Physical Activity Programs with Post-Intervention Follow-Up in Children: A Comprehensive Review According to Categories of Intervention
Abstract
:1. Introduction
2. Methods
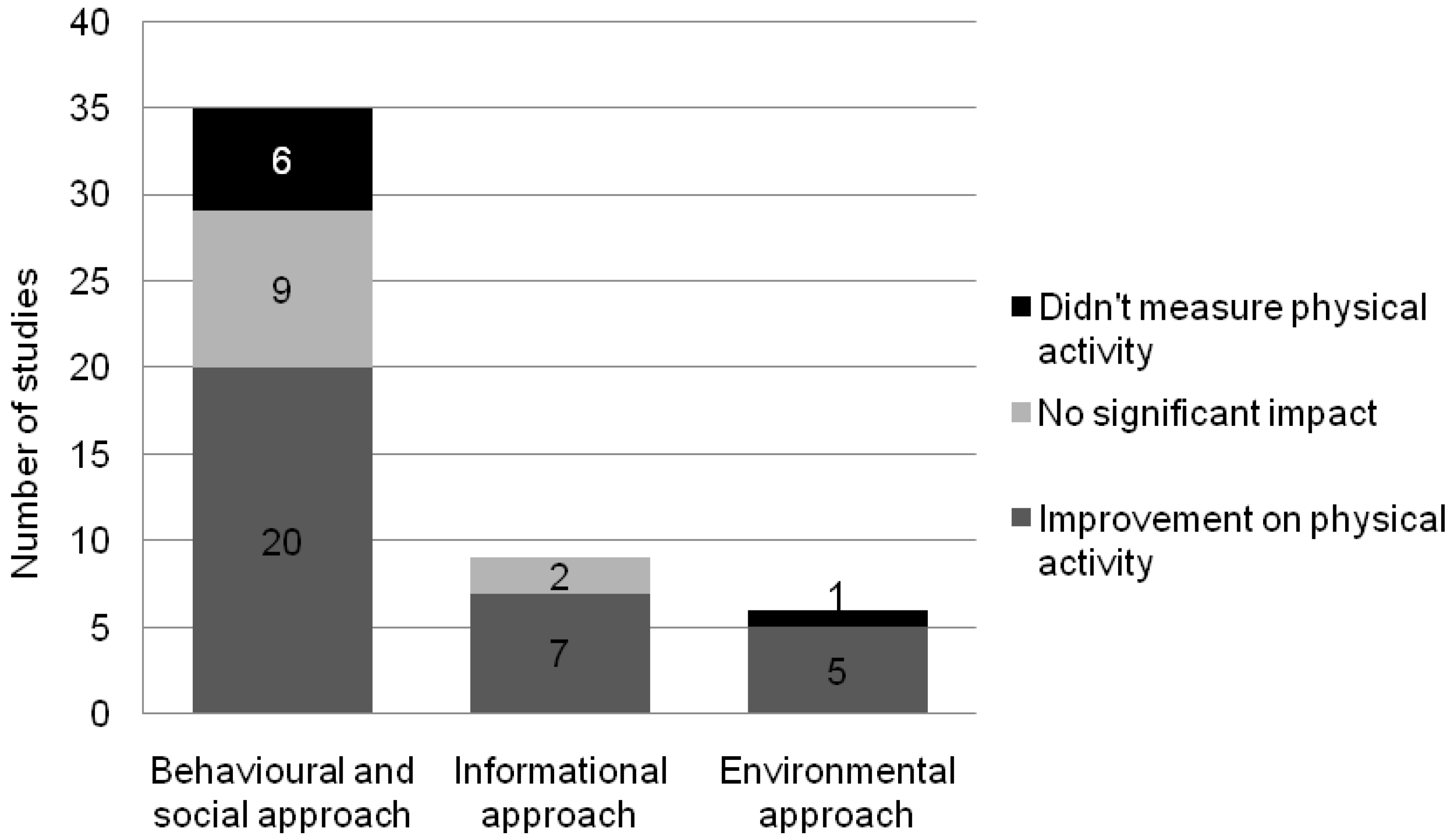
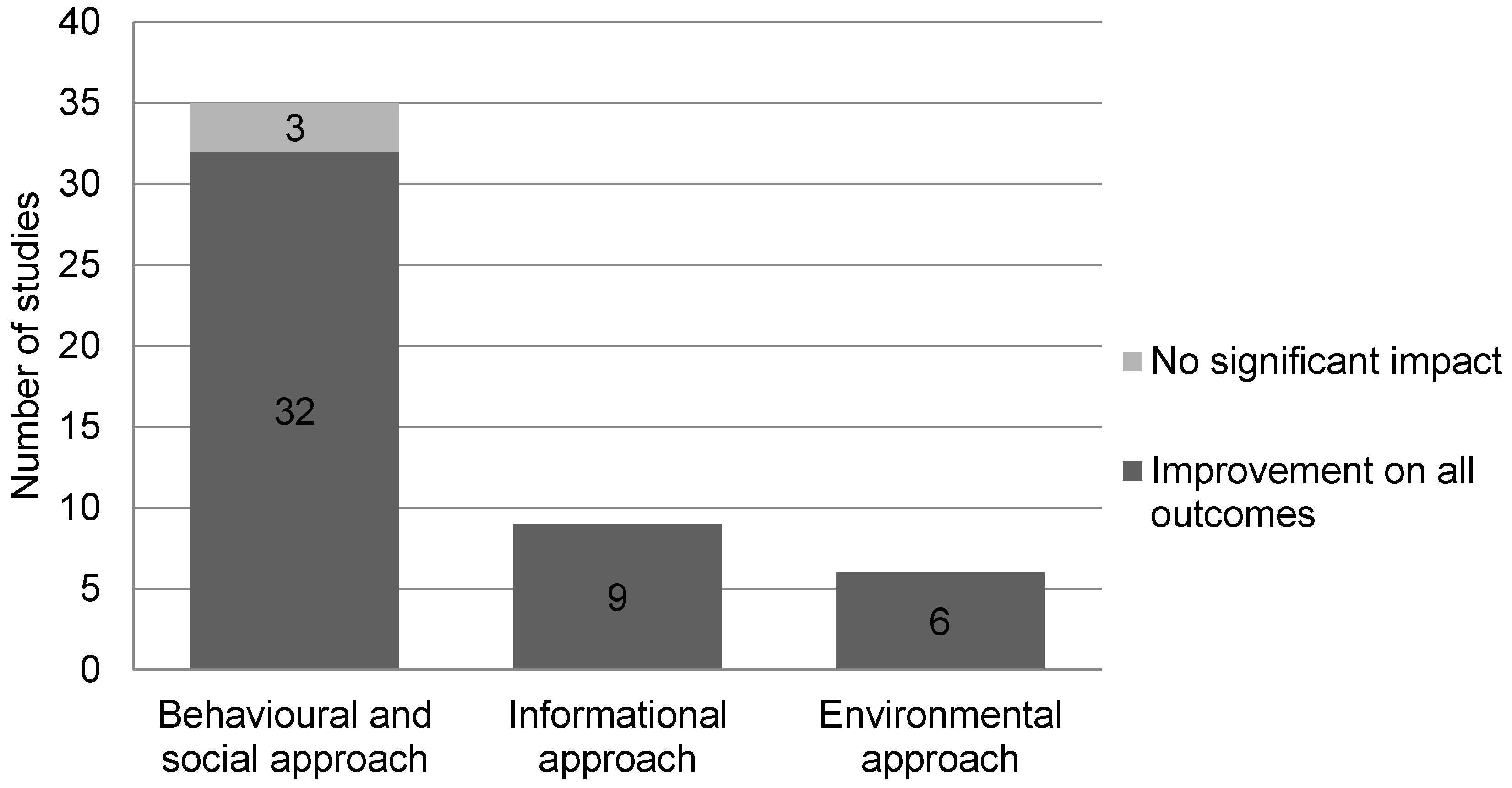
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Janssen, I.; Leblanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.A.; McNeil, D.A.; Maloff, B.; Mutasingwa, D.; Wu, M.; Ford, C.; Tough, S.C. Reducing obesity and related chronic disease risk in children and youth: A synthesis of evidence with “best practice” recommendations. Obes. Rew. Off. J. Int. Assoc. Study Obes. 2006, 7, 7–66. [Google Scholar] [CrossRef] [PubMed]
- Warschburger, P. The unhappy obese child. Int. J. Obes. 2005, 29, S127–S129. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Willms, J.D. Secular trends in the body mass index of canadian children. CMAJ Can. Med. Assoc. J. 2000, 163, 1429–1433. [Google Scholar]
- The Participaction Report Card on Physical Activity for Children and Youth. Available online: http://www.participaction.com/wp-content/uploads/2015/03/2015-Report-Card-Infographic-EN-FINAL.pdf (accessed on 7 March 2016).
- World Health Organization. Physical Activity and Young People. Available online: http://www.who.int/dietphysicalactivity/factsheet_young_people/en/ (accessed on 7 March 2016).
- American Heart Association. The Aha’s Recommendations for Physical Activity in Children. Available online: http://www.heart.org/HEARTORG/GettingHealthy/HealthierKids/ActivitiesforKids/The-AHAs-Recommendations-for-Physical-Activity-in-Children_UCM_304053_Article.jsp (accessed on 8 July 2015).
- Hayman, L.L.; Meininger, J.C.; Daniels, S.R.; McCrindle, B.W.; Helden, L.; Ross, J.; Dennison, B.A.; Steinberger, J.; Williams, C.L.; American Heart Association Committee on Atherosclerosis; et al. Primary prevention of cardiovascular disease in nursing practice: Focus on children and youth: A scientific statement from the american heart association committee on atherosclerosis, hypertension, and obesity in youth of the council on cardiovascular disease in the young, council on cardiovascular nursing, council on epidemiology and prevention, and council on nutrition, physical activity, and metabolism. Circulation 2007, 116, 344–357. [Google Scholar] [PubMed]
- Tarro, L.; Llaurado, E.; Albaladejo, R.; Morina, D.; Arija, V.; Sola, R.; Giralt, M. A primary-school-based study to reduce the prevalence of childhood obesity—The edal (educacio en alimentacio) study: A randomized controlled trial. Trials 2014, 15, 58. [Google Scholar] [CrossRef] [PubMed]
- Penalvo, J.L.; Sotos-Prieto, M.; Santos-Beneit, G.; Pocock, S.; Redondo, J.; Fuster, V. The program SI! Intervention for enhancing a healthy lifestyle in preschoolers: First results from a cluster randomized trial. BMC Public Health 2013, 13, 1208. [Google Scholar] [CrossRef] [PubMed]
- D’Haese, S.; Van Dyck, D.; De Bourdeaudhuij, I.; Deforche, B.; Cardon, G. Organizing ”play streets” during school vacations can increase physical activity and decrease sedentary time in children. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mura, G.; Rocha, N.B.; Helmich, I.; Budde, H.; Machado, S.; Wegner, M.; Nardi, A.E.; Arias-Carrion, O.; Vellante, M.; Baum, A.; et al. Physical activity interventions in schools for improving lifestyle in european countries. Clin. Pract. Epidemiol. Ment. Health 2015, 11, 77–101. [Google Scholar] [CrossRef] [PubMed]
- Kahn, E.B.; Ramsey, L.T.; Brownson, R.C.; Heath, G.W.; Howze, E.H.; Powell, K.E.; Stone, E.J.; Rajab, M.W.; Corso, P. The effectiveness of interventions to increase physical activity. Syst. Rev. Am. J. Perv. Med. 2002, 22, 73–107. [Google Scholar] [CrossRef]
