Environmental Factors and WASH Practices in the Perinatal Period in Cambodia: Implications for Newborn Health
Abstract
:1. Introduction
2. Experimental Section
| Methods | Data Collected | Participants | Location |
|---|---|---|---|
| Observation, photos, video | Hygiene and IPC practices in health centers and related equipment and supplies | 10 Health centers | Health center |
| Newborn care practices related to WASH | 4 Newborns (less than 29 days old) and their mothers at home | Home | |
| Semi-structured interviews | Hand washing Diapering Water and Sanitation Bathing | 27 Mothers/Caregivers; 16 village health support group volunteers | Health center |
| Focus group discussions | Hygiene and IPC practices in health centers Newborn care practices | 2 Focus groups | Health center |
| Domain | Features Checked |
|---|---|
| Health Center Environment | |
| Infrastructure | Electricity |
| Backup electricity | |
| Designated rooms for delivery and post-delivery care | |
| Sufficient lighting for health care activities | |
| Hand hygiene | Hand washing points |
| |
| Routine cleaning | Condition of: |
| |
| Availability of cleaning supplies | |
| Availability of cleaning equipment | |
| Sanitation | Latrines |
| |
| Sharps disposal | |
| Waste disposal | |
| Water | Indoor running water |
| Outdoor running water | |
| Appearance of water | |
| Sterilization | Sterilizing equipment |
| Electric autoclave | |
| Health care equipment and supplies | Sterile/non-sterile gloves |
| Plastic sheeting for delivery | |
| Clean linens for delivery and post-partum care | |
| Clean cord care items | |
| Home Environment | |
| Sanitation | Toilet present |
| Animals | Presence of animals |
| Hand hygiene | Hand washing station at toilet |
| Water at hand washing station | |
| Soap at hand washing station | |
| Water | Source of household water |
| Storage of household water |
3. Results
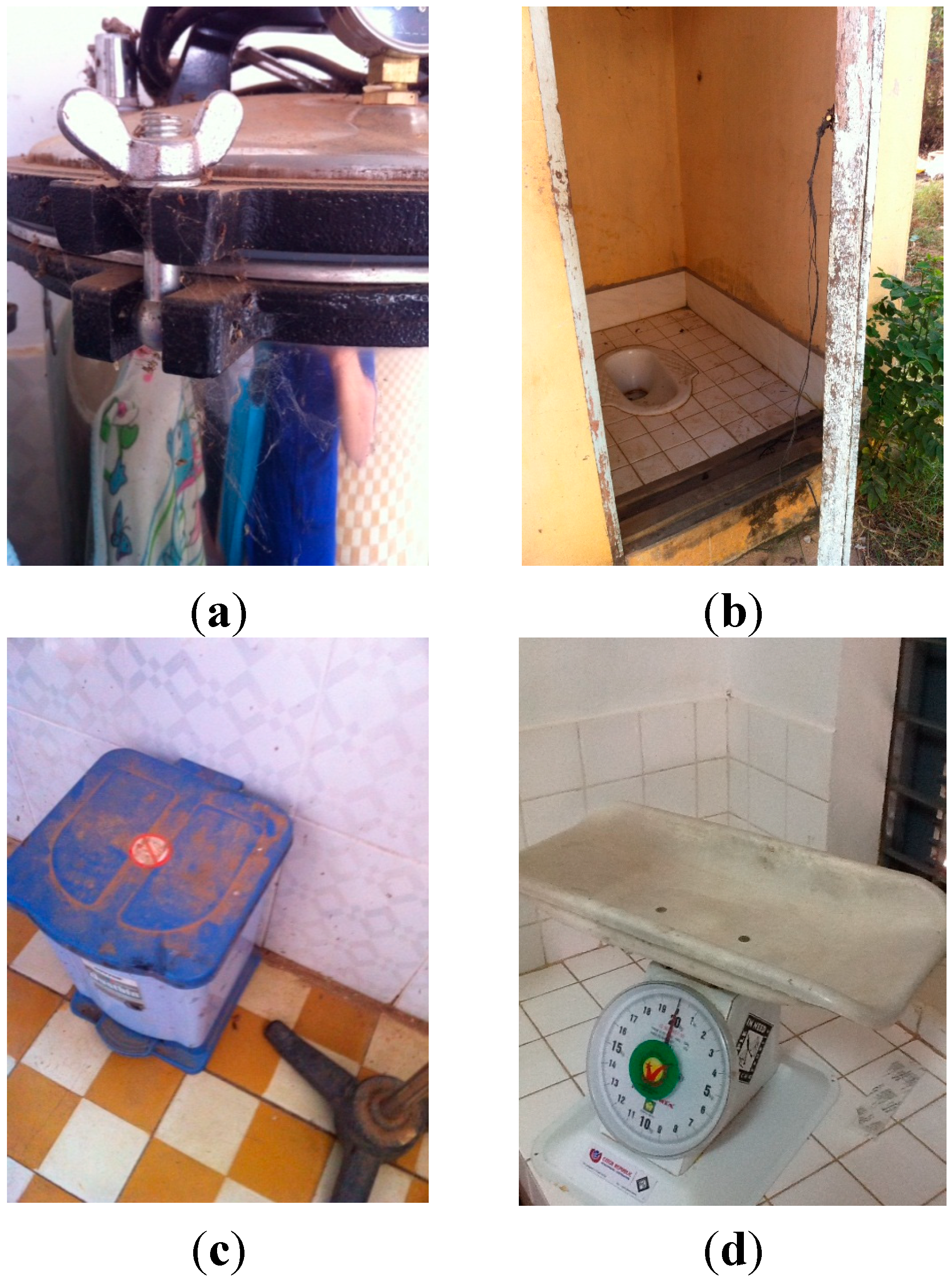
3.1. Immediate Newborn Care Environment: Structured Observations of Health Centers
3.1.1. Infrastructure
Electricity
Designated Delivery and Post-Delivery Rooms
Sufficient Lighting for Healthcare Activities
3.1.2. Hand Hygiene
3.1.3. Routine Cleaning
Condition of Floors, Operating Tables, Surfaces for Mother and Newborn
Availability of Cleaning Supplies and Equipment
3.1.4. Sanitation
Latrines
Sharps Disposal
3.1.5. Water
3.1.6. Sterilization
3.1.7. Health Care Equipment and Supplies
| Domain | Number of Health Centers with Feature | Number of Health Centers without Feature (Missing) |
|---|---|---|
| Infrastructure | ||
| Electricity | 9 | 1 |
| Backup electricity | 5 | 5 |
| Delivery room | 10 | 0 |
| Post-delivery room | 10 | 0 |
| Sufficient lighting in delivery room | 10 | 0 |
| Hand Hygiene | ||
| Adequate hand washing points | 1 | 9 |
