“Look at the Whole Me”: A Mixed-Methods Examination of Black Infant Mortality in the US through Women’s Lived Experiences and Community Context
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Background
2.2. Qualitative Data Collection
2.3. Qualitative Data Analysis
2.4. Quantitative Data Collection
2.5. Quantitative Data Analysis
3. Results
3.1. Qualitative Results: Descriptive Analysis of Interview Data
3.2. Individual Experiences
“I had the drug addict mom and moved backwards and forwards. I think that’s what brought the PTSD and depression on as I got older. And that’s the only thing I can contribute the loss of my child to, my mental state.”“They put me on antidepressants. I just rather deal with it on my own. Some days I cry a lot. Some days I’m mad. Some days I’m OK. But, it changed me. I can say that.”
“They [hospital staff] were like, ‘Your baby is dead. What you gonna do now?’ Basically.”“I did counseling for a while, but I stopped. How can you sit down with somebody and they telling me how to feel? I don’t like that. They never lost a child, but tell me how to feel? I mean, we planned her. We wanted her.”
“I highly recommend finding a support group or focus group. That helped me tremendously like I cannot stress how deeply those people impacted me. It would really make a difference in your whole grieving process because when you go to this support group again you are surrounded by people who totally understand you because they are going through the same thing.”“I think that if you are surrounded by people who are going through that same thing and you hear their stories and they hear your story, you come together.”“Yeah because there were other women there too were just like me and they had stories and some things helped me out and some things helped them out. So it was good. To even share that experience with other people when we had to go through the same thing.”
3.3. Interactions with Healthcare Providers and the Healthcare System
“Maybe they would have given me different care. Now that I see that with certain things they treat you based on what kind of insurance you have. I didn’t know it was like that until I fell victim to it.”“Get them in and get them out. Or make you sit there for hours before you are getting seen. Then they finally see you, they ask a few questions, they leave out the room. They’re ready to write you a prescription for something. They [the health care system] don’t care about Black people.“So the divisiveness in my healthcare came when I had to go to the hospital and was being treated by people who I had never known, and who didn’t know anything about me.”“I had a doctor say, ‘Oh, you’re young, you can have more kids.’ You don’t know what I have been through to even say that. Prior to my twins I had already lost two. I already had two miscarriages, two losses. I don’t want to hear that when I’m trying to fight for my child to be alive.”“I watched documentaries, I read books. I knew what I wanted, but I was treated like I didn’t know what I wanted.”“I remember the doctor not even looking at me. He was talking to me and he treated me like I said like a number. He said ‘How many times have you been pregnant?’ and I’m like never. Then he had to turn around like ‘Oh’ ... he’s looking like, ‘She’s just another Black girl in here and she needs health care and she probably had 4 or 5 children already.’ It’s like No! We are human. We care about our well-being just like you do.”
3.4. Contextual Factors
“A lot of Black people can’t afford what is necessary to make those changes, so you buy what you can afford to get cause you need to survive. And because we stay in survival mode, I feel that that is a great impact on how we’re affected in our health and other areas as well.”
“I didn’t have a car then. To get the faster bus, that was about a 15 min walk. So, we are in the hood. To get to the good grocery store, you would have to drive far out. Maybe 30 min away from where you stay at. It’s all city, it’s no country. It’s all city houses, buses, smog, dope boys, dope girls. It’s all city.”“You’re walking to the bus stop and you’re carrying cans, carrying cans from the grocery store. I’m carrying those gallons of milk from the WIC. I’m on the bus, I’ve got to go downtown. Gotta get on three buses, I’m pregnant. You can’t do that.”“But if you go to the White neighborhood you see health food stores. Yeah the good stuff, organic stuff. The Black neighborhood right now they not having those.”
“The police came and were asking us all types of questions like we did something wrong. They asked if she slept with us in the bed because that wouldn’t be safe and if she did, they were going to arrest us.”“Then the policemen came, taking pictures, questioning. I went off! As if we didn’t just lose our child. They questioned us like we did something wrong. Like we are some kind of criminals.”
