Factors Associated with Community Participation among Individuals Who Have Experienced Homelessness
Abstract
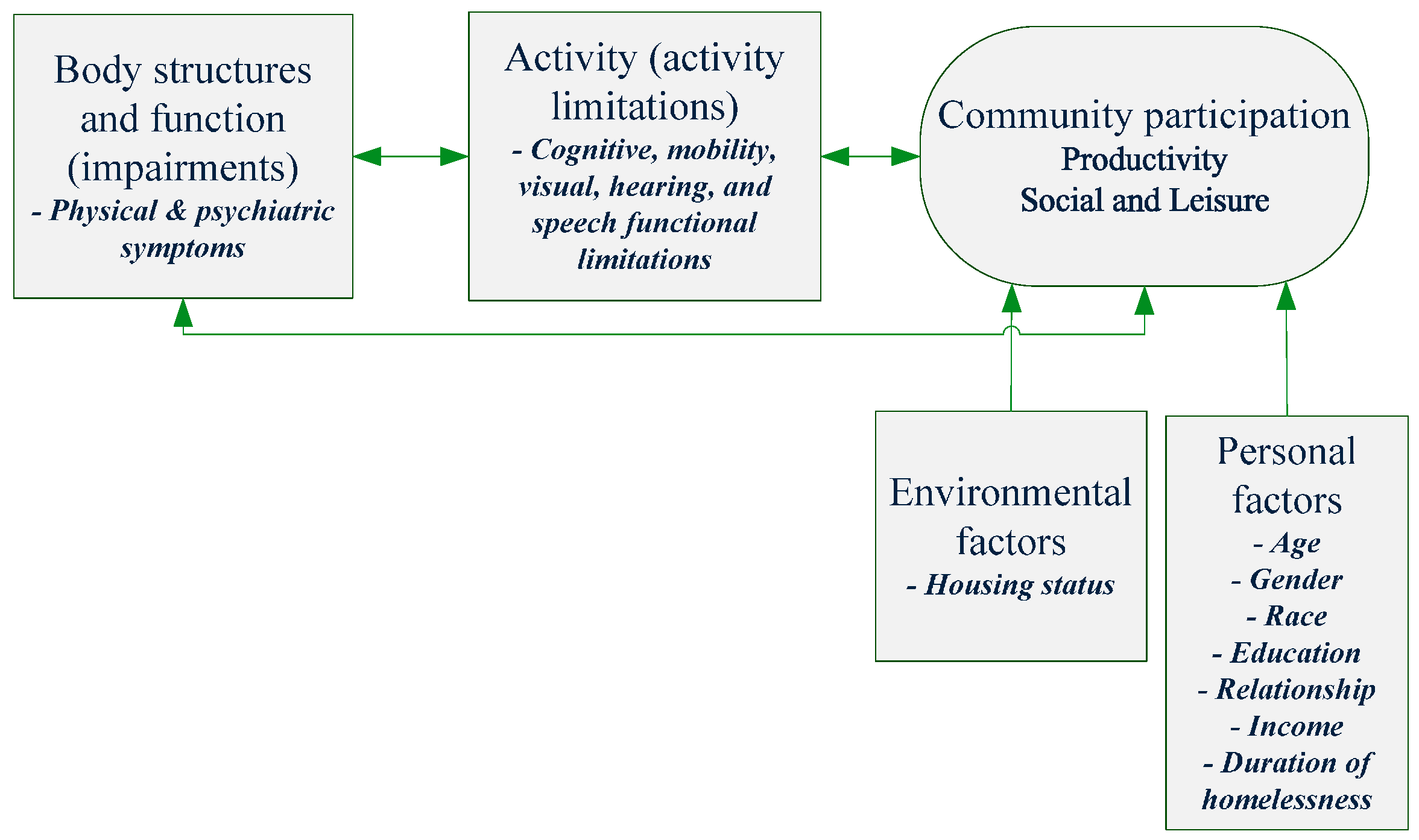
:1. Introduction
2. Methods
2.1. Participants
2.2. Measures
2.2.1. Dependent Variable: Community Participation
2.2.2. Predictor Variables
2.2.3. Psychiatric Symptoms
2.2.4. Physical Symptoms
2.2.5. Cognitive Ability
2.2.6. Other Functional Limitations
2.2.7. Personal and Environmental Factors
2.3. Statistical Analyses
3. Results
| Characteristics | N (%) | Mean (SD) (years) |
|---|---|---|
| Age | 48.76 (10.22) | |
| Gender | ||
| Male | 74 (61.67%) | |
| Female | 46 (38.33%) | |
| Race | ||
| White | 55 (45.83%) | |
| African-American | 52 (43.33%) | |
| Hispanic/Asian/Other | 13 (10.83%) | |
| Education | ||
| Less than high school | 19 (16.10%) | |
| High school graduate or GED | 41 (34.75%) | |
| Some college | 34 (28.81%) | |
| College graduate or more | 24 (20.34%) | |
| Duration of homelessness (days) | 5.31 (6.31) | |
| >1 year | 94 (81.03%) | |
| <1 year | 22 (18.97%) | |
| Housing programs | ||
| Housing search | 40 (33.33%) | |
| Housing placement | ||
| (Housing first) | 34 (28.33%) | |
| (Housing stabilization) | 46 (38.33%) | |
| Relationship status | ||
| Married, life partner, in a relationship | 24 (20.17%) | |
| Single, widowed, separated, divorced | 95 (79.83%) | |
| Living with children | 2 (1.67%) | |
| Disability | 83 (69.75%) | |
| Diagnosis of mental illness | 77 (64.71%) | |
| Substance abuse | 69 (60.00%) | |
| Overall CP | Productivity | Social and Leisure | ||
|---|---|---|---|---|
| Impairment Variables | ||||
| IESR | r = −0.07 | r = 0.16 † | r = −0.16 † | |
| Psychiatric symptoms (CASIG) | r = 0.17 | r = −0.06 | r = −0.13 | |
| Number of physical symptoms | r = −0.06 | r = −0.05 | r = −0.13 | |
| Activity Limitation Variables | ||||
| ACL | r = 0.20 * | r = 0.29 ** | r = 0.11 | |
| Cognitive difficulty (CASIG) | r = −0.19 * | r = −0.01 | r = −0.23 * | |
| Mobility limitation | Yes | 7.13 ** | 0.97 | 6.16 ** |
| No | 9.49 | 1.51 | 7.98 | |
