Estimation of the Biological Half-Life of Methylmercury Using a Population Toxicokinetic Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Methylmercury Assessment in Diet
2.3. Methylmercury Assessment in Blood
2.4. One-Compartment Toxicokinetic Model
2.5. Statistical Model
3. Results
3.1. Characteristics of Study Population
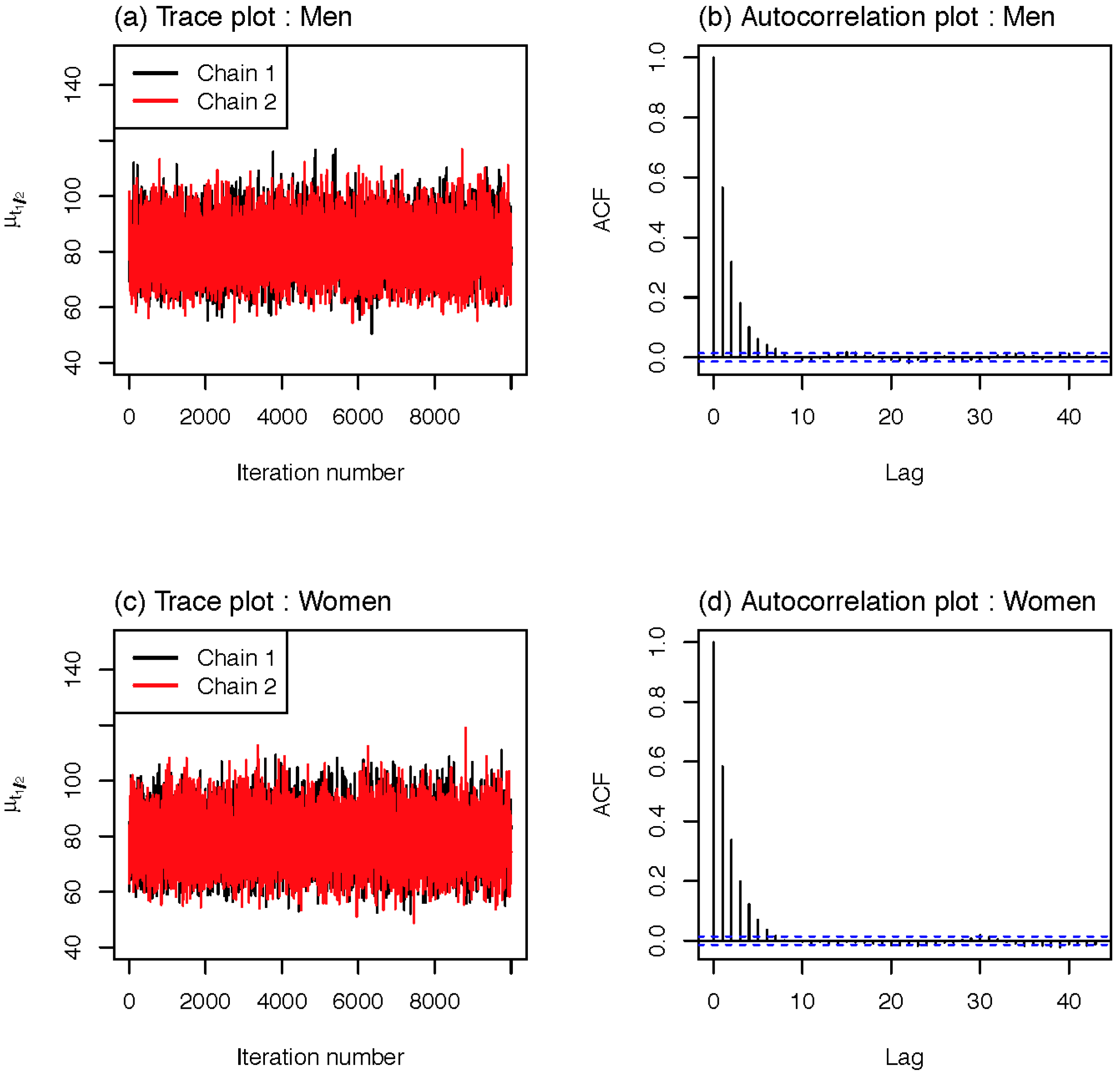
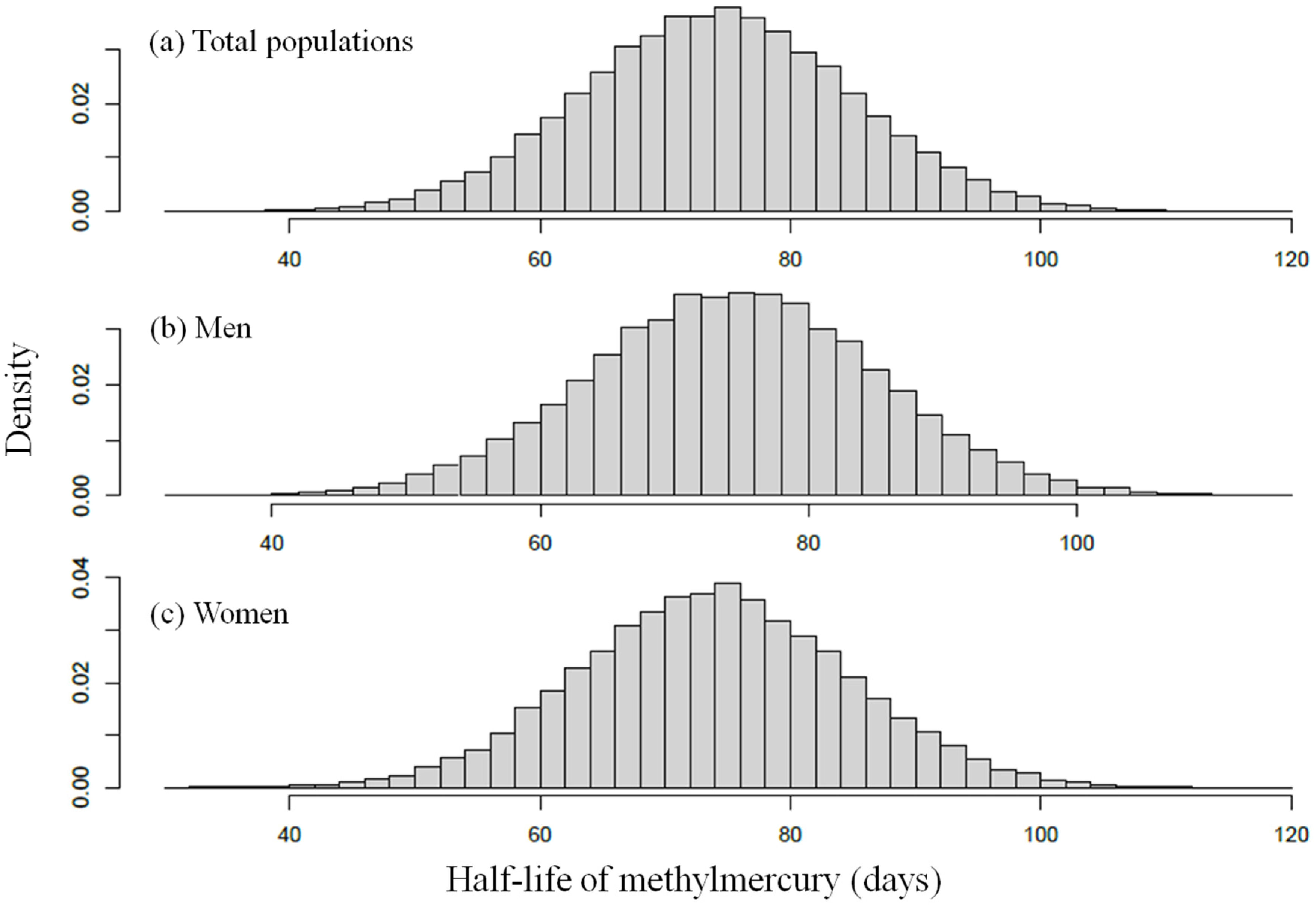
3.2. The Estimated Biological Half-Lives of Methylmercury
3.3. The Reported Half-Life of Methylmercury
4. Discussion
| Variables | Total (n = 304) | Male (n = 167) | Female (n = 137) | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Median | Mean ± SD | Median | Mean ± SD | Median | |
| Age (years) | 48 ± 14 | 50 | 47 ± 14 | 47 | 50 ± 14 | 51 |
| Weight (kg) | 66 ± 12 | 65 | 72 ± 11 | 72 | 60 ± 10 | 58 |
| Total mercury in blood (µg/L) | 8.69 ± 5.96 | 7.37 | 10.12 ± 6.9 | 8.33 | 6.94 ± 3.93 | 5.93 |
| Methylmercury in blood (µg/L) | 6.23 ± 4.31 | 4.98 | 6.97 ± 4.84 | 5.72 | 5.32 ± 3.36 | 4.17 |
| Methylmercury intake from food (µg/kg bw/day) | 0.05 ± 0.06 | 0.031 | 0.048 ± 0.056 | 0.031 | 0.053 ± 0.063 | 0.033 |
| Parameters | Total (n = 304) | Male (n = 167) | Female (n = 137) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | 2.5% | 50% | 97.5% | Mean | SD | 2.5% | 50% | 97.5% | Mean | SD | 2.5% | 50% | 97.5% | |
| μ (days) | 80.2 | 8.6 | 64.0 | 80.0 | 97.8 | 81.6 | 8.4 | 66.0 | 81.4 | 98.8 | 78.9 | 8.6 | 62.8 | 78.6 | 96.4 |
| τ (days) | 25.0 | 8.6 | 10.8 | 25.0 | 39.1 | 25.0 | 8.6 | 10.8 | 25.0 | 39.2 | 25.0 | 8.6 | 10.8 | 25.0 | 39.2 |
| Abs | 0.955 | 0.028 | 0.904 | 0.956 | 0.998 | 0.955 | 0.028 | 0.904 | 0.958 | 0.998 | 0.954 | 0.028 | 0.904 | 0.956 | 0.998 |
| Vb | 3.423 | 0.330 | 3.004 | 3.349 | 4.193 | 3.372 | 0.307 | 3.001 | 3.297 | 4.136 | 3.474 | 0.345 | 3.008 | 3.410 | 4.227 |
| fracb | 0.089 | 0.008 | 0.069 | 0.091 | 0.100 | 0.091 | 0.007 | 0.072 | 0.092 | 0.100 | 0.088 | 0.009 | 0.067 | 0.090 | 0.100 |
| σ (µg/L) | 1.388 | 0.108 | 1.191 | 1.388 | 1.601 | 1.459 | 0.081 | 1.310 | 1.454 | 1.631 | 1.318 | 0.082 | 1.170 | 1.314 | 1.490 |
| Reference | Sample Collection | Population/n | Exposure | Half-Life Measurement | Mean Intake | Concentration (Hair or Blood) | Half-Life/Mean (Days) |