“I was being treated like my pregnancy was a nuisance to them where her [my coworker] pregnancy and the pregnancies of other White women were celebrated.”“I’m a Black girl in the hood and all the people that got the power see is Black people having babies. They don’t see our conditions. They don’t see really what we go through. They don’t see the prejudices that we have to go through. A White girl 16 and pregnant and she is trash in poverty is better than a Black girl that is 16 and pregnant and she is trash in poverty.”“There is so much more to a woman than her pregnancy. They need to understand our eating, our living situation, our support system, our mental and physical health. It all makes a difference. Look at the whole me.”
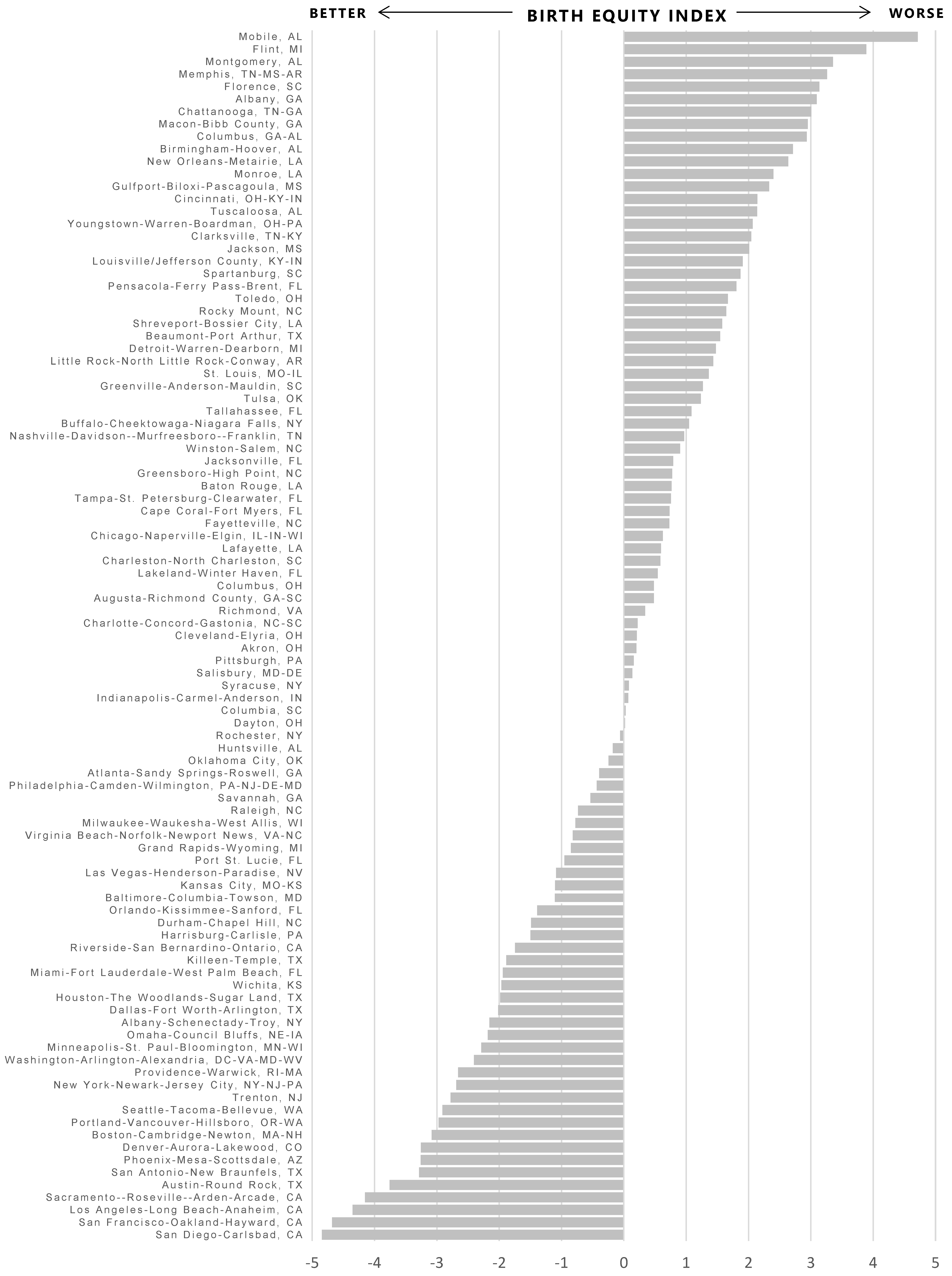
3.5. Quantitative Results: Associations between Contextual Indicators and Black Infant Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Matthews, T.J.; MacDorman, M.F.; Thoma, M.E. Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl. Vital Stat. Rep. 2015, 64, 1–30. [Google Scholar] [PubMed]
- Lorenz, J.M.; Ananth, C.V.; Polin, R.A.D.; Alton, M.E. Infant mortality in the United States. J. Perinatol. 2016, 36, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Marks, J. New information, enduring questions: Race, genetics, and medicine in the 21st century. Genewatch 2005, 18, 11–16. [Google Scholar] [PubMed]
- Feagin, J.; Bennefield, Z. Systemic racism and U.S. health care. Soc. Sci. Med. 2014, 103, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N. Methods for the scientific study of discrimination and health: An ecosocial approach. Am. J. Public Health 2012, 102, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Do, D.P.; Finch, B.K.; Basurto-Davila, R.; Bird, C.; Escarce, J.; Lurie, N. Does place explain racial health disparities? Quantifying the contribution of residential context to the Black/White health gap in the United States. Soc. Sci. Med. 2008, 67, 1258–1268. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, S.V.; Jones, K.; Kaddour, A.; Krieger, N. Revisiting Robinson: The perils of individualistic and ecologic fallacy. Int. J. Epidemiol. 2009, 38, 342–360. [Google Scholar] [CrossRef] [PubMed]
