1. Introduction
Global climate change has become a growing public health concern in recent years. As one of the biggest global health threats in the 21st century [
1,
2], climate change has led to an increased frequency and intensity of extreme temperatures [
3], especially increased heat wave events. Moreover, health impacts due to climate change will continue to occur, at least for the foreseeable future [
4]. Therefore, it is of great significance and urgency for decision makers to develop adaptive strategies to climate change based on local cold- and heat-related epidemiological studies.
A non-linear U, J, or V-shaped relationship between temperature and mortality has been identified in many previous studies, which revealed the adverse effects of low and/or high temperatures [
5,
6,
7]. However, the associations between temperature and mortality varied by geographic locations, study populations, and climatic characteristics [
8,
9,
10]. Thus, it is quite necessary for different regions to conduct locally-based environmental epidemiology studies when assessing temperature-related mortality impact for local public health decision-making.
People in developing countries are anticipated to be susceptible to the impact of extreme temperatures because of more limited adaptive capacity and more vulnerable than people in developed countries [
2,
11]. Nevertheless, current knowledge of health effects of temperature on mortality is mainly from developed countries, and only a limited number of studies have been conducted in developing countries [
3]. In China, mortality impact assessment of extreme temperatures has got increasing attention in recent years and relevant studies have been conducted in several large cities in southeastern coastal areas, like Beijing [
12,
13], Shanghai [
14], Guangzhou [
15,
16], Suzhou [
3], and Tianjin [
17]. However, to date, less studies have been reported in Chinese inland areas, including several major cities in central China. Moreover, previous studies usually used mean temperature as the temperature metric, few of them have compared the effects of different temperature indicators on mortality.
As the largest city in central China, Wuhan has a climate characterized by cold winters and extremely hot summers. In order to help establishing local warning and preventive control systems to reduce both cold- and heat-related adverse health effects, the present study assessed the locally-based association between ambient temperature and cause-specific mortality and evaluated the predictive ability of different temperature indicators (minimum, mean, and maximum) on mortality in Wuhan, China.
3. Results
During the study period (1 January 2003–31 December 2010), there were 32,721 non-accidental deaths in total; 15,303 persons (46.8%) died from cardiovascular disease, including 9204 (28.1%) of stroke and 3900 (11.9%) of IHD, and 3081 persons (9.4%) died from respiratory disease (
Table 1). An average of 11.2, 5.2, 3.1, 1.3, and 1.1 cases per day occurred for non-accidental, cardiovascular, stroke, IHD, and respiratory mortality, respectively. The average daily maximum, mean, and minimum temperature were 22.2 °C (range: −1.9 °C, 39.6 °C), 17.9 °C (range: −2.7 °C, 35.8 °C), and 14.6 °C (range: −5.2 °C, 32.3 °C), respectively. The average daily relative humidity was 71.3% and ranged from 21.0% to 97.0%. The mean concentrations of daily PM
10, SO
2, and NO
2 were 115.0 μg/m
3, 50.2 μg/m
3 and 57.6 μg/m
3, respectively, which were well above the international health-based standards.
Table 2 shows the Spearman correlation coefficients of weather conditions and ambient pollutants. Three temperature measures were strongly correlated with each other, negatively correlated with ambient pollutants, and moderately correlated with relative humidity. PM
10, SO
2, and NO
2 were strongly correlated with each other.
Table 3 calculates the QAIC values of non-threshold and double-threshold DLNM models predicted by different temperature measures. Double-threshold DLNM models performed better than non-threshold DLNM models with smaller QAIC values, and mean temperature had the best predictive ability for mortality. Therefore, the results of associations between mean temperature and mortality were only reported in this paper. Cold and hot thresholds used by the double-threshold DLNM models were presented in
Table 4.
