The Role of Body Adiposity Index in Determining Body Fat Percentage in Colombian Adults with Overweight or Obesity
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Sample Population
2.2. Procedures
2.3. Ethics Statement
2.4. Data Analysis
3. Results
3.1. Descriptive Characteristics
3.2. Correlation between BF% Determined by BAI and Different Variables
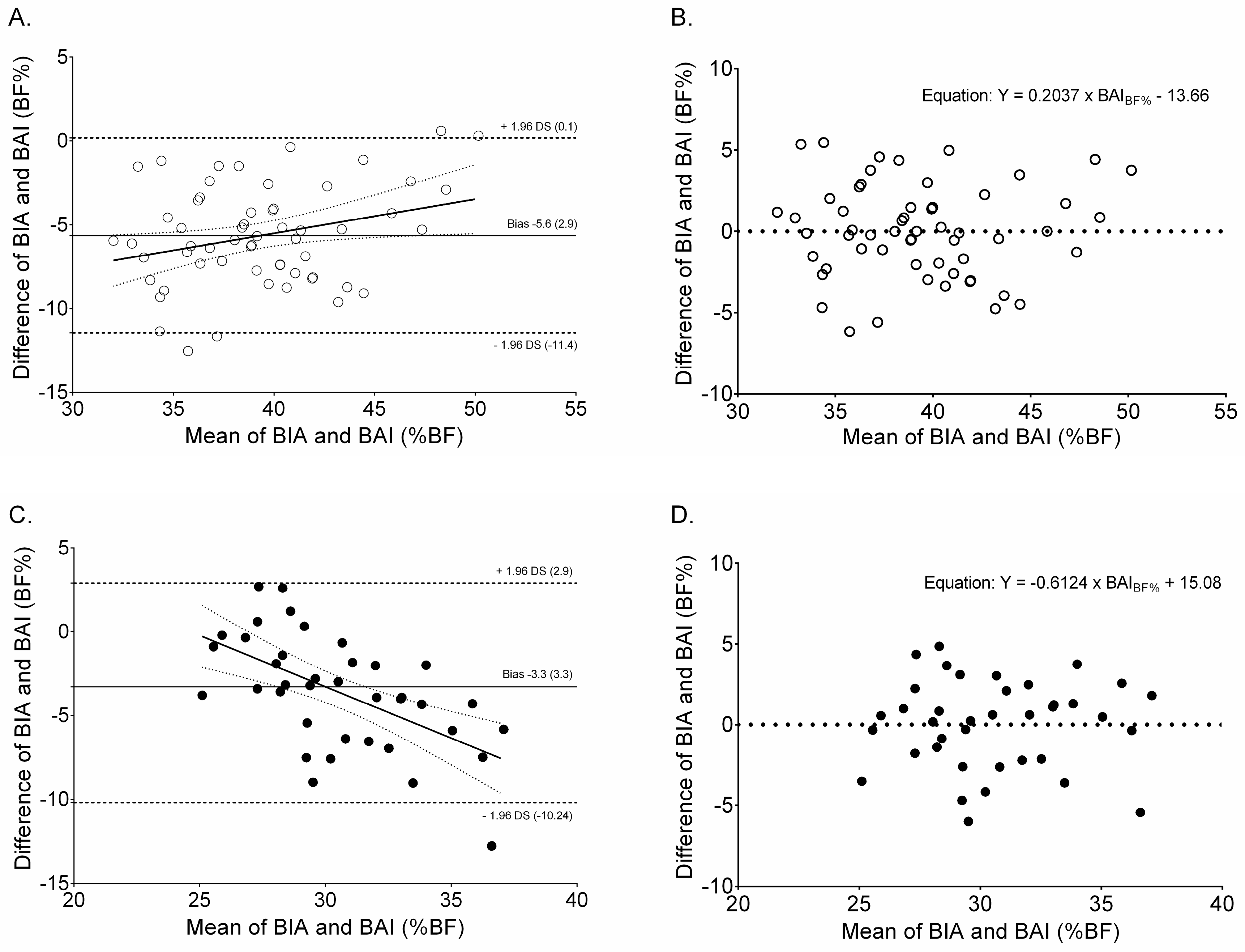
3.3. Fat Mass by BIA and BAI According to Distinct Levels of Adiposity by Sex
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| BAI | Body adiposity index |
| BIA | Bioelectrical impedance analysis |
| BF% | Body fat percentage |
| BMI | Body mass index |
| DXA | Dual-energy X-ray absorptiometry |
| KIDMED Index | Adherence to the Mediterranean index |
| WC | Waist circumference |
| WHtR | Waist-to-height ratio |
| pc | Lin’s concordance correlation coefficient |
References
- Bhupathiraju, S.N.; Hu, F.B. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ. Res. 2016, 118, 1723–1735. [Google Scholar] [CrossRef] [PubMed]
- Booth, A.; Magnuson, A.; Fouts, J.; Foster, M.T. Adipose tissue: An endocrine organ playing a role in metabolic regulation. Horm. Mol. Biol Clin. Investig. 2016, 26, 25–42. [Google Scholar] [CrossRef] [PubMed]
- Smitka, K.; Marešová, D. Adipose tissue as an endocrine organ: An update on pro-inflammatory and anti-inflammatory microenvironment. Prague Med. Rep. 2015, 116, 87–111. [Google Scholar] [CrossRef] [PubMed]
- Maddaloni, E.; Cavallari, I.; De Pascalis, M.; Keenan, H.; Park, K.; Manfrini, S.; Buzzetti, R.; Patti, G.; Di Sciascio, G.; Pozzilli, P. Relation of body circumferences to cardiometabolic disease in overweight-obese subjects. Am. J. Cardiol. 2016, 118, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Guh, D.P.; Zhang, W.; Bansback, N.; Amarsi, Z.; Birmingham, C.L.; Anis, A.H. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 2009, 9, 88. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Gallagher, D. Assessment methods in human body composition. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Correa-Bautista, J.E.; González-Ruíz, K.; Vivas, A.; García-Hermoso, A.; Triana-Reina, H.R. Predictive validity of the body adiposity index in overweight and obese adults using dual-energy X-ray absorptiometry. Nutrients 2016, 8, 737. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.C.; Guarnotta, V.; Giordano, C. Body composition assessment for the definition of cardiometabolic risk. J. Endocrinol. Investg. 2013, 36, 537–543. [Google Scholar]
