The Cost-Effectiveness of Lowering Permissible Noise Levels Around U.S. Airports
Abstract
:1. Introduction
2. Materials and Methods
2.1. Overview
- (1)
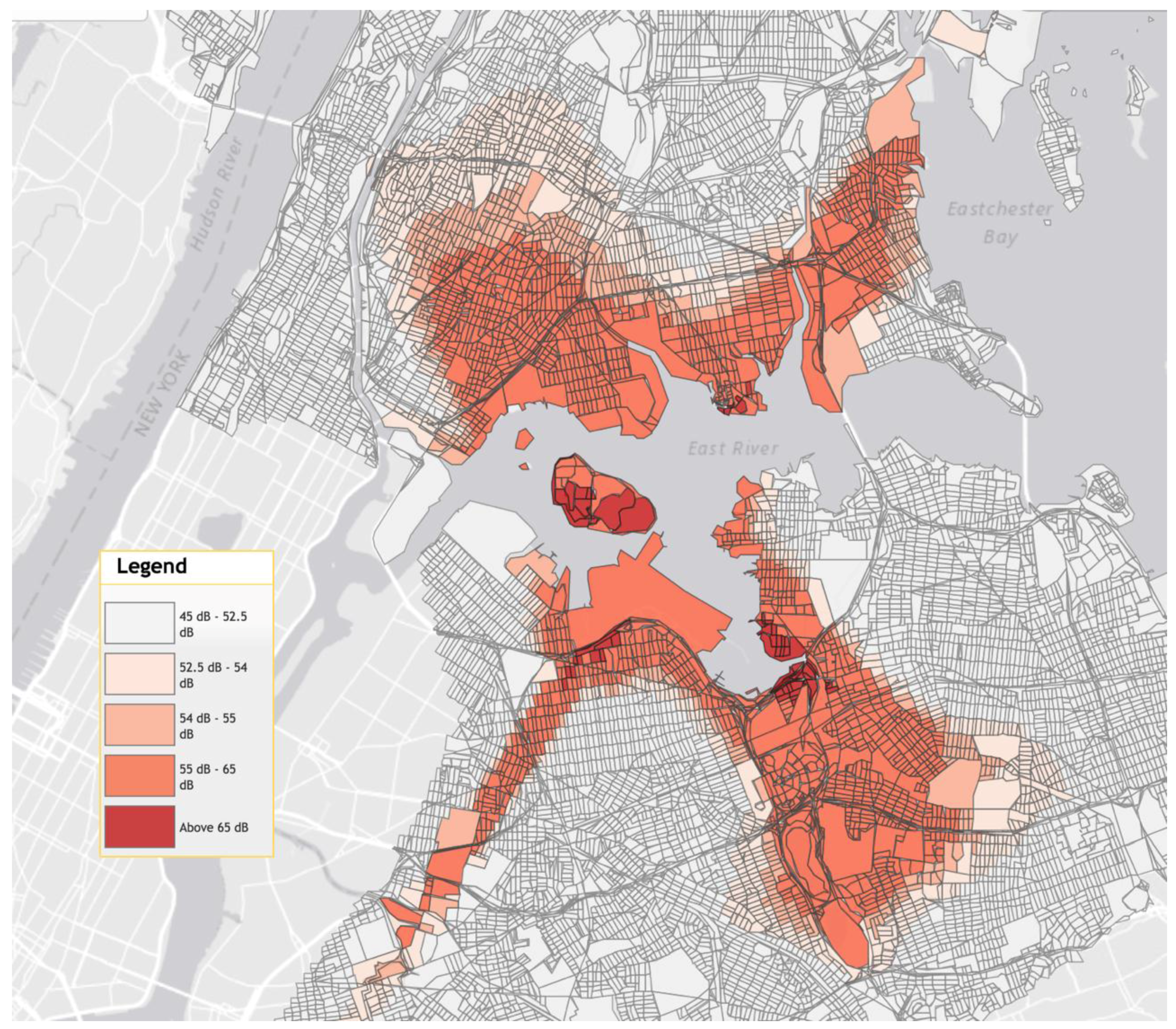
- People currently being exposed to >55 to ≤65 dB DNL;
- (2)
- The same cohort with noise insulation adequate to reduce noise exposure to below 55 dB DNL.
