Understanding the Social Context of the ASGM Sector in Ghana: A Qualitative Description of the Demographic, Health, and Nutritional Characteristics of a Small-Scale Gold Mining Community in Ghana
Abstract
:1. Introduction
2. Methods
3. Results and Discussion
3.1. Household Population and Housing Characteristics
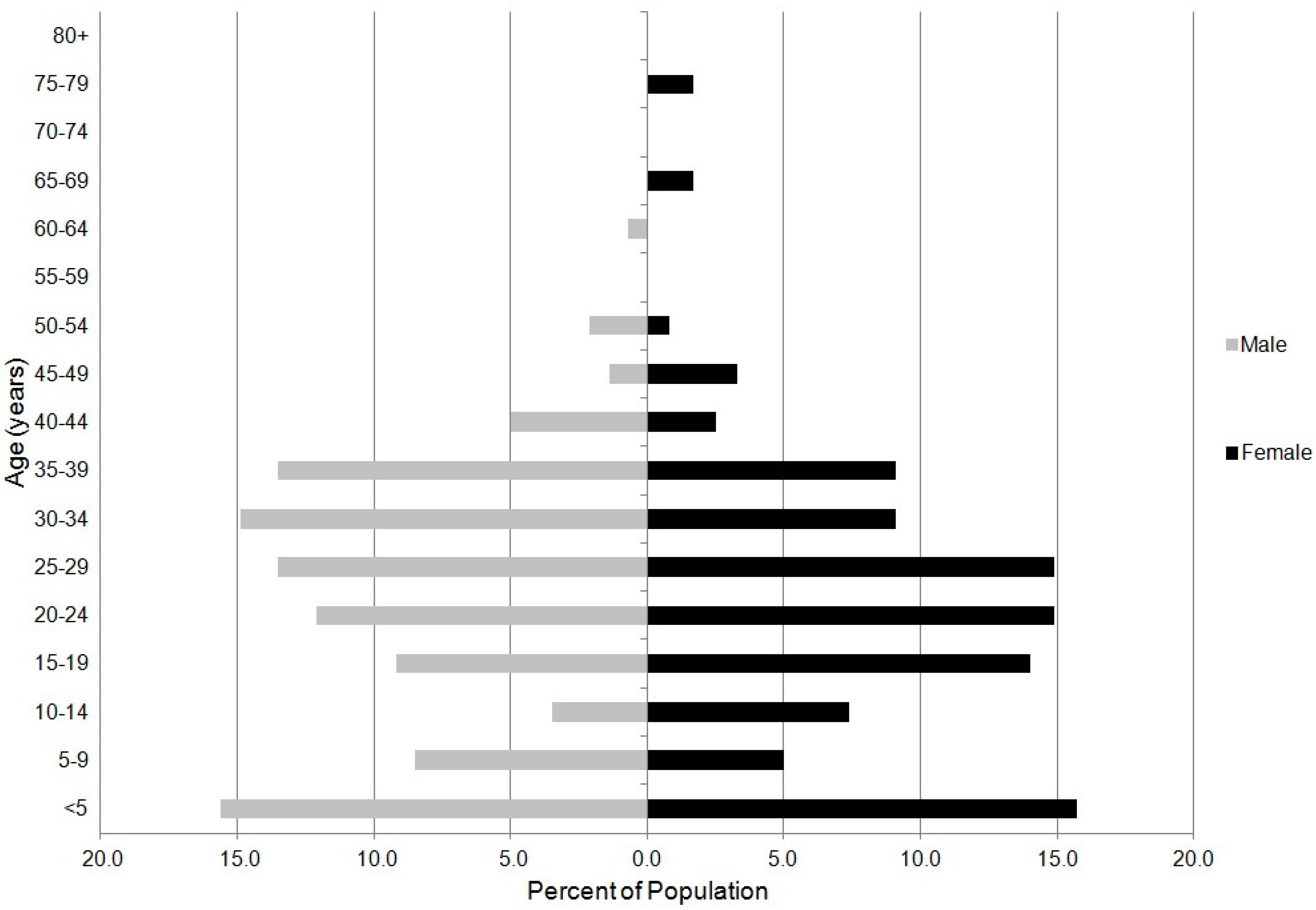
3.1.1. Population Characteristics
| Ghana DHS 2008 | Survey 2011 | |||
|---|---|---|---|---|
| Urban | Rural | Total | Kejetia | |
| Flooring Material | ||||
| Earth/sand | 3.8 | 21.5 | 13.0 | 74.1 |
| Dung | 0.1 | 2.0 | 1.1 | 0.0 |
| Wood/planks | 0.1 | 0.0 | 0.1 | 0.0 |
| Palm/bamboo | 0.0 | 0.0 | 0.0 | 0.0 |
| Parquet or polished wood | 0.2 | 0.0 | 0.1 | 0.0 |
| Ceramic tiles/terrazzo | 5.0 | 0.7 | 2.7 | 0.0 |
| Cement | 56.0 | 65.3 | 60.8 | 25.9 |
| Woolen carpet/synthetic carpet | 18.3 | 3.6 | 10.6 | 0.0 |
| Linoleum/rubber carpet | 16.2 | 6.8 | 11.3 | 0.0 |
| Other | 0.3 | 0.0 | 0.1 | 0.0 |
| Total | 100.0 | 99.9 | 99.8 | 100.0 |
| Rooms used for sleeping | ||||
| One | 63.4 | 56.3 | 59.7 | 38.9 |
| Two | 23.8 | 26.0 | 24.9 | 35.2 |
| Three or more | 12.0 | 17.4 | 14.8 | 26.1 |
| Missing | 0.8 | 0.4 | 0.6 | 0.0 |
| Total | 100.0 | 100.1 | 100.0 | 100.2 |
| Place for cooking ** | ||||
| In the house | 46.6 | 33.5 | 39.8 | 16.7 |
| In a separate building | 11.2 | 26.5 | 19.2 | 7.4 |
| Outdoors | 37.9 | 37.5 | 37.7 | 64.8 |
| Other | NA | NA | NA | 1.9 |
| Missing | 4.3 | 2.5 | 3.3 | 11.1 |
| Total | 100.0 | 100.0 | 100.0 | 101.9 |
| Cooking fuel | ||||
| Electricity | 0.9 | 0.2 | 0.5 | 0 |
| LPG/natural gas/biogas | 24 | 3.1 | 13.1 | 0 |
| Kerosene | 0.8 | 0.2 | 0.5 | 0 |
| Charcoal | 55.9 | 18.9 | 36.6 | 66.7 |
| Wood | 14.1 | 74.9 | 45.8 | 20.4 |
| Straw/shrubs/grass | 0.1 | 0.2 | 0.2 | 0 |
| No food cooked in household | 4.3 | 2.4 | 3.3 | 11.1 |
| Missing | -- | -- | -- | 1.9 |
| Total | 100.1 | 99.9 | 100.0 | 100.1 |
| Percentage using solid fuel * | 70.1 | 94.0 | 82.6 | 94.0 |
| Type of fire/stove among households using solid fuels * | ||||
| Closed stove/coal pot with chimney | 0.1 | 0.2 | 0.2 | 0.0 |
| Open fire/coal pot/open stove without chimney or hood | 99.8 | 99.7 | 99.8 | 100.0 |
| Missing | 0.1 | 0.1 | 0.1 | 0.0 |
| Total | 100.0 | 100.0 | 100.1 | 100.0 |
3.1.2. Household Characteristics and Amenities

3.1.3. Water
3.2. Characteristics of Survey Respondents
