Socioeconomic Inequalities in Health and Perceived Unmet Needs for Healthcare among the Elderly in Germany
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Socioeconomic Status
2.3. Health Problems
2.4. Unmet Healthcare Needs
2.5. Covariates
2.6. Statistical Methods
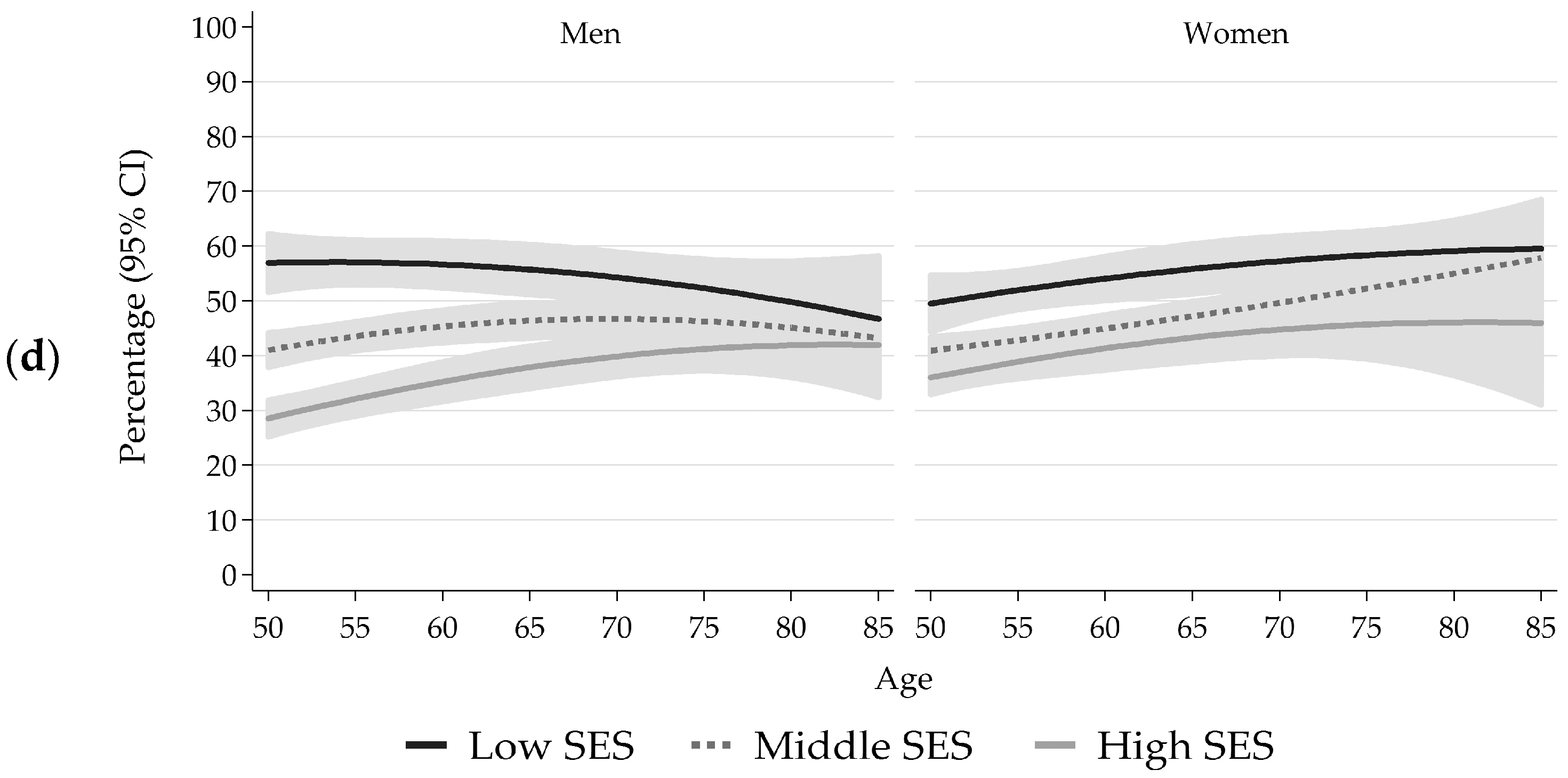
3. Results
4. Discussion
4.1. Strengths and Limitations
4.2. Comparison with Previous Findings and Possible Explanations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Pförtner, T.-K.; Richter, M. Getting social: Public Health’s increasing awareness of the social determinants of health. J. Public Health 2011, 19, 1–2. [Google Scholar] [CrossRef]
- Lampert, T.; Richter, M.; Schneider, S.; Spallek, J.; Dragano, N. Social inequality and health: Status and prospects of socio-epidemiological research in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2016, 59, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Marmot, M.G.; Wilkinson, R.G. Social Determinants of Health; Oxford University Press: Oxford, UK, 2006. [Google Scholar]
- Mackenbach, J.P.; Stirbu, I.; Roskam, A.-J.R.; Schaap, M.M.; Menvielle, G.; Leinsalu, M.; Kunst, A.E. Socioeconomic inequalities in health in 22 European countries. N. Engl. J. Med. 2008, 358, 2468–2481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chetty, R.; Stepner, M.; Abraham, S.; Lin, S.; Scuderi, B.; Turner, N.; Bergeron, A.; Cutler, D. The association between income and life expectancy in the United States, 2001–2014. JAMA 2016, 315, 1750–1766. [Google Scholar] [CrossRef] [PubMed]
- European Commission. Health Inequalities in the EU: Final Report of a Consortium. Consortium Lead: Sir Michael Marmot; European Commission Directorate—General for Health and Consumers: Brussels, Belgium, 2013. [Google Scholar]
- Lampert, T.; Kroll, L.E. Social differences in mortality and life expectancy. GBE Kompakt 2014, 5, 1–11. [Google Scholar]
- Bengtson, V.L.; Schaie, K.W. Handbook of Theories of Aging; Sringer: Heidelberg, Germany, 1999. [Google Scholar]
- Ben-Shlomo, Y.; Kuh, D. A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. Int. J. Epidemiol. 2002, 31, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Power, C.; Kuh, D. Life course development of unequal health. In Social Inequalities in Health: New Evidence and Policy Implications; Siegrist, J., Marmot, M., Eds.; Oxford University Press: Oxford, UK, 2006; pp. 27–53. [Google Scholar]
- Kuh, D.; Karunananthan, S.; Bergman, H.; Cooper, R. A life-course approach to healthy ageing: Maintaining physical capability. Proc. Nutr. Soc. 2014, 73, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Blane, D.; Netuveli, G.; Stone, J. The development of life course epidemiology. Rev. Epidemiol. Sante Publ. 2007, 55, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Shaw, B.A.; McGeever, K.; Vasquez, E.; Agahi, N.; Fors, S. Socioeconomic inequalities in health after age 50: Are health risk behaviors to blame? Soc. Sci. Med. 2014, 101, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Fors, S.; Thorslund, M. Enduring inequality: Educational disparities in health among the oldest old in Sweden 1992–2011. Int. J. Public Health 2015, 60, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Read, S.; Grundy, E.; Foverskov, E. Socio-economic position and subjective health and well-being among older people in Europe: A systematic narrative review. Aging Ment. Health 2016, 20, 529–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huisman, M.; Read, S.; Towriss, C.A.; Deeg, D.J.H.; Grundy, E. Socioeconomic inequalities in mortality rates in old age in the World Health Organization Europe region. Epidemiol. Rev. 2013, 35, 84–97. [Google Scholar] [CrossRef] [PubMed]
