Highly Pathogenic Avian Influenza H5N1 in Mainland China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data on HPAI H5N1
2.2. Ecologic Variables
2.3. Spatiotemporal Analysis
2.4. Analysis of Potential Factors Associated with the HPAI H5N1 Outbreak in Poultry
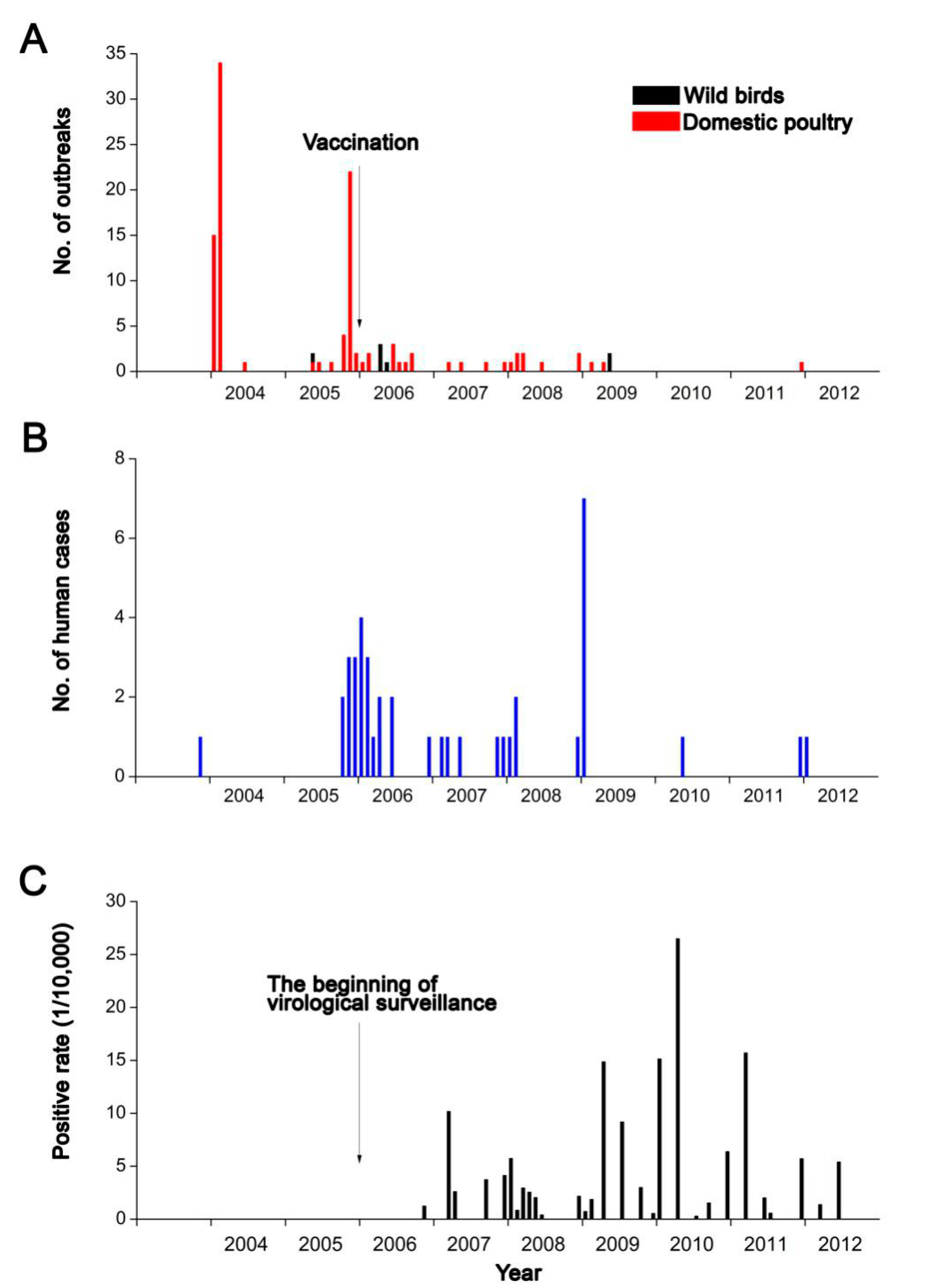
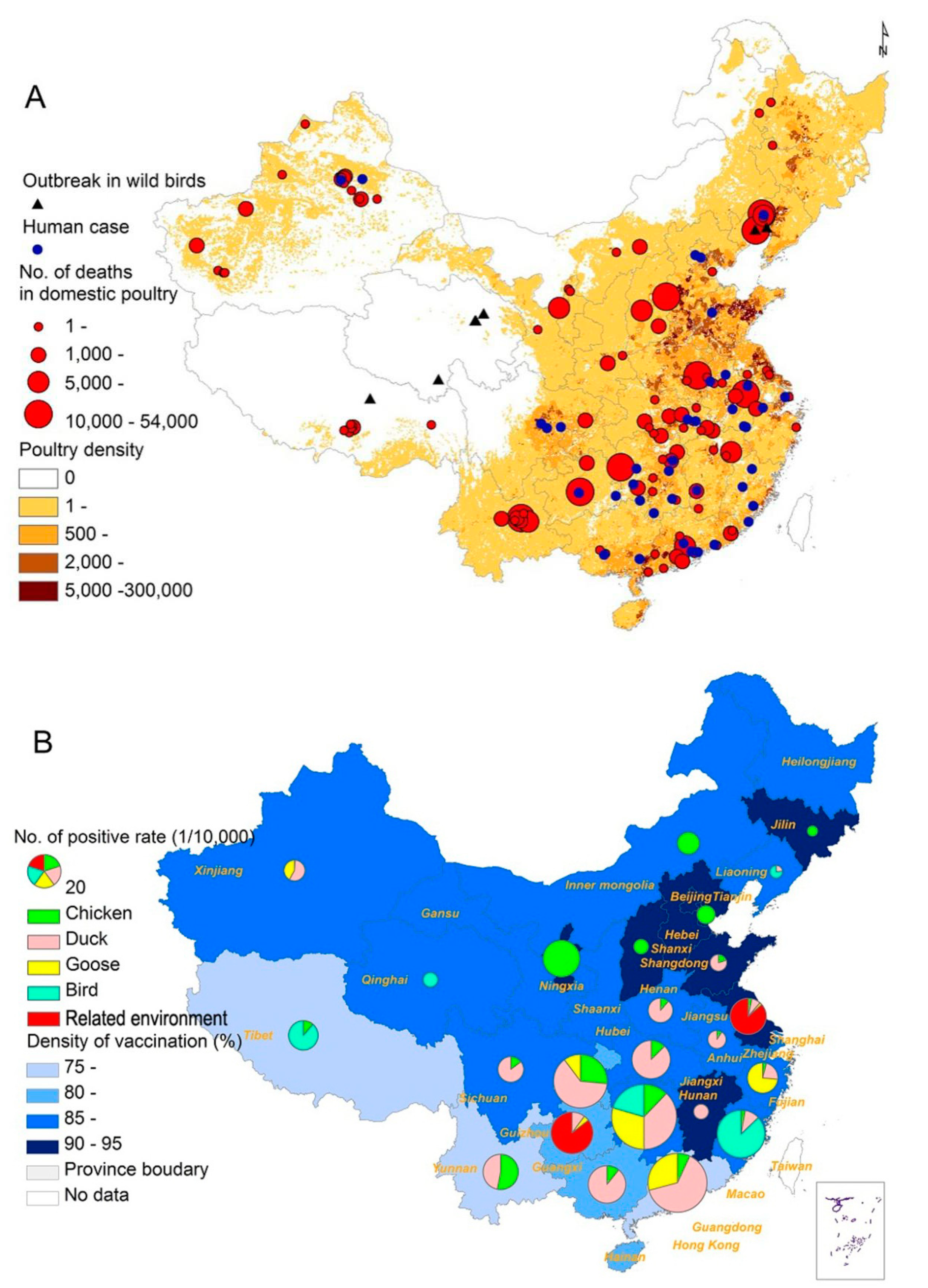
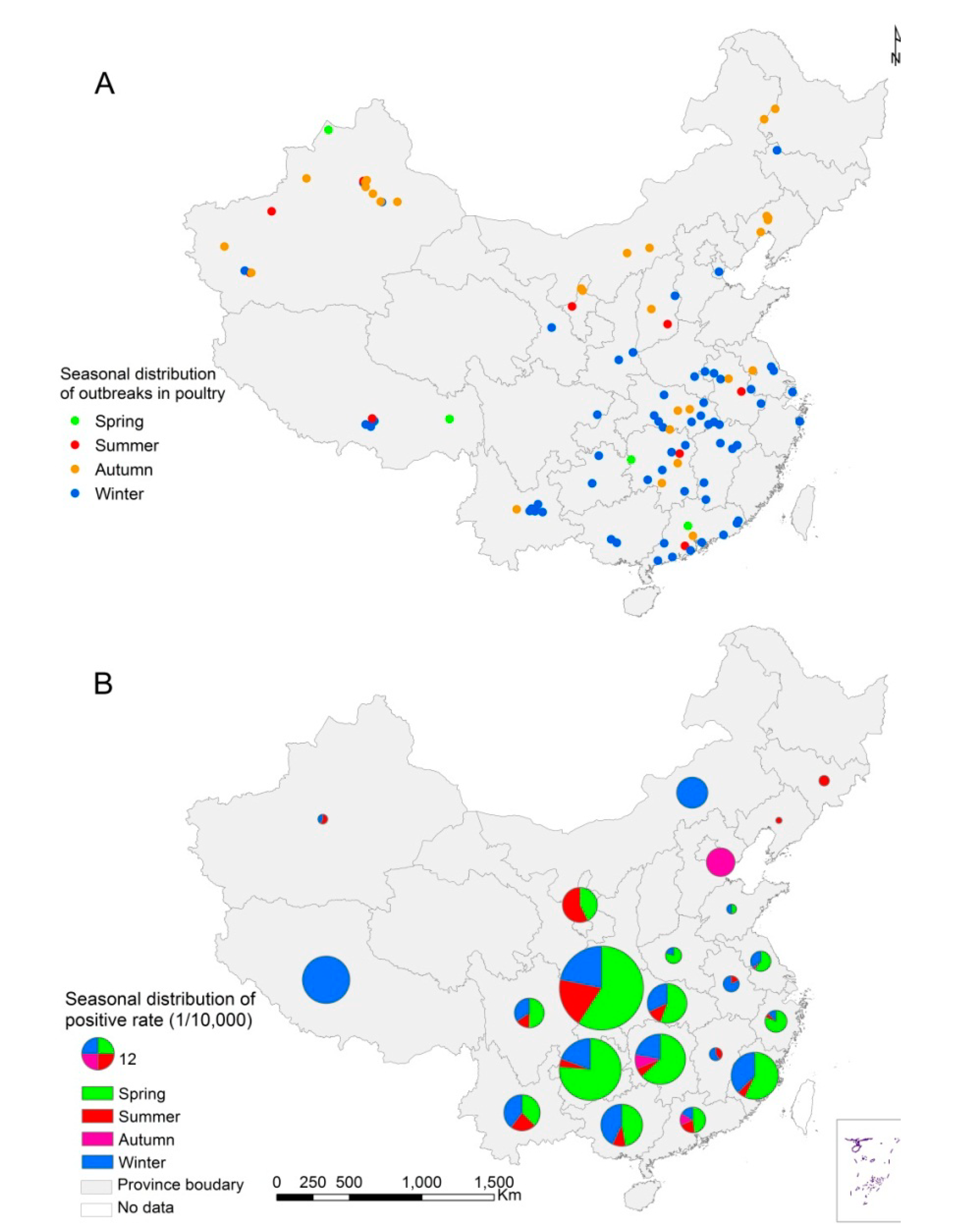
3. Results
| Month | Outbreaks (%) | Species of Domestic Poultry | Deaths (Feature) | Destroyed (Feature) |
|---|---|---|---|---|
| January | 17 (16.04%) | Chicken, duck, and goose | 51,638 | 1,295,494 |
| February | 39 (36.79%) | Chicken & goose | 131,029 | 4,131,160 |
| March | 3 (2.83%) | Chicken | 1062 | 9558 |
| April | 1 (0.94%) | Chicken | 1500 | 1679 |
| May | 2 (1.89%) | Duck & goose | 11,632 | 66,331 |
| June | 6 (5.66%) | Chicken, duck, and goose | 14,799 | 2,393,358 |
| July | 1 (0.94%) | Chicken | 3045 | 356,976 |
| August | 2 (1.89%) | Chicken | 1938 | 295,805 |
| September | 3 (2.83%) | Chicken & duck | 11,815 | 234,920 |
| October | 4 (3.77%) | Chicken, duck, and goose | 12,655 | 6,138,323 |
| November | 22 (20.75%) | Chicken, duck, and goose | 133,777 | 15,799,404 |
| December | 6 (5.66%) | Chicken, duck, and goose | 8873 | 194,930 |
| Variables ( Unit ) a | No. of Outbreaks (95% CI) | Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |||
| Vaccination rate (categorical, %) | ||||||
| <70 | 85 (68, 102) | |||||
| 70– | 13 (6, 20) | |||||
| >90 | 5 (1, 9) | |||||
| Vaccination rate (continuous, 10 %) | 0.80 (0.76, 0.85) | <0.001 | 0.79 (0.74, 0.84) | <0.001 | ||
| Distance to the nearest transportation routes | ||||||
| National highway (categorical, 10 km) | ||||||
| <1 | 57 (43, 71) | |||||
| 1– | 36 (24, 48) | |||||
| >3 | 10 (2, 12) | |||||
| National highway (continuous, 10 km) | 0.66 (0.57, 0.77) | <0.001 | ||||