3.2.1. Education
3.2.2. Exposure to Mass Media
3.2.3. Employment
3.2.4. Health Insurance
3.2.5. Tobacco Usage
3.3. Maternal and Child Health
Delivery and Antenatal Care
| Percent distribution of women age 15–49 who had a live birth in the five years preceding the survey by antenatal care (ANC) provider | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Doctor | Nurse/Midwife | Auxiliary Midwife | Community Health Officer | Traditional Birth Attendant (Trained) | Traditional Birth Attendant (Untrained) | Other | No One | Missing | Total | Percentage Receiving Antenatal Care from a Skilled Provider * | |
| Residence | |||||||||||
| Urban | 33.9 | 60.1 | 2.0 | 1.8 | 0.3 | 0.0 | 0.3 | 1.4 | 0.2 | 100.0 | 97.8 |
| Rural | 16.4 | 65.3 | 4.3 | 7.8 | 0.2 | 0.1 | 1.0 | 4.8 | 0.1 | 100.0 | 93.9 |
| Region | |||||||||||
| Upper East | 14.3 | 67.9 | 0.7 | 12.9 | 0.0 | 0.0 | 0.0 | 3.7 | 0.6 | 100.0 | 95.7 |
| Total | 23.5 | 63.2 | 3.4 | 5.4 | 0.2 | 0.1 | 0.7 | 3.5 | 0.1 | 0.0 | 95.4 |
| Kejetia 2010 | 3.3 | 76.7 | 0.0 | 6.7 | 0.0 | 3.3 | 0.0 | 3.3 | 6.7 | 100.1 | 86.7 |
| Percent distribution of live births in the five years preceding the survey by person providing assistance during delivery | |||||||||||
| Residence | |||||||||||
| Urban | 19.6 | 61.6 | 2.6 | 0.6 | 8.6 | 3.5 | 2.0 | 1.2 | 0.4 | 100.1 | 84.3 |
| Rural | 5.8 | 32.8 | 2.3 | 2.0 | 20.8 | 20.5 | 11.9 | 3.4 | 0.5 | 100.0 | 43.0 |
| Region | |||||||||||
| Upper East | 1.4 | 33.7 | 3.8 | 7.8 | 6.5 | 16.0 | 27.7 | 2.2 | 0.9 | 100.0 | 46.7 |
| Total | 11.0 | 43.7 | 2.4 | 1.5 | 16.2 | 14.1 | 8.1 | 2.5 | 0.5 | 0.0 | 58.7 |
| Kejetia 2010 ** | 3.4 | 48.3 | 3.4 | 3.4 | 0.0 | 13.8 | 17.2 | 0.0 | 10.3 | 100.0 | 58.5 |
3.4. Malaria
Mosquito Net Ownership and Usage
3.5. Diet and Nutrition
3.5.1. Diet and Nutrition
| Ghana DHS 2008 | Survey 2011 | ||||
|---|---|---|---|---|---|
| Urban * | Rural * | Upper East * | Total | Kejetia ** | |
| Milk | 27.9 | 10.5 | 15.4 | 17.2 | 45.2 |
| Tea/coffee | 31.7 | 14.8 | 23.1 | 21.3 | 16.1 |
| Other liquids (including alcohol) | 21.1 | 12.2 | 7.7 | 15.6 | 19.4 |
| Foods made from grains | 88.2 | 84.7 | 96.5 | 86.0 | 100.0 |
| Foods made from roots/tubers | 59.0 | 69.1 | 41.9 | 65.2 | 9.7 |
| Foods made from legumes | 24.2 | 27.7 | 35.0 | 26.4 | 51.6 |
| Meat/fish/shellfish/poultry/eggs | 93.5 | 84.8 | 82.7 | 88.1 | 100.0 |