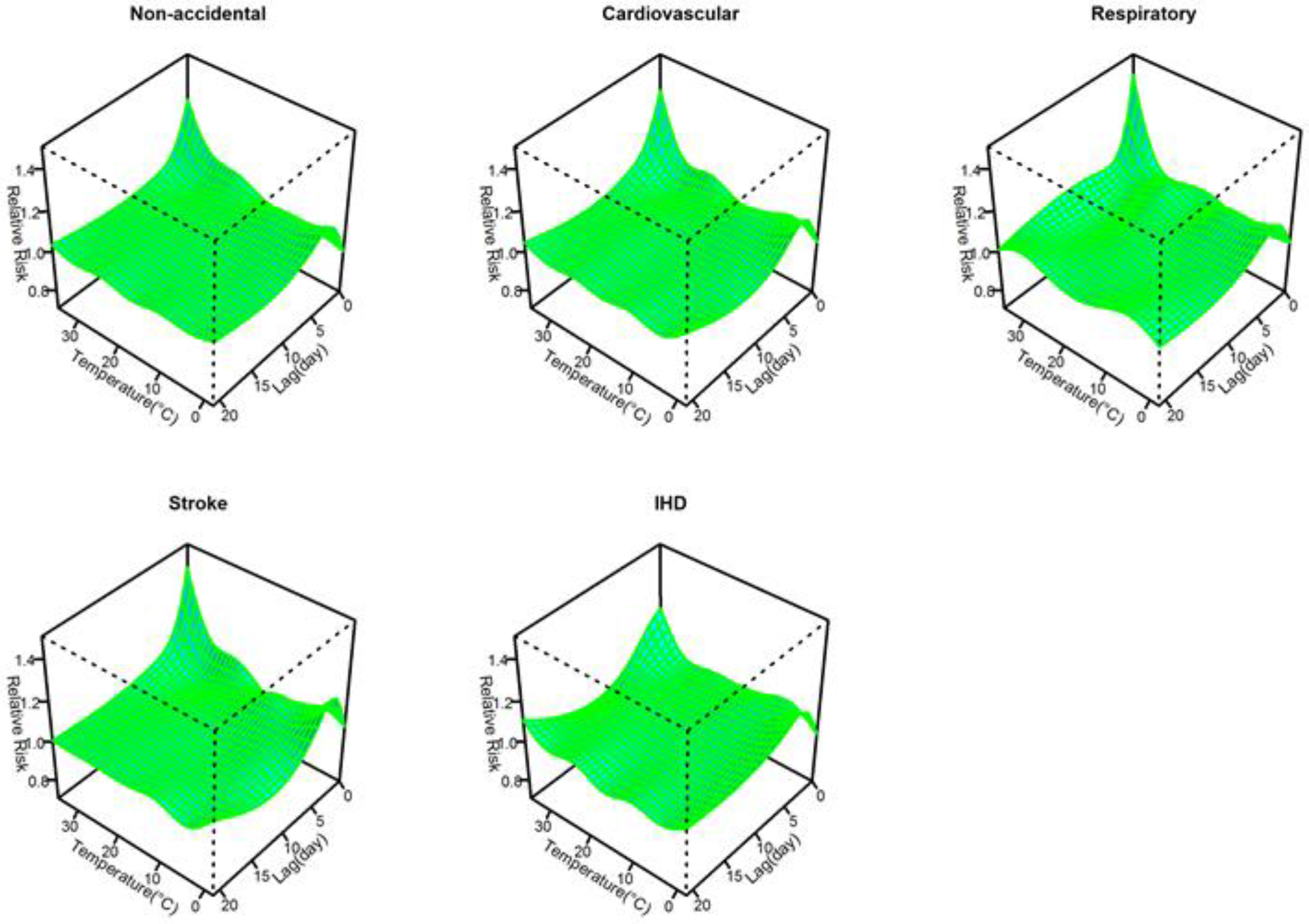
Figure 1 shows the three-dimensional plots of the relationships between mean temperature and cause-specific mortality along lags of 21 days. The estimated effects of temperature were non-linear for all cause-specific mortality categories, with higher relative risks at hot and cold temperatures, while extremely hot temperatures were associated with much higher relative risks than extremely cold temperatures within a lag of 3 days.