- Lukachko, A.; Hatzenbuehler, M.L.; Keyes, K.M. Structural racism and myocardial infarction in the United States. Soc. Sci. Med. 2014, 103, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, A.; Jones, M.K.; Bruce, D.J.; Erwin, P.C. Do racial inequities in infant mortality correspond to variations in societal conditions? A study of state-level income inequality in the USA, 1992–2007. Soc. Sci. Med. 2016, 164, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Fry-Johnson, Y.W.; Levine, R.; Rowley, D.; Agboto, V.; Rust, G. United States Black: White infant mortality disparities are not inevitable: Identification of community resilience independent of socioeconomic status. Ethn. Dis. 2010, 20, S1:131–S1:135. [Google Scholar]
- Schoendorf, K.C.; Hogue, C.J.; Kleinman, J.C.; Rowley, D. Mortality among infants of Black as compared with White college-educated parents. N. Engl. J. Med. 1992, 326, 1522–1526. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.R.; Hogue, C.J.; Dunlop, A.L.; Menon, R. Preconceptional stress and racial disparities in preterm birth: An overview. Acta Obstet. Gynecol. Scand. 2011, 90, 1307–1316. [Google Scholar] [CrossRef] [PubMed]
- Hogue, C.J.; Hargraves, M.A. Class, race, and infant mortality in the United States. Am. J. Public Health 1993, 83, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Saada, A. The social determinants of infant mortality and birth outcomes in western developed nations: A cross-country systematic review. Int. J. Environ. Res. Public Health 2013, 10, 2296–2335. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. 2008. Available online: http://apps.who.int/iris/bitstream/10665/43943/1/9789241563703_eng.pdf (accessed on 7 March 2017).
- Collins, J.W., Jr.; Hawkes, E.K. Racial differences in post-neonatal mortality in Chicago: What risk factors explain the Black infant’s disadvantage? Ethn. Health 1997, 2, 117–125. [Google Scholar] [CrossRef] [PubMed]
- National Birth Equity Collaborative 2016. Available online: http://birthequity.org/ (accessed on 7 March 2017).