- Von dem Knesebeck, O.; Lüschen, G.; Cockerham, W.C.; Siegrist, J. Socioeconomic status and health among the aged in the United States and Germany: A comparative cross-sectional study. Soc. Sci Med. 2003, 57, 1643–1652. [Google Scholar] [CrossRef]
- Schöllgen, I.; Huxhold, O.; Tesch-Römer, C. Socioeconomic status and health in the second half of life: Findings from the German Ageing Survey. Eur. J. Ageing 2010, 7, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Demakakos, P.; Biddulph, J.P.; Bobak, M.; Marmot, M.G. Wealth and mortality at older ages: A prospective cohort study. J. Epidemiol. Community Health 2016, 70, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Von dem Knesebeck, O.; Vonneilich, N.; Lüdecke, D. Income and functional limitations among the aged in Europe: A trend analysis in 16 countries. J. Epidemiol. Community Health 2017, 71. [Google Scholar] [CrossRef] [PubMed]
- Mielck, A.; Kiess, R.; von dem Knesebeck, O.; Stirbu, I.; Kunst, A.E. Association between forgone care and household income among the elderly in five Western European countries: Analyses based on survey data from the SHARE-study. BMC Health Serv. Res. 2009, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- O’Rand, A.M.; Henretta, J.C. Age and Inequality: Diverse Pathways through Later Life; Westview Press: Boulder, CO, USA, 1999. [Google Scholar]
- Ross, C.E.; Wu, C.L. Education, age, and the cumulative advantage in health. J. Health Soc. Behav. 1996, 37, 104–120. [Google Scholar] [CrossRef] [PubMed]
- Herd, P. Do functional health inequalities decrease in old age? Educational status and functional decline among the 1931–1941 birth cohort. Res. Aging 2006, 28, 375–392. [Google Scholar] [CrossRef]
- Lynch, S.M. Cohort and life-course patterns in the relationship between education and health: A hierarchical approach. Demography 2003, 40, 309–331. [Google Scholar] [CrossRef] [PubMed]
- Leopold, L.; Engelhartdt, H. Education and physical health trajectories in old age. Evidence from the Survey of Health, Ageing and Retirement in Europe (SHARE). Int. J. Public Health 2013, 58, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Baeten, S.; Van Ourti, T.; van Doorslaer, E. The socioeconomic health gradient across the life cycle: What role for selective mortality and institutionalization? Soc. Sci. Med. 2013, 97, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Parker, M.G.; Ahacic, K.; Thorslund, M.; Lundberg, O. Socioeconomic status and health among elderly people in Sweden. Ann. N. Y. Acad. Sci. 1999, 896, 383–385. [Google Scholar] [CrossRef] [PubMed]
- Stolpe, S. Age-related social inequality in mortality. Gesundheitswesen 1997, 59, 242–247. [Google Scholar] [PubMed]
