Prevalence and Risk Factors Associated with Dyslipidemia in Chongqing, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population Sample
2.2. Data Collection and Measurements
2.3. Definitions of Variables
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Population
3.2. Prevalence of Dyslipidemia
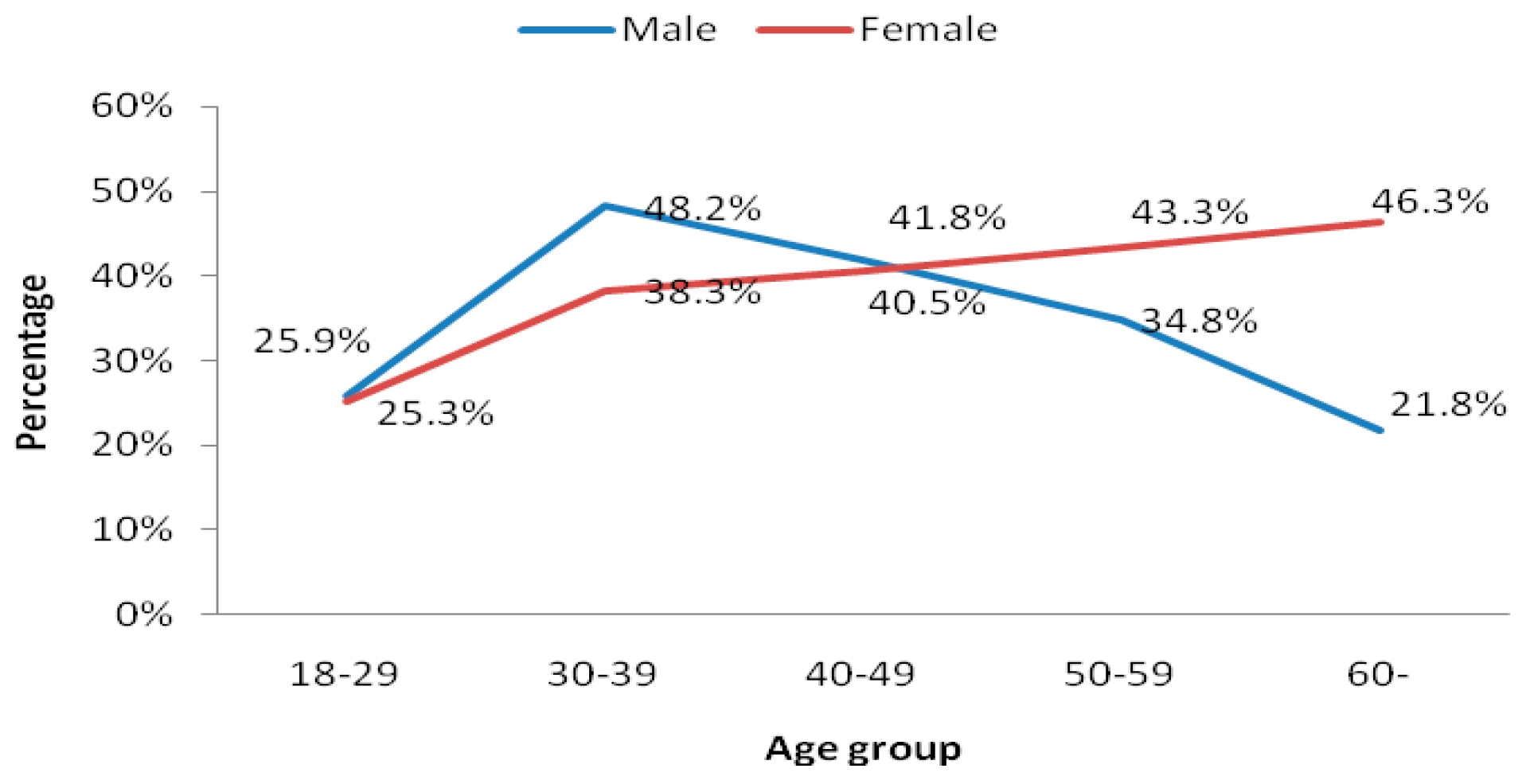
3.3. Gender and Age Difference in Dyslipidemia Prevalence
| Characteristics | Total (n = 5375) | Male (n = 2030) | Female (n = 3345) | p-Value |
|---|---|---|---|---|
| TG (mmol/L), geometric mean | 1.74 | 1.74 | 1.75 | 0.791 |
| TC (mmol/L), mean (SD) | 4.9 ± 1.0 | 4.9 ± 0.9 | 5.1 ± 0.1 | 0.000 |
| HDL_C (mmol/L), mean (SD) | 1.5 ± 0.4 | 1.5 ± 0.5 | 1.6 ± 0.4 | 0.000 |
| Dyslipidemia, % (95% CI) | 37.4 (36.7, 38.0) | 29.1 (28.2, 30.2) | 42.4 (41.5, 43.3) | 0.000 |
| Isolated hypertriglyceridemia, % (95% CI) | 16.5 (16.0, 17.0) | 16.3 (15.5, 17.1) | 16.6 (16.0, 17.3) | 0.762 |
| Isolated hypercholesterolemia, % (95% CI) | 5.5 (5.2, 5.8) | 3.5 (3.1. 3.9) | 6.7 (6.3, 7.1) | 0.000 |
| Mixed hyperlipidemia, % (95% CI) | 4.9 (4.6, 5.2) | 4.2 (3.8, 4.6) | 5.4 (5.0, 5.8) | 0.067 |
| Isolated low HDL-C, % (95% CI) | 10.5 (10.0, 10.9) | 5.1 (4.6, 5.6) | 13.7 (13.1, 14.3) | 0.000 |
| Age-standardized dyslipidemia *, % (95% CI) | 35.5 (34.8, 36.1) | 34.4 (33.3, 35.4) | 37.6 (36.7, 38.4) | 0.000 |
3.4. Factors Associated with Dyslipidemia
| Characteristics | All subjects (n = 5375) | Male (n = 2037) | Female (n = 3357) | With Dyslipidemia (n = 2009 ) | Without Dyslipidemia (n = 3366) | p-Value * | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Isolated Hypertriglyceridemia (n = 887) | Isolated Hypercholesterolemia (n = 295) | Mixed Hyperlipidemia (n = 265) | Isolated Low HDL-C (n = 562) | ||||||
| Male, n (%) | 2030 (37.8) | − | − | 592 (29.5) | 331 (37.3) | 71 (24.1) | 86 (32.5) | 104 (18.5) | 1438 (42.7) | 0.000 |
| Age (years), mean (SD) | 57.7 (13.2) | 59.7 (13.2) | 56.6 (13.1) | 57.1 (12.6) | 57.0 (12.3) | 60.8 (10.6) | 58.5 (11.4) | 54.7 (14.1) | 58.1 (13.5) | 0.002 |
| ≥Junior high school education | 614 (11.4) | 298 (14.6) | 316 (9.4) | 259 (12.8) | 127 (14.3) | 16 (5.4) | 30 (11.3) | 86 (15.3) | 355 (10.5) | 0.009 |
| BMI (kg/m2), mean (SD) | 23.9 (3.4) | 23.4 (3.2) | 24.2 (3.4) | 25.1 (3.3) | 25.5 (3.4) | 23.9 (3.1) | 25.8 (3.1) | 24.9 (3.4) | 23.2 (3.1) | 0.002 |