| Soap present | 3 | 7 |
| Clean towels present for drying hands | 1 | 9 |
| Near toilets | 4 | 6 |
| Routine Cleaning | ||
| Delivery room clean | 7 | 3 |
| Post-delivery room clean | 6 | 4 |
| Newborn scale is clean | 3 | 7 |
| Delivery bed is clean | 5 | 5 |
| Detergent present for cleaning delivery room | 7 | 2 (1) |
| Disinfectant present for delivery room | 1 | 7 (2) |
| Brooms or mops present for cleaning | 9 | 0 (1) |
| Sanitation | ||
| Adequate toilets | 6 | 3 (1) |
| Toilets are clean | 1 | 9 |
| Toilets are accessible to all users | 4 | 6 |
| There is a sharps disposal present | 10 | 0 |
| Water | ||
| Indoor running water | 10 | 0 |
| Outdoor running water | 8 | 2 |
| Sterilization | ||
| Electric autoclave | 10 | 0 |
| Health Care Equipment and Supplies | ||
| Sterile or non-sterile gloves | 9 | 0 (1) |
| Plastic sheeting for delivery | 6 | 2 (2) |
| Clean towels or cloths for drying baby | 3 | 7 |
| Clean, sterile, unused umbilical clamps | 7 | 2 (1) |
3.2. Immediate Newborn Care Environment: Focus Group Discussions with Health Center Staff
The midwife who handles the delivery is responsible for all hygiene and cleaning after that delivery (the laundering of the white cloths (for drying baby), asking the family to clean the delivery room table and floor after the delivery, throwing away used supplies such as needles, sutures.(Primary midwife, 24 years old)
The hygiene is sometimes not good enough because the cleaner does not come often.(Primary midwife, 28 years old)
After the delivery we need to wash some items with soap and water then we will sterilize it later. So that is the scissors, forceps, catheter. Other items will be thrown away. We give the disposables such as the needles, sutures and other things to the family along with the placenta for them to bury somewhere.(Primary midwife, 24 years old)
We ask the family to sweep, use the broom and also to use dishwashing soap to clean the floor if the floor was tainted by amniotic water. It’s not usual that there is amniotic water on the floor. We use a bucket to catch amniotic water but it sometimes spills over onto the floor.(Primary midwife, 46 years old)
I did have training on infection prevention and control at midwifery training and it was mainly about how to prevent myself from getting HIV from a patient using the protective glasses, long gloves but also now we do HIV testing and refer those women who have HIV to delivery elsewhere.(Primary midwife, 24 years old)
Yes we do wash our hands with bar soap and then apply the gel before putting our gloves on. If we are rushing we just use 2 pairs of gloves. We use the same gloves from start to finish with the mother and the newborn. We don’t change the gloves until we are completely finished with the mom and the baby, including the weighing of the baby.
3.3. Post Partum Environment: The Home and Community
3.3.1. Home Observation and Interviews with Mothers and Primary Caregivers
| Environment | Number of Homes Observed with Feature or Behavior (n = 4) |
|---|---|
| Sanitation | |
| Toilet | 2 |
| Animals | |
| Presence of animals | 2 |
| Hand Hygiene | |
| Hand washing station at toilet | 0 |
| Water at hand washing station | 0 |
| Soap at hand washing station | 0 |
| Source of Drinking Water | |
| Well water | 2 |
| Pond water | 1 |
| Bottled water (purchased) | 1 |
| Behaviors and Newborn Care | |
| Washed hands before touching newborn | 0 |
| Changed diaper when soiled | 3 |
| Bathed newborn | 3 |
We never wash hand before touching the baby, because every time we hold the baby is for giving bath, so we don’t need to wash our hands, for me during the baby was under 1 month old, I did nothing, I rest on the bed all the time and I didn’t touch anything. I wash my hands every time I use the toilet.(Mother, 23 years old)
We mostly don’t wash hands before touching the baby, but I wash my hands after using the bathroom.(Mother, 31 years old)
My mother always washed her hands before taking care (of the newborn). I only wash my hands during my regular shower, 3 times a day.(Mother, 27 years old)
I never paid any attention to hand washing, there’s not enough time, or I forget. So when I finish weaving I just take the baby (without washing my hands). I don’t have a hand washing habit. I was told by the midwife to wash hands.(Mother, 38 years old)
I have heard advice about washing hands regularly and I practice that. Especially before eating anything. And I also heard that after toilet you should wash hands. I know that is to protect from germs in the stool that you might touch. These germs from the stool can be anywhere in the area of the latrine, they can be everywhere we cannot see. But sometimes we do not wash our hands before touching the baby. Yes that happens.(Grandmother, 55 years old)

There are 142 total households and most get water from shared well. Some wells have clear water and use for cooking/drinking, other wells are not clear (and only used) for laundry. Only 2–3 families have pond in dry season. Rainy season have more ponds and they use that water for washing clothes, bathing or boil for drinking.(Village Chief, 72 years old, male)
Mothers leave babies with grandmas to go to the field and the grandmas give baby unclean water with sugar (making them ill). If the mother doesn’t clean the house, the baby will get a lot of sickness, and get into a bad condition because of the dust in the house. Families in not so good condition store water in huge clay jars outside the house, but families in good condition use machine to filter water. Some also boil water to avoid diarrhea.(Village Health Volunteer, 46 years old, female)


We have 12 (cloth) diapers and washed 2 times a day all with well water, (we use) cold water in well container, powder soap, my husband does it. Paper towel from the diapers is buried or burned.(Mother, 22 years old)
During that 1st month, the baby only received condensed milk mixed with water.(Father, 30 years old)
I gave (baby) water with spoon and cup, boiled water, each time after breastfeeding.(Mother, 26 years old)

4. Discussion
4.1. Findings and Discussion
4.2. Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- You, D.; Bastian, P.; Wu, J.; Wardlow, T. Levels and Trends in Child Mortality. Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation Report; UNICEF, WHO, The World Bank, and United Nations: New York, NY, USA, 2013. [Google Scholar]
- Lawn, J.; Blencowe, H.; Oza, S.; You, D.; Lee, A.; Waiswa, P.; Lalli, M.; Bhutta, Z.; Barros, A.; Christian, P.; et al. Every newborn: Progress, priorities, and potential beyond survival. Lancet 2014, 384, 189–205. [Google Scholar]
- Ministry of Health, Kingdom of Cambodia. Fast Track Initiative Road Map for Reducing Maternal & Newborn Mortality; Ministry of Health: Phonm Penh, Cambodia, 2010. [Google Scholar]
- Liljestrand, J.; Sambath, M.R. Socio-economic improvements and health system strengthening of maternity care are contributing to maternal mortality reduction in Cambodia. Reprod. Health Matters 2012, 20, 62–72. [Google Scholar] [CrossRef]