2.2. Model Parameters
2.2.1. Probability
2.2.2. Relative Risk
2.2.3. Cost
2.2.4. Health Utility
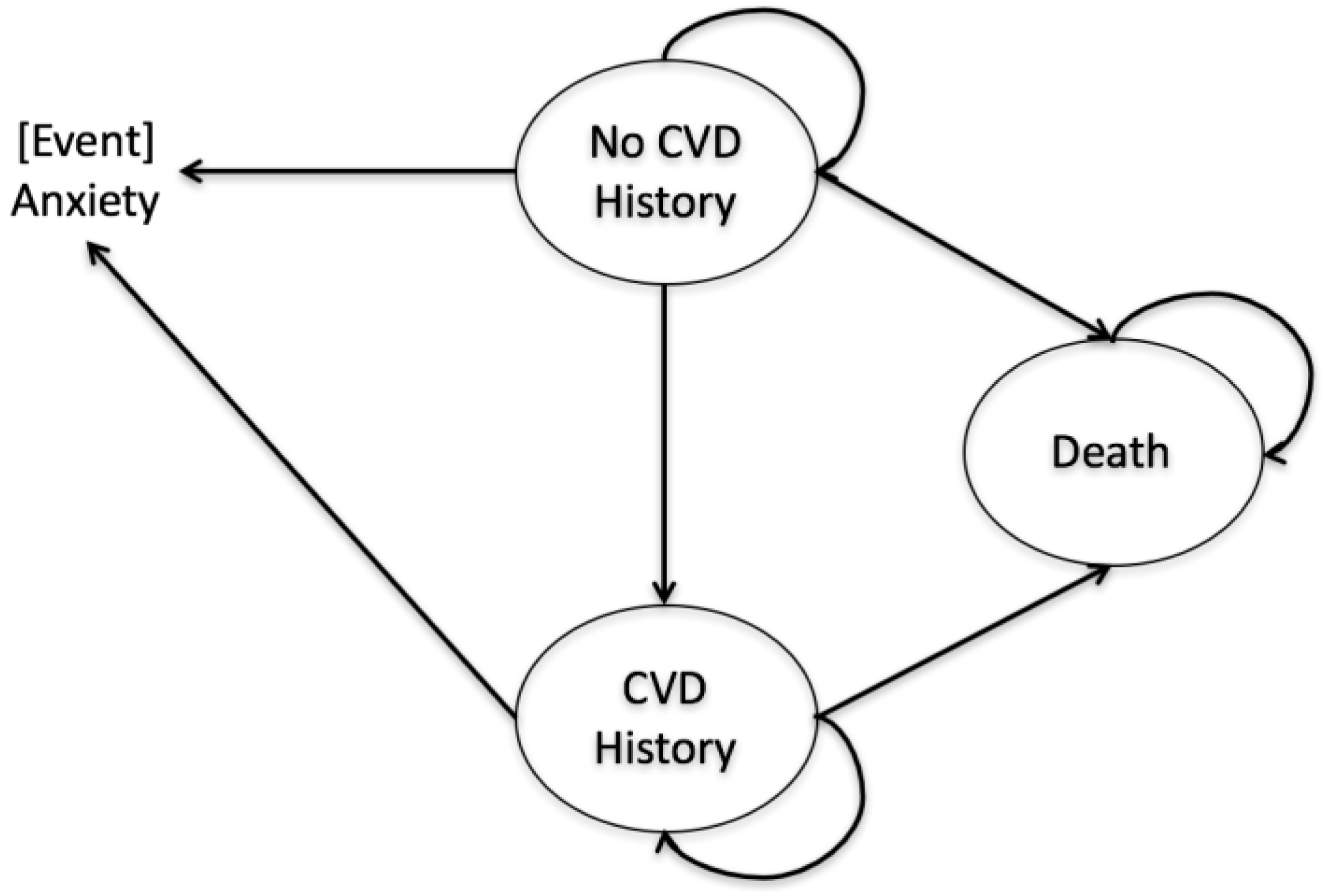
2.3. Decision Analysis Models
- (1)
- We used the average nation-wide cost of sound insulation per person for our model. It was assumed that the household size in neighborhoods near LGA was same as nation-wide average household size.