- Kröger, H.; Fritzell, J.; Hoffmann, R. The association of levels of and decline in grip strength in old age with trajectories of life course occupational position. PLoS ONE 2016, 11, e0155954. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Durden, E. Socioeconomic status and age trajectories of health. Soc. Sci. Med. 2007, 65, 2489–2502. [Google Scholar] [CrossRef] [PubMed]
- House, J.S.; Lantz, P.M.; Herd, P. Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ Changing Lives Study). J. Gerontol. B Psychol. Sci. Soc. Sci. 2005, 60, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Beckett, M. Converging health inequalities in later life: An artifact of mortality selection. J. Health Soc. Behav. 2000, 41, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Federal Statistical Office of Germany. Bevölkerung und Erwerbstätigkeit 2015. Fachserie 1: Reihe 1.3; Destatis: Wiesbaden, Germany, 2016.
- Kurth, B.-M.; Lange, C.; Kamtsiuris, P.; Hölling, H. Health monitoring at the Robert Koch Institute: Status and perspectives. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2009, 52, 557–570. [Google Scholar] [CrossRef] [PubMed]
- Lange, C.; Jentsch, F.; Allen, J.; Hoebel, J.; Kratz, A.L.; von der Lippe, E.; Müters, S.; Schmich, P.; Thelen, J.; Wetzstein, M.; et al. Data Resource Profile: German Health Update (GEDA)—The health interview survey for adults in Germany. Int. J. Epidemiol. 2015, 44, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Lange, C.; Finger, J.D.; Allen, J.; Born, S.; Hoebel, J.; Kuhnert, R.; Müters, S.; Thelen, J.; Schmich, P.; Varga, M.; et al. Implementation of the European Health Interview Survey (EHIS) into the German Health Update (GEDA). Arch. Public Health 2017, 75, 40. [Google Scholar] [CrossRef] [PubMed]
- BIK Regionen. Available online: http://www.bik-gmbh.de/produkte/regionen/index.html (accessed on 10 July 2017).
- Cox, L.H. A constructive procedure for unbiased controlled rounding. J. Am. Stat. Assoc. 1987, 82, 520–524. [Google Scholar] [CrossRef]
- American Association for Public Opinion Research. Standard Definitions—Final Dispositions of Case Codes and Outcome Rates for Surveys; Revised 2011; AAPOR: Deerfield, MA, USA, 2011. [Google Scholar]
- Lampert, T.; Kroll, L.E.; Müters, S.; Stolzenberg, H. Measurement of socioeconomic status in the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013, 56, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Lampert, T.; Kroll, L.E.; Müters, S.; Stolzenberg, H. Measurement of the socioeconomic status within the German Health Update 2009 (GEDA). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013, 56, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Brauns, H.; Scherer, S.; Steinmann, S. The CASMIN educational classification in international comparative research. In Advances in Cross-National Comparison: An European Working Book for Demographic and Socio-Economic Variables; Hoffmeyer-Zlotnik, J.H.P., Wolf, C., Eds.; Kluwer: New York, NY, USA, 2003; pp. 196–221. [Google Scholar]
- Ganzeboom, H.G.B.; De Graaf, P.M.; Treimann, D.J. A standard international socioeconomic index of occupational status. Soc. Sci. Res. 1992, 21, 1–56. [Google Scholar] [CrossRef]
- What Are Equivalence Scales? Available online: http://www.oecd.org/eco/growth/OECD-Note-EquivalenceScales.pdf (accessed on 16 November 2016).