| Cheese/yogurt | 12.4 | 4.3 | 5.4 | 7.4 | 0.0 |
| Vitamin A-rich fruits/vegetables | 59.2 | 62.8 | 95.5 | 61.4 | 48.4 |
| Other fruits/vegetables | 68.9 | 62.3 | 57.2 | 64.8 | 25.8 |
| Other solid or semi-solid food | 27.5 | 26.4 | 70.6 | 26.8 | 0.0 |
| Foods made with oil/fat/butter | 59.8 | 47.5 | 59.4 | 52.2 | 74.2 |
| Sugary foods | 22.8 | 12.8 | 14.6 | 16.6 | 16.1 |
| Number of women | 571 | 921 | 81 | 1492 | 31 |
3.5.2. Dietary Diversity
4. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Bank. Communities and Small-Scale Mining (CASM); World Bank: New York, NY, USA, 2008; pp. 1–4. [Google Scholar]
- United Nations Environment Programme (UNEP). Global Mercury Assessment 2013: Sources, Emissions, Releases and Environmental Transport; UNEP: Geneva, Switzerland, 2013. [Google Scholar]
- Tschakert, P.; Laliberte, N. Contaminated identities: Understanding human and environmental risks and livelihood options among small-scale gold miners in Ghana. In Environment and Health in Sub-Saharan Africa: Managing an Emerging Crisis; Luginaah, I.N., Yanful, E.K., Eds.; Springer: Dordrecht, The Netherlands, 2009; pp. 65–75. [Google Scholar]
- Hilson, G.M. Harvesting mineral riches: 1000 years of gold mining in Ghana. Resour. Policy 2002, 28, 13–26. [Google Scholar] [CrossRef]
- United Nations. United Nations International Merchandise Trade Statistics Yearbook 2013: Ghana; United Nationa: New York, NY, USA, 2013. [Google Scholar]
- Bawa, I. A viewpoint on small-scale gold mining in Ghana: A regulatory perspective on current practices, mercury use and the UNIDO and EU projects. Int. J. Environ. Pollut. 2010, 41, 195–201. [Google Scholar] [CrossRef]
- Mohammed Banchirigah, S. How have reforms fuelled the expansion of artisanal mining? Evidence from sub-Saharan Africa. Resour. Policy 2006, 31, 165–171. [Google Scholar] [CrossRef]
- Sackey, H. Poverty in Ghana from an assets-based perspective: An application of probit technique. Afr. Dev. Bank 2005, 17, 41–69. [Google Scholar] [CrossRef]
- Banchirigah, S.M.; Hilson, G.M. De-agrarianization, re-agrarianization and local economic development: Re-orientating livelihoods in African artisanal mining communities. Policy Sci. 2009, 43, 157–180. [Google Scholar] [CrossRef]
- Hilson, G.M.; Clifford, M.J. Small-scale gold mining, the environment and human health: An introduction to the Ghana case. Int. J. Environ. Pollu. 2010, 41, 185–194. [Google Scholar] [CrossRef]