- (2)
- The RRs of CVD and anxiety associated with aircraft noises were based on studies conducted in the United Kingdom and Italy. We assumed that they were generalizable to the United States.
- (3)
- There was no data on RRs of CVD and anxiety associated with aircraft noises for different age groups. They were assumed to be constant over the life course.
- (4)
- For those who developed both CVD and anxiety, we assumed that health utility decrement due to anxiety was already captured in health utility decrement due to CVD.
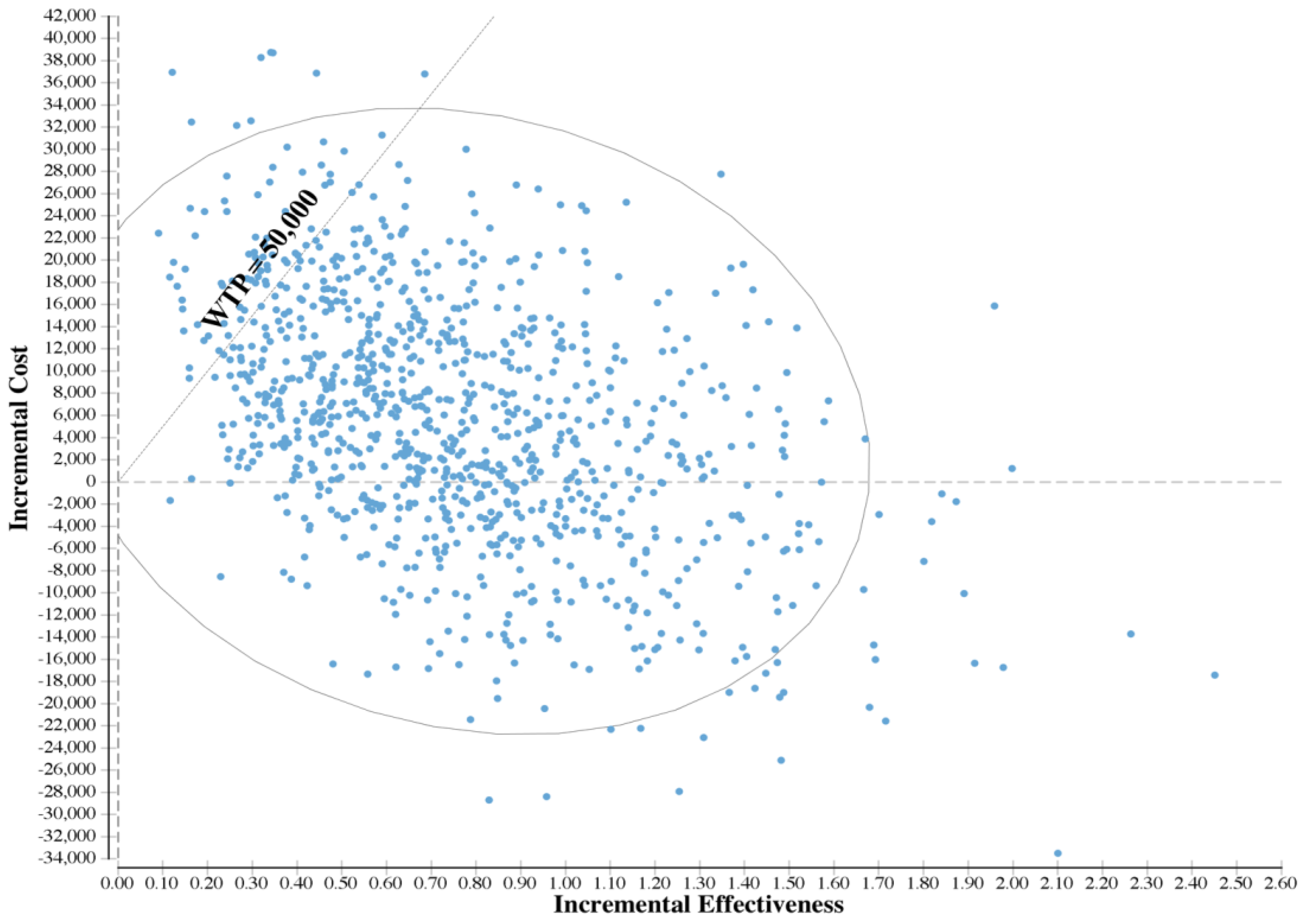
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Holzman, D. Plane pollution. Environ. Health Perspect. 1997, 105, 1300. [Google Scholar] [CrossRef] [PubMed]
- Kryter, K.D. Acoustical, sensory, and psychological research data and procedures for their use in predicting effects of environmental noises. J. Acoust. Soc. Am. 2007, 122, 2601–2614. [Google Scholar] [CrossRef] [PubMed]
- Mestre, V.; Schomer, P.; Fidell, S.; Berry, B. Technical Support for Day/Night Average Sound Level (DNL) Replacement Metric Research. 2011. Available online: https://nqsc.org/downloads/volpereport.pdf (accessed on 6 September 2017).
- Fritschi, L.; Brown, L.; Kim, R.; Schwela, D.; Kephalopolous, S. Burden of Disease from Environmental Noise: Quantification of Healthy Years Life Lost in Europe; World Health Organisation: Geneva, Switzerland, 2011. [Google Scholar]
- World Health Organization. Guidelines for Community Noise; WHO: Geneva, Switzerland, 1999. [Google Scholar]
- European Environment Agency. Noise in Europe 2014; EEA: Copenhagen, Denmark, 2014. [Google Scholar]
- Basner, M.; Babisch, W.; Davis, A.; Brink, M.; Clark, C.; Janssen, S.; Stansfeld, S. Auditory and non-auditory effects of noise on health. Lancet 2014, 383, 1325–1332. [Google Scholar] [CrossRef]
- Hansell, A.L.; Blangiardo, M.; Fortunato, L.; Floud, S.; de Hoogh, K.; Fecht, D.; Ghosh, R.E.; Laszlo, H.E.; Pearson, C.; Beale, L. Aircraft noise and cardiovascular disease near heathrow airport in london: Small area study. BMJ 2013, 347, f5432. [Google Scholar] [CrossRef] [PubMed]