- Bergman, R.N.; Stefanovski, D.; Buchanan, T.A.; Sumner, A.E.; Reynolds, J.C.; Sebring, N.G.; Xiang, A.H.; Watanabe, R.M. A better index of body adiposity. Obesity 2011, 19, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Geliebter, A.; Atalayer, D.; Flancbaum, L.; Gibson, C.D. Comparison of body adiposity index (BAI) and BMI with estimations of % body fat in clinically severe obese women. Obesity 2013, 21, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Bernhard, A.B.; Scabim, V.M.; Serafim, M.P.; Gadducci, A.V.; Santo, M.A.; de Cleva, R. Modified body adiposity index for body fat estimation in severe obesity. J. Hum. Nutr. Diet. 2017, 30, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Ezeukwu, A.O.; Ezeoranu, C.G.; Egwuonwu, A.V.; Ugwoke, U.M.; Ekechukwu, N.E.; Nwankwo, M.J. Comparison of body fat percentages in Nigerian obese females using field methods. J. Health Sci. 2015, 5, 18–23. [Google Scholar]
- Silva, M.I.; Vale, B.S.; Lemos, C.C.; Torres, M.R.; Bregman, R. Body adiposity index assesses body fat with high accuracy in nondialyzed chronic kidney disease patients. Obesity 2013, 21, 546–552. [Google Scholar] [CrossRef] [PubMed]
- García, A.I.; Niño-Silva, L.A.; González-Ruíz, K.; Ramírez-Vélez, R. Body adiposity index as marker of obesity and cardiovascular risk in adults from Bogotá, Colombia. Endocrinol. Nutr. 2015, 62, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Fuente-Martín, E.; Argente-Arizón, P.; Ros, P.; Argente, J.; Chowen, J.A. Sex differences in adipose tissue: It is not only a question of quantity and distribution. Adipocyte 2013, 2, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, D.; Visser, M.; Sepúlveda, D.; Pierson, R.N.; Harris, T.; Heymsfield, S.B. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am. J. Epidemiol. 1996, 143, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Sato, S.; Demura, S.; Kitabayashi, T.; Noguchi, T. Segmental body composition assessment for obese Japanese adults by single-frequency bioelectrical impedance analysis with 8-point contact electrodes. J. Physiol. Anthropol. 2007, 26, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Correa-Bautista, J.E.; González-Ruíz, K.; Vivas, A.; Triana-Reina, H.R.; Martínez-Torres, J.; Prieto-Benavides, D.H.; Carrillo, H.A.; Ramos-Sepúlveda, J.A.; Villa-González, E. Body Adiposity Index performance in estimating body fat percentage in Colombian college students: Findings from the FUPRECOL-Adults Study. Nutrients 2017, 9, 40. [Google Scholar] [CrossRef] [PubMed]
- Segheto, W.; Coelho, F.A.; Guimarães da Silva, C.D.; Hallal, P.C.; Marins, J.C.; Ribeiro, A.Q.; Pessoa, M.C.; Morais, S.H.; Longo, G.Z. Validity of body adiposity index in predicting body fat in Brazilian adults. Obesity 2017, 29. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Jaramillo, P.; Lahera, V.; Lopez-Lopez, J. Epidemic of cardiometabolic diseases: A Latin American point of view. Ther. Adv. Cardiovasc. Dis. 2011, 5, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Parra, D.C.; Iannotti, L.; Gomez, L.F.; Pachón, H.; Haire-Joshu, D.; Sarmiento, O.L.; Kuhlmann, A.S.; Brownson, R.C. The nutrition transition in Colombia over a decade: A novel household classification system of anthropometric measures. Arch. Public Health 2015, 73, 12. [Google Scholar] [CrossRef] [PubMed]
