prev. Med. Trib. 2014, 20, 677–681. [Google Scholar]
- Li, R.; Zhang, T.; Liang, Y.; Luo, C.; Jiang, Z.; Xue, F.; Liu, Y.; Liu, J.; Li, X. Application of SARIMA model in predicting of the incidence of mumps. J. Shandong Univ. (Health Sci.) 2015, 54, 82–86. [Google Scholar]
- Valipour, M. Long-term runoff study using SARIMA and ARIMA models in the United States. Meteorol. Appl. 2015, 22, 592–598. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, Y.; Yang, M.; Zhang, T.; Young, A.; Li, X. Comparative study of four time series methods in forecasting typhoid fever incidence in China. PLoS ONE 2013, 8, e63116. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Tian, F. Application of time series analysis in the prediction of Hypertension incidence. Chin. J. Gerontol. 2010, 30, 1777–1780. [Google Scholar]
- Bas, M.; del, C.; Ortiz, J.; Ballesteros, L.; Martorell, S. Evaluation of a multiple linear regression model and SARIMA model in forecasting 7 Be air concentrations. Chemosphere 2017, 177, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Kam, H.J.; Sung, J.O.; Park, R.W. Prediction of daily patient numbers for a regional emergency medical center using time series analysis. Healthc. Inform. Res. 2010, 16, 158–165. [Google Scholar] [CrossRef] [PubMed]
| Models | Parameter Estimation | t-test (Parameters Equalization Values With Zero) | Goodness of Fits for Models | Correlation Coefficient | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | Standard Error | Lag | t | p | AIC | SBC | MAPE | r | p | |
| SARIMA (0, 1, 1) (0, 1, 1)12 | 157.528 | 165.190 | 0.297 | 0.833 | <0.001 | |||||
| MA | 0.369 | 0.098 | 1 | 3.760 | <0.001 | |||||
| SMA | 0.635 | 0.085 | 12 | 7.440 | <0.001 | |||||
| SARIMA (1, 1, 0) (0, 1, 1)12 | 158.413 | 166.074 | 0.293 | 0.831 | <0.001 | |||||
| AR | −0.350 | 0.098 | 1 | −3.550 | 0.001 | |||||
| SMA | 0.626 | 0.086 | 12 | 7.310 | <0.001 | |||||
| SARIMA (1, 1, 0) (1, 1, 0)12 | 170.668 | 178.329 | 0.429 | 0.813 | <0.001 | |||||
| AR | −0.265 | 0.101 | 1 | −2.620 | 0.010 | |||||
| SAR | −0.439 | 0.097 | 12 | −4.530 | <0.001 | |||||
| SARIMA (0, 1, 1) (1, 1, 0)12 | 170.240 | 177.901 | 0.405 | 0.814 | <0.001 | |||||
| MA | 0.280 | 0.101 | 1 | 2.770 | 0.007 | |||||
| SAR | −0.434 | 0.097 | 12 | −4.460 | <0.001 | |||||
| Time (Month) | January | February | March | April | May | June | July | August | September | October | November | December |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Actual Cases | 21 | 31 | 38 | 58 | 55 | 41 | 38 | 26 | 27 | 13 | 13 | 20 |
| Forecasted Cases | 38.63 | 27.54 | 32.19 | 47.82 | 62.45 | 49.93 | 27.41 | 16.89 | 14.42 | 17.00 | 19.34 | 20.87 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, Q.; Li, R.; Liu, Y.; Luo, C.; Xu, A.; Xue, F.; Xu, Q.; Li, X. Forecasting the Incidence of Mumps in Zibo City Based on a SARIMA Model. Int. J. Environ. Res. Public Health 2017, 14, 925. https://doi.org/10.3390/ijerph14080925
Xu Q, Li R, Liu Y, Luo C, Xu A, Xue F, Xu Q, Li X. Forecasting the Incidence of Mumps in Zibo City Based on a SARIMA Model. International Journal of Environmental Research and Public Health. 2017; 14(8):925. https://doi.org/10.3390/ijerph14080925
Chicago/Turabian StyleXu, Qinqin, Runzi Li, Yafei Liu, Cheng Luo, Aiqiang Xu, Fuzhong Xue, Qing Xu, and Xiujun Li. 2017. "Forecasting the Incidence of Mumps in Zibo City Based on a SARIMA Model" International Journal of Environmental Research and Public Health 14, no. 8: 925. https://doi.org/10.3390/ijerph14080925