| Visual limitation | Yes | 7.05 * | 0.44 | 6.21 † |
| No | 8.92 | 1.84† | 7.48 | |
| Hearing limitation | Yes | 6.42 | 0.67 | 5.75 † |
| No | 8.71 * | 1.36 † | 7.34 | |
| Speech limitation | Yes | 6.64 † | 1.14 | 5.50 * |
| No | 8.61 | 1.24 | 7.37 | |
| Personal and Environmental Variables | ||||
| Gender | Male | 8.49 | 1.51 * | 6.97 |
| Female | 7.87 | 0.76 | 7.11 | |
| Age | r = −0.17 † | r = −0.20 * | r = −0.12 | |
| Race | White | 8.75 | 1.13 | 7.62 |
| Black | 8.12 | 1.33 | 6.79 | |
| Other | 6.33 | 1.67 | 4.67 | |
| Education | Less than high school | 9.00 | 1.58 | 7.42 |
| High school graduate or GED | 7.00 | 0.85 | 6.15 | |
| Some college | 9.68 | 1.79 | 7.88 | |
| College graduate or more | 7.50 | 0.75 | 6.75 | |
| Homeless duration | >1 year | 7.84 * | 1.04 * | 6.80 † |
| <1 year | 10.55 | 2.18 | 8.36 | |
| Relationship status | Married/life partner/in a relationship | 9.75 † | 1.75 † | 8.00 |
| Single/widowed/separated/divorced | 7.79 | 1.03 | 6.76 | |
| Mental illness | Yes | 7.86 | 1.12 | 6.74 |
| No | 8.93 | 1.40 | 7.52 | |
| Substance use | Yes | 8.83 | 1.43 | 7.39 |
| No | 7.70 | 1.00 | 6.70 | |
| Housing status | Housed through housing programs | 7.24 | 0.83 * | 6.41 * |
| Homeless | 10.28 ** | 2.03 | 8.25 | |
| N | Overall CP | Productivity | Social and Leisure |
|---|---|---|---|
| 118 | 105 | 118 | |
| R2 | 0.16 | 0.22 | 0.17 |
| F-value (** p < 0.01) | 7.00 ** | 9.23 ** | 5.60 ** |
| Variables | standardized β (p-value) | ||
| Cognitive difficulty | −0.16 (0.06) † | -- | −0.19 (0.03) * |
| ACL | -- | 0.26 (0.006) ** | -- |
| Mobility limitation | −0.19 (0.03) * | -- | −0.20 (0.03) * |
| Speech limitation | -- | -- | −0.16 (0.07) † |
| Relationship status | -- | 0.19 (0.03) * | -- |
| Housing status | −0.25 (0.004) ** | −0.27 (0.003) ** | −0.18 (0.04) * |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- National Alliance to End Homelessness. The State of Homelessness in America 2012. Available online: http://www.endhomelessness.org/content/article/detail/4361 (accessed on 5 September 2015).
- Martins, D.C. Experiences of homeless people in the health care delivery system: A descriptive phenomenological study. Public Health Nurs. 2008, 25, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Zlotnick, C.; Robertson, M.J.; Lahiff, M. Getting off the streets: Economic resources and residential exits from homelessness. J. Community Psychol. 1999, 27, 209–224. [Google Scholar] [CrossRef]
- Tsai, J.; Mares, A.S.; Rosenheck, R.A. Does housing chronically homeless adults lead to social integration? Psychiatr. Serv. 2012, 63, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Huebner, R.A.; Johnson, K.; Bennett, C.M.; Schneck, C. Community participation and quality of life outcomes after adult traumatic brain injury. Am. J. Occup. Ther. 2003, 57, 177–185. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Chang, F.; Coster, W.J.; Helfrich, C.A. Community participation measures for people with disabilities: A systematic review of content from an international classification of functioning, disability and health perspective. Arch. Phys. Med. Rehabil. 2013, 94, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.A.; Andersen, R.; Gelberg, L. Applying the gelberg-andersen behavioral model for vulnerable populations to health services utilization in homeless women. J. Health Psychol. 2007, 12, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Gulcur, L.; Tsemberis, S.; Stefancic, A.; Greenwood, R.M. Community integration of adults with psychiatric disabilities and histories of homelessness. Community Ment. Health J. 2007, 43, 211–228. [Google Scholar] [CrossRef] [PubMed]
- Radey, M.; Wilkins, B. Short-term employment services for homeless individuals: Perceptions from stakeholders in a community partnership. J. Soc. Serv. Res. 2010, 37, 19–33. [Google Scholar] [CrossRef]
- Bryant, R.A.; Marosszeky, J.E.; Crooks, J.; Baguley, I.J.; Gurka, J.A. Posttraumatic stress disorder and psychosocial functioning after severe traumatic brain injury. J. Nerv. Ment. Dis. 2001, 189, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Jette, A.M.; Keysor, J.; Coster, W.; Ni, P.; Haley, S. Beyond function: Predicting participation in a rehabilitation cohort. Arch. Phys. Med. Rehabil. 2005, 86, 2087–2094. [Google Scholar] [CrossRef] [PubMed]
- Sveen, U.; Mongs, M.; Røe, C.; Sandvik, L.; Bautz-Holter, E. Self-rated competency in activities predicts functioning and participation one year after traumatic brain injury. Clin. Rehabil. 2008, 22, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Burke, M.A. Active Members of Diverse Communities: Race and the Doing of Diversity. Ph.D. Thesis, Loyola University Chicago, Illinois, IL, USA, August 2010. [Google Scholar]
- Yanos, P.T.; Barrow, S.M.; Tsemberis, S. Community integration in the early phase of housing among homeless persons diagnosed with severe mental illness: Successes and challenges. Community Ment. Health J. 2004, 40, 133–150. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, R.; Peat, G.; Thomas, E.; Croft, P. Factors associated with participation restriction in community-dwelling adults aged 50 years and over. Qual. Life Res. 2007, 16, 1147–1156. [Google Scholar] [CrossRef] [PubMed]
- Burr, J.A.; Caro, F.G.; Moorhead, J. Productive aging and civic participation. J. Aging Stud. 2002, 16, 87–105. [Google Scholar] [CrossRef]
- Solarz, A.; Bogat, G.A. When social support fails: The homeless. J. Community Psychol. 1990, 18, 79–96. [Google Scholar] [CrossRef]
- Wallace, C.J.; Liberman, R.P. Client’s Assessment of Skills, Interests & Goals (CASIG) Manual and Psychometrics; Psychiatric Rehabilitation Consultants: Camarillo, CA, USA, 2002. [Google Scholar]
- Chang, F.-H.; Chang, C.; Cheng, Y. Factors influencing employers’ willingness to hire people with mental illness: Based on planned behavior theory. Formosa J. Ment. Health 2012, 25, 74–105. [Google Scholar]
- Chang, F.-H. Factors associated with community participation among people who are homeless with disabilities. Arch. Phys. Med. Rehabil. 2013, 94. [Google Scholar] [CrossRef]
- Weiss, D.S. The impact of event scale-revised. In Assessing Psychological Trauma and PTSD, 2nd ed.; Wilson, J.P., Keane, T.M., Eds.; Guilford Press: New York, NY, USA, 2004. [Google Scholar]
- Creamer, M.; Bell, R.; Failla, S. Psychometric properties of the impact of event scale-revised. Behav. Res. Ther. 2003, 41, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- United States Census Bureau. Survey of Income and Program Participation (SIPP). Available online: http://www.census.gov/sipp/ (accessed on 5 September 2015).
- Allen, C.K.; Austin, S.L.; David, S.K.; Earhart, C.A.; McCraith, D.B.; Riska-Williams, L. Allen Cognitive Level Screen-5 (ACLS-5) and Large Allen Cognitive Level screen-5 (LACLS-5); ACLS and LACLS Committee: Camarillo, CA, USA, 2007. [Google Scholar]
- Browne, G.; Hemsley, M. Consumer participation in housing: Reflecting on consumer preferences. Australas. Psychiatry 2010, 18, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Browne, G.; Courtney, M. Exploring the experience of people with schizophrenia who live in boarding houses or private homes: A grounded theory study. Contemp. Nurse 2005, 18, 233–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirkpatrick, H.; Byrne, C. A narrative inquiry: Moving on from homelessness for individuals with a major mental illness. J. Psychiatr. Ment. Health Nurs. 2009, 16, 68–75. [Google Scholar] [CrossRef] [PubMed]
- De Ward, S.L.; Moe, A.M. “Like a prison!”: Homeless women’s narratives of surviving shelter. J. Sociol. Soc. Welf. 2010, 37, 115–135. [Google Scholar]
- Burlingham, B.; Andrasik, M.P.; Larimer, M.; Marlatt, A.; Spigner, C. A house is not a home: A qualitative assessment of the life experiences of alcoholic homeless women. J. Soc. Work Pract. Addict. 2010, 10, 158–179. [Google Scholar] [CrossRef]
- McBride, R.G. Survival on the streets: Experiences of the homeless population and constructive suggestions for assistance. J. Multicult. Counse. Dev. 2012, 40, 49–61. [Google Scholar] [CrossRef]
- Reirzes, D.C.; Crimmins, T.J.; Yarbrough, J.; Parker, J. Social support and social network ties among the homeless in a downtown atlanta park. J. Community Psychol. 2011, 39, 274–291. [Google Scholar] [CrossRef]
- Murphy, G.C.; Middleton, J.; Quirk, R.; de Wolf, A.; Cameron, I.D. Predicting employment status at 2 years’ postdischarge from spinal cord injury rehabilitation. Rehabil. Psychol. 2011, 56, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Burns, S.M.; Boyd, B.L.; Hill, J.; Hough, S. Psychosocial predictors of employment status among men living with spinal cord injury. Rehabil. Psychol. 2010, 55, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Brown, V.L.; Riley, M.A. Social support, drug use, and employment among low-income women. Am. J. Drug Alcohol Abuse 2005, 31, 203–223. [Google Scholar] [CrossRef] [PubMed]
- Meadows-Oliver, M. Social support among homeless and housed mothers: An integrative review. J. Psychosoc. Nurs. Ment. Health Serv. 2005, 43, 40–47. [Google Scholar] [PubMed]
- Hwang, S.W.; Kirst, M.J.; Chiu, S.; Tolomiczenko, G.; Kiss, A.; Cowan, L.; Levinson, W. Multidimensional social support and the health of homeless individuals. J. Urban Health 2009, 86, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Grav, S.; Hellzèn, O.; Romild, U.; Stordal, E. Association between social support and depression in the general population: The HUNT study, a cross-sectional survey. J. Clin. Nurs. 2012, 21, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Bhui, K.; Shanahan, L.; Harding, G. Homelessness and mental illness: A literature review and a qualitative study of perceptions of the adequacy of care. Int. J. Soc. Psychiatry 2006, 52, 152–165. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.; Coster, W.J. Conceptualizing the construct of participation in adults with disabilities. Arch. Phys. Med. Rehabil. 2014, 95, 1791–1798. [Google Scholar] [CrossRef] [PubMed]
- Salzer, M.S.; Brusilovskiy, E.; Prvu-Bettger, J.; Kottsieper, P. Measuring community participation of adults with psychiatric disabilities: Reliability of two modes of data collection. Rehabil. Psychol. 2014, 59, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.; Coster, W.J.; Salzer, M.S.; Brusilovskiy, E.; Ni, P.; Jette, A.M. A multidimensional measure of participation for adults with serious mental illnesses. Disabil. Rehabil. 2015. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, F.-H.; Helfrich, C.A.; Coster, W.J.; Rogers, E.S. Factors Associated with Community Participation among Individuals Who Have Experienced Homelessness. Int. J. Environ. Res. Public Health 2015, 12, 11364-11378. https://doi.org/10.3390/ijerph120911364
Chang F-H, Helfrich CA, Coster WJ, Rogers ES. Factors Associated with Community Participation among Individuals Who Have Experienced Homelessness. International Journal of Environmental Research and Public Health. 2015; 12(9):11364-11378. https://doi.org/10.3390/ijerph120911364
Chicago/Turabian StyleChang, Feng-Hang, Christine A. Helfrich, Wendy J. Coster, and E. Sally Rogers. 2015. "Factors Associated with Community Participation among Individuals Who Have Experienced Homelessness" International Journal of Environmental Research and Public Health 12, no. 9: 11364-11378. https://doi.org/10.3390/ijerph120911364