- Cetin, D.; Lessig, B.A.; Nasr, E. Comprehensive evaluation for obesity: Beyond Body Mass Index. J. Am. Osteopath. Assoc. 2016, 116, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Kahn, H.S.; Bullard, K.M. Beyond Body Mass Index: Advantages of abdominal measurements for recognizing cardiometabolic disorders. Am. J. Med. 2016, 129, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Johnson Stoklossa, C.A.; Forhan, M.; Padwal, R.S.; Gonzalez, M.C.; Prado, C.M. Practical considerations for body composition assessment of adults with class II/III obesity using bioelectrical impedance analysis or dual-energy X-ray absorptiometry. Curr. Obes. Rep. 2016, 5, 389–396. [Google Scholar] [CrossRef] [PubMed]
- González-Ruíz, K.; Correa-Bautista, J.E.; Ramírez-Vélez, R. Evaluation of the body adiposity index in predicting percentage body fat among Colombian adults. Nutr. Hosp. 2015, 32, 55–60. [Google Scholar] [PubMed]
- Ramírez-Vélez, R.; Hernandez, A.; Castro, K.; Tordecilla-Sanders, A.; González-Ruíz, K.; Correa-Bautista, J.E.; Izquierdo, M.; García-Hermoso, A. High intensity interval- vs. resistance or combined-training for improving cardiometabolic health in overweight adults (Cardiometabolic HIIT-RT Study): Study protocol for a randomised controlled trial. Trials 2016, 17, 298. [Google Scholar] [CrossRef] [PubMed]
- Marfell-Jones, M.; Olds, T.; Stewart, A. International Standards for Anthropometric Assessment; ISAK: Potchefstroom, South Africa, 2006. [Google Scholar]
- World Health Organization. Obesity: Preventing and managing the global epidemic. In Proceedings of the Report of a WHO Consultation on Obesity, Geneva, Switzerland, 3–5 June 1997; WHO: Geneva, Switzerland, 1997. [Google Scholar]
- Sandercock, G.R.; Lobelo, F.; Correa-Bautista, J.E.; Tovar, G.; Cohen, D.D.; Knies, G.; Ramírez-Vélez, R. The relationship between socioeconomic status, family income, and measures of muscular and cardiorespiratory fitness in Colombian schoolchildren. J. Pediatr. 2017, 185. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, R.; Gerber, M. Evaluating and adapting the Mediterranean diet for non-Mediterranean populations: A critical appraisal. Nutr. Rev. 2013, 71, 573–584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaki, M.E.; Kamal, S.; Reyad, H.; Yousef, W.; Hassan, N.; Helwa, I.; Kholoussi, S. The validity of body adiposity indices in predicting metabolic syndrome and its components among Egyptian women. Open Access Maced. J. Med. Sci. 