Tempo-Spatial Variations of Ambient Ozone-Mortality Associations in the USA: Results from the NMMAPS Data
Abstract
:1. Introduction
2. Experimental Section
2.1. Study Setting
2.2. Data Collection
2.3. Statistical Analysis
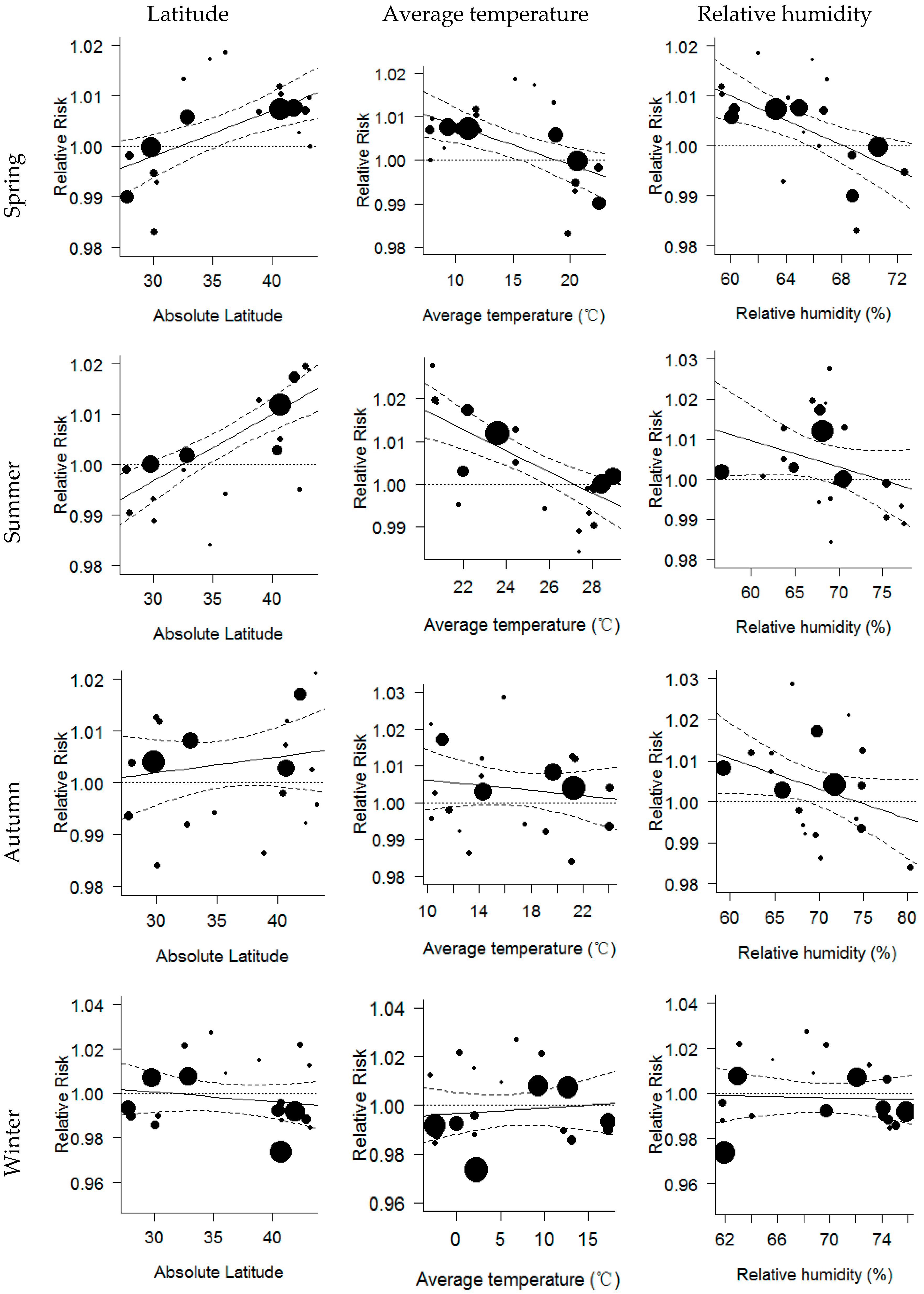
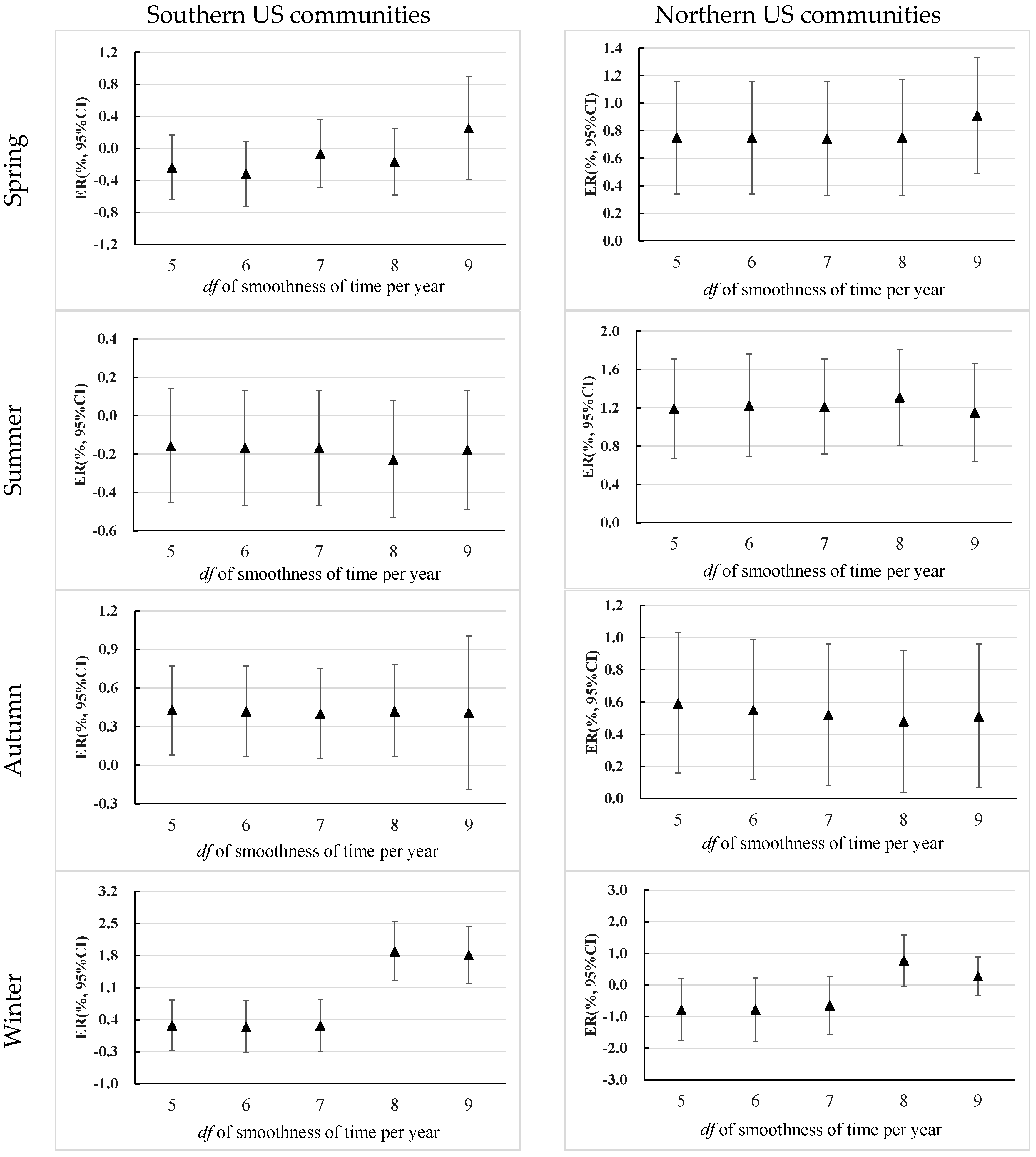
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wang, T.; Wei, X.; Ding, A.; Poon, C.; Lam, K.; Li, Y.; Chan, L.; Anson, M. Increasing surface ozone concentrations in the background atmosphere of Southern China, 1994–2007. Atmos. Chem. Phys. Discuss. 2009, 9, 10429–10455. [Google Scholar] [CrossRef]
- World Health Organization. Air Quality Guidelines: Global Update 2005: Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide; World Health Organization: Geneva, Switzerland, 2006; Available online: http://www.euro.who.int/__data/assets/pdf_file/0005/78638/E90038.pdf (accessed on 13 November 2013).