- Eurostat. European Health Interview Survey (EHIS Wave 2): Methodological Manual, 2013th ed.; Publications Office of the European Union: Luxembourg, 2013. [Google Scholar]
- Cox, B.; van Oyen, H.; Cambois, E.; Jagger, C.; le Roy, S.; Robine, J.M.; Romieu, I. The reliability of the Minimum European Health Module. Int. J. Public Health 2009, 54, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Lungen, M.; Stollenwerk, B.; Messner, P.; Lauterbach, K.; Gerber, A. Waiting times for elective treatments according to insurance status: A randomized empirical study in Germany. Int. J. Equity Health 2008, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Graubard, B.I.; Korn, E.L. Predictive margins with survey data. Biometrics 1999, 55, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Mackenbach, J.P.; Kunst, A.E. Measuring the magnitude of socio-economic inequalities in health: An overview of available measures illustrated with two examples from Europe. Soc. Sci. Med. 1997, 44, 757–771. [Google Scholar] [CrossRef]
- Mackenbach, J.P.; Martikainen, P.; Menvielle, G.; de Gelder, R. The arithmetic of reducing relative and absolute inequalities in health: A theoretical analysis illustrated with European mortality data. J. Epidemiol. Community Health 2016, 70, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Gaertner, B.; Seitz, I.; Fuchs, J.; Busch, M.A.; Holzhausen, M.; Martus, P.; Scheidt-Nave, C. Baseline participation in a health examination survey of the population 65 years and older: Who is missed and why? BMC Geriatr. 2016, 16, 21. [Google Scholar] [CrossRef] [PubMed]
- Bowling, A. Mode of questionnaire administration can have serious effects on data quality. J. Public Health 2005, 27, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Hoebel, J.; von der Lippe, E.; Lange, C.; Ziese, T. Mode differences in a mixed-mode health interview survey among adults. Arch. Public Health 2014, 72, 46. [Google Scholar] [CrossRef] [PubMed]
- Schouten, B.; Cobben, F.; Bethlehem, J. Indicators for the representativeness of survey response. Surv. Methodol. 2009, 35, 101–113. [Google Scholar]
- Groves, R.M.; Peytcheva, E. The impact of nonresponse rates on nonresponse bias: A metaanalysis. Public Opin. Q. 2008, 72, 167–189. [Google Scholar] [CrossRef]
- Lampert, T.; Kroll, L.E.; von der Lippe, E.; Müters, S.; Stolzenberg, H. Socioeconomic status and health: Results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013, 56, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Geyer, S. Single indicator or index? Comparison of measures of social differentiation. Gesundheitswesen 2008, 70, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Bammann, K. Additive Sozialschichtindizes als Instrumente zur Beschreibung der sozialen Ungleichheit von Gesundheit: Untersuchung am Beispiel der Statusinkonsistenz. In Sozial-Epidemiologie; Mielck, A., Bloomfield, K., Eds.; Juventa: Weinheim, Germany, 2001; pp. 50–59. [Google Scholar]
- Geyer, S.; Hemström, O.; Peter, R.; Vågerö, D. Education, income, and occupational class cannot be used interchangeably in social epidemiology: Empirical evidence against a common practice. J. Epidemiol. Community Health 2006, 60, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, B.; Lampert, T. Socioeconomic factors and obesity. Dtsch. Arztebl. Int. 2010, 107, 517–522. [Google Scholar] [PubMed]
- Hoebel, J.; Richter, M.; Lampert, T. Social status and participation in health checks in men and women in Germany: Results from the German Health Update (GEDA), 2009 and 2010. Dtsch. Arztebl. Int. 2013, 110, 679–685. [Google Scholar] [PubMed]