- Werch, C.; Moore, M.; DiClemente, C.C.; Owen, D.M.; Jobli, E.; Bledsoe, R. A sport-based intervention for preventing alcohol use and promoting physical activity among adolescents. J. Sch. Health 2003, 73, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Werch, C.C.; Moore, M.J.; DiClemente, C.C.; Bledsoe, R.; Jobli, E. A multihealth behavior intervention integrating physical activity and substance use prevention for adolescents. Prev. Sci. Off. J. Soc. Prev. Res. 2005, 6, 213–226. [Google Scholar] [CrossRef] [PubMed]
- De Bourdeaudhuij, I.; Maes, L.; De Henauw, S.; De Vriendt, T.; Moreno, L.A.; Kersting, M.; Sarri, K.; Manios, Y.; Widhalm, K.; Sjostrom, M.; et al. Evaluation of a computer-tailored physical activity intervention in adolescents in six european countries: The activ-o-meter in the helena intervention study. J. Adolesc. Health 2010, 46, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Prins, R.G.; Brug, J.; van Empelen, P.; Oenema, A. Effectiveness of youraction, an intervention to promote adolescent physical activity using personal and environmental feedback: A cluster rct. PLoS ONE 2012, 7, e32682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jemmott, J.B., 3rd; Jemmott, L.S.; O’Leary, A.; Ngwane, Z.; Icard, L.; Bellamy, S.; Jones, S.; Landis, J.R.; Heeren, G.A.; Tyler, J.C.; et al. Cognitive-behavioural health-promotion intervention increases fruit and vegetable consumption and physical activity among south african adolescents: A cluster-randomised controlled trial. Psychol. Health 2011, 26, 167–185. [Google Scholar] [PubMed]
- Cui, Z.; Shah, S.; Yan, L.; Pan, Y.; Gao, A.; Shi, X.; Wu, Y.; Dibley, M.J. Effect of a school-based peer education intervention on physical activity and sedentary behaviour in chinese adolescents: A pilot study. BMJ Open 2012, 2. [Google Scholar] [CrossRef] [PubMed]
- Latif, H.; Watson, K.; Nguyen, N.; Thompson, D.; Baranowski, J.; Jago, R.; Cullen, K.W.; Baranowski, T. Effects of goal setting on dietary and physical activity changes in the boy scout badge projects. Health Educ. Behav. Off. Publ. Soc. Public Health Educ. 2011, 38, 521–529. [Google Scholar] [CrossRef] [PubMed]
- McCallum, Z.; Wake, M.; Gerner, B.; Baur, L.A.; Gibbons, K.; Gold, L.; Gunn, J.; Harris, C.; Naughton, G.; Riess, C.; et al. Outcome data from the LEAP (live, eat and play) trial: A randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. Int. J. Obes. 2007, 31, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Araujo-Soares, V.; McIntyre, T.; MacLennan, G.; Sniehotta, F.F. Development and exploratory cluster-randomised opportunistic trial of a theory-based intervention to enhance physical activity among adolescents. Psychol. Health 2009, 24, 805–822. [Google Scholar] [CrossRef] [PubMed]
- Pettee Gabriel, K.K.; DiGioacchino DeBate, R.; High, R.R.; Racine, E.F. Girls on the run: A quasi-experimental evaluation of a developmentally focused youth sport program. J. Phys. Act. Health 2011, 8, S285–S294. [Google Scholar] [PubMed]
- Sacher, P.M.; Kolotourou, M.; Chadwick, P.M.; Cole, T.J.; Lawson, M.S.; Lucas, A.; Singhal, A. Randomized controlled trial of the mend program: A family-based community intervention for childhood obesity. Obesity 2010, 18, S62–S68. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; Paluch, R.A.; Kilanowski, C.K.; Raynor, H.A. The effect of reinforcement or stimulus control to reduce sedentary behavior in the treatment of pediatric obesity. Health Psychol. Off. J. Division Health Psychol. Am. Psychol. Assoc. 2004, 23, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Plachta-Danielzik, S.; Pust, S.; Asbeck, I.; Czerwinski-Mast, M.; Langnase, K.; Fischer, C.; Bosy-Westphal, A.; Kriwy, P.; Muller, M.J. Four-year follow-up of school-based intervention on overweight children: The kops study. Obesity 2007, 15, 3159–3169. [Google Scholar] [CrossRef] [PubMed]