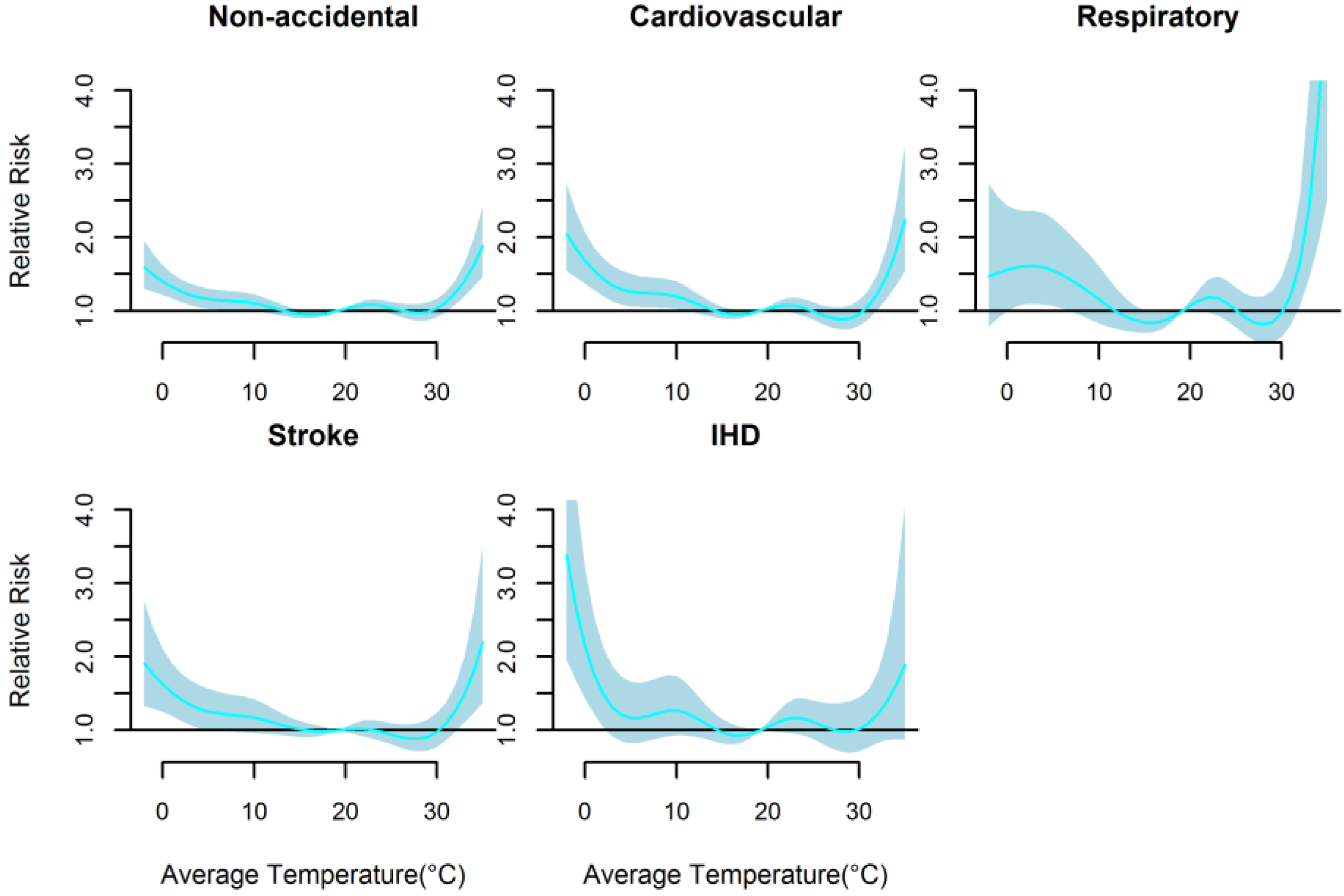
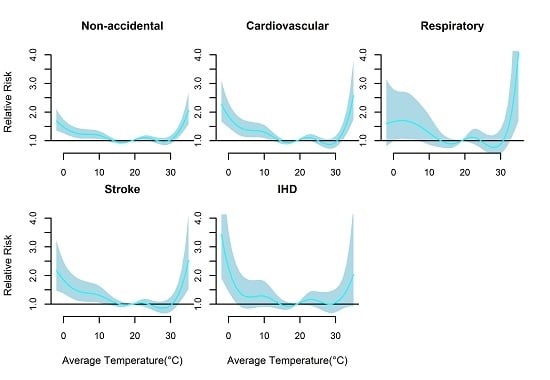
Figure 2 presents the non-linear effects of mean temperature on cause-specific mortality over 21 days. There were U-shaped relationships between mean temperature and all mortality types. The relative risks of all mortality types increased rapidly only when mean temperature were above 30.0 °C (approximately
P90 quantile of the temperature distribution), while increased slowly below 20.2 °C (approximately
P54 quantile of the temperature distribution) except IHD mortality with rapid increase below 3.5 °C. The cold and hot thresholds were 18.1 °C and 31.7 °C for non-accidental mortality, 15.6 °C and 31.4 °C for cardiovascular mortality, 14.6 °C and 31.2 °C for respiratory mortality, and 20.2 °C and 32.2 °C for stroke mortality, and 3.5 °C and 30.0 °C for IHD mortality (
Table 4).
