The Relationship of Policymaking and Networking Characteristics among Leaders of Large Urban Health Departments
Abstract
:1. Introduction
2. Methodology
2.1. Two Datasets
2.2. The Survey
2.3. Contact Network Definitions
2.4. Network Density and Communication Patterns
3. Results
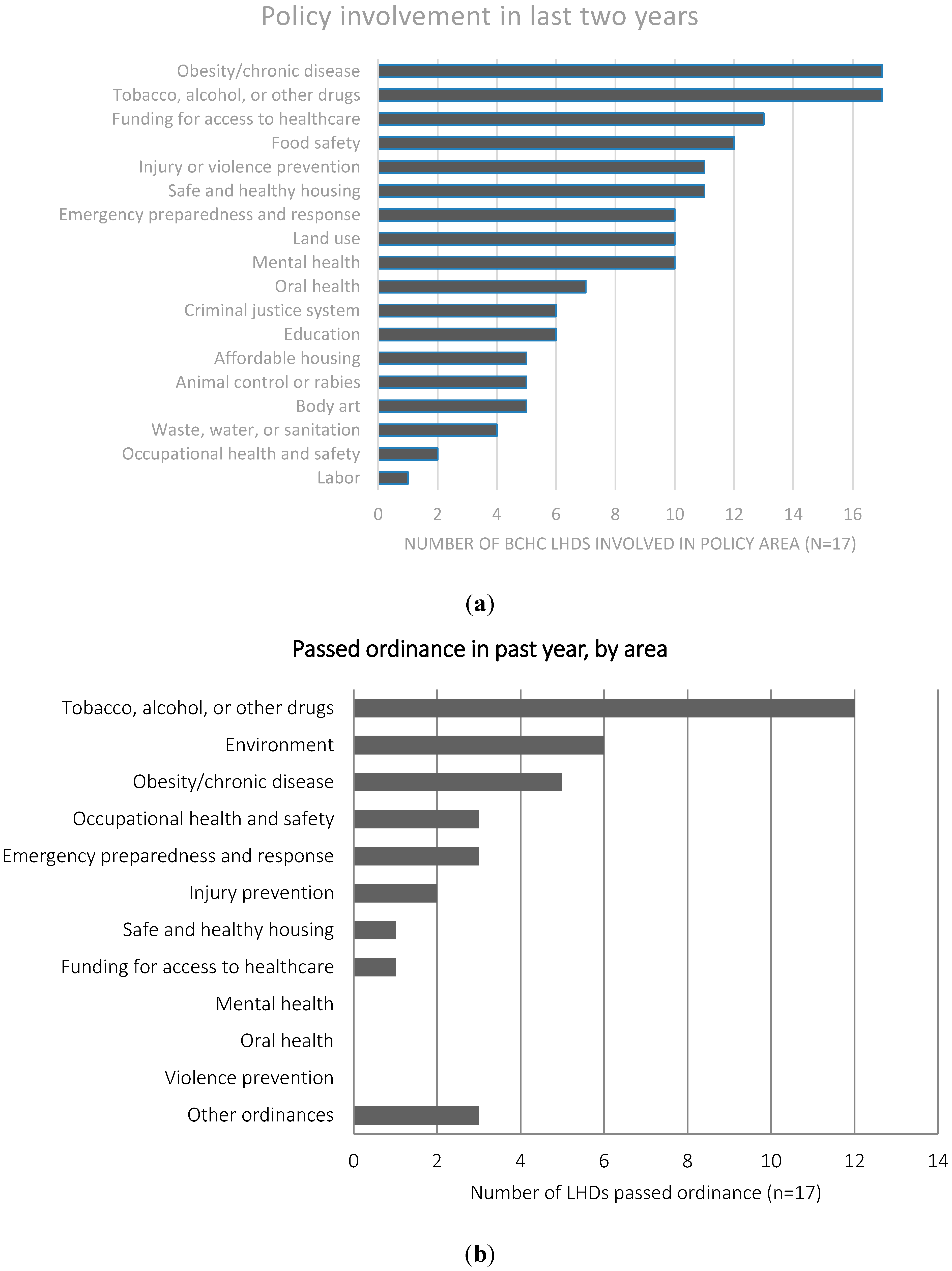
3.1. Policy Activity
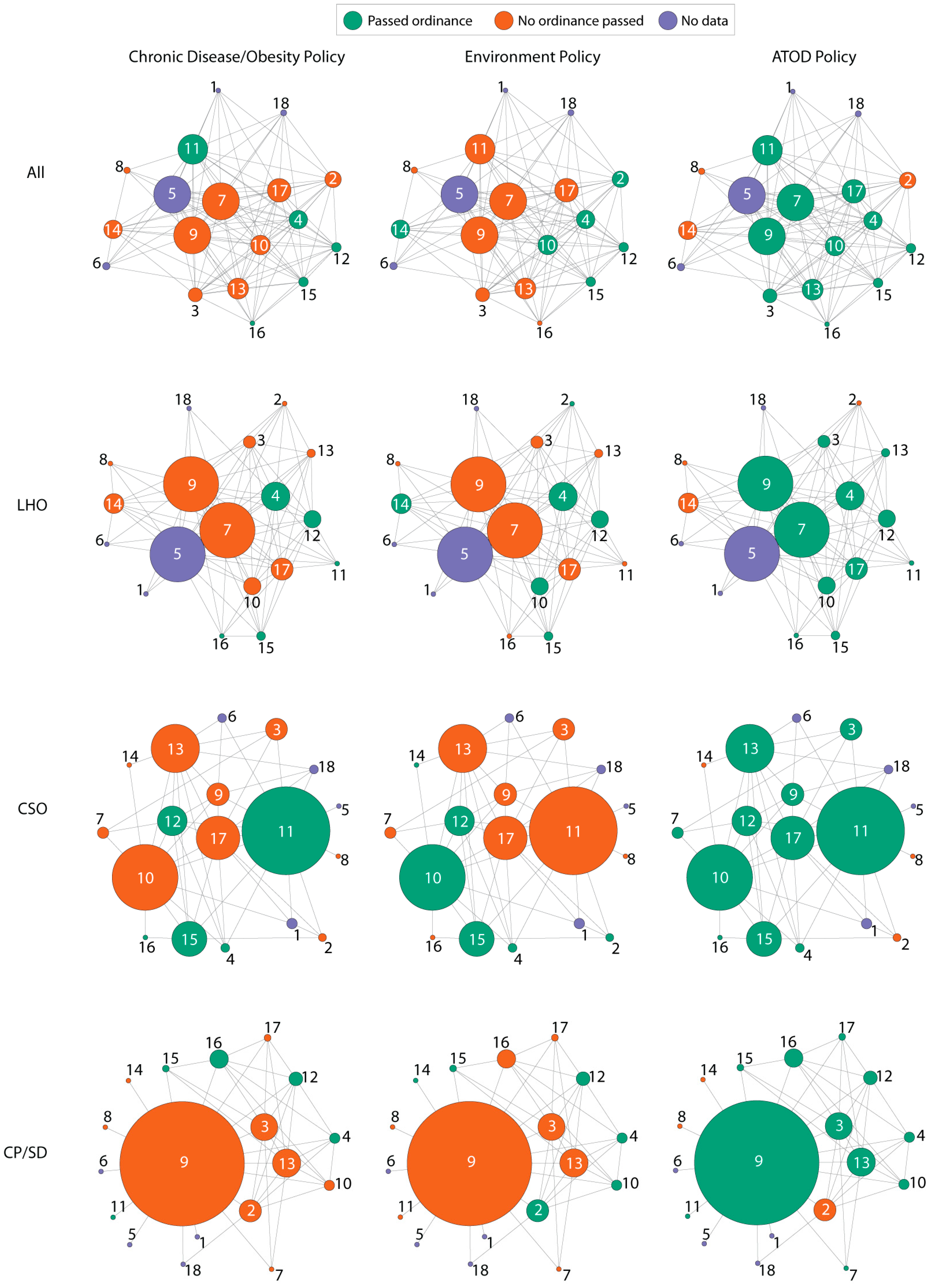
3.2. Contact between BCHC Staff
| LHOs OR (95% CI) | CSO OR (95% CI) | Sr Dep OR (95% CI) | |
|---|---|---|---|
| Edges (constant) | 0.31 (0.13–0.72) * | 0.14 (0.06–0.31) * | 0.02 (0.01–0.08) * |
| LHD leadership linked | Na | 0.87 (0.38–1.98) | 5.91 (2.11–16.59) * |
| >2 years current position | 1.74 (1.01–3.01) * | 2.05 (1.15–3.66) * | 2.71 (1.35–5.44) * |
| Policy homophily | |||
| ATOD | 4.13 (1.83–9.29) * | 5.48 (2.28–13.17) * | 3.10 (1.24–7.71) * |
| Environmental | 0.89 (0.38–2.10) | 0.76 (0.31–1.84) | 1.34 (0.52–3.47) |
| Obesity/Chronic | 1.93 (0.84–4.44) | 0.93 (0.40–2.17) | 2.09 (0.85–5.11) |
4. Discussion
Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- The Public Health System and the 10 Essential Public Health Services. Available online: http://www.cdc.gov/nphpsp/essentialServices.html (accessed on 16 June 2015).
- Corso, L.C.; Wiesner, P.J.; Halverson, P.K.; Brown, C.K. Using the essential services as a foundation for performance measurement and assessment of local public health systems. J. Public Health Manag. Pract. 2000, 6, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Satterfield, D.W.; Murphy, D.; Essien, J.D.; Hosey, G.; Stankus, M.; Hoffman, P.; Beartusk, K.; Mitchell, P.L.; Alfaro Correa, A. Using the essential public health services as strategic leverage to strengthen the public health response to diabetes. Public Health Rep. 2004, 119, 311–321. [Google Scholar] [CrossRef] [PubMed]
- 2013 National Profile of Local Health Departments. Available online: http://www.naccho.org/topics/infrastructure/profile/upload/2013-National-Profile-of-Local-Health-Departments-report.pdf (accessed on 16 June 2015).
- Leep, C.J.; Shah, G.H. Naccho’s national profile of local health departments study: The premier source of data on local health departments for surveillance, research, and policymaking. J. Public Health Manag. Pract. 2012, 18, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.K.; Mueller, N.L. Policy activity and policy adoption in rural, suburban, and urban local health departments. J. Public Health Manag. Pract. 2013, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hearne, S.; Castrucci, B.C.; Leider, J.P.; Rhoades, E.K.; Russo, P.; Bass, V. The future of urban health: Needs, barriers, opportunities, and policy advancement at large urban health departments. J. Public Health Manag. Pract. 2015, 21, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Schwarte, L.; Samuels, S.E.; Boyle, M.; Clark, S.E.; Flores, G.; Prentice, B. Local public health departments in california: Changing nutrition and physical activity environments for obesity prevention. J. Public Health Manag. Pract. 2010, 16, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.W.; Brownson, R.C.; Kruger, J.; Miles, R.; Powell, K.E.; Ramsey, L.T. The effectiveness of urban design and land use and transport policies and practices to increase physical activity: A systematic review. J. Phys. Act. Health 2006, 3, 55–76. [Google Scholar]
- Morello-Frosch, R.; Zuk, M.; Jerrett, M.; Shamasunder, B.; Kyle, A.D. Understanding the cumulative impacts of inequalities in environmental health: Implications for policy. Health Aff. 2011, 30, 879–887. [Google Scholar] [CrossRef] [PubMed]
- Leider, J.P.; Castrucci, B.C.; Hearne, S.; Russo, P. Organizational characteristics of large urban health departments. J. Public Health Manag. Pract. 2015, 21, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Wholey, D.R.; Gregg, W.; Moscovice, I. Public health systems: A social networks perspective. Health Serv. Res. 2009, 44, 1842–1862. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, M.W.; Scutchfield, F.D.; Charnigo, R.; Riddell, M.C.; Mays, G.P. New data, same story? Revisiting studies on the relationship of local public health systems characteristics to public health performance. J. Public Health Manag. Pract. 2010, 16, 110–117. [Google Scholar] [PubMed]
- Improving Public Health System Performance through Multiorganizational Partnerships. Available online: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2995603/ (accessed on 16 June 2015).
- Mays, G.P.; Scutchfield, F.D.; Bhandari, M.W.; Smith, S.A. Understanding the organization of public health delivery systems: An empirical typology. Milbank Q. 2010, 88, 81–111. [Google Scholar] [CrossRef] [PubMed]
- Sandström, A.; Carlsson, L. The performance of policy networks: The relation between network structure and network performance. Policy Stud. J. 2008, 36, 497–524. [Google Scholar] [CrossRef]
- Big Cities Health Inventory. Available online: http://www.cityofchicago.org/dam/city/depts/cdph/statistics_and_reports/SR_2003BCHI.pdf (accessed on 16 June 2015).
- Lumpkin, J. Life in the Big City: Building a Culture of Health. J. Public Health Manag. Pract. 2015, 21, S93–S94. [Google Scholar] [CrossRef] [PubMed]
- Fielding, J.E. Public health in big cities: Looking back, looking forward. J. Public Health Manag. Pract. 2015, 21, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.K. An Introduction to Exponential Random Graph Modeling; Sage Publications: California, CA, USA, 2013; Vol. 173. [Google Scholar]
- Harris, J.K. Communication ties across the national network of local health departments. Am. J. Prev. Med. 2013, 44, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Health Officials Call for Regs on E-Cigarettes. Available online: http://thehill.com/regulation/204997-health-officials-call-for-candy-e-cig-regs (accessed on 16 June 2015).