- Plachta-Danielzik, S.; Landsberg, B.; Lange, D.; Seiberl, J.; Muller, M.J. Eight-year follow-up of school-based intervention on childhood overweight—The kiel obesity prevention study. Obes. Facts 2011, 4, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Deforche, B.; De Bourdeaudhuij, I.; Tanghe, A.; Hills, A.P.; De Bode, P. Changes in physical activity and psychosocial determinants of physical activity in children and adolescents treated for obesity. Patient Educ. Couns. 2004, 55, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Hermann, J.R.; Parker, S.P.; Brown, B.J.; Siewe, Y.J.; Denney, B.A.; Walker, S.J. After-school gardening improves children’s reported vegetable intake and physical activity. J. Nutr. Educ. Behav. 2006, 38, 201–202. [Google Scholar] [CrossRef] [PubMed]
- Stahl, C.E.; Necheles, J.W.; Mayefsky, J.H.; Wright, L.K.; Rankin, K.M. 5-4-3-2-1 go! Coordinating pediatric resident education and community health promotion to address the obesity epidemic in children and youth. Clin. Pediatr. 2011, 50, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Cao, D.S.; Lippke, S. Stage-matched minimal interventions to enhance physical activity in chinese adolescents. J. Adolesc. Health 2010, 47, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Spruijt-Metz, D.; Nguyen-Michel, S.T.; Goran, M.I.; Chou, C.P.; Huang, T.T. Reducing sedentary behavior in minority girls via a theory-based, tailored classroom media intervention. Int. J. Pediatri. Obes. 2008, 3, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Francis, M.; Nichols, S.S.; Dalrymple, N. The effects of a school-based intervention programme on dietary intakes and physical activity among primary-school children in trinidad and tobago. Public Health Nutr. 2010, 13, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Balamurugan, A.; Oakleaf, E.J.; Rath, D. Using paid radio advertisements to promote physical activity among arkansas tweens. Prev. Chronic Dis. 2005, 2, A08. [Google Scholar] [PubMed]
- Chen, J.L.; Weiss, S.; Heyman, M.B.; Vittinghoff, E.; Lustig, R. Pilot study of an individually tailored educational program by mail to promote healthy weight in chinese american children. J. Spec. Pediatr. Nurs. JSPN 2008, 13, 212–222. [Google Scholar] [CrossRef] [PubMed]
- McDermott, R.J.; Davis, J.L.; Bryant, C.A.; Courtney, A.H.; Alfonso, M.L. Increasing physical activity in children 8 to 12 years old: Experiences with verb summer scorecard. Percept. Motor Skills 2010, 111, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Manios, Y.; Kafatos, I.; Kafatos, A. Ten-year follow-up of the cretan health and nutrition education program on children’s physical activity levels. Perv. Med. 2006, 43, 442–446. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.R.; Saunders, R.; Dishman, R.K.; Addy, C.; Dowda, M.; Ward, D.S. Long-term effects of a physical activity intervention in high school girls. Am. J. Perv. Med. 2007, 33, 276–280. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, T.L.; Li, D.; Derby, C.A.; Webber, L.S.; Luepker, R.V.; Cribb, P. Maintenance of effects of the catch physical education program: Results from the catch-on study. Health Educ. Behav. 2003, 30, 447–462. [Google Scholar] [CrossRef] [PubMed]
- Webber, L.S.; Osganian, S.K.; Feldman, H.A.; Wu, M.; McKenzie, T.L.; Nichaman, M.; Lytle, L.A.; Edmundson, E.; Cutler, J.; Nader, P.R.; et al. Cardiovascular risk factors among children after a 2 1/2-year intervention-the catch study. Perv. Med. 1996, 25, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Haerens, L.; De Bourdeaudhuij, I.; Maes, L.; Cardon, G.; Deforche, B. School-based randomized controlled trial of a physical activity intervention among adolescents. J. Adolesc. Health 2007, 40, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T.; Baranowski, J.; Thompson, D.; Buday, R.; Jago, R.; Griffith, M.J.; Islam, N.; Nguyen, N.; Watson, K.B. Video game play, child diet, and physical activity behavior change a randomized clinical trial. Am. J. Perv. Med. 2011, 40, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Horne, P.J.; Hardman, C.A.; Lowe, C.F.; Rowlands, A.V. Increasing children’s physical activity: A peer modelling, rewards and pedometer-based intervention. Eur. J. Clin. Nutr. 2009, 63, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Hardman, C.A.; Horne, P.J.; Fergus Lowe, C. Effects of rewards, peer-modelling and pedometer targets on children’s physical activity: A school-based intervention study. Psychol. Health 2011, 26, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Ezendam, N.P.; Brug, J.; Oenema, A. Evaluation of the web-based computer-tailored fataintphat intervention to promote energy balance among adolescents: Results from a school cluster randomized trial. Arch. Pediatr. Adolesc. Med. 2012, 166, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Wake, M.; Baur, L.A.; Gerner, B.; Gibbons, K.; Gold, L.; Gunn, J.; Levickis, P.; McCallum, Z.; Naughton, G.; Sanci, L.; et al. Outcomes and costs of primary care surveillance and intervention for overweight or obese children: The LEAP 2 randomised controlled trial. BMJ 2009, 339. [Google Scholar] [CrossRef] [PubMed]
- Colchico, K.; Zybert, P.; Basch, C.E. Effects of after-school physical activity on fitness, fatness, and cognitive self-perceptions: A pilot study among urban, minority adolescent girls. Am. J. Public Health 2000, 90, 977–978. [Google Scholar] [PubMed]
- Wilson, D.K.; Van Horn, M.L.; Kitzman-Ulrich, H.; Saunders, R.; Pate, R.; Lawman, H.G.; Hutto, B.; Griffin, S.; Zarrett, N.; Addy, C.L.; et al. Results of the ”active by choice today” (act) randomized trial for increasing physical activity in low-income and minority adolescents. Health Psychol. 2011, 30, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Erwin, H.E.; Beighle, A.; Morgan, C.F.; Noland, M. Effect of a low-cost, teacher-directed classroom intervention on elementary students’ physical activity. J. Sch. Health 2011, 81, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Gutin, B.; Owens, S. Role of exercise intervention in improving body fat distribution and risk profile in children. Am. J. Hum. Biol. 1999, 11, 237–247. [Google Scholar] [CrossRef]
- Jones, R.A.; Riethmuller, A.; Hesketh, K.; Trezise, J.; Batterham, M.; Okely, A.D. Promoting fundamental movement skill development and physical activity in early childhood settings: A cluster randomized controlled trial. Pediatr. Exerc. Sci. 2011, 23, 600–615. [Google Scholar] [PubMed]
- Burke, V.; Milligan, R.A.; Thompson, C.; Taggart, A.C.; Dunbar, D.L.; Spencer, M.J.; Medland, A.; Gracey, M.P.; Vandongen, R.; Beilin, L.J. A controlled trial of health promotion programs in 11-year-old using physical activity ”enrichment” for higher risk children. J. Pediatr. 1998, 132, 840–848. [Google Scholar] [CrossRef]
- Hopper, C.A.; Munoz, K.D.; Gruber, M.B.; Nguyen, K.P. The effects of a family fitness program on the physical activity and nutrition behaviors of third-grade children. Res. Q. Exerc. Sport 2005, 76, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Manios, Y.; Moschandreas, J.; Hatzis, C.; Kafatos, A. Health and nutrition education in primary schools of crete: Changes in chronic disease risk factors following a 6-year intervention programme. Br. J. Nutr. 2002, 88, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.W.; McAuley, K.A.; Barbezat, W.; Strong, A.; Williams, S.M.; Mann, J.I. Apple project: 2-y findings of a community-based obesity prevention program in primary school age children. Am. J. Clin. Nutr. 2007, 86, 735–742. [Google Scholar] [PubMed]
- Webber, L.S.; Catellier, D.J.; Lytle, L.A.; Murray, D.M.; Pratt, C.A.; Young, D.R.; Elder, J.P.; Lohman, T.G.; Stevens, J.; Jobe, J.B.; et al. Promoting physical activity in middle school girls: Trial of activity for adolescent girls. Am. J. Perv. Med. 2008, 34, 173–184. [Google Scholar] [CrossRef] [PubMed]