| Railway (categorical, 10 km) | ||||||
| <3 | 87 (69, 105) | |||||
| 3– | 10 (4, 16) | |||||
| >10 | 6 (1, 10) | |||||
| Railway (continuous, 10 km) | 0.91 (0.87, 0.96) | <0.001 | ||||
| Freeway (categorical, 10 km) | ||||||
| <3 | 83 (66, 100) | |||||
| 3– | 11(5, 17) | |||||
| >50 | 9 (3, 15) | |||||
| Freeway (continuous, 10 km) | 0.99 (0.98, 1.00) | 0.217 | ||||
| Distance to the nearest city (categorical, 10 km) | ||||||
| <5 | 72 (56, 88) | |||||
| 5– | 24 (14, 34) | |||||
| >10 | 7 (2, 12) | |||||
| Distance to the nearest city (continuous, 10 km) | 0.78 (0.73, 0.84) | <0.001 | ||||
| Interaction between distance to the nearest city and national highway (continuous, 10 km * 10 km) | 0.93 (0.91, 0.96) | <0.001 | 0.96 (0.94, 0.99) | 0.002 | ||
| Distance to the nearest water body | ||||||
| Lake (categorical, 1 km) | ||||||
| <30 | 96 (77, 115) | |||||
| 30– | 5 (1, 9) | |||||
| >50 | 2 (0, 5) | |||||
| Lake (continuous, 10 km) | 0.60 (0.49, 0.72) | <0.001 | ||||
| Water reservoir (categorical, 10 km) | ||||||
| <10 | 83 (66, 100) | |||||
| 10– | 12 (5, 19) | |||||
| >30 | 8 (3, 13) | |||||
| Water reservoir (continuous, 10 km) | 0.95 (0.91, 1.00) | 0.031 | ||||
| River (categorical, 10 km) | ||||||
| <3 | 64 (49, 79) | |||||
| 3– | 29 (19, 39) | |||||
| >10 | 10 (4, 16) | |||||
| River (continuous, 10 km) | 0.99 (0.98, 1.01) | 0.491 | ||||
| Distance to the nearest wetland (categorical, 10 km) | ||||||
| <2 | 88 (70, 106) | |||||
| 2– | 13 (6, 20) | |||||
| >5 | 2 (0, 5) | |||||
| Distance to the nearest wetland (continuous, 10 km) | 0.60 (0.48, 0.75) | <0.001 | ||||
| Interaction between distance to the nearest Lake and wetland (10 km * 10 km) | 0.76 (0.67, 0.85) | <0.001 | 0.87 (0.78, 0.96) | <0.001 | ||
| Density of human population (categorical, 1000 persons per km2) | ||||||
