Community-Engaged Modeling of Geographic and Demographic Patterns of Multiple Public Health Risk Factors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Methodology
2.2.1. Construct New Bedford Synthetic Microdata
2.2.2. Prioritize Health Outcomes and Risk Factors
2.2.3. Literature Search for Candidate Predictors
2.2.4. Regression Modeling
2.2.5. Outcome Prediction
2.2.6. Outcome Presentation
3. Results
3.1. Literature Search Results
3.2. Regression Model Results
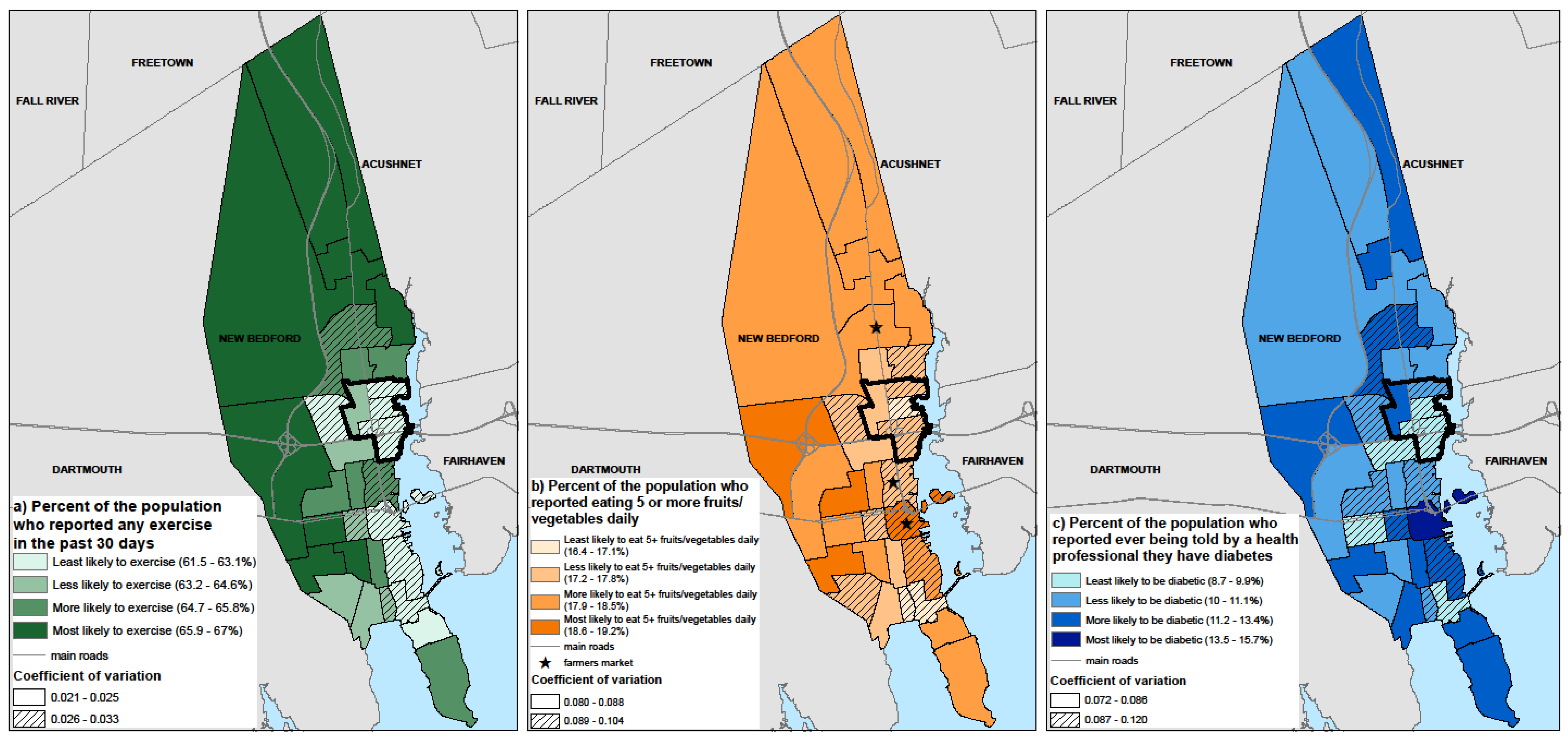
3.3. Identification of Census Tracts with Populations at High Risk for Modeled Outcomes
3.4. Evaluation of Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Dubowitz, T.; Williams, M.; Steiner, E.; Weden, M.; Miyashiro, L.; Jacobson, D.; Lurie, N. Using Geographic Information Systems to Match Local Health Needs With Public Health Services and Programs. Am. J. Public Health 2011, 101, 1664. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.M.; Pearce, J.R.; Harland, K. Can a Deterministic Spatial Microsimulation Model Provide Reliable Small-Area Estimates of Health Behaviours? An Example of Smoking Prevalence in New Zealand. Health Place 2011, 17, 618–624. [Google Scholar] [CrossRef] [PubMed]
- Riva, M.; Smith, D.M. Generating Small-Area Prevalence of Psychological Distress and Alcohol Consumption: Validation of a Spatial Microsimulation Method. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Koh, K.; Grady, S.C.; Vojnovic, I. Using Simulated Data to Investigate the Spatial Patterns of Obesity Prevalence at the Census Tract Level in Metropolitan Detroit. Appl. Geogr. 2015, 62, 19–28. [Google Scholar] [CrossRef]
- Edwards, K.L.; Clarke, G.P.; Ransley, J.K.; Cade, J. The Neighbourhood Matters: Studying Exposures Relevant to Childhood Obesity and the Policy Implications in Leeds, UK. J. Epidemiol. Community Health 2010, 64, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Tanton, R. Spatial Microsimulation as a Method for Estimating Different Poverty Rates in Australia. Popul. Space Place 2011, 17, 222–235. [Google Scholar] [CrossRef]