- Tashakkori, A.M.; Teddlie, C.B. Handbook of Mixed Methods in the Social and Behavioral Sciences, 2nd ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2010. [Google Scholar]
- Creswell, J.W. Research design: Qualitative, Quantitative, and Mixed Methods Approaches, 4th ed.; Sage Publications: Los Angeles, CA, USA, 2014. [Google Scholar]
- Everitt, B.S.; Dunn, G. Principal components analysis. In Applied Multivariate Data Analysis, 2nd ed.; Wiley & Sons, Ltd.: Hoboken, NJ, USA, 1993; pp. 48–73. [Google Scholar]
- Williams, D.R.; Mohammed, S.A. Racism and health ii: A needed research agenda for effective interventions. Am. Behav. Sci. 2013, 57, 1200–1226. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Collins, C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep. 2001, 116, 404–416. [Google Scholar] [CrossRef]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Rothwell, J.T.; Massey, D.S. Density zoning and class segregation in U.S. metropolitan areas. Soc. Sci. Q. 2010, 91, 1123–1143. [Google Scholar] [CrossRef] [PubMed]
- US Census Bureau. Racial and Ethnic Segregation in the United States: 1980–2000. Available online: https://www.census.gov/hhes/www/housing/resseg/pdf/app_b.pdf (accessed on 15 June 2017).
- Britton, M.L.; Shin, H. Metropolitan residential segregation and very preterm birth among African American and Mexican-origin women. Soc. Sci. Med. 2013, 98, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Debbink, M.P.; Bader, M.D. Racial residential segregation and low birth weight in Michigan’s metropolitan areas. Am. J. Public Health 2011, 101, 1714–1720. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.R.; Cooper, H.L.; Drews-Botsch, C.D.; Waller, L.A.; Hogue, C.R. Metropolitan isolation segregation and Black-White disparities in very preterm birth: A test of mediating pathways and variance explained. Soc. Sci. Med. 2010, 71, 2108–2116. [Google Scholar] [CrossRef] [PubMed]
- Mason, S.M.; Messer, L.C.; Laraia, B.A.; Mendola, P. Segregation and preterm birth: The effects of neighborhood racial composition in North Carolina. Health Place 2009, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Nyarko, K.A.; Wehby, G.L. Residential segregation and the health of African-American infants: Does the effect vary by prevalence? Matern. Child Health J. 2012, 16, 1491–1499. [Google Scholar] [CrossRef] [PubMed]
- Grady, S.C. Racial disparities in low birthweight and the contribution of residential segregation: A multilevel analysis. Soc. Sci. Med. 2006, 63, 3013–3029. [Google Scholar] [CrossRef] [PubMed]
- Messer, L.C.; Laraia, B.A.; Kaufman, J.S.; Eyster, J.; Holzman, C.; Culhane, J.; Elo, I.; Burke, J.G.; O’Campo, P. The development of a standardized neighborhood deprivation index. J. Urban Health 2006, 83, 1041–1062. [Google Scholar] [CrossRef] [PubMed]
- Cerda, M.; Tracy, M.; Ahern, J.; Galea, S. Addressing population health and health inequalities: The role of fundamental causes. Am. J. Public Health 2014, 104, S609–S619. [Google Scholar] [CrossRef] [PubMed]
| Indicator | Definition | Source and Year |
|---|---|---|
| Education | % of Non-Hispanic (NH) Black residents age 25 and older with less than a high school education | American Community Survey, 2009–2013 5-year estimate |