- Hilson, G.M. Child labour in African artisanal mining communities: Experiences from northern Ghana. Dev. Change 2010, 41, 445–473. [Google Scholar] [CrossRef]
- Long, R.; Renne, E.; Robins, T.; Wilson, M.; Pelig-ba, K.; Rajaee, M.; Yee, A.; Koomson, E.; Sharp, C.; Lu, J.; Basu, N. Water values in a Ghanaian small-scale gold mining community. Hum. Organ. 2013, 72, 199–210. [Google Scholar] [CrossRef]
- Basu, N.; Clarke, E.; Green, A.; Long, R.; Calys-Tagoe, B.; Chan, L.H.M.; Dzodzomenyo, M.; Fobil, J.N.; Neitzel, R.L.; Obiri, S.; Odei, E.; Ovadje, L.; Rajaee, M.; Quansah, R.; Wilson, M.L. Integrated assessment of artisanal and small-scale gold mining in Ghana—Part 1: Human health review. Int. J. Environ. Res. Public Heal. 2015, 12, 5143–5176. [Google Scholar] [CrossRef] [PubMed]
- Nartey, V.; Klake, R.K.; Hayford, E.; Doamekpor, L.K.; Appoh, R. Assessment of mercury pollution in rivers and streams around artisanal gold mining areas of the Birim North District of Ghana. J. Environ. Prot. (Irvine Calif.). 2011, 2, 1227–1239. [Google Scholar]
- Bose-O’Reilly, S.; Lettmeier, B.; Gothe, R.M.; Beinhoff, C.; Siebert, U.; Drasch, G. Mercury as a serious health hazard for children in gold mining areas. Environ. Res. 2008, 107, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Adimado, A.A.; Baah, D.A. Mercury in human blood, urine, hair, nail, and fish from the Ankobra and Tano River Basins in Southwestern Ghana. Bull. Environ. Contam. Toxicol. 2002, 68, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Paruchuri, Y.; Siuniak, A.; Johnson, N.; Levin, E.; Mitchell, K.; Goodrich, J.M.; Renne, E.P.; Basu, N. Occupational and environmental mercury exposure among small-scale gold miners in the Talensi-Nabdam District of Ghana’s Upper East region. Sci. Total Environ. 2010, 408, 6079–6085. [Google Scholar] [CrossRef] [PubMed]
- Asante, K.A.; Agusa, T.; Subramanian, A.; Ansa-Asare, O.D.; Biney, C.A.; Tanabe, S.; Ansong, K. Contamination status of arsenic and other trace elements in drinking water and residents from Tarkwa, a historic mining township in Ghana. Chemosphere 2007, 66, 1513–1522. [Google Scholar] [CrossRef] [PubMed]