| WC (cm), mean (SD) | 81.9 (9.4) | 82.6 (9.5) | 81.5 (9.4) | 85.1 (9.5) | 86.5 (9.3) | 82.0 (9.3) | 87.2 (8.8) | 85.1 (9.5) | 80.0 (8.9) | 0.001 |
| Regular physical activity, n (%) | 2014 (37.5) | 603 (29.1) | 1411 (42.0) | 607 (30.2) | 290 (32.7) | 72 (24.4) | 60 (22.6) | 185 (32.9) | 1407 (41.8) | 0.002 |
| Habitual drinking, n (%) | 4086 (76.0) | 1810 (88.8) | 2276 (67.8) | 1612 (80.2) | 675 (76.1) | 241 (81.7) | 206 (77.7) | 490 (87.2) | 2474 (73.5) | 0.000 |
| Current smoking, n (%) | 3141 (58.4) | 1752 (86.0) | 1389 (41.4) | 1202 (59.8) | 511 (57.6) | 169 (57.3) | 147 (55.5) | 375(66.7) | 1939 (57.6) | 0.109 |
| Variables | Male | Female | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age, per 10-year increment | 0.82 (0.78, 0.86) | 0.000 | 1.16 (1.13, 1.19) | 0.000 |
| ≥Junior high school education | 1.35 (1.20, 1.50) | 0.043 | 1.26 (1.14, 1.39) | 0.046 |
| Regular physical activity | 0.79 (0.68, 0.90) | 0.032 | 0.83 (0.76, 0.91) | 0.020 |
| Central obesity # | 1.90 (1.76, 2.04) | 0.000 | 1.72 (1.63, 1.80) | 0.000 |
| Obesity # | 2.73 (2.61, 2.85) | 0.000 | 1.52 (1.45, 1.59) | 0.000 |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
References
- Jayarama, N.; Lakshmaiah, M.R. Prevalence and pattern of dyslipidemia in type 2 diabetes mellitus patients in a rural tertiary care centre, southern India. Glob. J. Med. Public Health 2012, 1, 24–27. [Google Scholar]
- Zhou, X.; Zhang, W.; Liu, X.; Li, Y. Interrelationship between diabetes and periodontitis: Role of hyperlipidemia. Arch. Oral. Biol. 2014, 60, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Snehalatha, C.; Nanditha, A.; Shetty, A.S.; Ramachandran, A. Hypertriglyceridaemia either in isolation or in combination with abdominal obesity is strongly associated with atherogenic dyslipidaemia in Asian Indians. Diabetes Res. Clin. Pract. 2011, 94, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Berenson, G.S.; Srinivasan, S.R.; Bao, W.; Newman, W.P., 3rd; Tracy, R.E.; Wattigney, W.A. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa heart study. N. Engl. J. Med. 1998, 338, 1650–1656. [Google Scholar] [CrossRef] [PubMed]