- Enteen, L.; Bauer, J.; McLean, R.; Wheeler, E.; Huriaux, E.; Kral, A.H.; Bamberger, J.D. Overdose prevention and naloxone prescription for opioid users in san francisco. J. Urban Health 2010, 87, 931–941. [Google Scholar] [CrossRef] [PubMed]
- America under the Affordable Care Act. Available online: https://folio.iupui.edu/handle/10244/989 (accessed on 16 June 2015).
- Leider, J.P.; Castrucci, B.C.; Russo, P.; Hearne, S. Perceived impacts of health care reform on large urban health departments. J. Public Health Manag. Pract. 2015, 21, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, K.A.; Leatherdale, S.T.; Marx, C.M.; Yan, Y.; Colditz, G.A.; Brownson, R.C. Where is obesity prevention on the map? Distribution and predictors of local health department prevention activities in relation to county-level obesity prevalence in the United States. J. Public Health Manag. Pract. 2012, 18, 402–411. [Google Scholar] [CrossRef] [PubMed]
- Provan, K.; Fish, A.; Sydow, J. Interorganizational networks at the network level: A review of the empirical literature on whole networks. J. Manage. 2007, 33, 479–516. [Google Scholar] [CrossRef]
- Sellers, K.; Leider, J.P.; Harper, M.; Castrucci, B.; Bharthapdui, K.; Liss-Levinson, R.; Jarris, P.; Hunter, E. Highlights from the public health workforce interests and needs survey: The first nationally-representative survey of state health agency employee. J. Public Health Manag. Pract. 2015, (in press). [Google Scholar]
- Liss-Levinson, R.; Bharthapudi, K.; Leider, J.P.; Sellers, K. Loving and leaving public health: Predictors of intentions to quit among state health agency workers. J. Public Health Manag. Pract. 2015, (in press). [Google Scholar]
- Porshaban, D.; Basurto-Davila, R.; Shih, M. Building and sustaining strong public health agencies: Determinants of workforce turnover. J. Public Health Manag. Pract. 2015, (in press). [Google Scholar]
- Newman, S.J.; Ye, J.; Leep, C.J. Workforce turnover at local health departments: Nature, characteristics, and implications. Am. J. Prev. Med. 2014, 47, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Leider, J.P.; Shah, G.H.; Castrucci, B.C.; Leep, C.J.; Sellers, K.; Sprague, J.B. Changes in public health workforce composition: Proportion of part-time workforce and its correlates, 2008–2013. Am. J. Prev. Med. 2014, 47, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.K. The network of web 2.0 connections among state health departments: New pathways for dissemination. J. Public Health Manag. Pract. 2013, 19, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Chaloupka, F.J. Maximizing the public health impact of alcohol and tobacco taxes. Am. J. Prev. Med. 2013, 44, 561–562. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.K.; Luke, D.A.; Burke, R.C.; Mueller, N.B. Seeing the forest and the trees: Using network analysis to develop an organizational blueprint of state tobacco control systems. Soc. Sci. Med. 2008, 67, 1669–1678. [Google Scholar] [CrossRef] [PubMed]
- Tauras, J.A.; Chaloupka, F.J.; Farrelly, M.C.; Giovino, G.A.; Wakefield, M.; Johnston, L.D.; O’Malley P, M.; Kloska, D.D.; Pechacek, T.F. State tobacco control spending and youth smoking. Am. J. Public Health 2005, 95, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Luke, D.A.; Harris, J.K.; Shelton, S.; Allen, P.; Carothers, B.J.; Mueller, N.B. Systems analysis of collaboration in 5 national tobacco control networks. Am. J. Public Health 2010, 100, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leider, J.P.; Castrucci, B.C.; Harris, J.K.; Hearne, S. The Relationship of Policymaking and Networking Characteristics among Leaders of Large Urban Health Departments. Int. J. Environ. Res. Public Health 2015, 12, 9169-9180. https://doi.org/10.3390/ijerph120809169
Leider JP, Castrucci BC, Harris JK, Hearne S. The Relationship of Policymaking and Networking Characteristics among Leaders of Large Urban Health Departments. International Journal of Environmental Research and Public Health. 2015; 12(8):9169-9180. https://doi.org/10.3390/ijerph120809169
Chicago/Turabian StyleLeider, Jonathon P., Brian C. Castrucci, Jenine K. Harris, and Shelley Hearne. 2015. "The Relationship of Policymaking and Networking Characteristics among Leaders of Large Urban Health Departments" International Journal of Environmental Research and Public Health 12, no. 8: 9169-9180. https://doi.org/10.3390/ijerph120809169