| <0.1 | 16(8, 24) | |||||
| 0.1– | 32(21, 43) | |||||
| >0.4 | 55(41, 69) | |||||
| Density of human population (continuous, 1000 persons per km2) | 1.66 (1.42, 1.95) | <0.001 | 1.44 (1.19, 1.73) | <0.001 | ||
| Density of poultry (categorical, 100 poultry per km2) | ||||||
| <1 | 28(18,38) | |||||
| 1– | 26(16,35) | |||||
| >5 | 49(36,62) | |||||
| Density of poultry (continuous, 100 poultry per km2) | 1.02 (1.01, 1.03) | <0.001 | ||||
| Quadratic density of poultry (continuous) | 1.00 (1.00, 1.00) | 0.082 | ||||
| Climate | ||||||
| Mean temperature in summer (categorical, 1 centigrade) | ||||||
| <20 | 11(5, 17) | |||||
| 20– | 33(22, 44) | |||||
| >25 | 59(44, 74) | |||||
| Mean temperature in summer (continuous, 1 centigrade) | 1.11 (1.04, 1.17) | 0.001 | ||||
| Mean temperature in winter (categorical, 1 centigrade) | ||||||
| <0 | 7 (2, 12) | |||||
| 0– | 25 (15,35) | |||||
| >10 | 71 (55, 87) | |||||
| Mean temperature in winter(continuous, 1 centigrade) | 1.04 (1.02, 1.07) | <0.001 | ||||
| Precipitation in spring and summer(categorical, 100mm) | ||||||
| <1 | 7 (2,12) | |||||
| 1– | 29 (19, 39) | |||||
| >5 | 67 (51,83) | |||||
| Precipitation in spring and summer(continuous,100mm) | 1.07 (1.02, 1.12) | 0.004 | ||||
| Precipitation in autumn and winter (categorical, 100mm) | ||||||
| <0.5 | 13 (6, 20) | |||||
| 0.5– | 28 (18, 38) | |||||
| >2 | 62 (47,77) | |||||
| Precipitation in autumn and winter (continuous,100mm) | 1.12 (0.99, 1.27) | 0.064 | ||||
| NDVI (categorical) | ||||||
| <100 | 28 (18, 38) | |||||
| 100– | 42 (30, 54) | |||||
| >150 | 33 (21, 44) | |||||
| NDVI (continuous) | 1.00 (1.00, 1.01) | 0.556 | ||||
| Quadratic NDVI (continuous) | 1.00 (1.00, 1.00) | 0.808 | ||||
| Land use (10 %) | ||||||
| Percentage coverage of cropland (categorical, 10%) | ||||||