- Kalavainen, M.P.; Korppi, M.O.; Nuutinen, O.M. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. Int. J. Obes. 2007, 31, 1500–1508. [Google Scholar] [CrossRef] [PubMed]
- Toruner, E.K.; Savaser, S. A controlled evaluation of a school-based obesity prevention in Turkish school children. J. Sch. Nurs. 2010, 26, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Balas-Nakash, M.; Benitez-Arciniega, A.; Perichart-Perera, O.; Valdes-Ramos, R.; Vadillo-Ortega, F. The effect of exercise on cardiovascular risk markers in mexican school-aged children: Comparison between two structured group routines. Salud Publica Mex. 2010, 52, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Okely, A.D.; Collins, C.E.; Morgan, P.J.; Jones, R.A.; Warren, J.M.; Cliff, D.P.; Burrows, T.L.; Colyvas, K.; Steele, J.R.; Baur, L.A. Multi-site randomized controlled trial of a child-centered physical activity program, a parent-centered dietary-modification program, or both in overweight children: The hikcups study. J. Pediatr. 2010, 157, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Martinez Vizcaino, V.; Salcedo Aguilar, F.; Franquelo Gutierrez, R.; Solera Martinez, M.; Sanchez Lopez, M.; Serrano Martinez, S.; Lopez Garcia, E.; Rodriguez Artalejo, F. Assessment of an after-school physical activity program to prevent obesity among 9- to 10-year-old children: A cluster randomized trial. Int. J. Obes. 2008, 32, 12–22. [Google Scholar] [CrossRef] [PubMed]
- DeVault, N.; Kennedy, T.; Hermann, J.; Mwavita, M.; Rask, P.; Jaworsky, A. It’s all about kids: Preventing overweight in elementary school children in Tulsa, OK. J. Am. Diet. Assoc. 2009, 109, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.W.; McAuley, K.A.; Barbezat, W.; Farmer, V.L.; Williams, S.M.; Mann, J.I. Two-year follow-up of an obesity prevention initiative in children: The apple project. Am. J. Clin. Nutr. 2008, 88, 1371–1377. [Google Scholar] [PubMed]
| Type of INT | Duration (Frequency) | Sample (Characteristics) | FU | Articles and Description | Drop-Out (%) | Results Date | Outcomes and Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ant | PA | SB | Diet | Psy | Others | |||||||
| Behavioral and Social Approach | 20 wk (3×/wk, 20 min) | 97 (4.1 y) | 6 wk | Jones (2011) [51] Structured lessons and unstructured activities with equipment | 11 | 6 mo FU | ↔ | ↑ | ↔ | Movement skills: ↑ | ||
| 9 mo | 4997 (6.3 y) | 4 y | Plachta-Danielzik (2007) [26] Messages to increase PA, healthy eating and decrease SB | 65 | 4 y FU | ↔ | ↔ | ↔ | Incidence of OW: ↑ | |||
| 9 mo | 4997 (6.3 y) | 8 y | Plachta-Danielzik (2011) [27] Messages to increase PA, healthy eating and decrease SB | 76 | 8 y FU | ↔ | ↔ | ↔ | Lifestyle: ↔ BP: ↔ | |||
| 4 mo (5×/wk, 40 min) | 79 (7–11 y, OB) | 4 mo | Gutin (1999) [50] Physical training 5 d/wk, 40 min | 11 | End of INT | ↑ | ↑ | ↔ | Insulin: ↑ Leptin: ↑ Lipids: ↔ BP: ↔ Left ventricle: ↔ Hemodynamic: ↔ | |||
| 4 mo FU | ↔ | ↑ | ↔ | Insulin: ↔ Leptin: ↔ Lipids: ↔ BP: ↔ Left ventricle: ↔ Hemodynamic: ↔ | ||||||||
| (12×) | 386 (7–11 y) | 14 wk | Hardman (2011) [44] (1) Peer-modeling, pedometer step goals and tangible rewards to increase PA; (2) same INT, without rewards | 39 | During INT | ↔ | (1) ↑↑ (2) ↑ | |||||
| 14 wk FU | ↔ | (1) ↑ (2) ↑↑ | ||||||||||
| 12 wk (4×) | 163 (7.4 ± 1.6 y) | 9 and 15 mo | McCallum (2007) [21] LEAP: GP consultations targeting change in nutrition, PA, SB supported with materials | 10 | 9 mo FU | ↔ | ↑ | ↑ | ↔ | |||
| 15 mo FU | ↔ | ↔ | ↑ | ↔ | ||||||||
| 12 wk (4×) | 258 (7.4 ± 1.6 y) | 6 and 12 mo | Wake (2009) [46] LEAP 2: Consultations with GP targeting change in nutrition, PA, SB supported with materials | 6 | 6 mo FU | ↔ | ↔ | ↔ | ↔ | |||
| 12 mo FU | ↔ | ↔ | ↔ | ↔ | ||||||||
| 20 wk (5×/wk, 30 min) | 238 (8–9 y) | 12 mo | Hopper (2005) [53] School-based and home programs for PA and nutrition | N/A | End of INT | ↔ | ↔ | ↑ | Knowledge: ↑ Cholesterol: ↔ | |||
| 12 mo FU | ↔ | ↔ | ↑ | Knowledge: ↔ Cholesterol: ↔ | ||||||||
| 20 wk (15×, 90 min) | 70 (8 y) | 6 mo | Kalavainen (2007) [57] Nutrition and PA education, decrease SB and behavioral therapy | 3 | End of INT | ↑ | ||||||
| 6 mo FU | ↔ | |||||||||||
| (8×) | 100 (9–11 y) | 12 wk | Horne (2009) [43] Peer modeling, rewards and pedometer feedback to increase PA | 11 | During INT | ♂: ↑ ♀: ↑ | ||||||
| 12 wk FU | ♂: ↔ ♀: ↑ | |||||||||||
| 10 wk (7×, 40–120 min) | 84 (9 y, OW and OB) | 12 mo | Toruner (2010) [58] Games and skill building activities on perception of competence, PA, nutrition, SB and goal setting + parent training | 4 | 3 mo FU | ↔ | Children knowledge: ↑ Parents knowledge: ↑ | |||||
| 12 mo FU | ↑ | |||||||||||
| 24 wk (3×/wk, 90 min) | 1119 (9.4 ± 0.7 y) | 9 mo | Martinez Vizcaino (2008) [61] Afterschool recreational, non-competitive PA | 7 | 9 mo FU | ↔ | Triceps skinfold: ↑ Apolipoprotein B: ♂: ↓, ♀: ↔ Apolipoprotein A: ♂: ↑, ♀: ↔ Cholesterol: ↔ Triglycerides: ↔ BP: ↔ except ♂: ↓dBP | |||||
| 6 h, (1×) | 153 (10–12 y) | 2 mo | Baranowski (2011) [42] 2 games to provide practical knowledge related to change goals | 13 | 2 mo FU | ↔ | ↔ | ↑ | ||||
| 6 mo (18×, 2 h) | 116 (INT 10.3 ± 1.3 y) | 6 mo | Sacher (2010) [24] Group education and PA session (MEND) | 31 | End of INT | ↑ | ↑ | ↑ | ↑ | Cardiovascular fitness: ↑ | ||
| 6 mo FU | ↑ | ↑ | ↔ | ↑ | Cardiovascular fitness: ↑ | |||||||
| 20 wk (4×/wk, 19 min ) | 800 (11 y) | 6 mo | Burke (1998) [52] 2 INT: (1) Daily fitness sessions + nutrition; (2) Enriched daily fitness sessions for “at risk” children + nutrition | 10 | End of INT | (1) ♂: ↑ ♀: ↔ | ↔ | ↔ | ↔ | Cardiovascular fitness: ↑ Cholesterol: ↑ BP: ↔ Triceps skinfold ♀: ↑, ♂: ↔ | ||
| (2) ♂: ↔ ♀ :↑ | ↔ | ↓ | ↔ | Cardiovascular fitness: ↑ Cholesterol: ↑ for ♀ only BP: ↔Triceps skinfold: ↑ | ||||||||
| 6 mo FU | (1) ♂: ↔ ♀: ↔ | ↔ | ↔ | ↔ | Cardiovascular fitness: ↑ for ♀ Cholesterol: ↑ BP: ↔ Triceps skinfold ♀: ↑, ♂: ↔ | |||||||
| (2) ♂: ↔ ♀ :↔ | ↔ | ↔ | ↔ | Cardiovascular fitness: ↑ for ♀ Cholesterol: ↑ BP: ↔ Triceps skinfold: ↔ | ||||||||
| 17 wk (4×/wk, 2 h) | 1422 (11.3 ± 0.6 years, low income and minority) | 2 wk | Wilson (2011) [48] Promotion of behavioral skills to increase PA | 25 | Mid-INT | ↑ | ↑ | |||||
| 2 wk FU | ↔ | ↑ | ||||||||||
| 4 wk (1×/wk, 40 min + 3× 90 min) | 729 (12 y) | 3 and 7 mo | Cui (2012) [19] Workshops and lessons focused on food choices, PA and SB | 6 | 3 mo FU | ↔ | ↔ | |||||
| 7 mo FU | ↔ | ↑ | ||||||||||
| 12 wk (1×/wk, 90 min) | 291 (INT 12.2 ± 1.1 y, Portuguese) | 3 and 9 mo | Araujo-Soares (2009) [22] Sessions on health behaviors, PA, diet, physical and psychosexual development, prevention of risk behaviors (STD, smoking, alcohol), assertiveness | 33 | End of INT | ↔ | ↔ | Coping planning: ↑ | ||||
| 3 mo FU | ↑ | ↔ | ||||||||||
| 9 mo FU | ↑↑ | ↔ | ||||||||||
| 5 mo FU | ↔ | ↑ | ||||||||||
| (2) ↑ | ↔ | BP: ↑, mostly sBP Triglycerides: ↑ Insulin resistance and level: ↔ Glucose: ↔ Cholesterol: ↔ | ||||||||||
| 6 d (1h, 12×) | 1057 (12.4 ± 1.2 y) | 3, 6 and 12 mo | Jemmott (2011) [18] Increase fruits and vegetables intake and PA, decrease smoking and alcohol | 3 | 3 mo FU | ↑↑↑ | ↑↑↑ | ↑↑↑ | Knowledge: ↑↑↑ Drugs: ↔ Alcohol: ↔ | |||
| 6 mo FU | ↑↑ | ↑↑ | ↑↑ | Knowledge: ↑↑ Drugs: ↔ Alcohol: ↔ | ||||||||
| 12 mo FU | ↑ | ↑ | ↑ | Knowledge: ↑ Drugs: ↔ Alcohol: ↔ | ||||||||
| 10 wk (8×, 15 min) | 883 (INT 12.7 ± 0.7 y) | 4 and 24 mo | Ezendam (2012) [45] Computer-tailored intervention with feedback | 14 | 4 mo FU | ↔ | ↓ | ↔ | ↑ | |||
| 24 mo FU | ↔ | ↔ | ↔ | ↑ | ||||||||