- Westfall, J.M.; Fagnan, L.J.; Handley, M.; Salsberg, J.; Mcginnis, P.; Zittleman, L.K.; Macaulay, A.C. Practice-Based Research Is Community Engagement. J. Am. Board Fam. Med. 2009, 22, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Detres, M.; Lucio, R.; Vitucci, J. GIS as a Community Engagement Tool: Developing a Plan to Reduce Infant Mortality Risk Factors. Matern. Child. Health J. 2014, 18, 1049–1055. [Google Scholar] [CrossRef] [PubMed]
- Kruger, D.J.; Brady, J.S.; Shirey, L.A. Using GIS to Facilitate Community-Based Public Health Planning of Diabetes Intervention Efforts. Health Promot. Pract. 2008, 9, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Levy, J.I.; Fabian, M.P.; Peters, J.L. Community-Wide Health Risk Assessment Using Geographically Resolved Demographic Data: A Synthetic Population Approach. PLoS ONE 2014, 9, e87144. [Google Scholar] [CrossRef] [PubMed]
- Peters, J.L.; Fabian, M.P.; Levy, J.I. Combined Impact of Lead, Cadmium, Polychlorinated Biphenyls and Non-Chemical Risk Factors on Blood Pressure in NHANES. Environ. Res. 2014, 132, 93–99. [Google Scholar] [CrossRef] [PubMed]
- US Census Bureau. QuickFacts: New Bedford, Massachusetts. Available online: http://www.census.gov/quickfacts/table/PST045215/2545000,25 (accessed on 28 February 2016).
- US EPA, R. 01. Harbor Cleanup. Available online: https://www.epa.gov/new-bedford-harbor/harbor-cleanup#Why (accessed on 2 May 2016).
- MA Executive Office of Energy and Environmental Affairs. 2010 Environmental Justice Populations. Available online: http://www.mass.gov/anf/docs/itd/services/massgis/ej-2010-communitystatistics.pdf (accessed on 2 May 2016).
- Payne-Sturges, D.C.; Korfmacher, K.S.; Cory-Slechta, D.A.; Jimenez, M.; Symanski, E.; Carr Shmool, J.L.; Dotson-Newman, O.; Clougherty, J.E.; French, R.; Levy, J.I.; et al. Engaging Communities in Research on Cumulative Risk and Social Stress-Environment Interactions: Lessons Learned from EPA’s STAR Program. Environ. Justice 2015, 8, 203–212. [Google Scholar] [CrossRef] [PubMed]
- CDC. About BRFSS. Available online: http://www.cdc.gov/brfss/about/index.htm (accessed on 2 May 2016).