| <1 | 15 (7, 21) | |||||
| 1– | 34 (23, 45) | |||||
| >5 | 55 (41, 69) | |||||
| Percentage coverage of cropland (continuous, 10%) | 1.18 (1.11, 1.25) | <0.001 | ||||
| Percentage coverage of grassland (categorical, 10%) | ||||||
| <2 | 59 (44, 74) | |||||
| 2– | 31 (20, 42) | |||||
| >5 | 13 (6, 20) | |||||
| Percentage coverage of grassland (continuous, 10%) | 0.91 (0.84, 0.99) | 0.022 | ||||
| Percentage coverage of shrub (categorical, 10%) | ||||||
| <0.05 | 56 (42, 70) | |||||
| 0.05– | 34 (27, 45) | |||||
| >0.1 | 13 (6, 20) | |||||
| Percentage coverage of shrub (continuous, 10%) | 0.66 (0.52, 0.85) | 0.001 | ||||
| Percentage coverage of forest (categorical, 10%) | ||||||
| <0.05 | 59 (44, 74) | |||||
| 0.05– | 25 (15, 35) | |||||
| >0.5 | 19 (11, 27) | |||||
| Percentage coverage of forest (continuous, 10%) | 0.88 (0.76, 1.03) | 0.104 | ||||
| Percentage coverage of buildup (categorical, 10%) | ||||||
| <0.05 | 36 (24, 48) | |||||
| 0.05– | 35 (24, 46) | |||||
| >0.5 | 32 (21, 42) | |||||
| Percentage coverage of buildup (continuous, 10%) | 1.52 (1.31, 1.76) | <0.001 | ||||
| Mean elevation (categorical , 100 m) | ||||||
| <5 | 66 (50, 82) | |||||
| 5– | 29 (19, 39) | |||||
| >20 | 8 (2, 14) | |||||
| Mean elevation (continuous , 100 m) | 0.96 (0.94, 0.99) | 0.002 | ||||
| Autoregressive term (continuous) | 1.50 (1.39, 1.63) | <0.001 | 1.40 (1.28, 1.54) | <0.001 | ||
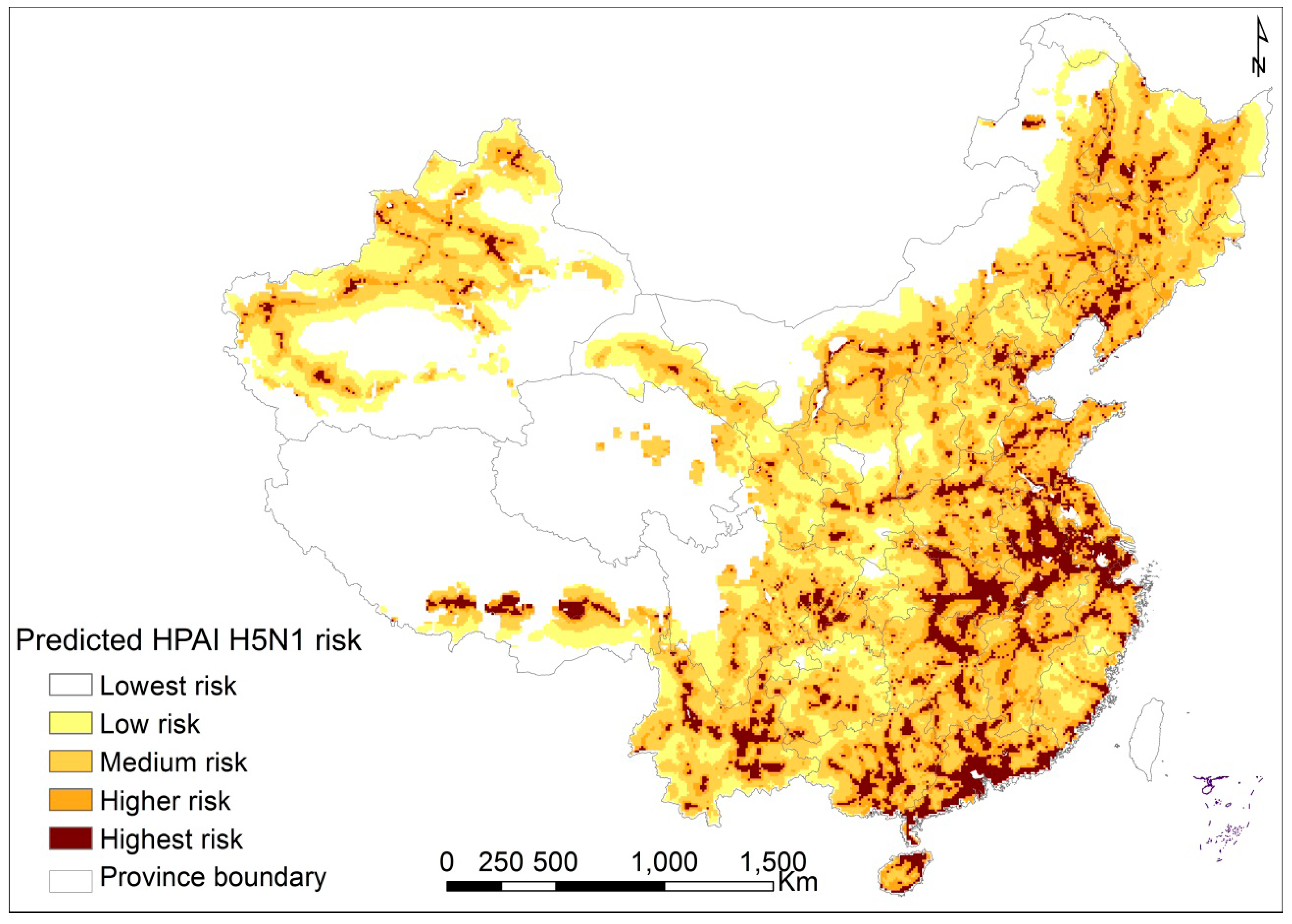
4. Discussion
5. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Edge, L. Asian H5N1 still going strong at 10 years old. Lancet Infect. Dis. 2007, 7. [Google Scholar] [CrossRef]
- De Jong, J.; Claas, E.; Osterhaus, A.; Webster, R.; Lim, W. A pandemic warning? Nature 1997, 389, 554–554. [Google Scholar] [CrossRef] [PubMed]