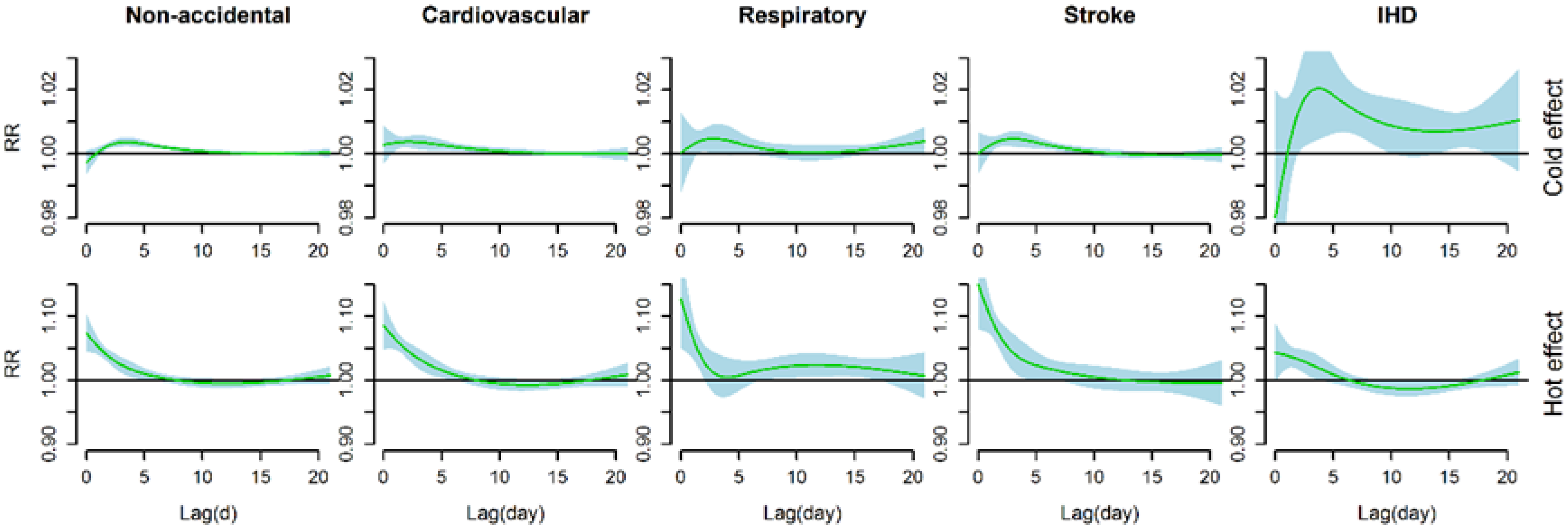
Figure 3 shows the estimated effects of cold effects (a 1 °C decrease in mean temperature below the cold threshold) and heat effects (a 1 °C increase in mean temperature above the hot threshold) on cause-specific mortality over 21 days of lag. Significant cold effects appeared after a lag of 1–2 days and lasted about 10 days (about 14 days for IHD mortality), whereas significant hot effects occurred immediately and lasted less than a week (about 10 days for respiratory mortality).
We calculated the cumulative effects of mean temperature on cause-specific mortality at different amounts of lag (
Table 5). For cold effects over a lag of 0–21 days, a 1 °C decrease in mean temperature below the cold thresholds was associated with a 2.39% (95% CI: 1.71, 3.08) increase in non-accidental mortality, 3.65% (95% CI: 2.62, 4.69) increase in cardiovascular mortality, 3.87% (95% CI: 1.57, 6.22) increase in respiratory mortality, 3.13% (95% CI: 1.88, 4.38) increase in stroke mortality, and 21.57% (95% CI: 12.59, 31.26) increase in IHD mortality. For hot effects over lag 0–7 days, a 1 °C increase in mean temperature above the hot thresholds was associated with a 25.18% (95% CI: 18.74, 31.96) increase in non-accidental mortality, 34.10% (95% CI: 25.63, 43.16) increase in cardiovascular mortality, 24.27% (95% CI: 7.55, 43.59) increase in respiratory mortality, 59.1% (95% CI: 41.81, 78.5) increase in stroke mortality, and 17.00% (95% CI: 7.91, 26.87) increase in IHD mortality. Hot effects over lag of different days were much greater than cold effects consistently except for IHD mortality at lags of longer than 14 days.