- Kuruvilla, S.; Schweizer, J.; Bishai, D.; Chowdhury, S.; Caramani, D.; Frost, L.; Cortez, R.; Daelmans, B.; de Francisco, A.; Adam, T.; et al. Success factors for reducing maternal and child mortality. Bull. World Health Organ. 2014, 92, 465–544. [Google Scholar]
- World Health Organization. Trends in Maternal Mortality: 1990 to 2013. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- National Institute of Statistics, Directorate General for Health, ICF Macro. Cambodia Demographic and Health Survey 2005; National Institute of Public Health: Phnom Penh, Cambodia, 2006. [Google Scholar]
- National Institute of Statistics, Directorate General for Health, and ICF Macro. Cambodia Demographic and Health Survey 2010; National Institute of Statistics Directorate General for Health ICF Macro: Phnom Penh, Cambodia, 2011. [Google Scholar]
- Liu, L.; Johnson, H.L.; Cousens, S.; Perin, J.; Scott, S.; Lawn, J.E.; Rudan, I.; Campbell, H.; Cibulskis, R.; Li, M.; et al. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet 2012, 379, 2151–2161. [Google Scholar]
- Lawn, J.; Wilczynska-Ketende, K.; Cousens, S. Estimating the causes of 4 million neonatal deaths in the year 2000. Int. J. Epidemiol. 2006, 35, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Blencowe, H.; Vos, T.; Lee, A.C.; Philips, R.; Lozano, R.; Alvarado, M.R.; Cousens, S.; Lawn, J.E. Estimates of neonatal morbidities and disabilities at regional and global levels for 2010: Introduction, methods overview, and relevant findings from the Global Burden of Disease study. Pediatr. Res. 2013, 74, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar]
- National Maternal Child Health Center. Verbal Autopsy Study Svay Rieng; National Maternal Child Health Center: Phnom Penh, Cambodia, 2009. [Google Scholar]
- Blencowe, H.; Cousens, S.; Mullany, L.; Lee, A.; Kerber, K.; Wall, S.; Darmstadt, G.; Lawn, J. Clean birth and postnatal care practices to reduce neonatal deaths from sepsis and tetanus: A systematic review and Delphi estimation of mortality effect. BMC Public Health 2011, 11. [Google Scholar] [CrossRef] [PubMed]
- Ganatra, H.; Stoll, B.; Zaidi, A. International perspective on early-onset neonatal sepsis. Clin. Perinatol. 2010, 37, 501–523. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, A.K.; Huskins, W.C.; Thaver, D.; Bhutta, Z.A.; Abbas, Z.; Goldmann, D.A. Hospital-acquired neonatal infections in developing countries. Lancet 2005, 365, 1175–1188. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.; Mrcog, M.R. Guidelines for Perinatal Care, 6th ed.; James, A., Lemnos, M.F., Charles, J., Lockwood, M.A., Eds.; Amer Academy of Pediatrics: Elk Grove Village, IL, USA, 2008; pp. 303–344. [Google Scholar]
- Lawn, J.; Cousens, S.; Zupan, J. 4 Million neonatal deaths: When? Where? Why? Lancet 2005, 365, 891–900. [Google Scholar] [CrossRef]
- World Health Organization. World Health Statistics 2011; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Curtis, V.; Cairncross, S.; Yonli, R. Review: Domestic hygiene and diarrhoea-pinpointing the problem. Trop. Med. Int. Health 2000, 5, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Bukenya, G.B.; Nwokolo, N. Compound hygiene, presence of standpipe and the risk of childhood diarrhoea in an urban settlement of Papua New Guinea. Int. J. Epidemiol. 1991, 20, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Biran, A.; Rabie, T.; Schmidt, W.; Juvekar, S.; Hirve, S.; Curtis, V. Comparing the performance of indicators of hand-washing practices in rural Indian households. Trop. Med. Int. Health 2008, 13, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Manun’Ebo, M.; Cousens, S.; Haggerty, P.; Kalengaie, M.; Ashworth, A.; Kirkwood, B. Measuring hygiene practices: A comparison of questionnaires with direct observations in rural Zaire. Trop. Med. Int. Health 1997, 2, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Greenland, K.; Iradati, E.; Ati, A.; Maskoen, Y.Y.; Aunger, R. The context and practice of handwashing among new mothers in Serang, Indonesia: A formative research study. BMC Public Health 