2016, 4, 25–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freedman, D.S.; Thornton, J.C.; Pi-Sunyer, F.X.; Heymsfield, S.B.; Wang, J.; Pierson, R.N., Jr.; Blanck, H.M.; Gallagher, D. The body adiposity index (hip circumference ÷ height(1.5)) is not a more accurate measure of adiposity than is BMI, waist circumference, or hip circumference. Obesity 2012, 20, 2438–2444. [Google Scholar] [CrossRef] [PubMed]
- Johnson, W.; Chumlea, W.C.; Czerwinski, S.A.; Demerath, E.W. Concordance of the recently published body adiposity index with measured body fat percent in European-American adults. Obesity 2012, 20, 900–903. [Google Scholar] [CrossRef] [PubMed]
- Appelhans, B.M.; Kazlauskaite, R.; Karavolos, K.; Janssen, I.; Kravitz, H.M.; Dugan, S.; Powell, L.H. How well does the body adiposity index capture adiposity change in midlife women? The SWAN fat patterning study. Am. J. Hum. Biol. 2012, 24, 866–869. [Google Scholar] [CrossRef] [PubMed]
- Verdich, C.; Barbe, P.; Petersen, M.; Grau, K.; Ward, L.; Macdonald, I.; Sørensen, T.I.; Oppert, J.M. Changes in body composition during weight loss in obese subjects in the NUGENOB study: Comparison of bioelectrical impedance vs. dual-energy X-ray absorptiometry. Diabetes Metab. 2011, 37, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Aslam, M.; Eckhauser, A.W.; Dorminy, C.A.; Dosset, C.M.; Choi, L.; Buchowski, M.S. Assessing body fat changes during moderate weight loss with anthropometry and bioelectrical impedance. Obes. Res. Clin. Pract. 2009, 3, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Beeson, W.L.; Batech, M.; Schultz, E.; Salto, L.; Firek, A.; Deleon, M.; Balcazar, H.; Cordero-Macintyre, Z. Comparison of body composition by bioelectrical impedance analysis and dual-energy X-ray absorptiometry in Hispanic diabetics. Int. J. Body Compos. Res. 2010, 8, 45–50. [Google Scholar] [PubMed]
- Lohman, T.G. Advances in Body Composition Assessment; Human Kinetics Publisher: Champaign, IL, USA, 1992. [Google Scholar]
- Kuhn, P.C.; Vieira-Filho, J.P.; Franco, L.; Dal Fabbro, A.; Franco, L.J.; Moises, R.S. Evaluation of body adiposity index (BAI) to estimate percent body fat in an indigenous population. Clin. Nutr. 2014, 33, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Bennasar-Veny, M.; Lopez-Gonzalez, A.A.; Tauler, P.; Cespedes, M.L.; Vicente-Herrero, T.; Yanez, A.; Aguilo, A. Body adiposity index and cardiovascular health risk factors in Caucasians: A comparison with the body mass index and others. PLoS ONE 2013, 8, e63999. [Google Scholar] [CrossRef] [PubMed]
- McRae, M.P. Male and female differences in variability with estimating body fat composition using skinfold calipers. J. Chiropr. Med. 2010, 9, 157–161. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 96) | Women (n = 58) | Men (n = 38) | p Value |