- Blane, D.; Netuveli, G.; Bartley, M. Does quality of life at older ages vary with socioeconomic position? Sociology 2007, 41, 717–726. [Google Scholar] [CrossRef]
- Pongiglione, B.; De Stavola, B.L.; Ploubidis, G.B. A systematic literature review of studies analyzing inequalities in health expectancy among the older population. PLoS ONE 2015, 10, e0130747. [Google Scholar] [CrossRef] [PubMed]
- Thorslund, M.; Lundberg, O. Health and inequalities among the oldest old. J. Aging Health 1994, 6, 51–69. [Google Scholar] [CrossRef] [PubMed]
- Buttery, A.K.; Busch, M.A.; Gaertner, B.; Scheidt-Nave, C.; Fuchs, J. Prevalence and correlates of frailty among older adults: Findings from the German health interview and examination survey. BMC Geriatr. 2015, 15, 22. [Google Scholar] [CrossRef] [PubMed]
- Huisman, M.; Kunst, A.E.; Mackenbach, J.P. Socioeconomic inequalities in morbidity among the elderly: A European overview. Soc. Sci. Med. 2003, 57, 861–873. [Google Scholar] [CrossRef]
- Fors, S.; Modin, B.; Koupil, I.; Vågerö, D. Socioeconomic inequalities in circulatory and all-cause mortality after retirement: The impact of mid-life income and old-age pension. Evidence from the Uppsala Birth Cohort Study. J. Epidemiol. Community Health 2011, 66, e16. [Google Scholar] [CrossRef] [PubMed]
- Chandola, T.; Ferrie, J.; Sacker, A.; Marmot, M. Social inequalities in self reported health in early old age: Follow-up of prospective cohort study. BMJ 2007, 334, 990. [Google Scholar] [CrossRef] [PubMed]
- Avendano, M.; Jürges, H.; Mackenbach, J.P. Educational level and changes in health across Europe: Longitudinal results from SHARE. J. Eur. Soc. Policy 2009, 19, 301–316. [Google Scholar] [CrossRef]
- Henretta, J.C. Status attainment and status maintenance: A study of stratification in old age. Am. Sociol. Rev. 1976, 41, 981–992. [Google Scholar] [CrossRef]
- Virtanen, M.; Ferrie, J.E.; Batty, G.D.; Elovainio, M.; Jokela, M.; Vahtera, J.; Singh-Manoux, A.; Kivimaki, M. Socioeconomic and psychosocial adversity in midlife and depressive symptoms post retirement: A 21-year follow-up of the Whitehall II study. Am. J. Geriatr. Psychiatry 2015, 23, 99–109.e101. [Google Scholar] [CrossRef] [PubMed]
- Markides, K.S.; Machalek, R. Selective survival, aging and society. Arch. Gerontol. Geriatr. 1984, 3, 207–222. [Google Scholar] [CrossRef]
- Wing, S.; Manton, K.G.; Stallard, E.; Hames, C.G.; Tryoler, H.A. The black/white mortality crossover: Investigation in a community-based study. J. Gerontol. 1985, 40, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Mackenbach, J.P.; Looman, C.W.; Artnik, B.; Bopp, M.; Deboosere, P.; Dibben, C.; Kalediene, R.; Kovács, K.; Leinsalu, M.; Martikainen, P.; et al. ‘Fundamental causes’ of inequalities in mortality: An empirical test of the theory in 20 European populations. Sociol. Health Illn. 2017, 39, 1117–1133. [Google Scholar] [CrossRef] [PubMed]
- Roger, V.L. The heart failure epidemic. Int. J. Environ. Res. Public Health 2010, 7, 1807–1830. [Google Scholar] [CrossRef] [PubMed]
- Ward, A.; Payne, K.A.; Caro, J.J.; Heuschmann, P.U.; Kolominsky-Rabas, P.L. Care needs and economic consequences after acute ischemic stroke: The Erlangen Stroke Project. Eur. J. Neurol. 2005, 12, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Schneider, K.; Heise, M.; Heuschmann, P.; Berger, K. Situation of life and care in patients with a stroke. Nervenheilkunde 2009, 28, 114–118. [Google Scholar]