|---|---|---|---|---|---|---|---|
| Miettinen et al. (1971) [16] | Hg/Blood | Finland, adults/6 | Radiolabeled MeHg meal | No consideration of the baseline blood Hg concentration | 0.3 (µg/kg/day) | − | 49.8 |
| Al-Shahristani and Shihab (1974) [18] | Hg/Hair at 8 to 12 mo. | Iraq (0.5–60 yr) /48 | MeHg-contaminated grain | − | − | − | (Total) 72 (35–120), (90%) 65 (35–100) |
| Kershaw et al. (1980) [15] | Hg/Blood | Canada, male adults (19–44yr)/5 | A single meal of fish (20 µg Hg/kg bw) | Consideration of the baseline blood Hg concentration | 20.0 (18.1–21.8) µg/kg | − | 52 |
| Sherlock et al. (1984) [17] | Hg/Blood | UK, adults/20 | High Hg concentrated fish, over 3 months | Consideration of the baseline blood Hg concentration | A 2.99, B 1.58, C 1.15, D 0.59, (µg/kg/day) | − | 50 |
| Smith et al. (1994) [19] | MeHg/Blood | U.S., male adults/7 | Radiolabeled MeHg intravenously | MeHg remaining in the blood | − | − | 44.8 (35.1–52.8) |
| Albert et al. (2010) [13] | Hg/ Hair at 12 wk/32 wk | French, pregnant women/125 | FFQ conducted twice (seafood) | − | 12 wk: 0.56, 32 wk: 0.67 (µg/kg/week) | Hair (µg/g): 12 wk: 0.82, 32 wk: 0.79 | 65.4 |
| Yaginuma-Sakurai et al. (2012) [20] | Hg/ Blood and Hair | Japan, college students and graduates/27 | Fish consumption (3.4 µg/kg/week) | With/without consideration of the baseline blood Hg concentration | 3.4 (µg/kg/week) | Blood; 6.7 (3.2–19.8) ng/g, Hair; 2.3 (1.1–6.5) µg/g | Blood; 94 (58–155), Hair; 102 (60–192) |
5. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflict of interest
References
- Choi, A.L.; Grandjean, P. Methylmercury exposure and health effects in humans. Environ. Chem. 2008, 5, 112–120. [Google Scholar] [CrossRef] [Green Version]
- Li, P.; Feng, X.; Qiu, G. Methylmercury exposure and health effects from rice and fish consumption: A review. Int. J. Environ. Res. Public Health 2010, 7, 2666–2691. [Google Scholar] [CrossRef] [PubMed]
- Mergler, D.; Anderson, H.A.; Chan, L.H.M.; Mahaffey, K.R.; Murray, M.; Sakamoto, M.; Stern, A.H. Methylmercury exposure and health effects in humans: A worldwide concern. AMBIO 2007, 36, 3–11. [Google Scholar] [CrossRef]