We changed df (3–8 per year) for time to control for the season, which gave similar results. We changed df (4–7) for humidity, PM
10, SO
2, and NO
2, and varied the maximum lag from 22 to 30 days, the estimated effects of temperature did not substantially change. In addition, we conducted sensitivity analyses for total mortality using different threshold values, which also gave similar results (
Figure S1). Also, age-stratified analyses confirmed our results of relationships between cause-specific mortality and mean temperature (
Figures S2 and S3 and Table S1). All in all, the models used in this study seemed to have adequately captured the main effects of temperature on mortality.
4. Discussion
In the present study, we examined the effects of ambient temperature on cause-specific mortality in Wuhan, China during the years 2003 to 2010. Non-linear and U-shaped relationshps were consistently found between temperature and all cause-specific mortality categories, which revealed that both cold and high temperarure increased the risk of mortality. Further, our data suggested that the effects of hot temperatures on mortality were much larger than that of cold temperatures. These findings may have important implications for public health policies in Wuhan, China.
The study area of the present study, Wuhan, used to be known as one of the Three Furnaces of China. During the study period 2003 to 2010, Wuhan experienced hot summers (June to August) with an average daily temperature of 28.5 °C, and about 28 high temperature days (daily maximum temperature ≥35 °C) occurred per summer. The present study provided an opportunity to examine the temperature-mortality relationship in the extremely hot areas. Jiang’an District located in the central urban area in Wuhan, with a high population density and relatively concentrated and similar living conditions. Considering these factors, the study focus on mortality impact of temperature with a long period in Jiang’an District, Wuhan City may have less assessment bias compared with studies conducted in large cities with great variation in environmental factors, and thus the results of our study may be more proper and applicable to the local practice.
U-shaped relationships were observed between temperature and cause-specific mortality categories in Wuhan, which indicated that both low and high temperature were associated with increased mortality risk. The results were consistent with some previous studies conducted in China [
15,
17,
23,
24] and a systematic evaluation of temperature-mortality relationship in 12 countries/regions [
9]. However, according to previous studies, the impacts of temperature on different mortality categories may be less consistent. For instance, both cold and heat effects were obvious for cardiovascular disease mortality, but respiratory mortality was found only associated with high temperatures in two previous studies in Australia [
25] and Suzhou, China [
3]. In Chiang Mai, Thailand, only cold effects on cardiovascular mortality and heat effect on respiratory mortality were found to be significant [
26]. Moreover, the effects of temperature on mortality may vary by locations (such as latitudes, climatic conditions), study periods, study designs, and statistical approaches [
8,
12,
23,
27]. In addition, gender, age, educational attainment, and other sociodemographic factors of the study popolation can also modify the relationship between temperature and mortality [
27,
28,
29].
Several previous studies have compared the effects of various temperature indicators on different mortality categories [
17,
30,
31]. It was revealed that maximum, minimum, and mean temperatures had similar predictive ablity due to their strong correlations [
17,
31]. However, mean temperature was most usually used to assess the association between temperature and mortality because mean temperature can represent the exposure throughout the whole day and night and provide more easily interpreted results within a policy context [
3,
32]. Our study also suggested that mean temperature performed best for predicting the effects of temperature on cause-specific mortality according to AIC values. Nevertheless, Yu et al. [
30] found different age groups and death categories were sensitive to different temperature indicators, while the effect estimates from certain temperature indicators did not significantly differ from those of mean temperature. Thus, more epidemiological studies should be conducted to further examine the potential susceptibility differences of different populations to various temperature indicators.