- Kurokawa, J.; Ohara, T.; Uno, I.; Hayasaki, M.; Tanimoto, H. Influence of meteorological variability on interannual variations of springtime boundary layer ozone over Japan during 1981–2005. Atmos. Chem. Phys. 2009, 9, 6287–6304. [Google Scholar] [CrossRef]
- Oltmans, S.J.; Lefohn, A.S.; Harris, J.M.; Shadwick, D.S. Background ozone levels of air entering the west coast of the US and assessment of longer-term changes. Atmos. Environ. 2008, 42, 6020–6038. [Google Scholar] [CrossRef]
- Parrish, D.; Millet, D.; Goldstein, A. Increasing ozone in marine boundary layer inflow at the west coasts of North America and Europe. Atmos. Chem. Phys. 2009, 9, 1303–1323. [Google Scholar] [CrossRef]
- Zhong, L.; Louie, P.K.; Zheng, J.; Yuan, Z.; Yue, D.; Ho, J.W.; Lau, A.K. Science-policy interplay: Air quality management in the Pearl River Delta region and Hong Kong. Atmos. Environ. 2013, 76, 3–10. [Google Scholar] [CrossRef]
- Stocker, T.F.; Qin, D.; Plattner, G.-K.; Tignor, M.; Allen, S.K.; Boschung, J.; Nauels, A.; Xia, Y.; Bex, V.; Midgley, P.M. IPCC, 2013: Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2013. [Google Scholar]
- Atkinson, R.W.; Yu, D.; Armstrong, B.G.; Pattenden, S.; Wilkinson, P.; Doherty, R.M.; Heal, M.R.; Anderson, H.R. Concentration-response function for ozone and daily mortality: Results from five urban and five rural U.K. Populations. Environ. Health Perspect. 2012, 120, 1411–1417. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Dominici, F.; Samet, J.M. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology 2005, 16, 436. [Google Scholar] [CrossRef] [PubMed]
- Hunova, I.; Maly, M.; Rezacova, J.; Branis, M. Association between ambient ozone and health outcomes in Prague. Int. Arch. Occup. Environ. Health 2013, 86, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Ren, C.; Williams, G.M.; Mengersen, K.; Morawska, L.; Tong, S. Does temperature modify short-term effects of ozone on total mortality in 60 large eastern US communities?—An assessment using the NMMAPS data. Environ. Int. 2008, 34, 451–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gryparis, A.; Forsberg, B.; Katsouyanni, K.; Analitis, A.; Touloumi, G.; Schwartz, J.; Samoli, E.; Medina, S.; Anderson, H.R.; Niciu, E.M. Acute Effects of Ozone on Mortality from the “Air Pollution and Health a European Approach” Project. Am. J. Respir. Crit. Care Med. 2004, 170, 1080–1087. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; De Leon, S.F.; Lippmann, M. Associations between ozone and daily mortality: Analysis and meta-analysis. Epidemiology 2005, 16, 446–457. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J. How sensitive is the association between ozone and daily deaths to control for temperature? Am. J. Respir. Crit. Care Med. 2005, 171, 627–631. [Google Scholar] [CrossRef] [PubMed]
- Zanobetti, A.; Schwartz, J. Is there adaptation in the ozone-mortality relationship: A multi-city case crossover analysis. Environ. Health 2008, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Almeida, S.P.D.; Casimiro, E.; Calheiros, J. Short-term association between exposure to ozone and mortality in Oporto, Portugal. Environ. Res. 2011, 111, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Ou, C.Q.; Wong, C.M.; Ho, S.Y.; Schooling, M.; Yang, L.; Hedley, A.J.; Lam, T.H. Dietary habits and the short-term effects of air pollution on mortality in the Chinese population in Hong Kong. J. Epidemiol. Community Health 2012, 66, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Qian, Z.; He, Q.; Lin, H.M.; Kong, L.; Bentley, C.M.; Liu, W.; Zhou, D. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan, China. Environ. Health Perspect. 2008, 116, 1172–1178. [Google Scholar] [CrossRef] [PubMed]
- Tao, Y.; Huang, W.; Huang, X.; Zhong, L.; Lu, S.-E.; Li, Y.; Dai, L.; Zhang, Y.; Zhu, T. Estimated acute effects of ambient ozone and nitrogen dioxide on mortality in the Pearl River Delta of southern China. Environ. Health Perspect. 2012, 120, 393. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.M.; Ma, S.; Hedley, A.J.; Lam, T.H. Does ozone have any effect on daily hospital admissions for circulatory diseases? J. Epidemiol. Community Health 1999, 53, 580–581. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.M.; Ma, S.; Hedley, A.J.; Lam, T.H. Effect of air pollution on daily mortality in Hong Kong. Environ. Health Perspect. 2001, 109, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Yang, H.; Guo, S.; Wang, Z.; Xu, X.; Duan, X.; Kan, H. Alternative ozone metrics and daily mortality in Suzhou: The China Air Pollution and Health Effects Study (CAPES). Sci. Total Environ. 2012, 426, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Huang, W.; London, S.J.; Song, G.; Chen, G.; Jiang, L.; Zhao, N.; Chen, B.; Kan, H. Ozone and daily mortality in Shanghai, China. Environ. Health Perspect. 2006, 114, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Li, T.T.; Zhang, Y.H.; Xu, Y.J.; Lao, X.Q.; Rutherford, S.; Chu, C.; Luo, Y.; Zhu, Q.; Xu, X.J.; et al. The short-term effect of ambient ozone on mortality is modified by temperature in Guangzhou, China. Atmos. Environ. 2013, 76, 59–67. [Google Scholar] [CrossRef]
- Chen, R.; Cai, J.; Meng, X.; Kim, H.; Honda, Y.; Guo, Y.L.; Samoli, E.; Yang, X.; Kan, H. Ozone and Daily Mortality Rate in 21 Cities of East Asia: How Does Season Modify the Association? Am. J. Epidemiol. 2014, 180, 729–736. [Google Scholar] [CrossRef] [PubMed]
- National Morbidity Mortality and Air Pollution Study (NMMAPS) Database. Available online: http://www.ihapss.jhsph.edu/ (accessed on 5 March 2013).
- Bell, M.L.; McDermott, A.; Zeger, S.L.; Samet, J.M.; Dominici, F. Ozone and short-term mortality in 95 US urban communities, 1987–2000. JAMA 2004, 292, 2372–2378. [Google Scholar] [CrossRef] [PubMed]
- Internet-Based Health & Air Pollution Surveillance System (iHAPSS). Mortality, Air Pollution, and Meteorological Data for 108 U.S. Cities 1987–2000. Available online: http://www.ihapss.jhsph.edu/ (accessed on 1 December 2011).
- Abbey, D.E.; Burchette, R.J. Relative power of alternative ambient air pollution metrics for detecting chronic health effects in epidemiological studies. Environmetrics 1996, 7, 453–470. [Google Scholar] [CrossRef]
- Li, T.; Horton, R.M.; Kinney, P.L. Projections of seasonal patterns in temperature-related deaths for Manhattan, New York. Nat. Clim. Chang. 2013, 3, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Barnett, A.G.; Pan, X.; Yu, W.; Tong, S. The impact of temperature on mortality in Tianjin, China: A case-crossover design with a distributed lag nonlinear model. Environ. Health Perspect. 2011, 119, 1719–1725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, R.D.; Dominici, F.; Pastor-Barriuso, R.; Zeger, S.L.; Samet, J.M. Seasonal analyses of air pollution and mortality in 100 US cities. Am. J. Epidemiol. 2005, 161, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Wu, W.; Xiao, Y.; Li, G.; Zeng, W.; Lin, H.; Rutherford, S.; Xu, Y.; Luo, Y.; Xu, X.; Chu, C.; et al. Temperature-mortality relationship in four subtropical Chinese cities: A time-series study using a distributed lag non-linear model. Sci. Total Environ. 2013, 449, 355–362. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Hamra, G.B.; Guha, N.; Cohen, A.; Laden, F.; Raaschou-Nielsen, O.; Samet, J.M.; Vineis, P.; Forastiere, F.; Saldiva, P.; Yorifuji, T.; et al. Outdoor particulate matter exposure and lung cancer: A systematic review and meta-analysis. Environ. Health Perspect. 2014, 122, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A. Distributed lag linear and non-linear models in R: The package DLNM. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Jhun, I.; Fann, N.; Zanobetti, A.; Hubbell, B. Effect modification of ozone-related mortality risks by temperature in 97 US cities. Environ. Int. 2014, 73, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Burian, S.J.; Shepherd, J.M. Effect of urbanization on the diurnal rainfall pattern in Houston. Hydrol. Process. 2005, 19, 1089–1103. [Google Scholar] [CrossRef]
- Bell, M.L.; Dominici, F. Effect modification by community characteristics on the short-term effects of ozone exposure and mortality in 98 US communities. Am. J. Epidemiol. 2008, 167, 986–997. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.L.; Xu, B.; Switzer, P. Reassessing the relationship between ozone and short-term mortality in U.S. urban communities. Inhal. Toxicol. 2009, 21, 37–61. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Peng, J.; Zhang, Y.; Liu, T.; Rutherford, S.; Lin, H.; Qian, Z.; Huang, C.; Luo, Y.; Zeng, W. How much does latitude modify temperature–mortality relationship in 13 eastern US cities? Int. J. Biometeorol. 2015, 59, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Peng, R.D.; Dominici, F. Statistical Methods for Environmental Epidemiology with R: A Case Study in Air Pollution and Health; Springer: Berlin, Germany; Heidelberg, Germany, 2008; pp. 88–90. [Google Scholar]
- Roberts, S.; Martin, M. Applying a moving total mortality count to the cities in the nmmaps database to estimate the mortality effects of particulate matter air pollution. Occup. Environ. Med. 2006, 63, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Samet, J.; Zeger, S.; Dominici, F.; Curriero, F.; Coursac, I.; Dockery, D.; Schwartz, J.; Zanobetti, A. The national morbidity, mortality and air pollution study, part II: Morbidity and mortality from air pollution in the United States. Res. Rep. 2000, 94, 5–79. [Google Scholar]
- Reichert, T.A.; Simonsen, L.; Sharma, A.; Pardo, S.A.; Fedson, D.S.; Miller, M.A. Influenza and the winter increase in mortality in the United States, 1959–1999. Am. J. Epidemiol. 2004, 160, 492–502. [Google Scholar] [CrossRef] [PubMed]
- Weschler, C.J. Ozone’s impact on public health: Contributions from indoor exposures to ozone and products of ozone-initiated chemistry. Environ. Health Perspect. 2006, 114, 1489–1496. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Latitude (°) | Longitude (°) | Population (×100,000) | Average Daily Mortality | Annual Average Temperature (°C) | Annual Average Relative Humidity (%) | Average O3 Concentration (ppb) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Full Year | Spring | Summer | Autumn | Winter | |||||||
| Southern communities | |||||||||||
| Houston | 29.8 | 95.4 | 34.0 | 42.8 | 20.8 | 71.3 | 38.9 | 44.0 | 44.1 | 42.0 | 25.5 |
| Dallas | 32.8 | 96.8 | 42.0 | 54.5 | 19.2 | 59.8 | 41.4 | 45.2 | 53.7 | 41.2 | 25.3 |
| Tampa | 28.0 | 82.5 | 10.0 | 18.5 | 23.0 | 73.3 | 41.0 | 50.1 | 41.1 | 39.4 | 33.4 |
| Shreveport | 32.5 | 93.8 | 3.5 | 8.6 | 18.8 | 68.9 | 44.6 | 48.6 | 53.3 | 44.7 | 31.5 |
| Little Rock | 34.7 | 92.4 | 3.6 | 7.9 | 17.2 | 67.9 | 41.1 | 45.1 | 53.4 | 38.8 | 26.8 |
| St. Petersburg | 27.8 | 82.6 | 9.2 | 31.2 | 23.0 | 73.3 | 39.6 | 49.1 | 38.5 | 37.4 | 33.2 |
| Nashville | 36.2 | 86.8 | 5.7 | 11.6 | 15.6 | 66.3 | 34.7 | 38.9 | 50.4 | 31.2 | 17.8 |
| Austin | 30.3 | 97.8 | 8.1 | 8.6 | 20.8 | 62.9 | 40.2 | 45.4 | 43.8 | 42.3 | 29.2 |
| Jacksonville | 30.3 | 81.7 | 7.8 | 14.4 | 20.4 | 75.5 | 41.0 | 49.7 | 44.2 | 38.6 | 31.4 |
| New Orleans | 30.1 | 89.9 | 4.8 | 12.2 | 20.7 | 74.8 | 33.9 | 41.5 | 37.2 | 33.2 | 23.5 |
| Average | 31.3 | 90.0 | 12.9 | 21.0 | 20.0 | 69.4 | 39.6 | 45.8 | 46.0 | 38.9 | 27.8 |
| Northern communities | |||||||||||
| Jersey City | 40.7 | 74.1 | 6.1 | 11.5 | 13.2 | 62.4 | 34.3 | 37.2 | 56.7 | 27.4 | 15.5 |
| New York | 40.7 | 73.9 | 89.3 | 190.2 | 12.8 | 64.8 | 32.0 | 34.1 | 49.9 | 24.9 | 18.8 |
| Syracuse | 43.0 | 76.1 | 4.5 | 11.1 | 9.1 | 69.8 | 35.3 | 41.3 | 48.0 | 28.2 | 23.3 |
| Boston | 42.3 | 71.0 | 6.9 | 13.2 | 10.9 | 66.5 | 30.2 | 35.5 | 44.3 | 22.6 | 18.2 |
| Chicago | 41.8 | 87.7 | 53.8 | 115.4 | 10.1 | 69.6 | 28.9 | 33.0 | 45.0 | 22.7 | 14.4 |
| Newark | 40.7 | 74.2 | 7.9 | 18.5 | 13.2 | 62.4 | 28.4 | 30.7 | 45.8 | 20.3 | 14.6 |
| Pittsburgh | 40.4 | 80.0 | 12.8 | 38.3 | 11.0 | 65.7 | 35.8 | 40.3 | 55.6 | 27.0 | 18.7 |
| Buffalo | 42.9 | 78.9 | 9.5 | 25.5 | 9.2 | 69.9 | 35.4 | 40.0 | 50.8 | 27.6 | 22.7 |
| Washington | 38.9 | 77.0 | 5.7 | 15.7 | 12.8 | 67.4 | 32.6 | 33.7 | 55.7 | 25.8 | 14.7 |
| Rochester | 43.2 | 77.6 | 7.4 | 15.8 | 9.1 | 71.0 | 34.1 | 39.2 | 48.3 | 27.1 | 21.9 |
| Average | 41.5 | 77.1 | 20.4 | 45.5 | 11.1 | 67.0 | 32.7 | 36.5 | 50.0 | 25.4 | 17.9 |
| Southern Communities | Northern Communities | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Min | 25th | 75th | Max | Mean | Min | 25th | 75th | Max | |
| Full year | ||||||||||
| Total mortality | 21.0 | 7.9 | 8.6 | 34.1 | 54.5 | 45.5 | 11.1 | 12.8 | 57.6 | 190.2 |
| Mean temperature (°C) | 20.0 | 15.6 | 18.4 | 21.4 | 23.0 | 11.1 | 9.1 | 9.2 | 12.9 | 13.2 |
| Relative humidity (%) | 69.2 | 59.8 | 65.5 | 73.7 | 75.5 | 67.0 | 62.4 | 64.2 | 69.8 | 71.0 |
| Maximum 8 h O3 (ppb) | 39.7 | 34.5 | 37.9 | 41.2 | 44.7 | 32.1 | 28.9 | 29.8 | 34.5 | 35.7 |
| Spring | ||||||||||
| Total mortality | 21.0 | 8.1 | 9.3 | 28.6 | 54.1 | 45.4 | 11.1 | 13.9 | 35.5 | 188.3 |
| Mean temperature (°C) | 19.6 | 15.2 | 18.6 | 20.6 | 22.5 | 9.9 | 7.7 | 8.2 | 11.6 | 12.0 |
| Relative humidity (%) | 66.8 | 60.1 | 64.4 | 69.0 | 72.5 | 63.3 | 59.4 | 60.9 | 65.2 | 66.8 |
| Maximum 8 h O3 (ppb) | 45.8 | 38.9 | 44.2 | 49.0 | 50.1 | 36.5 | 30.7 | 33.8 | 39.8 | 41.3 |
| Summer | ||||||||||
| Total mortality | 19.8 | 7.4 | 8.3 | 31.7 | 50.9 | 42.5 | 10.5 | 12.0 | 53.3 | 177.4 |
| Mean temperature (°C) | 27.9 | 25.8 | 27.4 | 28.5 | 29.0 | 22.3 | 20.6 | 20.8 | 23.9 | 24.4 |
| Relative humidity (%) | 70.1 | 56.8 | 66.2 | 75.9 | 77.5 | 67.3 | 63.8 | 64.7 | 69.0 | 70.7 |
| Maximum 8 h O3 (ppb) | 46.1 | 38.1 | 40.5 | 53.4 | 53.7 | 49.9 | 44.6 | 45.2 | 55.1 | 56.7 |
| Autumn | ||||||||||
| Total mortality | 20.3 | 7.7 | 9.1 | 26.6 | 52.4 | 44.3 | 10.9 | 13.4 | 33.9 | 184.3 |
| Mean temperature (°C) | 20.5 | 15.9 | 19.3 | 21.4 | 24.0 | 12.3 | 10.3 | 10.7 | 14.0 | 14.3 |
| Relative humidity (%) | 70.3 | 59.3 | 67.2 | 74.8 | 80.3 | 69.0 | 64.7 | 66.3 | 71.0 | 74.2 |
| Maximum 8 h O3 (ppb) | 38.9 | 31.3 | 37.7 | 41.8 | 44.7 | 25.4 | 20.3 | 23.3 | 27.3 | 28.2 |
| Winter | ||||||||||
| Total mortality | 23.2 | 8.7 | 9.5 | 37.5 | 60.8 | 50.0 | 12.0 | 14.0 | 63.0 | 211.1 |
| Mean temperature (°C) | 11.7 | 5.2 | 8.7 | 14.2 | 17.2 | -0.2 | -3.0 | -2.5 | 2.0 | 2.2 |
| Relative humidity (%) | 70.3 | 62.9 | 67.2 | 74.2 | 75.1 | 68.2 | 61.8 | 61.9 | 74.6 | 75.9 |
| Maximum 8 h O3 (ppb) | 27.8 | 17.8 | 25.0 | 31.9 | 33.4 | 18.6 | 14.3 | 15.2 | 21.9 | 23.1 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, T.; Zeng, W.; Lin, H.; Rutherford, S.; Xiao, J.; Li, X.; Li, Z.; Qian, Z.; Feng, B.; Ma, W. Tempo-Spatial Variations of Ambient Ozone-Mortality Associations in the USA: Results from the NMMAPS Data. Int. J. Environ. Res. Public Health 2016, 13, 851. https://doi.org/10.3390/ijerph13090851
Liu T, Zeng W, Lin H, Rutherford S, Xiao J, Li X, Li Z, Qian Z, Feng B, Ma W. Tempo-Spatial Variations of Ambient Ozone-Mortality Associations in the USA: Results from the NMMAPS Data. International Journal of Environmental Research and Public Health. 2016; 13(9):851. https://doi.org/10.3390/ijerph13090851
Chicago/Turabian StyleLiu, Tao, Weilin Zeng, Hualiang Lin, Shannon Rutherford, Jianpeng Xiao, Xing Li, Zhihao Li, Zhengmin Qian, Baixiang Feng, and Wenjun Ma. 2016. "Tempo-Spatial Variations of Ambient Ozone-Mortality Associations in the USA: Results from the NMMAPS Data" International Journal of Environmental Research and Public Health 13, no. 9: 851. https://doi.org/10.3390/ijerph13090851