|---|---|---|---|---|
| Antropometric and body composition | ||||
| Age (years) | 39.9 (7.0) | 40.6 (7.5) | 38.8 (6.1) | 0.228 |
| Height (cm) | 162.9 (8.1) | 157.9 (5.3) | 170.6 (5.1) | <0.001 |
| Body mass (kg) | 80.2 (12.2) | 74.8 (9.4) | 88.3 (11.4) | <0.001 |
| Waist circumference (cm) | 92.6 (9.4) | 88.1 (7.9) | 99.5 (7.0) | <0.001 |
| Hip circumference (cm) | 106.5 (7.8) | 108.1 (8.6) | 104.0 (5.8) | 0.012 |
| WHtR | 0.57 (0.05) | 0.56 (0.06) | 0.58 (0.04) | 0.016 |
| BIA-BF% | 38.3 (6.4) | 42.2 (4.1) | 32.4 (4.4) | <0.001 |
| BAI-BF% | 33.4 (5.6) | 36.5 (4.9) | 28.7 (2.6) | <0.001 |
| Adiposity levels (BIA-BF%) n [%] | ||||
| 20.1 to 30.0 | 6 [[6.2] | 0 [[0.0] | 6 [[15.7] | <0.001 |
| 30.1 to 40.0 | 44 [[45.8] | 15 [[25.8] | 29 [[76.3] | <0.001 |
| >40.1 | 46 [[47.9] | 43 [[74.1] | 3 [[10.5] | <0.001 |
| Nutricional status | ||||
| BMI (kg/m2) | 30.1 (3.5) | 30.0 (3.8) | 30.2 (2.9) | 0.811 |
| BMI ≥ 30 (kg/m2) n [%] | 45 [[46.9] | 28 [[48.3] | 17 [[44.7] | 0.734 |
| Socioeconomic status n [%] | ||||
| Low-middle | 59 [[61.5] | 37 [[63.8] | 22 [[57.9] | 0.669 |
| Middle-high | 37 [[38.5] | 21 [[36.2] | 16 [[42.1] | 0.562 |
| KIDMED Index n [%] | ||||
| Low diet quality | 10 [[10.4] | 4 [[6.9] | 6 [[15.8] | 0.311 |
| Needs improvement | 50 [[52.1] | 30 [[51.7] | 20 [[52.6] | 0.317 |
| Optimal adherence | 36 [[37.5] | 24 [[41.1] | 12 [[31.6] | 0.162 |
| KIDMED Index | 6.7 (2.2) | 7.0 (2.2) | 6.2 (2.2) | 0.093 |
| Characteristics | Women (n = 58) | Men (n = 38) | ||
|---|---|---|---|---|
| BAI-BF% | 0.793 * | 0.773 *┼ | 0.638 * | 0.697 *┼ |
| Body mass (kg) | 0.631 * | 0.747 *┼ | 0.415 * | 0.737 *┼ |
| Waist circumference (cm) | 0.630 * | 0.651 *┼ | 0.373 * | 0.751 *┼ |
| Hip circumference (cm) | 0.822 * | 0.777 *┼ | 0.682 * | 0.790 *┼ |
| WHtR | 0.732 * | 0.635 *┼ | 0.621 * | 0.793 *┼ |
| BMI (kg/m2) | 0.886 * | 0.826 *┼ | 0.728 * | 0.846 *┼ |
| KIDMED Index | −0.148 | - | −0.061 | - |
| Characteristics | Women | Men | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | BAI-BF% | BIA-BF% | p Value | Difference between Measures (95% CI) | ρc (95% CI) | N | BIA-BF% | BAI-BF% | p Value | Difference between Measures (95% CI) | ρc (95% CI) | |
| BF% | 58 | 36.5 (4.9) | 42.2 (4.1) | <0.001 | −5.6 (−6.4 to −4.8) | 0.877 (0.655 to 0.864) * | 38 | 28.7 (2.6) | 32.4 (4.4) | <0.001 | −3.6 (−4.7 to −2.5) | 0.719 (0.458 to 0.854) * |
| Adiposity Levels (BF% by BIA) | ||||||||||||
| 20.1 to 30.0 | - | - | - | - | - | - | 6 | 26.8 (2.6) | 27.4 (1.9) | 0.368 | −0.5 (−2.8 to 1.8) | 0.384 (-0-443 to 0.858) |
| 30.1 to 40.0 | 15 | 33.4 (2.6) | 38.1 (2.5) | <0.001 | −4.4 (−6.4 to −2.9) | 0.469 (−0.655 to 0.829) * | 29 | 28.6 (2.1) | 32.5 (3.2) | <0.001 | −3.9 (−5.0 to −2.8) | 0.651 (0.235 to 0.841) * |