- Renne, E.P.; Basu, N.; Gager, E.; Koomson, E.; Lee, B.; Lee, S.; Leeth, A.; Manigault, D., III; Rajaee, M.; Sajjad, A.; Smith, M.; Yee, A. Women’s work, health and the environment in a small-scale mining site in northeastern Ghana. Women Environ. Int. Mag. 2011, 201, 13–16. [Google Scholar]
- Ghana Statistical Service (GSS); Ghana Health Service (GHS); ICF Macro. Ghana Demographic and Health Survey 2008; GSS, GHS, and ICF Macro: Accra, Ghana, 2009. [Google Scholar]
- Thomas, K.J. Child mortality and socioeconomic status: An examination of differentials by migration status in South Africa. Int. Migr. Rev. 2007, 41, 40–74. [Google Scholar] [CrossRef]
- Boadu, K. Social class and health status in Ghana. Curr. Sociol. 2002, 50, 531–553. [Google Scholar] [CrossRef]
- Fullerton, D.G.; Bruce, N.; Gordon, S.B. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Osumanu, I.K. Environmental concerns of poor households in low-income cities: The case of the Tamale Metropolis, Ghana. GeoJournal 2012, 68, 343–355. [Google Scholar] [CrossRef]
- Gobah, F.K.; Zhang, L. The national health insurance scheme in Ghana: Prospects and challenges: A cross-sectional evidence. Glob. J. Health Sci. 2011, 3, 90–102. [Google Scholar] [CrossRef]
- Colditz, G.A. Illnesses caused by smoking cigarettes. Cancer Causes Control 2000, 11, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Cheraghi, M.; Salvi, S. Environmental tobacco smoke (ETS) and respiratory health in children. Eur. J. Pediatr. 2009, 168, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Nyonator, F.K.; Awoonor-Williams, J.K.; Phillips, J.F.; Jones, T.C.; Miller, R. The Ghana community-based health planning and services initiative for scaling up service delivery innovation. Health Policy Plan. 2005, 20, 25–34. [Google Scholar] [CrossRef] [PubMed]
- United States Agency for International Development (USAID). U.S. Announces Community Grant Awards to Fight Malaria. Available online: http://www.usaid.gov/content/us-announces-community-grant-awards-fight-malaria (accessed on 20 December 2012).
- Victora, C.G.; Adair, L.; Fall, C.; Hallal, P.C.; Martorell, R.; Richter, L.; Sachdev, H.S. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- Abu-Saad, K.; Fraser, D. Maternal nutrition and birth outcomes. Epidemiol. Rev. 2010, 32, 5–25. [Google Scholar] [PubMed]
- Tielsch, J.M.; Sommer, A. The epidemiology of vitamin A deficiency and xerophthalmia. Annu. Rev. Nutr. 1984, 4, 183–205. [Google Scholar] [CrossRef]
- