Prevalence of Methicillin-Resistant Staphylococcus aureus and Other Staphylococcus Species in Raw Meat Samples Intended for Human Consumption in Benin City, Nigeria: Implications for Public Health
Abstract
:1. Introduction
2. Materials and Methods
2.1. Collection of Samples
2.2. Sample Preparation and Isolation
2.3. Identification of the Staphylococcal Isolates
2.4. Molecular Identification by Polymerase Chain Reaction (PCR)
2.4.1. Genomic DNA Extraction
2.4.2. PCR for Identification of Staphylococcal Isolates
2.4.3. Sequencing of the 16S rRNA Genes
2.4.4. Specific PCR for the Identification of Staphylococcus Aureus
2.4.5. Specific PCR for the Identification of Methicillin-Resistant Staphylococcus Species
2.4.6. Detection Luk S/F Gene Sequence That Encodes Virulence Determinants in Staphylococci
2.5. Determination of the Antibiotic Resistance Profiles of Staphylococcal Isolates
Antibiotic Susceptibility Testing
2.6. Statistical Analysis
3. Results
3.1. Distribution of the Staphylococci Isolates
3.2. Multidrug Resistance Pattern of the Staphylococcus Species
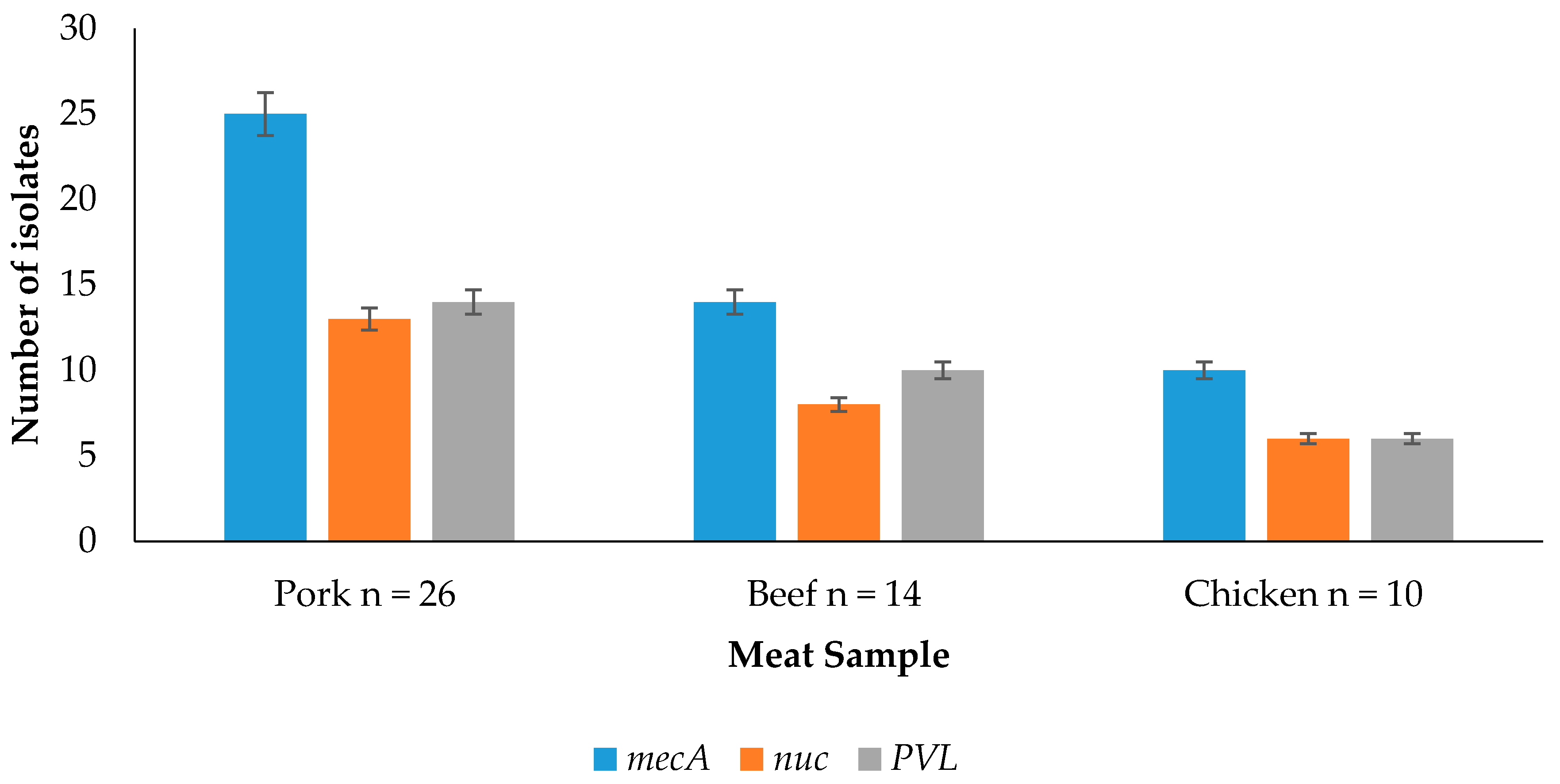
3.3. Detection of Resistance and Virulence Genes from the Meat Samples
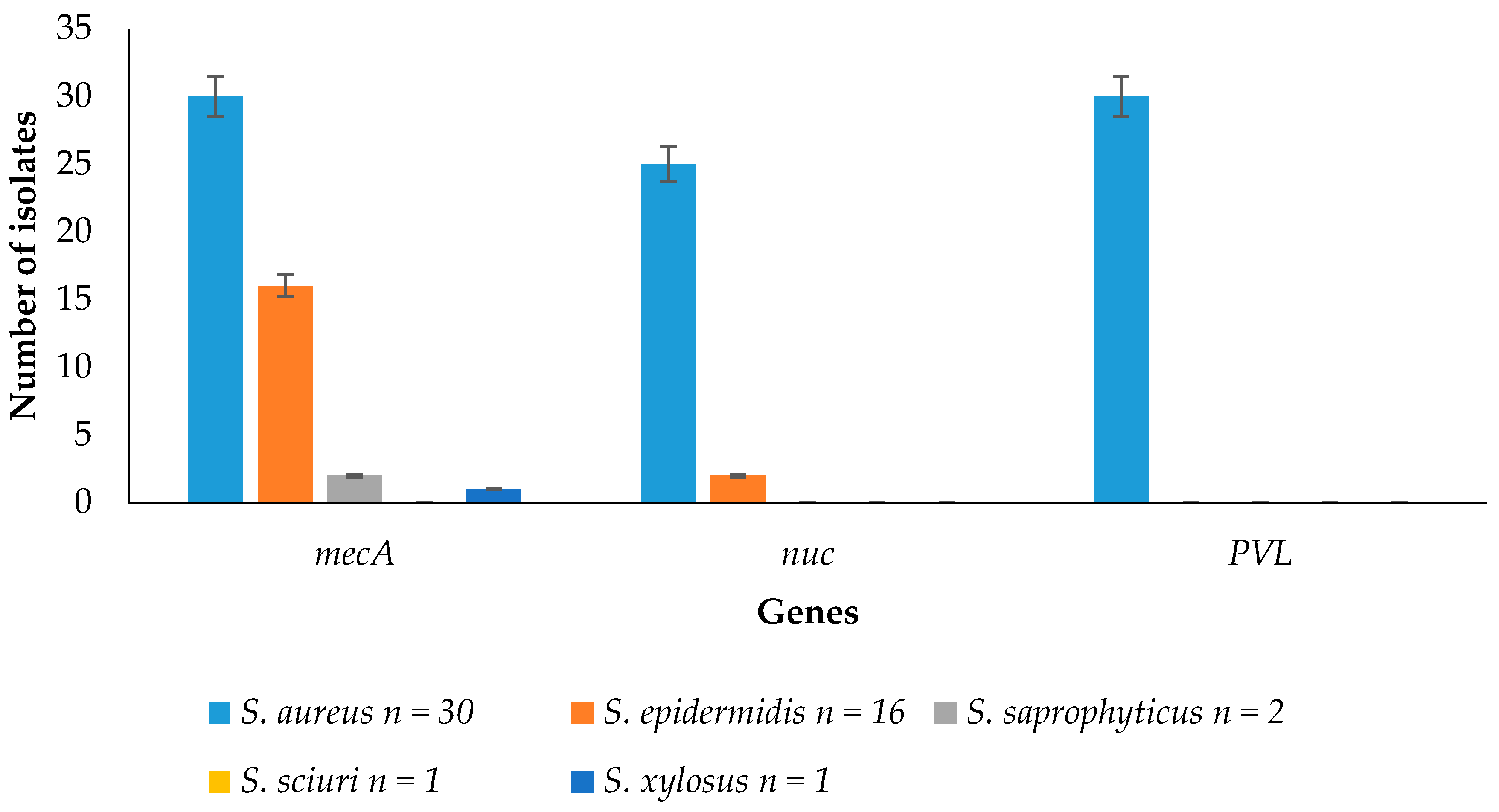
3.4. Detection of Resistance and Virulence Genes from the Staphylococcus Species
4. Discussion
4.1. Distribution of the Staphylococci Isolates
4.2. Multidrug Resistance Pattern of the Staphylococcus Species
4.3. Detection of Resistance and Virulence Genes from the Meat Samples
4.4. Detection of Resistance and Virulence Genes from the Staphylococcus Species
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Igbinosa, E.O.; Beshiru, A.; Akporehe, L.U.; Ogofure, A.G. Detection of methicillin-resistant staphylococci isolated from food producing animals: A public health implication. Vet. Sci. 2016, 3, 1–11. [Google Scholar] [CrossRef]
- Wang, X.; Tao, X.; Xia, X.; Yang, B.; Xi, M.; Meng, J.; Zhang, J.; Xu, B. Staphylococcus aureus and methicillin-resistant Staphylococcus aureus in retail raw chicken in China. Food Control 2013, 29, 103–106. [Google Scholar] [CrossRef]
- Vanegas-López, M.C.; Moreno, E.J.; Rueda, R.V.; Chirivi, S.J.; Garzón, A.; Arévalo, A.S.; Martínez, F.M.; Gardeazábal, P.A.; Baquero, C. Methicillin-resistant Staphylococcus aureus (MRSA) isolated from Colombian foods. Can. Cent. Acad. Art Sci. 2012, 2, 61–67. [Google Scholar] [CrossRef]
- Khalifa, S.M.; Abdel-Rhman, H.S.H.; Abd-El-Galil, K.H.; Habib, E.; Barwa, R. Occurrence and characterization of Staphylococcus aureus in meat and meat products marketed in Mansoura, Egypt. Egypt. J. Med. Microbiol. 2014, 23, 47–56. [Google Scholar] [CrossRef]
- Beshiru, A.; Igbinosa, I.; Igbinosa, E. Antimicrobial resistance of methicillin-resistant staphylococci isolated from food producing animal. 17th International Congress on Infectious Diseases. Int. J. Infect. Dis. 2016, 45, 93. [Google Scholar] [CrossRef]
- Mirzaei, H.; Farhoudi, H.; Tavassoli, H.; Farajli, M.; Monadi, A. Presence and antimicrobial susceptibility of methicillin resistant Staphylococcus aureus in raw and pasteurized milk and ice cream in Tabriz by culture and PCR techniques. Afr. J. Microbiol. Res. 2012, 6, 6224–6229. [Google Scholar] [CrossRef]
- Suleiman, A.; Zaria, L.T.; Grema, H.A.; Ahmadu, P. Antimicrobial resistant coagulase positive Staphylococcus aureus from chickens in Maiduguri, Nigeria. Sokoto J. Vet. Sci. 2013, 11, 51–53. [Google Scholar] [CrossRef]
- Diederen, B.M.W.; van Lo, I.H.M.; Savelkoul, P.; Woudenberg, J.H.C.; Roosendaal, R.; Verhulst, C.; van Keulen, P.H.J.; Kluytmans, J.A.J.W. Low prevalence of non-typable methicillin-resistant Staphylococcus aureus in meat products in the Netherlands. In Session 6: Antimicrobial Resistance; Safe Pork: Verona, Italy, 2007; pp. 398–401. [Google Scholar]
- De Boer, E.; Zwartkruis-Nahuis, J.T.M.; Wit, B.; Huijsdens, X.W.; de Neeling, A.J.; Bosch, T.; van Oosterom, R.A.A.; Vila, A.; Heuvelink, A.E. Prevalence of methicillin-resistant Staphylococcus aureus in meat. Int. J. Food Microbiol. 2009, 134, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Otalu, O.; Junaidu, K.; Chukwudi, E.O.; Jarlath, V.U. Multi-drug resistant coagulase positive Staphylococcus aureus from live and slaughtered chickens in Zaria, Nigeria. Int. J. Poult. Sci. 2011, 10, 871–875. [Google Scholar] [CrossRef]
- Youssef, A.I.; Hamed, D.M. Methicillin resistant Staphylococcus aureus (MRSA) associated with arthritis in broiler farms in Ismailia province, Egypt and its zoonotic potential significance. Suez Canal Vet. Med. J. 2012, 18, 309–322. [Google Scholar]
- Karmi, M. Prevalence of methicillin-resistant Staphylococcus aureus in poultry meat in Qena, Egypt. Vet. World 2013, 6, 711–715. [Google Scholar] [CrossRef]
- Yamada, K.; Wanchun, J.; Ohkura, T.; Murai, A.; Hayakawa, R.; Kinoshita, K.; Mizutani, M.; Okamoto, A.; Namikawa, T.; Ohta, M. Detection of methicillin-resistant Staphylococcus aureus using a specific anti-PBP2a chicken IgY antibody. Jpn. J. Infect. Dis. 2013, 66, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Nnachi, U.A.; Emele, E.F.; Ukaegbu, O.C.; Agah, V.M.; Udu-Ibiam, E.O.; Chukwu, O.S.; Agwu, M.M. Prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in raw meat and meat handlers in Onitsha, Nigeria. Eur. J. Prev. Med. 2014, 2, 9–15. [Google Scholar] [CrossRef]
- Cheesbrough, M. Microbiological test. In District Laboratory Practice in Tropical Countries; Part 2; Cambridge University Press: New York, NY, USA, 2000; p. 442. [Google Scholar]
- Rinsky, J.L.; Nadimpalli, M.; Wing, S.; Hall, D.; Baron, D.; Price, L.B.; Larsen, J.; Stegger, M.; Stewart, J.; Heaney, C.D. Livestock-associated methicillin and multidrug-resistant Staphylococcus aureus is present among industrial, not antibiotic-free livestock operation workers in North Carolina. PLoS ONE 2013, 8, e67641. [Google Scholar] [CrossRef] [PubMed]
- Cruickshank, R.; Duguid, J.P.; Marmion, B.R.; Swain, R.H. Medical Microbiology, 12th ed.; Churchill Livingstone: Edinburgh, UK, 1975. [Google Scholar]
- Ma, A.; Lv, D.; Zhuang, X.; Zhuang, G. Quorum quenching in culturable phyllosphere bacteria from tobacco. Int. J. Mol. Sci. 2013, 14, 14607–14619. [Google Scholar] [CrossRef] [PubMed]
- Tamura, K.; Dudley, J.; Nel, M.; Kumar, S. MEGA 4: Molecular evolutionary genetics analysis (MEGA) software version 4.0. Mol. Biol. Evol. 2007, 24, 1596–1599. [Google Scholar] [CrossRef] [PubMed]
- Altschul, S.F.; Madden, T.L.; Schaffer, A.A.; Zhang, J.; Zhang, Z.; Miller, W.; Lipman, D.J. Gapped BLAST and PSIBLAST: A new generation of protein database search programs. Nucleic Acids Res. 1997, 25, 3389–3402. [Google Scholar] [CrossRef] [PubMed]
- Othman, E.H.; Merza, S.N.; Jubrael, S.M. Nucleotide sequence analysis of methicillin-resistant Staphylococcus aureus in Kurtdistan Region-Iraq. J. Univ. Zakho 2014, 2, 1–13. [Google Scholar]
- Ahmed, B.O.; Elmekki, A.M.; Omer, E.E.; Elhassan, M. Molecular detection of methicillin-resistant Staphylococcus aureus in patients with urinary tract infections in Khartoum State. J. Sci. Technol. 2014, 15, 1–8. [Google Scholar]
- McDonald, R.R.; Antonishyn, A.N.; Hansen, T.; Snook, A.L.; Nagle, E.; Mulvey, R.M.; Levett, N.P.; Horsman, B.G. Development of a triplex real-time PCR assay for detection of panton-valentine leucocidin toxin genes in clinical isolates of methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 2005, 43, 6147–6149. [Google Scholar] [CrossRef] [PubMed]
- Bauer, A.W.; Kirby, M.M.W.; Sherris, J.C.; Turck, M. Antibiotic’s susceptibility testing by a standardized single disk method. Am. J. Clin. Pathol. 1966, 36, 493–496. [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fourth International Supplements; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2014; p. 230. [Google Scholar]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhang, J.; Yu, S.; Wu, Q.; Guo, W.; Huang, J.; Cai, S. Prevalence of Staphylococcus aureus and methicillin-resistant Staphylococcus aureus in retail ready-to-eat foods in China. Front. Microbiol. 2016, 7, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.G.L.; Kasim, K.A.; Lekshmi, M.; Nayak, B.B.; Kumar, S. Incidence of methicillin-resistant staphylococci in fresh seafood. Adv. Microbiol. 2016, 6, 399–406. [Google Scholar] [CrossRef]
- Contreras, A.P.C.; da Silva, N.N.S.; Ferreira, G.C.D.; Ferreira, D.J.; Almeida, D.C.R. Prevalence of methicillin-resistant Staphylococcus aureus in raw hamburgers and ready-to-eat sandwiches commercialized in supermarkets and fast food outlets in Brazil. Food Nutr. Sci. 2015, 6, 1324–1331. [Google Scholar] [CrossRef]
- Alexandra, F.; Britta, K.; Gladys, K.; Beatriz, G.; Katja, A.; Jens-André, H.; Annemarie, K.; Juliane, B.; Bernd, A.; Bernd-Alois, T. Methicillin susceptible and resistant Staphylococcus aureus from farm to fork impact on food safety. Tehnol. Mesa 2011, 52, 60–65. [Google Scholar]
| Staphylococcus Species | Pork Isolates n = 26 (%) | Beef Isolates n = 14 (%) | Chicken Isolates n = 10 (%) | Total n = 50 (%) | p-Value |
|---|---|---|---|---|---|
| S. aureus | 14 (53.85) | 10 (71.43) | 6 (60) | 30 (60) | 0.868 |
| S. epidermidis | 9 (34.62) | 4 (28.57) | 3 (30) | 16 (32) | 0.756 |
| S. saprophyticus | 2 (7.69) | - | - | 2 (4) | 0.422 |
| S. sciuri | 1 (3.85) | - | - | 1 (2) | 0.421 |
| S. xylosus | - | - | 1 (10) | 1 (2) | 0.421 |
| Total | 26 (100) | 14 (100) | 10 (100) | 50 (100) |
| Phenotype Resistance | Number of Isolates n = 50 |
|---|---|
| METR, PENR, CLNR | 50 |
| METR, PENR, CLNR, CHLR, SXTR, KANR | 50 |
| METR, PENR, CLNR, CHLR, SXTR, KANR, AMXR | 48 |
| METR, PENR, CLNR, CHLR, SXTR, KANR, AMXR, CLXR | 47 |
| METR, PENR, CLNR, CHLR, SXTR, KANR, AMXR, CLXR, ERYR | 41 |
| METR, PENR, CLNR, CHLR, SXTR, KANR, AMXR, CLXR, ERYR, VANR | 29 |
| METR, PENR, CLNR, CHLR, SXTR, KANR, AMXR, CLXR, ERYR, VANR, GENR | 7 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Igbinosa, E.O.; Beshiru, A.; Akporehe, L.U.; Oviasogie, F.E.; Igbinosa, O.O. Prevalence of Methicillin-Resistant Staphylococcus aureus and Other Staphylococcus Species in Raw Meat Samples Intended for Human Consumption in Benin City, Nigeria: Implications for Public Health. Int. J. Environ. Res. Public Health 2016, 13, 949. https://doi.org/10.3390/ijerph13100949
Igbinosa EO, Beshiru A, Akporehe LU, Oviasogie FE, Igbinosa OO. Prevalence of Methicillin-Resistant Staphylococcus aureus and Other Staphylococcus Species in Raw Meat Samples Intended for Human Consumption in Benin City, Nigeria: Implications for Public Health. International Journal of Environmental Research and Public Health. 2016; 13(10):949. https://doi.org/10.3390/ijerph13100949
Chicago/Turabian StyleIgbinosa, Etinosa O., Abeni Beshiru, Lucy U. Akporehe, Faith E. Oviasogie, and Owen O. Igbinosa. 2016. "Prevalence of Methicillin-Resistant Staphylococcus aureus and Other Staphylococcus Species in Raw Meat Samples Intended for Human Consumption in Benin City, Nigeria: Implications for Public Health" International Journal of Environmental Research and Public Health 13, no. 10: 949. https://doi.org/10.3390/ijerph13100949