- Grandjean, P.; Weihe, P.; White, R.F.; Debes, F.; Araki, S.; Yokoyama, K.; Murata, K.; Sørensen, N.; Dahl, R.; Jørgensen, P.J. Cognitive deficit in 7-year-old children with prenatal exposure to methylmercury. Neurotoxicol. Teratol. 1997, 19, 417–428. [Google Scholar] [CrossRef]
- Marsh, D.O.; Clarkson, T.W.; Cox, C.; Myers, G.J.; Amin-Zaki, L. Fetal methylmercury poisoning: Relationship between concentration in single strands of maternal hair and child effects. Arch. Neurol. 1987, 44, 1017–1022. [Google Scholar] [CrossRef] [PubMed]
- Birke, G.; Johnels, A.G.; Plantin, L.-O.; Sjöstrand, B.; Skerfving, S.; Westermark, T. Studies on humans exposed to methyl mercury through fish consumption. Arch. Environ. Health 1972, 25, 77–91. [Google Scholar] [CrossRef] [PubMed]
- NRC. Toxicological Effects of Methylmercury; National Academy Press: Washington D.C., USA, 2000.
- Kris-Etherton, P.M.; Taylor, D.S.; Yu-Poth, S.; Huth, P.; Moriarty, K.; Fishell, V.; Hargrove, R.L.; Zhao, G.; Etherton, T.D. Polyunsaturated fatty acids in the food chain in the United States. Amer. J. Clin. Nutr. 2000, 71, S179–S188. [Google Scholar]
- Bazinet, R.P.; Layé, S. Polyunsaturated fatty acids and their metabolites in brain function and disease. Nat. Rev. Neurosci. 2014, 15, 771–785. [Google Scholar] [CrossRef] [PubMed]
- U.S. EPA. Water Quality Criterion for the Protection of Human Health: Methylmercury; U.S. Environmental Protection Agency: Washington D.C., USA, 2001.
- JECFA. Evaluation of Certain Food Additives and Contaminants (Sixty-First Report of the Joint Fao/Who Expert committee on Food Additives). Available online: http://www.who.int/foodsafety/publications/jecfa-reports/en/ (accessed on 24 August 2014).
- EFSA. Scientific opinion on the risk for public health related to the presence of mercury and methylmercury in food. Efsa panel on contaminants in the food chain (contam). EFSA 2012. [Google Scholar] [CrossRef]
- Albert, I.; Villeret, G.; Paris, A.; Verger, P. Integrating variability in half-lives and dietary intakes to predict mercury concentration in hair. Regul. Toxicol. Pharmacol. 2010, 58, 482–489. [Google Scholar] [CrossRef] [PubMed]
- U.S. EPA. Mercury study report to congress. In Health Effects of Mercury and Mercury Compounds; Office of Air Quality Planning & Standards and Office of Research and Development. U.S. Environmental Protection Agency: Washington, DC, USA, 1997. [Google Scholar]