- OIE. Avian Influenza Portal. Available online: http://www.oie.int/animal-health-in-the-world/web-portal-on-avian-influenza (accessed on 1 October 2014).
- WHO. H5N1 influenza. Available online: http://www.who.int/influenza/human_ animal_interface/avian_influenza/h5n1_research/faqs/en/ (accessed on 1 October 2014).
- Ducatez, M.F.; Olinger, C.M.; Owoade, A.A.; de Landtsheer, S.; Ammerlaan, W.; Niesters, H.G.; Osterhaus, A.D.; Fouchier, R.A.; Muller, C.P. Avian flu: Multiple introductions of H5N1 in Nigeria. Nature. 2006, 442. [Google Scholar] [CrossRef] [PubMed]
- Peiris, J.M.; de Jong, M.D.; Guan, Y. Avian influenza virus (H5N1): A threat to human health. Clin. Microbiol. Rev. 2007, 20, 243–267. [Google Scholar] [CrossRef] [PubMed]
- Krau, S.D.; Parsons, L.C. Avian influenza: Are we ready? Crit. Care Nurs. Clin. North Amer. 2007, 19, 107–113. [Google Scholar] [CrossRef]
- Ungchusak, K.; Auewarakul, P.; Dowell, S.F.; Kitphati, R.; Auwanit, W.; Puthavathana, P.; Uiprasertkul, M.; Boonnak, K.; Pittayawonganon, C.; Cox, N.J. Probable person-to-person transmission of avian influenza a (H5N1). N. Engl. J. Med. 2005, 352, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Gao, R.; Cao, B.; Hu, Y.; Feng, Z.; Wang, D.; Hu, W.; Chen, J.; Jie, Z.; Qiu, H.; Xu, K.; et al. Human infection with a novel avian-origin influenza a (H7N9) virus. N. Engl. J. Med. 2013, 368, 1888–1897. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.Q.; de Vlas, S.J.; Liang, S.; Looman, C.W.; Gong, P.; Xu, B.; Yan, L.; Yang, H.; Richardus, J.H.; Cao, W.C. Environmental factors contributing to the spread of H5N1 avian influenza in mainland China. PLoS One 2008. [Google Scholar] [CrossRef]