- Du, Y.; Heidemann, C.; Gösswald, A.; Schmich, P.; Scheidt-Nave, C. Prevalence and comorbidity of diabetes mellitus among non-institutionalized older adults in Germany: Results of the national telephone health interview survey ‘German Health Update (GEDA)’ 2009. BMC Public Health 2013, 13, 166. [Google Scholar] [CrossRef] [PubMed]
- McMunn, A.; Nazroo, J.; Breeze, E. Inequalities in health at older ages: A longitudinal investigation of the onset of illness and survival effects in England. Age Ageing 2009, 38, 181–187. [Google Scholar] [CrossRef] [PubMed]
- House, J.S.; Lepkowski, J.M.; Kinney, A.M.; Mero, R.P.; Kessler, R.C.; Herzog, A.R. The social stratification of aging and health. J. Health Soc. Behav. 1994, 35, 213–234. [Google Scholar] [CrossRef] [PubMed]
- Christensen, K.; Vaupel, J.W. Determinants of longevity: Genetic, environmental and medical factors. J. Intern. Med. 1996, 240, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Cylus, J.; Papanicolas, I. An analysis of perceived access to health care in Europe: How universal is universal coverage? Health Policy 2015, 119, 1133–1144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elstad, J.I. Income inequality and foregone medical care in Europe during The Great Recession: Multilevel analyses of EU-SILC surveys 2008–2013. Int. J. Equity Health 2016, 15, 101. [Google Scholar] [CrossRef] [PubMed]
- Detollenaere, J.; Hanssens, L.; Vyncke, V.; De Maeseneer, J.; Willems, S. Do we reap what we sow? Exploring the association between the strength of European primary healthcare systems and inequity in unmet need. PLoS ONE 2017, 12, e0169274. [Google Scholar] [CrossRef] [PubMed]
- Krůtilová, V. Unmet need for health care: A serious issue for European elderly? Procedia—Soc. Behav. Sci. 2016, 220, 217–225. [Google Scholar] [CrossRef]
- Litwin, H.; Sapir, E.V. Forgone health care due to cost among older adults in European countries and in Israel. Eur. J. Ageing 2009, 6, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Chaupain-Guillot, S.; Guillot, O. Health system characteristics and unmet care needs in Europe: An analysis based on EU-SILC data. Eur. J. Health Econ. 2015, 16, 781–796. [Google Scholar] [CrossRef] [PubMed]
- Allin, S.; Masseria, C. Unmet need as an indicator of health care access. Eurohealth 2009, 15, 7–9. [Google Scholar]
- Yamada, T.; Chen, C.C.; Murata, C.; Hirai, H.; Ojima, T.; Kondo, K.; Harris, J.R., 3rd. Access disparity and health inequality of the elderly: Unmet needs and delayed healthcare. Int. J. Environ. Res. Public Health 2015, 12, 1745–1772. [Google Scholar] [CrossRef] [PubMed]
- Fjær, E.L.; Stornes, P.; Borisova, L.V.; McNamara, C.L.; Eikemo, T.A. Subjective perceptions of unmet need for health care in Europe among social groups: Findings from the European social survey (2014) special module on the social determinants of health. Eur. J. Public Health 2017, 27, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Pfaff, H.; Pförtner, T.K. Contribution of health care research to establishing social equality in health and health care opportunities. Gesundheitswesen 2016, 78, 91–96. [Google Scholar] [PubMed]
- Walendzik, A.; Rabe-Menssen, C.; Lux, G.; Wasem, J.; Jahn, R. The health-care situation in outpatient psychiatry: Results of a survey among members of the Germany Association of Psychotherapists. Gesundheitswesen 2014, 76, 135–146. [Google Scholar] [PubMed]