- Kershaw, T.G.; Dhahir, P.H.; Clarkson, T.W. The relationship between blood levels and dose of methylmercury in man. Arch. Environ. Health 1980, 35, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Miettinen, J.; Rahola, T.; Hattula, T.; Rissanen, K.; Tillander, M. Elimination of 203hg methylmercury in man. Ann. Clin. Res. 1971, 3, 116–122. [Google Scholar] [PubMed]
- Sherlock, J.; Hislop, J.; Newton, D.; Topping, G.; Whittle, K. Elevation of mercury in human blood from controlled chronic ingestion of methylmercury in fish. Hum. Toxicol. 1984, 3, 117–131. [Google Scholar] [CrossRef] [PubMed]
- Al-Shahristani, H.; Shihab, K.M. Variation of biological half-life of methylmercury in man. Arch. Environ. Health 1974, 28, 342–344. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.C.; Allen, P.V.; Turner, M.D.; Most, B.; Fisher, H.L.; Hall, L.L. The kinetics of intravenously administered methyl mercury in man. Toxicol. Appl. Pharmacol. 1994, 128, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Yaginuma-Sakurai, K.; Murata, K.; Iwai-Shimada, M.; Nakai, K.; Kurokawa, N.; Tatsuta, N.; Satoh, H. Hair-to-blood ratio and biological half-life of mercury: Experimental study of methylmercury exposure through fish consumption in humans. J. Toxicol. Sci. 2012, 37, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Aberg, B.; Ekman, L.; Falk, R.; Greitz, U.; Persson, G.; Snihs, J.O. Metabolism of methyl mercury (203hg) compounds in man: Excretion and distribution. Arch. Environ. Health 1969, 19, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.A.; Chung, D.; On, J.; Moon, M.H.; Lee, J.; Pyo, H. Correlation between total mercury and methyl mercury-in whole blood of South Korean. Bull. Korean Chem. Soc 2013, 34, 1101–1107. [Google Scholar] [CrossRef]
- Swartout, J.; Rice, G. Uncertainty analysis of the estimated ingestion rates used to derive the methylmercury reference dose. Drug Chem. Toxicol. 2000, 23, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Stern, A.H. Estimation of the interindividual variability in the one-compartment pharmacokinetic model for methylmercury: Implications for the derivation of a reference dose. Regul. Toxicol. Pharmacol. 1997, 25, 277–288. [Google Scholar] [CrossRef] [PubMed]