Consistent with most previous studies, our study found that cold effects on different mortality types were delayed about 1–2 days and hot effects occurred immediately. When assessing the effects of temperature on mortality, using short lags cannot completely capture both the cold effects and hot effects [
17]. Cold effects may be underestimated because they usually lasted for more than a week and hot effects may be overestimated because potential mortality displacement, also referred to as harvesting, might occure in longer lags. Mortality displacement refers to the phenomenon in which a specific exposure, such as temperature, impacts already frail individuals whose deaths may have only been brought forward by a few days [
33]. At least some or all of the observed effect of mortality from temperature may be explained by mortality displacement [
33]. Mortality displacement has been obseverd in many studies when evaluating the effects of heat stress and cold spells on mortality [
17,
34]. However, the presence of mortality displacement was not consistently found in some other studies [
12,
33]. Moreover, a global analysis revealed that absence of displacement phenomenon of cold effects was consistently observed but varied greatly in displacement of hot effects in 12 countries/regions [
9]. In our present study, both cold effect and hot effect lasted for several days and no obvious mortality displacement was observed in different mortality types, which suggests that both cold and high temperature exposure have broader impacts on the public health in Wuhan.
The results of low temperature and mortality in this study are generally comparable with previous studies in China (
Table 6). For non-accidental mortality, for instance, a 1 °C decrease in mean temperature below the cold threshold in our study was associated with a 2.39% (95% CI: 1.71, 3.08) increase with a lag of 21 days, and 2.99% (95% CI: 0.85, 5.17) with a lag of 18 days in Tianjin [
17], 4.3% (95% CI: 1.3, 7.5), and 4.4% (95% CI: 3.4, 5.5) in Changsha and Kunming, respectively, with a lag of 20 days [
15]. Some differences, however, were that the hot effects on different mortality types were much stronger in Wuhan, which can be explained by the very high hot thresholds of mean temperature (above 30 °C, which were approximately equal to the 90th percentile of temperature distribution during the study period) due to acclimatization to local extremely hot summers, strong urban heat island effects, and high housing density in inner central urban areas. Even so, it was notable that the range from cold thresholds to minimum temperature in our study were much wider than that from hot thresholds to maximum temperature, and in this sense, extremely cold temperatures may make comparable contributions to mortality risk with extremely hot temperatures.
Compared to a substudy of PHEWE project, in which Baccini et al. [
35] assessed the impact of summer heat on mortality in 15 European cities over the 1990s, our study showed a much steeper slope above threshold, which indicated higher mortality risk associated with summer heat. As previous studies noted, heat-related mortality risks varied greatly from city to city [
9,
36], and people in developing countries are more susceptible to heat-related mortality than developed countries due to limited adaptive capacity [
2]. Also, previous evidence suggested that the elderly appeared to be at higher risk than younger populations during hot days [
37], and the elderly aged over 65 accounted for 12.7% of the total population in this study. An ageing population, very hot summers, and high housing density will increase vulnerability to summer weather [
38], which may contribute a lot to strong hot effects in our study area. Previous epidemiologic evidence indicated that air pollution, such as PM
10 and O
3, may modify the association between temperature and mortality, while the modified effects were not consistent in different studies [
39]. Basu reviewed epidemiological studies from 2001 to 2008 and found that this effect modification by air pollutants was relatively small, and there was clearly an independent effect of both temperature and air pollution on mortality [
39]. Additionally, a number of recent studies demonstrated that temperature-related mortality risks remained almost unchanged with and without adjusting for air pollutants [
9], as well as mortality effects of heat waves [
40], and cold spells [
41]. Moreover, the relationship between mortality and temperature was not likely to have been substantially confounded by the effects of air pollution since the effects of air pollution on mortality were much lower than the effects of temperature [
41]. Thus, we did not consider the potential interactive effects between air pollution and temperature in the present study.
Some limitations should be mentioned. First, the daily mortality data was obtained from only one district of Wuhan City, which may not completely capture the mortality effects of temperature in the whole city. Nevertheless, extreme temperature-related mortality may vary greatly within a large city [
42]. Thus in our study, relatively concentrated living area, similar living conditions, and a relatively long study period may enhance the assessment precision of our study and the applicability of our results to local decision-making guidance. Second, the relatively small number of deaths due to cause-specific diseases may on one hand have limited our ability to detect tenuous differences in associations between temperature and cause-specific mortality but would not substantially affect our main findings. On the other hand, we did not use methods that could deal directly with excess zeros for respiratory and IHD mortality, such as zero-inflated Poisson models. This may thus result in some potential distortion when assessing temperature-mortality relationships. In addition, environmental exposure factors (temperature, relative humidity, and ambient pollutants) in the present study were monitored in fixed monitoring sites and cannot completely represent the actual exposure of individual level; therefore, there might exist some inevitable assessment error.