- Gilbert, M.; Xiao, X.; Chaitaweesub, P.; Kalpravidh, W.; Premashthira, S.; Boles, S.; Slingenbergh, J. Avian influenza, domestic ducks and rice agriculture in Thailand. Agric. Ecosyst. Environ. 2007, 119, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.A.; Peterson, A.T. Ecology and geography of avian influenza (HPAI H5N1) transmission in the middle east and northeastern Africa. Int. J. Health Geogr. 2009, 8. [Google Scholar] [CrossRef]
- Pfeiffer, D.U.; Minh, P.Q.; Martin, V.; Epprecht, M.; Otte, M.J. An analysis of the spatial and temporal patterns of highly pathogenic avian influenza occurrence in Vietnam using national surveillance data. Vet. J. 2007, 174, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.; Xiao, X.; Pfeiffer, D.U.; Epprecht, M.; Boles, S.; Czarnecki, C.; Chaitaweesub, P.; Kalpravidh, W.; Minh, P.Q.; Otte, M.J.; et al. Mapping H5N1 highly pathogenic avian influenza risk in Southeast Asia. Proc. Natl. Acad. Sci. USA 2008, 105, 4769–4774. [Google Scholar] [CrossRef] [PubMed]
- Rivas, A.L.; Chowell, S.J.; Schwager, F.O.; Fasina, A.L.; Hoogesteijn, S.D.; Smith, S.P.R.; Bisschop, K.L.; Anderson, J.M.; Hyman, J.M. Lessons from Nigeria: the role of roads in the geo-temporal progression of avian influenza (H5N1) virus. Epidemiol. Infect. 2010, 138, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Martin, V.; Pfeiffer, D.U.; Zhou, X.; Xiao, X.; Prosser, D.J.; Guo, F.; Gilbert, M. Spatial distribution and risk factors of highly pathogenic avian influenza (HPAI) H5N1 in China. PLoS Pathog. 2011, 7. [Google Scholar] [CrossRef]
- Li, K.S.; Guan, Y.; Wang, J. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature 2004, 30, 209–213. [Google Scholar] [CrossRef]
- Durand, P.; Glew, D.; Gross, M.; Kasper, S.; Trock, K.; Kim, J.S.; Bresee, R.; Donis, T.M.; Uyeki, M.A.; Widdowson, E.; et al. Timing of influenza a (H5N1) in poultry and humans and seasonal influenza activity worldwide, 2004–2013. Emerg. Infect. Dis. 2015, 21, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.J.; Chen, D.M.; Chen, Y.; Wang, B.; Hu, L.; Gao, J.; Sun, L.Q.; Li, R.; Xiong, C.L. Evaluating the impact of environmental temperature on global highly pathogenic avian influenza (HPAI) H5N1 outbreaks in domestic Poultry. Int. J. Environ. Res. Public Health. 2014, 11, 6388–6399. [Google Scholar] [CrossRef]
- Tian, H.Y.; Zhou, S.; Dong, L.; Boeckel, T.; Cui, Y.J.; Wu, Y.R.; Cazelles, B.; Huang, S.Q.; Yang, R.F.; Grenfell, B.; Xu, B. Avian influenza H5N1 viral and bird migration networks in Asia. Proc. Natl. Acad. Sci. USA 2015, 112, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Prosser, D.J.; Cui, P.; Takekawa, J.Y.; Tang, M.J.; Hou, Y.S.; Collins, B.M.; Yan, B.P.; Hill, N.J.; Li, T.X.; Li, Y.D.; et al. Wild Bird Migration across the Qinghai-Tibetan Plateau: A transmission route for highly pathogenic H5N1. PLoS One 2011, 6. [Google Scholar] [CrossRef] [PubMed]
- Cui, P.; Hou, Y.S.; He, Y.B.; Li, T.X.; Guo, S.; Luo, Z.; Yan, B.P.; Yin, Z.H.; Lei, F.M. Bird migration and risk for H5N1 transmission into Qinghai lake, China. Vector Borne Zoonotic. Dis. 2011, 11, 567–676. [Google Scholar] [CrossRef] [PubMed]
- Takekawa, J.Y.; Newman, S.H.; Xiao, X.M.; Prosser, D.J.; Spragens, K.A.; Palm, E.C.; Yan, B.P.; Li, T.X.; Lei, F.M.; Zhao, D.L.; et al. Migration of waterfowl in the east Asian flyway and spatial relationship to HPAI H5N1 outbreaks. Avian Dis. 2010, 54, 466–476. [Google Scholar] [CrossRef] [PubMed]
- MoA China. Technical Requirements for Prevention and Control of Highly Pathogenic Avian Influenza. Available online: http://www.moa.gov.cn/zwllm/nybz/200803/t20080304_1028653.htm (accessed on on 1 October 2014).
- MoA China. Official Veterinary Bulletin. Available online: http://www.moa.gov.cn/zwllm/tzgg/gb/sygb/ index_1.htm (accessed on 1 October 2014).