- Gelman, A. Prior distributions for variance parameters in hierarchical models (comment on article by browne and draper). Bayesian Anal. 2006, 1, 515–534. [Google Scholar]
- Environmental Health Criteria N 101: Methylmercury. Available online: http://www.inchem.org/documents/ehc/ehc/ehc101.htm (accessed on 24 August 2014).
- Stern, A.H. A revised probabilistic estimate of the maternal methyl mercury intake dose corresponding to a measured cord blood mercury concentration. Environ. Health Perspect. 2005, 155–163. [Google Scholar] [CrossRef]
- Dakeishi, M.; Nakai, K.; Sakamoto, M.; Iwata, T.; Suzuki, K.; Liu, X.-J.; Ohno, T.; Kurosawa, T.; Satoh, H.; Murata, K. Effects of hair treatment on hair mercury—The best biomarker of methylmercury exposure? Environ. Health Prev. Med. 2005, 10, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.-G.; Jo, E.-M.; Kim, G.-Y.; Kim, D.-S.; Kim, Y.-M.; Kim, R.-B.; Suh, B.-S.; Hong, Y.-S. Analysis of methylmercury concentration in the blood of koreans by using cold vapor atomic fluorescence spectrophotometry. Ann. Lab. Med. 2012, 32, 31–37. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jo, S.; Woo, H.D.; Kwon, H.-J.; Oh, S.-Y.; Park, J.-D.; Hong, Y.-S.; Pyo, H.; Park, K.S.; Ha, M.; Kim, H.; et al. Estimation of the Biological Half-Life of Methylmercury Using a Population Toxicokinetic Model. Int. J. Environ. Res. Public Health 2015, 12, 9054-9067. https://doi.org/10.3390/ijerph120809054
Jo S, Woo HD, Kwon H-J, Oh S-Y, Park J-D, Hong Y-S, Pyo H, Park KS, Ha M, Kim H, et al. Estimation of the Biological Half-Life of Methylmercury Using a Population Toxicokinetic Model. International Journal of Environmental Research and Public Health. 2015; 12(8):9054-9067. https://doi.org/10.3390/ijerph120809054
Chicago/Turabian StyleJo, Seongil, Hae Dong Woo, Ho-Jang Kwon, Se-Young Oh, Jung-Duck Park, Young-Seoub Hong, Heesoo Pyo, Kyung Su Park, Mina Ha, Ho Kim, and et al. 2015. "Estimation of the Biological Half-Life of Methylmercury Using a Population Toxicokinetic Model" International Journal of Environmental Research and Public Health 12, no. 8: 9054-9067. https://doi.org/10.3390/ijerph120809054