| Unemployment | % of NH Black residents in the civilian labor force who are unemployed | American Community Survey, 2009–2013 5-year estimate |
| Residential segregation | Isolation index is the minority-weighted average of the minority population i neach area. Values range from 0 (complete integration) to 1 (complete segregation) | Census, 2010 |
| Adult smoking | % of the adult population that currently smokes | Behavioral Risk Factor Surveillance System (BRFSS) |
| Poor mental health days | Average number of mentally unhealthy days reported in the past 30 days (age-adjusted) | BRFSS, 2006–2012 average |
| Poor physical health days | Average number of physically unhealthy days reported in the past 30 days (age-adjusted) | BRFSS, 2006–2012 average |
| Adult obesity | % of adults that report a body mass index (BMI) of ≥30 | Centers for Disease Control and Prevention (CDC) Diabetes Interactive Atlas, 2011 |
| Limited access to healthy foods | % of the population who are low-income and do not live close to a grocery store. | United States Department of Agriculture (USDA) Food Environment Atlas, 2010 |
| Homicide rate | Homicide deaths per 100,000 residents | CDC WONDER mortality data, 2006–2012 average |
| Air pollution | Daily fine particulate matter (average daily measure in micrograms per cubic meter). | CDC WONDER Environmental Data, 2011 |
| Jail admissions | Annual admissions per 100,000 residents age 15–64 | Bureau of Justice Statistics, 2012 |
| Structural racism (Racial inequality in income) | NH White to NH Black ratio of median household income | American Community Survey, 2009–2013 5-year estimate |
| Mean (Standard Deviation, STD) | Min | Max | IQR * | |
|---|---|---|---|---|
| Total IMR, deaths per 1000 live births | 6.86 (1.61) | 3.92 | 12.14 | 2.01 |
| NH Black IMR, deaths per 1000 live births | 11.66 (2.19) | 5.62 | 16.94 | 2.55 |
| NH White IMR, deaths per 1000 live births | 5.08 (1.17) | 2.32 | 8.44 | 1.62 |
| NH Black/NH White IMR ratio | 2.38 (0.61) | 1.10 | 6.26 | 0.67 |
| NH Black/NH White IMR difference | 6.58 (1.89) | 0.53 | 13.89 | 2.29 |
| Social Determinants Indicators | ||||
| NH Black unemployment, % | 16.84 (3.24) | 10.64 | 27.09 | 4.27 |
| NH Black population age 25 and older with less than a high school diploma, % | 17.17 (4.34) | 9.06 | 30.19 | 5.87 |
| Structural racism (ratio of NH White to NH Black median household income) | 1.80 (0.23) | 1.20 | 2.35 | 0.30 |
| Residential segregation (isolation) | 42.97 (16.05) | 8.80 | 80.90 | 21.95 |
| Smoking prevalence among adults, % | 19.77 (3.72) | 10.38 | 26.69 | 5.57 |
| Obesity prevalence among adults, % | 29.82 (3.95) | 18.94 | 36.90 | 5.07 |
| Limited access to healthy foods, % | 6.36 (3.09) | 1.19 | 16.83 | 3.85 |
| Homicide rate, per 100,000 population | 6.23 (2.86) | 2.18 | 15.20 | 3.39 |
| Air pollution (particulate matter <2.5 micrometers in aerodynamic diameter), mg/m3 | 11.70 (1.54) | 7.87 | 14.54 | 2.16 |
| Jail admission rate, per 100,000 population | 6428.23 (2598.94) | 1544.3 | 13,033.73 | 3524.22 |
| Poor mental health days, n | 3.57 (0.46) | 2.54 | 4.80 | 0.57 |
| Poor physical health days, n | 3.65 (0.49) | 2.60 | 4.93 | 0.76 |
| Poverty, % | 15.63 (3.18) | 8.20 | 26.10 | 3.65 |