- MA DPH. Data Query of 2005–2010 BRFSS Data from Health Survey Program at Massachusetts Department of Public Health; Maria McKenna and Paul Oppedisano: Boston, MA, USA. Available online: http://www.mass.gov/eohhs/gov/departments/dph/ (accessed on 18 May 2017).
- Boutelle, K.N.; Jeffery, R.W.; French, S.A. Predictors of Vigorous Exercise Adoption and Maintenance over Four Years in a Community Sample. Int. J. Behav. Nutr. Phys. Act. 2004, 1, 13. [Google Scholar] [CrossRef] [PubMed]
- Trudeau, E.; Kristal, A.R.; Li, S.; Patterson, R.E. Demographic and Psychosocial Predictors of Fruit and Vegetable Intakes Differ: Implications for Dietary Interventions. J. Am. Diet. Assoc. 1998, 98, 1412–1417. [Google Scholar] [CrossRef]
- Bruce, M.A.; Sims, M.; Miller, S.; Elliott, V.; Ladipo, M. One Size Fits All? Race, Gender and Body Mass Index among U.S. Adults. J. Natl. Med. Assoc. 2007, 99, 1152–1158. [Google Scholar] [PubMed]
- Ferriday, D.; Forde, C.G.; Brunstrom, J.M. Evaluating Predictors of BMI. Cross-Sectional Evidence from a Chicago-Based Cohort. Appetite 2012, 59. [Google Scholar] [CrossRef]
- Abbasi, A.; Peelen, L.M.; Corpeleijn, E.; van der Schouw, Y.T.; Stolk, R.P.; Spijkerman, A.M.; Moons, K.G.; Navis, G.; Bakker, S.J.; Beulens, J.W. Prediction Models for Risk of Developing Type 2 Diabetes: Systematic Literature Search and Independent External Validation Study. BMJ 2012, 345, e5900. [Google Scholar] [CrossRef] [PubMed]
- Carron, A.V.; Hausenblas, H.A.; Mack, D. Social Influence and Exercise: A Meta-Analysis. J. Sport Exerc. Psychol. 1996, 18, 1–16. [Google Scholar] [CrossRef]
- Humpel, N.; Owen, N.; Leslie, E. Environmental Factors Associated with Adults’ Participation in Physical Activity: A Review. Am. J. Prev. Med. 2002, 22, 188–199. [Google Scholar] [CrossRef]
- Shaikh, A.R.; Yaroch, A.L.; Nebeling, L.; Yeh, M.-C.; Resnicow, K. Psychosocial Predictors of Fruit and Vegetable Consumption in Adults: A Review of the Literature. Am. J. Prev. Med. 2008, 34, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Milton, B.; Attree, P.; French, B.; Povall, S.; Whitehead, M.; Popay, J. The Impact of Community Engagement on Health and Social Outcomes: A Systematic Review. Community Dev. J. 2012, 47, 316–334. [Google Scholar] [CrossRef]
- Grunbaum, J.A. Chapter 5: Challenges in Improving Community Engagement in Research; National Institutes of Health: Bethesda, MD, USA, 2011. [Google Scholar]
- Ahmed, S.M.; Palermo, A.-G.S. Community Engagement in Research: Frameworks for Education and Peer Review. Am. J. Public Health 2010, 100, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- US EPA Region 1. New Bedford, Community Involvement Plan (CIP) and Institutional Control Plan (ICP) for Seafood Consumption, 04-23-2015, SDMS# 574395; US EPA Region 1: Boston, MA, USA, 2015.