- Hardoy, M.C.; Carta, M.G.; Marci, A.R.; Carbone, F.; Cadeddu, M.; Kovess, V.; Dell’Osso, L.; Carpiniello, B. Exposure to aircraft noise and risk of psychiatric disorders: The elmas survey. Soc. Psychiatry Psychiatr. Epidemiol. 2005, 40, 24–26. [Google Scholar] [CrossRef] [PubMed]
- Hatfield, J.; Job, R.; Carter, N.; Peploe, P.; Taylor, R.; Morrell, S. The influence of psychological factors on self-reported physiological effects of noise. Noise Health 2001, 3, 1. [Google Scholar] [PubMed]
- Boes, S.; Nüesch, S.; Stillman, S. Aircraft noise, health, and residential sorting: Evidence from two quasi-experiments. Health Econ. 2013, 22, 1037–1051. [Google Scholar] [CrossRef] [PubMed]
- Lawton, R.N.; Fujiwara, D. Living with aircraft noise: Airport proximity, aviation noise and subjective wellbeing in England. Transp. Res. Part D Transp. Environ. 2016, 42, 104–118. [Google Scholar] [CrossRef]
- Lefèvre, M.; Carlier, M.-C.; Champelovier, P.; Lambert, J.; Laumon, B.; Evrard, A.-S. Effects of aircraft noise exposure on saliva cortisol near airports in France. Occup. Environ. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- European Environment Agency. Good Practice Guide on Noise Exposure and Potential Health Effects; EEA: Copenhagen, Denmark, 2010. [Google Scholar]
- Girvin, R. Aircraft noise-abatement and mitigation strategies. J. Air Transp. Manag. 2009, 15, 14–22. [Google Scholar] [CrossRef]
- Licitra, G.; Gagliardi, P.; Fredianelli, L.; Simonetti, D. Noise mitigation action plan of pisa civil and military airport and its effects on people exposure. Appl. Acoust. 2014, 84, 25–36. [Google Scholar] [CrossRef]
- Netjasov, F. Contemporary measures for noise reduction in airport surroundings. Appl. Acoust. 2012, 73, 1076–1085. [Google Scholar] [CrossRef]
- Ganic, E.M.; Netjasov, F.; Babic, O. Analysis of noise abatement measures on European airports. Appl. Acoust. 2015, 92, 115–123. [Google Scholar] [CrossRef]
- Ganic, E.; Dobrota, M.; Babic, O. Noise abatement measures at airports: Contributing factors and mutual dependence. Appl. Acoust. 2016, 112, 32–40. [Google Scholar] [CrossRef]