- Djelilovic-Vranic, J.; Alajbegovic, A.; Zelija-Asimi, V.; Niksic, M.; Tiric-Campara, M.; Salcic, S.; Celo, A. Predilection role diabetes mellitus and dyslipidemia in the onset of ischemic stroke. Med. Arch. 2013, 67, 120–123. [Google Scholar] [CrossRef] [PubMed]
- Tziomalos, K.; Athyros, V.G.; Karagiannis, A.; Mikhailidis, D.P. Dyslipidemia as a risk factor for ischemic stroke. Curr. Top. Med. Chem. 2009, 9, 1291–1297. [Google Scholar] [CrossRef] [PubMed]
- Stamler, J.; Daviglus, M.L.; Garside, D.B.; Dyer, A.R.; Greenland, P.; Neaton, J.D. Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. JAMA 2000, 284, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Vergani, C.; Lucchi, T. Plasma HDL cholesterol and risk of myocardial infarction. Lancet 2012, 380, 1989–1990. [Google Scholar] [CrossRef]
- Joint committee for developing Chinese guidelines on prevention and treatment of dyslipidemia in adults. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 2007, 35, 390–419. (In Chinese) [Google Scholar]
- Cai, L.; Zhang, L.; Liu, A.; Li, S.; Wang, P. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China. J. Atheroscler. Thromb. 2012, 19, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Xu, L.; Jonas, J.B.; You, Q.S.; Wang, Y.X.; Yang, H. Prevalence and associated factors of dyslipidemia in the adult Chinese population. PLoS ONE 2011. [Google Scholar] [CrossRef] [PubMed]
- Kish, L. A procedure for objective respondent selection within the household. J. Am. Stat. Assoc. 1949, 44, 380–387. [Google Scholar] [CrossRef]
- Marchesini, G.; Forlani, G.; Cerrelli, F.; Manini, R.; Natale, S.; Baraldi, L.; Ermini, G.; Savorani, G.; Zocchi, D.; Melchionda, N. Who and atpiii proposals for the definition of the metabolic syndrome in patients with type 2 diabetes. Diabetic Med. 2004, 21, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.G.; Peng, Y.D. Metabolic syndrome and non-alcoholic fatty liver disease: Asian definitions and Asian studies. Hepatob. Pancreat. Dis. Int. 2007, 6, 572–578. [Google Scholar]
- Anuurad, E.; Shiwaku, K.; Nogi, A.; Kitajima, K.; Enkhmaa, B.; Shimono, K.; Yamane, Y. The new bmi criteria for asians by the regional office for the western pacific region of who are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J. Occup. Health 2003, 45, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163.