- Jordan, S.; Hoebel, J. Health literacy of adults in Germany: Findings from the German Health Update (GEDA) study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2015, 58, 942–950. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, K.L.; Scott, S.E.; Wardle, J. Applying symptom appraisal models to understand sociodemographic differences in responses to possible cancer symptoms: A research agenda. Br. J. Cancer 2015, 112, 27–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terraneo, M. Inequities in health care utilization by people aged 50+: Evidence from 12 European countries. Soc. Sci. Med. 2015, 126, 154–163. [Google Scholar] [CrossRef] [PubMed]

| Men | Women | Total | |
|---|---|---|---|
| (n = 5702) | (n = 6109) | (n = 11,811) | |
| Age, years | |||
| Mean ± SD | 63.8 ± 9.7 | 64.8 ± 9.4 | 64.3 ± 9.6 |
| Age group, % (n) | |||
| 50–64 years | 55.8 (2952) | 51.5 (3466) | 53.6 (6418) |
| 65–85 years | 44.2 (2750) | 48.5 (2643) | 46.4 (5393) |
| Socioeconomic status, % (n) | |||
| Low | 20.9 (1083) | 23.7 (1198) | 22.4 (2281) |
| Medium | 55.8 (2884) | 63.2 (3626) | 59.7 (6510) |
| High | 23.3 (1724) | 13.1 (1272) | 18.0 (2996) |
| Health problems, % (n) | |||
| SRH (less than good) | 43.0 (2344) | 43.4 (2443) | 43.2 (4787) |
| Global activity limitations | 34.1 (1857) | 33.0 (1864) | 33.5 (3721) |
| Walking limitations | 18.6 (1019) | 24.2 (1251) | 21.6 (2270) |
| Low back complaints | 45.4 (2372) | 48.8 (2771) | 47.2 (5143) |
| Perceived unmet need, % 1 (n) | |||
| Medical care | 3.1 (142) | 4.0 (208) | 3.6 (350) |
| Dental care | 8.2 (381) | 8.0 (427) | 8.1 (808) |
| Prescribed medicines | 2.7 (125) | 3.2 (159) | 3.0 (284) |
| Mental healthcare | 1.7 (55) | 2.4 (83) | 2.1 (138) |
| Residential region, % (n) | |||
| West | 78.7 (4183) | 78.3 (4534) | 78.5 (8717) |
| East | 21.3 (1519) | 21.7 (1575) | 21.5 (3094) |
| Urbanization, % (n) | |||
| Rural area | 33.6 (1921) | 33.5 (2044) | 33.6 (3965) |
| Urban area | 66.4 (3781) | 66.5 (4065) | 66.4 (7846) |
| Immigrant status, % (n) | |||
| Not immigrated | 93.6 (5304) | 93.7 (5661) | 93.6 (10,965) |
| Immigrated | 6.4 (352) | 6.3 (396) | 6.4 (748) |
| Type of health insurance, % (n) | |||
| Statutory | 72.6 (3931) | 82.8 (4799) | 77.9 (8730) |
| Private | 25.9 (1552) | 16.5 (1120) | 21.0 (2672) |
| Other | 1.5 (77) | 0.8 (44) | 1.1 (121) |
| Self-Rated Health (Less Than Good) | Global Activity Limitations | Walking Limitations | Low Back Complaints | |||||
|---|---|---|---|---|---|---|---|---|
| % | OR 1 (95% CI) | % | OR 1 (95% CI) | % | OR 1 (95% CI) | % | OR 1 (95% CI) | |
| Men (50–64 years) | 38.0 | 30.6 | 11.8 | 44.2 | ||||
| Low SES | 58.4 | 5.12 (3.92–6.70) *** | 48.1 | 4.85 (3.69–6.38) *** | 25.4 | 7.64 (4.94–11.81) *** | 58.1 | 2.61 (1.98–3.46) *** |
| Middle SES | 37.8 | 2.23 (1.79–2.79) *** | 30.7 | 2.26 (1.78–2.87) *** | 10.1 | 2.50 (1.27–3.84) *** | 43.8 | 1.50 (1.22–1.84) *** |
| High SES (ref.) | 21.6 | 1.00 | 16.5 | 1.00 | 4.5 | 1.00 | 34.0 | 1.00 |
| Men (65–85 years) | 49.4 | 38.4 | 27.3 | 47.0 | ||||
| Low SES | 62.3 | 3.05 (2.33–4.00) *** | 44.9 | 1.76 (1.34–2.32) *** | 34.2 | 2.27 (1.66–3.11) *** | 53.4 | 1.70 (1.30–2.23) *** |
| Middle SES | 49.9 | 1.86 (1.46–2.36) *** | 38.7 | 1.39 (1.11–1.74) ** | 27.8 | 1.67 (1.27–2.21) *** | 47.3 | 1.36 (1.09–1.68) ** |
| High SES (ref.) | 34.7 | 1.00 | 31.5 | 1.00 | 19.2 | 1.00 | 39.9 | 1.00 |
| p-value for SES × age group | (0.028) | (<0.001) | (<0.001) | (0.076) | ||||
| Women (50–64 years) | 35.1 | 28.2 | 14.4 | 45.7 | ||||
| Low SES | 52.3 | 3.71 (2.79–4.92) *** | 39.2 | 2.54 (1.93–3.35) *** | 25.9 | 4.31 (2.92–6.37) *** | 55.2 | 2.00 (1.56–2.55) *** |