- Wolfe, P.J.; Malina, R.; Barrett, S.R.; Waitz, I.A. Costs and benefits of us aviation noise land-use policies. Transp. Res. Part D Transp. Environ. 2016, 44, 147–156. [Google Scholar] [CrossRef]
- Gagliardi, P.; Fredianelli, L.; Simonetti, D.; Licitra, G. Ads-B system as a useful tool for testing and redrawing noise management strategies at Pisa airport. Acta Acust. United Acust. 2017, 103, 543–551. [Google Scholar] [CrossRef]
- Cohen, J.P.; Coughlin, C.C. Changing noise levels and housing prices near the Atlanta airport. Growth Chang. 2009, 40, 287–313. [Google Scholar] [CrossRef]
- MSP FairSkies Coalition; University of Minnesota Center for Urban and Regional Affairs. Map of Airplane Noise Levels. 2010. Available online: http://mspfairskies.com/map-of-airplane-noise-levels/ (accessed on 10 March 2017).
- Walsh, K. Forgotton Queens; Arcadia Publishing: New York, NY, USA, 2013. [Google Scholar]
- New York City Department of City Planning. New York City Population-Population Fact; New York City Department of City Planning: New York, NY, USA, 2015. [Google Scholar]
- Mason, H.; Baker, R.; Donaldson, C. Willingness to pay for a QALY: Past, present and future. Expert Rev. Pharmacoecon. Outcomes Res. 2008, 8, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Neumann, P.J.; Cohen, J.T.; Weinstein, M.C. Updating cost-effectiveness—The curious resilience of the $50,000-per-QALY threshold. N. Engl. J. Med. 2014, 371, 796–797. [Google Scholar] [CrossRef] [PubMed]
- Paulden, M.; O’Mahony, J.F.; McCabe, C. Discounting the recommendations of the second panel on cost-effectiveness in health and medicine. PharmacoEconomics 2017, 35, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.-P.; Fullerton, H.J. Heart disease and stroke statistics—2016 update. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Arias, E.; Heron, M.; Xu, J. United States Life Tables. 2012. Available online: https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_08.pdf (accessed on 21 January 2017).