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- Rhee, V.; Mullany, L.C.; Khatry, S.K.; Katz, J.; LeClerq, S.C.; Darmstadt, G.L.; Tielsch, J.M. Maternal and birth attendant hand washing and neonatal mortality in southern Nepal. Arch. Pediatr. Adolesc. Med. 2008, 162, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Ith, P.; Dawson, A.; Homer, C.S.; Klinken Whelan, A. Practices of skilled birth attendants during labour, birth and the immediate postpartum period in Cambodia. Midwifery 2013, 29, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Mrisho, M.; Schellenberg, J.A.; Mushi, A.K.; Obrist, B.; Mshinda, H.; Tanner, M.; Schellenberg, D. Understanding home-based neonatal care practice in rural southern Tanzania. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 669–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moyer, C.A.; Aborigo, R.A.; Logonia, G.; Affah, G.; Rominski, S.; Adongo, P.B.; Williams, J.; Hodgson, A.; Engmann, C. Clean delivery practices in rural northern Ghana: A qualitative study of community and provider knowledge, attitudes, and beliefs. BMC Pregnancy Childb. 2012, 12. [Google Scholar] [CrossRef]
- Shamba, D.D.; Schellenberg, J.; Penfold, S.C.; Mashasi, I.; Mrisho, M.; Manzi, F.; Marchant, T.; Tanner, M.; Mshinda, H.; Schellenberg, D.; et al. Clean home-delivery in rural Southern Tanzania: Barriers, influencers, and facilitators. J. Health Popul. Nutr. 2013, 31, 110–117. [Google Scholar]
- Hill, Z.; Tawiah-Agyemang, C.; Okeyere, E.; Manu, A.; Fenty, J.; Kirkwood, B. Improving hygiene in home deliveries in rural Ghana: How to build on current attitudes and practices. Pediatr. Infect. Dis. J. 2010, 29, 1004–1008. [Google Scholar] [CrossRef] [PubMed]
- Bhutta, Z.A.; Darmstadt, G.L.; Hasan, B.S.; Haws, R.A. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: A review of the evidence. Pediatrics 2005, 115, 519–617. [Google Scholar] [PubMed]
- Clasen, T.; Boisson, S.; Routray, P.; Torondel, B.; Bell, M.; Cumming, O.; Ensink, J.; Freeman, M.; Jenkins, M.; Odagiri, M.; et al. Effectiveness of a rural sanitation programme on diarrhoea, soil-transmitted helminth infection, and child malnutrition in Odisha, India: A cluster-randomised trial. Lancet Glob. Health 2014, 2, e645–e653. [Google Scholar]
- Bowen, A.; Agboatwalla, M.; Ayers, T.; Tobery, T.; Tariq, M.; Luby, S.P. Sustained improvements in handwashing indicators more than 5 years after a cluster-randomised, community-based trial of handwashing promotion in Karachi, Pakistan. Trop. Med. Int. Health 2013, 18, 259–267. [Google Scholar] [PubMed]
- Biran, A.; Schmidt, W.-P.; Varadharjan, K.S.; Rajaraman, D.; Kumar, R.; Greenland, K.; Gopalan, B.; Aunger, R.; Curtis, V. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): A cluster-randomised trial. Lancet Glob. Health 2014, 2, e145–e154. [Google Scholar] [CrossRef] [PubMed]
- Curtis, V.A.; Danquah, L.O.; Aunger, R.V. Planned, motivated and habitual hygiene behaviour: An eleven country review. Health Educ. Res. 2009, 24, 655–673. [Google Scholar] [CrossRef] [PubMed]
- Huis, A.; van Achterberg, T.; de Bruin, M.; Grol, R.; Schoonhoven, L.; Hulscher, M. A systematic review of hand hygiene improvement strategies: A behavioural approach. Implement. Sci. IS 2012, 7. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bazzano, A.N.; Oberhelman, R.A.; Potts, K.S.; Gordon, A.; Var, C. Environmental Factors and WASH Practices in the Perinatal Period in Cambodia: Implications for Newborn Health. Int. J. Environ. Res. Public Health 2015, 12, 2392-2410. https://doi.org/10.3390/ijerph120302392
Bazzano AN, Oberhelman RA, Potts KS, Gordon A, Var C. Environmental Factors and WASH Practices in the Perinatal Period in Cambodia: Implications for Newborn Health. International Journal of Environmental Research and Public Health. 2015; 12(3):2392-2410. https://doi.org/10.3390/ijerph120302392
Chicago/Turabian StyleBazzano, Alessandra N., Richard A. Oberhelman, Kaitlin Storck Potts, Anastasia Gordon, and Chivorn Var. 2015. "Environmental Factors and WASH Practices in the Perinatal Period in Cambodia: Implications for Newborn Health" International Journal of Environmental Research and Public Health 12, no. 3: 2392-2410. https://doi.org/10.3390/ijerph120302392