- Fan, J.G.; Cai, X.B.; Li, L.; Li, X.J.; Dai, F.; Zhu, J. Alcohol consumption and metabolic syndrome among Shanghai adults: A randomized multistage stratified cluster sampling investigation. World J. Gastroenterol. 2008, 14, 2418–2424. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.H.; Zhang, J.; Zhai, Y.; You, Y.; Man, Q.Q.; Wang, C.R.; Li, H.; Li, Y.; Yang, X.G. Blood lipid profile and prevalence of dyslipidemia in Chinese adults. Biomed. Environ. Sci. 2007, 20, 329–335. [Google Scholar] [PubMed]
- Li, Z.; Yang, R.; Xu, G.; Xia, T. Serum lipid concentrations and prevalence of dyslipidemia in a large professional population in Beijing. Clin. Chem. 2005, 51, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Li, Q. Dyslipidemia among male university teaching and ministrative staffs in Beijing. Zhongguo Xue Xiao Wei Sheng 2012, 33, 883–884. (In Chinese) [Google Scholar]
- Wu, J.Y.; Duan, X.Y.; Li, L.; Dai, F.; Li, Y.Y.; Li, X.J.; Fan, J.G. Dyslipidemia in Shanghai, China. Prev. Med. 2010, 51, 412–415. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Fu, C. The prevalence and risk factors of dyslipidemia among residents in Guangdong, China. Huanan Yu Fang Yi Xue Za Zhi 2006, 5, 1–5. (In Chinese) [Google Scholar]
- Sharma, U.; Kishore, J.; Garg, A.; Anand, T.; Chakraborty, M.; Lali, P. Dyslipidemia and associated risk factors in a resettlement Colony of Delhi. J. Clin. Lipidol. 2013, 7, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Nadira Islam, Z.R.; Choudhury, S.; Afrin, L.; Rahman, S.; Aftabuddin, M. Prevalence of dyslipidemia and associated factors among the sub-urban Bangladeshi population. Univer. Heart J. 2012, 8, 15–19. [Google Scholar]
- De Souza, L.J.; Souto Filho, J.T.; de Souza, T.F.; Reis, A.F.; Gicovate Neto, C.; Bastos, D.A.; Cortes, V.A.; Chalita, F.E.; Teixeira, C.L. Prevalence of dyslipidemia and risk factors in Campos dos Goytacazes, in the Brazilian state of Rio de Janeiro. Arquivos Brasileiros de Cardiologia 2003, 81, 249–264. [Google Scholar] [CrossRef] [PubMed]
- Primatesta, P.; Poulter, N.R. Lipid concentrations and the use of lipid lowering drugs: Evidence from a national cross sectional survey. BMJ 2000, 321, 1322–1325. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; McGovern, P.G.; Jacobs, D.R., Jr.; Shahar, E.; Duval, S.; Blackburn, H.; Luepker, R.V. Fifteen-year trends in cardiovascular risk factors (1980–1982 through 1995–1997): The Minnesota heart survey. Amer. J. Epidemiol. 2002, 156, 929–935. [Google Scholar] [CrossRef]
- Chang, H.Y.; Yeh, W.T.; Chang, Y.H.; Tsai, K.S.; Pan, W.H. Prevalence of dyslipidemia and mean blood lipid values in Taiwan: Results from the nutrition and health survey in Taiwan (Nahsit, 1993–1996). Chin. J. Physiol. 2002, 45, 187–197. (In Chinese) [Google Scholar] [PubMed]
- Zhao, W.H.; Zhang, J.; You, Y.; Man, Q.Q.; Li, H.; Wang, C.R.; Zhai, Y.; Li, Y.; Jin, S.G.; Yang, X.G. Epidemiologic characteristics of dyslipidemia in people aged 18 years and over in China. Chin. J. Prev. Med. 2005, 39, 306–310. [Google Scholar]