| >40.1 | 43 | 37.8 (4.8) | 43.7 (3.4) | <0.001 | −5.8 (−6.7 to −4.9) | 0.859 (0.738 to 0.924) * | 3 | 32.4 (1.6) | 39.5 (3.3) | 0.052 | −7.0 (−14.1 to 0.08) | −0.455 (−0.953 to 0.705) |
| Study | Sample | Age (Years) | Device | Agreement between Measurement Methods/Bias | Main Finding |
|---|---|---|---|---|---|
| Present study | 96 subjects with overweight and obesity | Mean age | Tetrapolar frequency | Bland-Altman plots | Overall, BAI underestimated % BF |
| 39.9 ± 7.0 | Systemic bias −4.8% | ||||
| Geliebter et al. [10] | 19 pre-bariatric surgery non-diabetic women with clinically severe obesity | Mean age | Tetrapolar frequency | Bland-Altman plots | BAI underestimated BF% |
| 32.6 ± 7.7 | Systemic bias 2.2% | ||||
| Bernhard et al. [11] | 240 patients with severe obesity | Mean age | A single-frequency | Intraclass correlation | The two methods were similar according to the intraclass correlation (0.74; 95% confidence interval = 0.68 to 0.79) |
| 44.1 ± 11.1 | |||||
| Ezeukwu et al. [12] | 30 women with obesity | Mean age | A single-frequency | Bland-Altman plots | Overall, BAI underestimated BF% |
| 22.8 ± 3.3 | Systemic bias 15.0% | ||||
| Ramírez-Vélez et al. [18] | 903 apparently healthy persons and a sub-sample with overweight or obesity | Mean age | Tetrapolar frequency | Bland-Altman plots | Overall, BAI overestimated BF%, in overweight subjects the BAI overestimated BF%, and obese group the BAI underestimated BF% for both sexes |
| 21.4 ± 3.3 | Systemic bias 6.0% |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramírez-Vélez, R.; Correa-Bautista, J.E.; González-Ruíz, K.; Tordecilla-Sanders, A.; García-Hermoso, A.; Schmidt-RioValle, J.; González-Jiménez, E. The Role of Body Adiposity Index in Determining Body Fat Percentage in Colombian Adults with Overweight or Obesity. Int. J. Environ. Res. Public Health 2017, 14, 1093. https://doi.org/10.3390/ijerph14101093
Ramírez-Vélez R, Correa-Bautista JE, González-Ruíz K, Tordecilla-Sanders A, García-Hermoso A, Schmidt-RioValle J, González-Jiménez E. The Role of Body Adiposity Index in Determining Body Fat Percentage in Colombian Adults with Overweight or Obesity. International Journal of Environmental Research and Public Health. 2017; 14(10):1093. https://doi.org/10.3390/ijerph14101093
Chicago/Turabian StyleRamírez-Vélez, Robinson, Jorge Enrique Correa-Bautista, Katherine González-Ruíz, Alejandra Tordecilla-Sanders, Antonio García-Hermoso, Jacqueline Schmidt-RioValle, and Emilio González-Jiménez. 2017. "The Role of Body Adiposity Index in Determining Body Fat Percentage in Colombian Adults with Overweight or Obesity" International Journal of Environmental Research and Public Health 14, no. 10: 1093. https://doi.org/10.3390/ijerph14101093