| (3×) | 1213 (12.7 ± 0.5 y) | 1 and 6 mo | Prins (2012) [17] (1) Lessons + homework on PA self-regulation with feedback; (2) same INT without feedback | 32 | 1 mo FU | ↔ | ↔ | |||||
| 6 mo FU | ↔ | ↔ | ||||||||||
| 9 wk (1×/wk, 55 min) | 473 (12.8 ± 1.1 y) | 6 mo | Latif (2011) [20] 2 INT: (1) increase fruits and vegetables consumption; (2) increase PA, skill building activities for both and goal settings | 24 | End of INT | ↑ | ↑↑FJ ↑LV | ↔ | ||||
| 6 mo FU | ↑↑ | ↑FJ ↓LV | ↔ | |||||||||
| 60 min (1×) | 320 (13.1 ± 0.8 y) | 3 mo | Haerens (2007) [41] Computer tailored intervention to increase PA with feedback | 12 | 3 mo FU | ↑ School PA | but ↔ leisure and total PA | |||||
| 20 min (2×) | 1053 (14.5 ±1.4 y) | 1 and 3 mo | De Bourdeaudhuij (2010) [16] Computer-tailored advice on PA | 53 | 1 mo FU | ↑ | ||||||
| 3 mo FU | ↑↑ | |||||||||||
| 12 min (1×) | 604 (15.3 ± 1.09 y) | 3 and 12 mo | Werch (2005) [15] One on one screening and consultation on PA and alcohol use | 15 | 3 mo FU | ↑ | Alcohol: ↑ Drug use: ↑ Cigarette: ↔ | |||||
| 12 mo FU | ↔ | Alcohol: ↑ Drug use: ↔ Cigarette: ↑ | ||||||||||
| Informational approach | 72 mo (2×/wk, 45 min + 13–17 h) | 716 (start of INT: 6.3 ± 0.3 y) | 48 mo | Manios (2006) [37] 4 y FU of a multi-component workbooks, nutrition and PA education and PA lessons (end of INT results and outcomes are cited in Manios (2002) [54]) | 41 | End of INT | ↔ | ↑ | ↓ | Lipids: ↑ Cardiovascular fitness: ↑ | ||
| 41 | 48 mo FU | ♂: ↑ ♀: ↔ | ||||||||||
| 1 month | 579 (INT 10.2 ± 1.0 y) | 3 mo | Francis (2010) [33] Lessons on nutrition education and PA | 18 | 3 mo FU | ↔ | ↑ | Knowledge: ↑ | ||||
| 5–7 days (2 h) | 459 (12.5 ± 0.6 y) | 3 mo | Spruijt-Metz (2008) [32] Theory-based classroom media to increase PA and decrease SB | N/A | 3 mo FU | ↔ | ↔ | ↑ | ↑ | |||
| 1 hour | 693 (13.8 ± 1.4 y) | 4 wk | Schwarzer (2010) [31] Theory-guided intervention to increase PA | 23 | 4 wk FU | ↑ | ||||||
| Environmental approach | 36 mo | 5106 (start of INT: 8–11 y) | 5 y | McKenzie (2003) [39] CATCH 5 y FU: food service modification, increase PA and classroom health curricula (during INT results and outcomes are cited in Webber (1996) [40]) | 21 | During INT (30 mo) | ↓ | ↑ | ↑ | ↑ | BP: ↔ Cardiovascular fitness: ↔ Skinfold: ↔ Lipids: ↔ Cholesterol: ↑ | |
| N/A | 5 y. FU | ↑ | ||||||||||
| 24 mo | 3502 (11–14 y, adolescent girls) | 12 mo | Webber (2008) [56] TAAG: increase opportunities, support, incentives for PA | N/A | End on INT | ↔ | ↔ | ↔ | Cardiovascular fitness: ↔ | |||
| N/A | 12 mo FU | ↔ | ↑ | ↑ | Cardiovascular fitness: ↔ | |||||||
| Type of INT | Duration (Frequency) | Sample (Characteristics) | FU | Articles and Description | Drop-Out (%) | Results Date | Outcomes and Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ant | PA | SB | Diet | Psy | Others | |||||||
| Behavioral and social approach | 4 mo (5×/wk, 5–10 min) | 213 (5–11 y) | 3 mo | Erwin (2011) [49] Teacher-directed classroom-based PA breaks | 50 | End of INT | ↑ | |||||
| 3 mo FU | ↑ | |||||||||||
| N/A | 43 (8–14 y) | N/A | Hermann (2006) [29] Afterschool education and gardening on nutrition and PA | N/A | N/A | ↑ | ↑ | |||||
| 12 wk (1×/wk, 90 min) | 1529 (8–11 y, girls) | 5 mo | Pettee Gabriel (2011) [23] Training for running event and physical, psychological and social development | 43 | End of INT | ↑ | ↑ | |||||
| 5 mo FU | ↔ | ↑ | ||||||||||
| 23 wk (10×, 2 h) | 165 (8 y, OW and OB) | 6 and 12 mo | Okely (2010) [60] (1) Parent-centered diet program; (2) child-centered PA program; or (3) combination of both; all include face-to-face sessions, homework and a prevention program | 36 | 6 mo FU | ↑ | Lipids: ↔ Insulin: ↑ for group (1) only Glucose: ↔ BP: ↔ | |||||
| 12 mo FU | ↑ | Lipids: ↔ Insulin: ↔ Glucose: ↔ BP: ↑sBP from group (2) only | ||||||||||