- Nichols, G.A.; Bell, T.J.; Pedula, K.L.; O’Keeffe-Rosetti, M. Medical care costs among patients with established cardiovascular disease. Am. J. Manag. Care 2010, 16, e86–e93. [Google Scholar] [PubMed]
- Fan, A.Z.; Strine, T.W.; Jiles, R.; Mokdad, A.H. Depression and anxiety associated with cardiovascular disease among persons aged 45 years and older in 38 states of the United States, 2006. Prev. Med. 2008, 46, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Chau, C.; Yik, F.; Hui, W.; Liu, H.; Yu, H. Environmental impacts of building materials and building services components for commercial buildings in Hong Kong. J. Clean. Prod. 2007, 15, 1840–1851. [Google Scholar] [CrossRef]
- Greenberg, P.E.; Sisitsky, T.; Kessler, R.C.; Finkelstein, S.N.; Berndt, E.R.; Davidson, J.R.; Ballenger, J.C.; Fyer, A.J. The economic burden of anxiety disorders in the 1990s. J. Clin. Psychiatry 1999, 60, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.; Adams, R.J.; Brown, T.M.; Carnethon, M.; Dai, S.; De Simone, G.; Ferguson, T.B.; Ford, E.; Furie, K.; Gillespie, C. Heart disease and stroke statistics—2010 update. Circulation 2010, 121, e46–e215. [Google Scholar] [PubMed]
- Whitehead, S.J.; Ali, S. Health outcomes in economic evaluation: The QALY and utilities. Br. Med. Bull. 2010, 96, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Ara, R.; Brazier, J. Health Related Quality of Life by Age, Gender and History of Cardiovascular Disease: Results from the Health Survey for England. 2009. Available online: http://eprints.whiterose.ac.uk/10880/ (accessed on 15 March 2017).
- Ara, R.; Brazier, J.E. Populating an economic model with health state utility values: Moving toward better practice. Value Health 2010, 13, 509–518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hurst, N.; Kind, P.; Ruta, D.; Hunter, M.; Stubbings, A. Measuring health-related quality of life in rheumatoid arthritis: Validity, responsiveness and reliability of EuroQol (EQ-5D). Rheumatology 1997, 36, 551–559. [Google Scholar] [CrossRef]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Shapiro, S.A. Lessons from a public policy failure: EPA and noise abatement. Ecol. Law Q. 1992, 19, 1. [Google Scholar]
- Bureau of Aircraft Accidents Archive. Available online: http://www.baaa-acro.com/general-statistics/death-rate-per-year/ (accessed on 6 September 2017).
- Tengs, T.O. Dying too Soon: How Cost-Effectiveness Analysis Can Save Lives; National Center for Policy Analysis: Dallas, TX, USA, 1997. [Google Scholar]
- Tengs, T.O.; Graham, J.D. The opportunity costs of haphazard social investments in life-saving. In Risks, Costs, and Lives Saved: Getting Better Results from Regulation; Oxford University Press: Oxford, UK, 1996; pp. 167–182. [Google Scholar]
- Tengs, T.O.; Adams, M.E.; Pliskin, J.S.; Safran, D.G.; Siegel, J.E.; Weinstein, M.C.; Graham, J.D. Five-hundred life-saving interventions and their cost-effectiveness. Risk Anal. 1995, 15, 369–390. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.G.; Mueller, J. A risk and cost-benefit assessment of United States aviation security measures. J. Transp. Secur. 2008, 1, 143–159. [Google Scholar] [CrossRef]
- Paltiel, A.D.; Weinstein, M.C.; Kimmel, A.D.; Seage, G.R., 3rd; Losina, E.; Zhang, H.; Freedberg, K.A.; Walensky, R.P. Expanded screening for HIV in the United States—An analysis of cost-effectiveness. N. Engl. J. Med. 2005, 352, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Di Nisi, J.; Muzet, A.; Ehrhart, J.; Libert, J. Comparison of cardiovascular responses to noise during waking and sleeping in humans. Sleep 1990, 13, 108–120. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Base | Standard Error/Range | Distribution * | Source |