- WHO. Cumulative Number of Confirmed Human Cases of Avian Influenza A(H5N1) Reported to WHO, 2003–2012. Available online: http://www.who.int/influenza/human_animal_interface/H5N1_cumulative_ table_archives/en (accessed on 1 October 2014).
- Fang, L.Q.; Li, X.L.; Liu, K.; Li, Y.J. Mapping spread and risk of Avian Influenza A (H7N9) in China. Sci. Rep. 2013, 3. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.; Newman, S.H.; Takekawa, J.Y.; Loth, L.; Biradar, C.; Prosser, D.J.; Balachandran, S.; Subba Rao, M.V.; Mundkur, T.; Yan, B.; et al. Flying over an infected landscape: Distribution of highly pathogenic avian influenza H5N1 risk in South Asia and satellite tracking of wild waterfowl. EcoHealth 2010, 7, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Cao, C.X. Risk analysis for the highly pathogenic avian influenza in mainland China using meta-modeling. Chin. Sci. Bull. 2010, 55, 4168–4178. [Google Scholar] [CrossRef]
- Paul, M.; Tavornpanich, S.; Abrial, D.; Gasqui, P.; Charras-Garrido, M.; Thanapongtharm, W.; Xiao, X.; Gilbert, M.; Roger, F.; Ducrot, C. Anthropogenic factors and the risk of highly pathogenic avian influenza h5n1: Prospects from a spatial-based model. Vet. Res. 2010, 41, 28. [Google Scholar] [CrossRef] [PubMed]
- FAO. Data for Global Livestock Density Poultry in the World. Available online: http://www.fao.org/ AG/againfo/resources/en/glw/GLW_dens.html (accessed on 1 October 2014).
- Dormann, C.F. Assessing the validity of autologistic regression. Ecol. Model. 2 2007, 207, 234–242. [Google Scholar] [CrossRef]
- Dormann, C.F.; McPherson, J.M.; Araújo, M.B.; Bivand, R.; Bolliger, J.; Carl, G.; Davies, R.G.; Hirzel, A.; Jetz, W.; Daniel Kissling, W.; et al. Methods to account for spatial autocorrelation in the analysis of species distributional data: A review. Ecography. 2007, 30, 609–628. [Google Scholar] [CrossRef]
- Gilbert, M.; Chaitaweesub, P.; Parakamawongsa, T.; Parakamawongsa, S.; Tiensin, T.; Kalpravidh, W.; Wagner, H.; Slingenbergh, J. Free-grazing ducks and highly pathogenic avian influenza, Thailand. Emerg. Infect Dis. 2006, 12, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Park, A.W.; Glass, K. Dynamic patterns of avian and human influenza in east and southeast Asia. Lancet Infect. Dis 2007, 7, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.; Slingenbergh, J.; Xiao, X. Climate change and avian influenza. Rev. Sci. Tech. 2008, 27, 459–466. [Google Scholar] [PubMed]
- Lowen, A.C.; Mubareka, S.; Steel, J.; Palese, P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007, 3, 1470–1476. [Google Scholar] [CrossRef] [PubMed]
- Kilpatrick, A.M.; Chmura, A.A.; Gibbons, D.W.; Fleischer, R.C.; Marra, P.P.; Daszak, P. Predicting the global spread of H5N1 avian influenza. Proc. Natl. Acad. Sci. USA 2006, 103, 19368–19373. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, X.-L.; Liu, K.; Yao, H.-W.; Sun, Y.; Chen, W.-J.; Sun, R.-X.; De Vlas, S.J.; Fang, L.-Q.; Cao, W.-C. Highly Pathogenic Avian Influenza H5N1 in Mainland China. Int. J. Environ. Res. Public Health 2015, 12, 5026-5045. https://doi.org/10.3390/ijerph120505026
Li X-L, Liu K, Yao H-W, Sun Y, Chen W-J, Sun R-X, De Vlas SJ, Fang L-Q, Cao W-C. Highly Pathogenic Avian Influenza H5N1 in Mainland China. International Journal of Environmental Research and Public Health. 2015; 12(5):5026-5045. https://doi.org/10.3390/ijerph120505026
Chicago/Turabian StyleLi, Xin-Lou, Kun Liu, Hong-Wu Yao, Ye Sun, Wan-Jun Chen, Ruo-Xi Sun, Sake J. De Vlas, Li-Qun Fang, and Wu-Chun Cao. 2015. "Highly Pathogenic Avian Influenza H5N1 in Mainland China" International Journal of Environmental Research and Public Health 12, no. 5: 5026-5045. https://doi.org/10.3390/ijerph120505026