- Erem, C.; Hacihasanoglu, A.; Deger, O.; Kocak, M.; Topbas, M. Prevalence of dyslipidemia and associated risk factors among Turkish adults: Trabzon lipid study. Endocrine 2008, 34, 36–51. [Google Scholar] [CrossRef] [PubMed]
- Li, L.M.; Rao, K.Q.; Kong, L.Z.; Yao, C.H.; Xiang, H.D.; Zhai, F.Y.; Ma, G.S.; Yang, X.G. A description on the chinese national nutrition and health survey in 2002. Zhonghua Liu Xing Bing Xue Za Zhi 2005, 26, 478–484. (In Chinese) [Google Scholar] [PubMed]
- Santos, A.C.; Barros, H. Prevalence and determinants of obesity in an urban sample of portuguese adults. Public Health 2003, 117, 430–437. [Google Scholar] [CrossRef]
- Hana, T.; AlMajed, A.T.A.; Ali, A.; Sadek, T.A.; AlMuaili, O.A.; AlMutairi, A.S.; Shaghouli, W.A. AlTorah Prevalence of dyslipidemia and obesity among college students in Kuwait. Alexandria J. Med. 2011, 47, 67–71. [Google Scholar]
- Lin, Y.C.; Yen, L.L.; Chen, S.Y.; Kao, M.D.; Tzeng, M.S.; Huang, P.C.; Pan, W.H. Prevalence of overweight and obesity and its associated factors: Findings from national nutrition and health survey in Taiwan, 1993–1996. Prev. Med. 2003, 37, 233–241. [Google Scholar] [CrossRef]
- Humayun, A.; Shah, A.S.; Alam, S.; Hussein, H. Relationship of body mass index and dyslipidemia in different age groups of male and female population of Peshawar. JAMC 2009, 21, 141–144. [Google Scholar] [PubMed]
- Bays, H.E.; Chapman, R.H.; Grandy, S. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: Comparison of data from two national surveys. Int. J. Clin. Pract. 2007, 61, 737–747. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Magno, C.P.; Lane, K.T.; Hinojosa, M.W.; Lane, J.S. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: Findings from the national health and nutrition examination survey, 1999 to 2004. J. Amer. Coll. Surgeons 2008, 207, 928–934. [Google Scholar] [CrossRef] [PubMed]
- Musunuru, K. Atherogenic dyslipidemia: Cardiovascular risk and dietary intervention. Lipids 2010, 45, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Paccaud, F.; Schluter-Fasmeyer, V.; Wietlisbach, V.; Bovet, P. Dyslipidemia and abdominal obesity: An assessment in three general populations. J. Clin. Epidemiol. 2000, 53, 393–400. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qi, L.; Ding, X.; Tang, W.; Li, Q.; Mao, D.; Wang, Y. Prevalence and Risk Factors Associated with Dyslipidemia in Chongqing, China. Int. J. Environ. Res. Public Health 2015, 12, 13455-13465. https://doi.org/10.3390/ijerph121013455
Qi L, Ding X, Tang W, Li Q, Mao D, Wang Y. Prevalence and Risk Factors Associated with Dyslipidemia in Chongqing, China. International Journal of Environmental Research and Public Health. 2015; 12(10):13455-13465. https://doi.org/10.3390/ijerph121013455
Chicago/Turabian StyleQi, Li, Xianbin Ding, Wenge Tang, Qin Li, Deqiang Mao, and Yulin Wang. 2015. "Prevalence and Risk Factors Associated with Dyslipidemia in Chongqing, China" International Journal of Environmental Research and Public Health 12, no. 10: 13455-13465. https://doi.org/10.3390/ijerph121013455