| Middle SES | 33.1 | 1.74 (1.39–2.18) *** | 27.1 | 1.50 (1.20–1.87) *** | 12.8 | 1.91 (1.34–2.72) *** | 44.8 | 1.31 (1.08–1.57) ** |
| High SES (ref.) | 22.3 | 1.00 | 19.7 | 1.00 | 7.1 | 1.00 | 37.8 | 1.00 |
| Women (65–85 years) | 52.4 | 38.2 | 34.7 | 52.3 | ||||
| Low SES | 63.7 | 2.91 (2.05–4.12) *** | 46.2 | 1.81 (1.24–2.64) ** | 45.6 | 2.21 (1.55–3.15) *** | 56.5 | 1.42 (1.02–1.98) * |
| Middle SES | 49.5 | 1.73 (1.27–2.36) *** | 35.8 | 1.23 (0.89–1.71) | 31.3 | 1.34 (0.96–1.86) | 51.2 | 1.13 (0.85–1.51) |
| High SES (ref.) | 34.6 | 1.00 | 29.8 | 1.00 | 23.5 | 1.00 | 46.9 | 1.00 |
| p-value for SES × age group | (0.104) | (0.015) | (<0.001) | (0.231) | ||||
| Unmet Need: Medical Care | Unmet Need: Dental Care | Unmet Need: Prescribed Medicines | Unmet Need: Mental Healthcare | |||||
|---|---|---|---|---|---|---|---|---|
| % | OR 1 (95% CI) | % | OR 1 (95% CI) | % | OR 1 (95% CI) | % | OR 1 (95% CI) | |
| Men (50–64 years) | 3.2 | 9.6 | 2.6 | 2.4 | ||||
| Low SES | 6.5 | 2.65 (1.13–6.24) * | 12.5 | 1.91 (1.13–3.22) * | 5.0 | 6.40 (2.09–19.62) ** | 5.1 | 11.75 (2.35–58.72) ** |
| Middle SES | 2.2 | 0.84 (0.40–1.75) | 10.3 | 1.72 (1.09–2.73) * | 2.5 | 3.24 (1.21–8.68) * | 1.7 | 3.92 (0.82–18.65) |
| High SES (ref.) | 2.5 | 1.00 | 5.7 | 1.00 | 0.8 | 1.00 | 0.6 | 1.00 |
| Men (65–85 years) | 2.9 | 6.5 | 2.9 | 1.0 | ||||
| Low SES | 4.6 | 3.83 (1.11–13.25) * | 8.5 | 4.50 (2.19–9.25) *** | 5.3 | 7.83 (2.13–28.75) ** | 0.8 | 0.87 (0.13–5.73) |
| Middle SES | 3.0 | 2.54 (0.78–8.29) | 7.4 | 4.18 (2.18–8.01) *** | 2.5 | 2.75 (0.95–7.99) | 1.1 | 1.23 (0.31–4.94) |
| High SES (ref.) | 0.8 | 1.00 | 1.6 | 1.00 | 0.9 | 1.00 | 0.9 | 1.00 |
| p-value for SES × age group | (0.131) | (0.003) | (0.760) | (0.058) | ||||
| Women (50–64 years) | 5.4 | 10.6 | 3.8 | 3.1 | ||||
| Low SES | 10.2 | 4.25 (2.28–7.94) *** | 16.9 | 2.48 (1.60–3.84) *** | 7.5 | 3.79 (1.67–8.59) ** | 6.1 | 3.43 (1.45–8.13) ** |
| Middle SES | 4.6 | 1.85 (1.04–3.29) * | 9.7 | 1.34 (0.89–2.00) | 3.2 | 1.69 (0.79–3.59) | 2.2 | 1.11 (0.49–2.50) |
| High SES (ref.) | 2.7 | 1.00 | 6.4 | 1.00 | 1.5 | 1.00 | 2.1 | 1.00 |
| Women (65–85 years) | 2.6 | 5.0 | 2.6 | 1.5 | ||||
| Low SES | 4.1 | 2.07 (0.59–7.21) | 7.5 | 2.15 (0.68–6.77) | 4.6 | 4.45 (1.05–18.85) * | 1.5 | 0.72 (0.12–4.53) |
| Middle SES | 1.8 | 0.98 (0.29–3.35) | 4.0 | 1.15 (0.38–3.51) | 1.9 | 2.14 (0.50–9.08) | 1.6 | 1.08 (0.19–6.21) |
| High SES (ref.) | 2.3 | 1.00 | 3.3 | 1.00 | 0.8 | 1.00 | 0.9 | 1.00 |
| p-value for SES × age group | (0.258) | (0.696) | (0.507) | (0.392) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoebel, J.; Rommel, A.; Schröder, S.L.; Fuchs, J.; Nowossadeck, E.; Lampert, T. Socioeconomic Inequalities in Health and Perceived Unmet Needs for Healthcare among the Elderly in Germany. Int. J. Environ. Res. Public Health 2017, 14, 1127. https://doi.org/10.3390/ijerph14101127
Hoebel J, Rommel A, Schröder SL, Fuchs J, Nowossadeck E, Lampert T. Socioeconomic Inequalities in Health and Perceived Unmet Needs for Healthcare among the Elderly in Germany. International Journal of Environmental Research and Public Health. 2017; 14(10):1127. https://doi.org/10.3390/ijerph14101127
Chicago/Turabian StyleHoebel, Jens, Alexander Rommel, Sara Lena Schröder, Judith Fuchs, Enno Nowossadeck, and Thomas Lampert. 2017. "Socioeconomic Inequalities in Health and Perceived Unmet Needs for Healthcare among the Elderly in Germany" International Journal of Environmental Research and Public Health 14, no. 10: 1127. https://doi.org/10.3390/ijerph14101127