| 6 mo (20 meetings, 1 h) | 63 (9.8 ± 1.3 y OB) | 6 mo | Epstein (2004) [25] Stimulus control or reinforcement to reduce SB and substitute for PA, enhance light diet and behavior change techniques | 3 | End of INT | ↑ | ↑ | ↑ | ↑ | |||
| 6 mo FU | ↑ | ↔ | ↔ | ↔ | ||||||||
| 12 wk (5×/wk, 10–30 min) | 319 (10 y) | 6 mo | Balas-Nakash (2010) [59] 2 INT: (1) 10 min of aerobic exercises; (2) 30 min of aerobic exercises | 33 | 6 mo FU | (1) ↑ | ↔ | BP: ↑, mostly dBP → Triglycerides: ↑ Insulin resistance and level: ↔ Glucose: ↔ Cholesterol: ↔ | ||||
| (2) ↑ | ↔ | BP: ↑, mostly sBP Triglycerides: ↑ Insulin resistance and level: ↔ Glucose: ↔ Cholesterol: ↔ | ||||||||||
| 9 mo (6×/wk, 30 min) | 140 (INT 10.1 y) | 3 wk | DeVault (2009) [62] PA (aerobic, strength and endurance) and nutrition lessons | 39 | 3 wk FU | ↔ | ↑ | ↑ | Knowledge: ↑ Aerobic fitness: ↑ | |||
| 12 wk (3×/wk) | 30 (12.6 ± 1.0 y, Hispanic and African American girls) | 1 wk | Colchico (2000) [47] Activities and exercise sessions | 0 | 1 wk FU | ↑ | ↑ | ↑ | Cardiovascular fitness: ↑ Muscle strength: ↑ Flexibility: ↑ | |||
| 10–25 min (1×) | 454 (13–14 y) | 3 mo | Werch (2003) [14] Prevent alcohol use and promote PA | 3 | 3 mo FU | ↑ | ↑ | Alcohol: ↑ | ||||
| 10 mo (8 h/wk) | 30 (13.5 ± 2.1 y, OB) | 6 mo | Deforche (2004) [28] Dietary, PA, psychological support, medical supervision | 20 | During INT | ↑ | ↑ | ↑ | ↔ | Social support: ↑ | ||
| 6 mo FU | ↑ | ↓ | ↓ | ↔ | Modelling for siblings: ↓ Modelling for parents: ↔ Social support: ↓ | |||||||
| Informational approach | 48 mo | 2215 (8–12 y) | 9 mo | McDermott (2010) [36] Media campaign to encourage PA | N/A | 9 mo FU | ↑ | |||||
| 1× | 509 (INT 8.3 y) | Several wk | Stahl (2011) [30] One motivational clinical visit to increase PA, healthy eating and decrease SB | 25 | Several wk FU | ↑ | ↑ | ↑ | ||||
| 11 mo | 57 (8.8 ± 0.8 y, Chinese American) | 2 wk, 1 and 6 mo | Chen (2008) [35] Mailed education package and tailored materials | 26 | 6 mo FU | ↑ | ↑ | ↓ | ↑ | Child Knowledge: ↑ Parent Knowledge: ↔ | ||
| 3 mo | 295 (9–13 y) | 3 mo | Balamurugan (2005) [34] Paid radio advertisement to promote PA | N/A | 3 mo FU | ↑ | ↑ | |||||
| Environmental approach | 24 mo | 554 (start of INT: 7.7 ± 1.8 y) | 24 mo | Taylor (2008) [63] 2 y FU of APPLE: encouraging healthy eating and increase PA with community activity coordinators (end of INT results and outcomes are cited in Taylor (2007) [55]) | 24 | During INT | ↑ | sBP: ↑ | ||||
| End of INT | ↑ | ↑ | ↔ | ↑ | BP: ↔ Cardiovascular fitness: ↔ | |||||||
| 24 mo FU | ↑ | ↑ | ||||||||||
| 12 mo | 1594 (17.7 ± 0.6 y, adolescent girls) | 36 mo | Pate (2007) [38] LEAP 2: increase PA through changes in practices and school environment | 34 | 36 mo FU | ↔ | ↑ | |||||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, S.; Häcker, A.-L.; Henderson, M.; Barnett, T.; Mathieu, M.-E.; Pagani, L.; Bigras, J.-L. Physical Activity Programs with Post-Intervention Follow-Up in Children: A Comprehensive Review According to Categories of Intervention. Int. J. Environ. Res. Public Health 2016, 13, 664. https://doi.org/10.3390/ijerph13070664
Nguyen S, Häcker A-L, Henderson M, Barnett T, Mathieu M-E, Pagani L, Bigras J-L. Physical Activity Programs with Post-Intervention Follow-Up in Children: A Comprehensive Review According to Categories of Intervention. International Journal of Environmental Research and Public Health. 2016; 13(7):664. https://doi.org/10.3390/ijerph13070664
Chicago/Turabian StyleNguyen, Sally, Anna-Luisa Häcker, Melanie Henderson, Tracie Barnett, Marie-Eve Mathieu, Linda Pagani, and Jean-Luc Bigras. 2016. "Physical Activity Programs with Post-Intervention Follow-Up in Children: A Comprehensive Review According to Categories of Intervention" International Journal of Environmental Research and Public Health 13, no. 7: 664. https://doi.org/10.3390/ijerph13070664