|---|---|---|---|---|
| Cost (2016 U.S.$) | ||||
| Direct Cost | ||||
| Medical cost of cardiovascular disease (CVD) | 23,229 | 5807 | Gamma | Nichols et al., 2010 |
| Medical cost of anxiety | 2814 | 704 | Gamma | Greenberg et al., 1999 |
| Cost of sound insulation | 18,959 | 4740 | Gamma | Wolfe et al., 2016 |
| Indirect Cost | ||||
| Productivity loss of CVD | 12,837 | 3209 | Gamma | Lloyd-Jones et al., 2010; Nichols et al., 2010 |
| Productivity loss of Anxiety | 313 | 78 | Gamma | Greenberg et al., 1999 |
| Health Utility Value | ||||
| Health utility decrement due to CVD | 0.283 | 0.0130 | Beta | Ara et al., 2010; Ara et al., 2009 |
| Health utility decrement due to anxiety | 0.156 | 0.0391 | Beta | EQ5D |
| Health utility of CVD history | 0.844 | 0.0096 | Beta | Ara et al., 2010; Ara et al., 2009 |
| Probability | ||||
| Probability of developing a CVD (by age) | Mozaffarian et al., 2016 | |||
| 35–44 | 0.15% | 0.04% | Beta | |
| 45–54 | 0.71% | 0.18% | Beta | |
| 55–64 | 1.49% | 0.37% | Beta | |
| 65–74 | 2.66% | 0.67% | Beta | |
| 75–84 | 4.78% | 1.20% | Beta | |
| 85 and above | 6.81% | 1.70% | Beta | |
| Probability of developing an anxiety disorder | 18.10% | 0.70% | Beta | Kessler et al., 2005 |
| Relative Risk (RR) | ||||
| RR of CVD for aircraft noise exposure | 1.12 | low: 1.07; high: 1.18 | Triangular | Hansell et al., 2013 |
| RR of anxiety for aircraft noise exposure | 1.69 | low: 1.00; high: 2.66 | Triangular | Hardoy et al., 2005 |
| RR of anxiety for CVD patients | 1.66 | low: 1.49; high: 1.82 | Triangular | Fan et al., 2008 |
| RR of CVD among those with prior CVD history | 1.97 | low: 1.67; high: 2.30 | Triangular | Nichols et al., 2010 |
| Strategy | Cost | Incremental Cost | QALY | Incremental QALY | ICER * |
|---|---|---|---|---|---|
| Status quo | 635,369 | 19.61 | |||
| Changing the regulatory DNL level from 65 dB to 55 dB | 642,162 | 6793 | 20.22 | 0.61 | 11,163 |
| Variable | Incremental Cost-Effectiveness Ratio * | |
|---|---|---|
| Low | High | |
| Relative risk (RR) of anxiety for aircraft noise exposure (Low: 1.00; High: 2.66) | 195,717 | Cost-saving |
| Cost of sound insulation (Low: −25%; High: +25%) † | Cost-saving | 24,448 |
| RR of cardiovascular disease (CVD) for aircraft noise exposure (Low: 1.07; High: 1.18) | 20,539 | 2822 |
| Medical cost of anxiety (Low: −25%; High: +25%) † | 16,316 | 6010 |
| Medical cost of CVD (Low: −25%; High: +25%) † | 15,931 | 6394 |
| Probability of developing a CVD (Low: −25%; High: +25%) | 13,830 | 7064 |
| RR of anxiety for CVD patients (Low: 1.49; High: 1.82) | 13,838 | 8912 |
| Health utility decrement due to anxiety (Low: 0.117; High: 0.195) | 13,914 | 9320 |
| Productivity loss of CVD (Low: −25%; High: +25%) † | 12,860 | 9466 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiao, B.; Zafari, Z.; Will, B.; Ruggeri, K.; Li, S.; Muennig, P. The Cost-Effectiveness of Lowering Permissible Noise Levels Around U.S. Airports. Int. J. Environ. Res. Public Health 2017, 14, 1497. https://doi.org/10.3390/ijerph14121497
Jiao B, Zafari Z, Will B, Ruggeri K, Li S, Muennig P. The Cost-Effectiveness of Lowering Permissible Noise Levels Around U.S. Airports. International Journal of Environmental Research and Public Health. 2017; 14(12):1497. https://doi.org/10.3390/ijerph14121497
Chicago/Turabian StyleJiao, Boshen, Zafar Zafari, Brian Will, Kai Ruggeri, Shukai Li, and Peter Muennig. 2017. "The Cost-Effectiveness of Lowering Permissible Noise Levels Around U.S. Airports" International Journal of Environmental Research and Public Health 14, no. 12: 1497. https://doi.org/10.3390/ijerph14121497