- Kennedy, S.; Kidd, M.P.; McDonald, J.T.; Biddle, N. The Healthy Immigrant Effect: Patterns and Evidence from Four Countries. J. Int. Migr. Integr. 2015, 16, 317–332. [Google Scholar] [CrossRef]
- Colasanti, K.J.A.; Conner, D.S.; Smalley, S.B. Understanding Barriers to Farmers’ Market Patronage in Michigan: Perspectives From Marginalized Populations. J. Hunger Environ. Nutr. 2010, 5, 316–338. [Google Scholar] [CrossRef]
| Main Effect Coefficients for Each Modeled Outcome | ||||
|---|---|---|---|---|
| Covariate | Exercise a | Fruit/vegetable b | BMI | Diabetes c |
| Sex | ||||
| Male | 0.086 * | −0.29 * | 0.036 * | 0.21 * |
| Age | ||||
| 18–29 | 0.40 * | −0.14 | 0.047 * | −1.65 * |
| 30–39 | 0.18 * | −0.35 * | 0.093 * | −0.93 * |
| 40–49 | 0.072 | −0.13 | 0.094 * | −0.29 * |
| 50–59 | −0.040 | 0.052 | 0.11 * | 0.44 * |
| 60–69 | −0.077 | 0.062 | 0.11 * | 0.72 * |
| 70–79 | −0.12 * | 0.16 | 0.079 * | 0.99 * |
| Race/ethnicity | ||||
| Black, non-Hispanic | −0.021 | 0.21 | NS | 0.071 |
| Hispanic | −0.35 * | 0.20 | NS | 0.19 |
| Other (includes Asian) | 0.24 * | −0.19 | NS | −0.11 |
| Income | ||||
| <$25,000 | −0.20 * | 0.051 | 0.02 * | 0.27 * |
| $25,000–34,999 | −0.014 | −0.17 * | 0.0098 | −0.068 |
| Education | ||||
| <High school | −0.26 * | −0.18 * | 0.034 * | NS |
| High school | −0.077 * | 0.000039 | 0.022 * | NS |
| Smoking | ||||
| Current | −0.30 * | −0.30 * | −0.05 * | −0.057 * |
| Former | 0.096 * | 0.078 | 0.0076 | 0.17 * |
| Alcohol | ||||
| At least one drink in past 30 days | 0.25 * | NS | −0.030 * | −0.36 * |
| Exercise | ||||
| Any exercise in past 30 days | N/A | 0.33 * | −0.043 * | −0.083 * |
| Fruit/vegetable consumption | ||||
| Five or more servings daily | N/A | N/A | −0.019 * | NS |
| BMI category | ||||
| Obese (BMI ≥ 30) | N/A | N/A | N/A | 0.91 * |
| Overweight (30 > BMI ≥ 25) | N/A | N/A | N/A | 0.054 |
| Normal Weight (25 > BMI ≥ 18.5) | N/A | N/A | N/A | −0.53 * |
| Outcome | New Bedford Synthetic Microdata Prevalence (95% CI) | New Bedford BRFSS Data, 2005–2010 Prevalence (95% CI) * | Massachusetts BRFSS Data, 2005–2010 Prevalence (95% CI) * |
|---|---|---|---|
| Exercise (self report in the past 30 days) | 64.9 (62.5–67.2) % | 66.3 (64.4–68.2) % | 78.2 (77.8–78.6) % |
| Fruit and vegetable consumption (>5 daily) | 17.9 (15.4–20.7) % | 20.6 (18.2–22.9) % | 27.5 (26.8–28.1) % |
| Diabetes (self reported doctor diagnosis) | 11.1 (9.8–12.4) % | 10.3 (9.3–11.4) % | 7.4 (7.2–7.6) % |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basra, K.; Fabian, M.P.; Holberger, R.R.; French, R.; Levy, J.I. Community-Engaged Modeling of Geographic and Demographic Patterns of Multiple Public Health Risk Factors. Int. J. Environ. Res. Public Health 2017, 14, 730. https://doi.org/10.3390/ijerph14070730
Basra K, Fabian MP, Holberger RR, French R, Levy JI. Community-Engaged Modeling of Geographic and Demographic Patterns of Multiple Public Health Risk Factors. International Journal of Environmental Research and Public Health. 2017; 14(7):730. https://doi.org/10.3390/ijerph14070730
Chicago/Turabian StyleBasra, Komal, M. Patricia Fabian, Raymond R. Holberger, Robert French, and Jonathan I. Levy. 2017. "Community-Engaged Modeling of Geographic and Demographic Patterns of Multiple Public Health Risk Factors" International Journal of Environmental Research and Public Health 14, no. 7: 730. https://doi.org/10.3390/ijerph14070730