| Model A a | Model B b | Model C c | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Indicator | RR | 95% CI | Beta | 95% CI | Beta | 95% CI | |||
| NH Black unemployment | 1.06 | 1.01 | 1.11 | 0.15 | 0.02 | 0.28 | 0.47 | 0.03 | 0.91 |
| NH Black less than high school education | 1.05 | 0.95 | 1.17 | 0.13 | −0.04 | 0.30 | 0.35 | −0.22 | 0.92 |
| Structural racism (racial income inequality) | 1.08 | 1.01 | 1.16 | 0.14 | −0.01 | 0.28 | 0.48 | −0.03 | 0.98 |
| Residential segregation (isolation) | 1.10 | 1.05 | 1.15 | 0.20 | 0.06 | 0.35 | 1.14 | 0.66 | 1.62 |
| Smoking prevalence among adults | 1.20 | 1.13 | 1.27 | −0.26 | −0.46 | −0.06 | 0.22 | −0.39 | 0.82 |
| Obesity prevalence among adults | 1.16 | 1.10 | 1.22 | −0.20 | −0.35 | −0.05 | 0.41 | −0.04 | 0.86 |
| Limited access to healthy foods | 1.09 | 1.01 | 1.19 | −0.09 | −0.21 | 0.03 | 0.01 | −0.43 | 0.45 |
| Homicide rate | 1.07 | 0.99 | 1.15 | 0.19 | 0.03 | 0.34 | 0.57 | 0.08 | 1.06 |
| Air pollution | 1.11 | 1.03 | 1.19 | −0.02 | −0.14 | 0.10 | 0.56 | 0.13 | 0.99 |
| Jail admission rate | 1.06 | 0.96 | 1.18 | −0.12 | −0.33 | 0.09 | −0.07 | −0.82 | 0.69 |
| Poor mental health days | 1.12 | 1.04 | 1.20 | −0.21 | −0.37 | −0.06 | −0.25 | −0.72 | 0.22 |
| Poor physical health days | 1.13 | 1.03 | 1.25 | −0.33 | −0.53 | −0.13 | −0.32 | −0.96 | 0.31 |
| Principal Component 1 | Principal Component 2 | Principal Component 3 | |
|---|---|---|---|
| Eigenvalue | 4.41 | 2.02 | 1.20 |
| % of total variance explained | 36.7% | 16.8% | 10.0% |
| Indicator Variable Loadings | |||
| NH Black unemployment, % | −0.43 | 0.68 | 0.20 |
| NH Black less than high school education, % | 0.38 | 0.53 | −0.16 |
| Structural racism (racial income inequality) | −0.04 | 0.70 | −0.39 |
| Residential segregation (isolation) | 0.44 | 0.60 | −0.08 |
| Smoking prevalence among adults, % | 0.38 | 0.29 | 0.49 |
| Obesity prevalence among adults, % | 0.74 | 0.19 | 0.14 |
| Limited access to healthy foods, % | 0.64 | −0.14 | 0.21 |
| Homicide rate, per 100,000 | 0.79 | 0.06 | −0.02 |
| Air pollution, mg/m3 | −0.04 | 0.66 | 0.35 |
| Jail admission rate, per 100,000 | 0.77 | −0.23 | 0.04 |
| Poor mental health days, n | −0.04 | −0.06 | 0.90 |
| Poor physical health days, n | 0.25 | −0.02 | 0.79 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wallace, M.E.; Green, C.; Richardson, L.; Theall, K.; Crear-Perry, J. “Look at the Whole Me”: A Mixed-Methods Examination of Black Infant Mortality in the US through Women’s Lived Experiences and Community Context. Int. J. Environ. Res. Public Health 2017, 14, 727. https://doi.org/10.3390/ijerph14070727
Wallace ME, Green C, Richardson L, Theall K, Crear-Perry J. “Look at the Whole Me”: A Mixed-Methods Examination of Black Infant Mortality in the US through Women’s Lived Experiences and Community Context. International Journal of Environmental Research and Public Health. 2017; 14(7):727. https://doi.org/10.3390/ijerph14070727
Chicago/Turabian StyleWallace, Maeve E., Carmen Green, Lisa Richardson, Katherine Theall, and Joia Crear-Perry. 2017. "“Look at the Whole Me”: A Mixed-Methods Examination of Black Infant Mortality in the US through Women’s Lived Experiences and Community Context" International Journal of Environmental Research and Public Health 14, no. 7: 727. https://doi.org/10.3390/ijerph14070727





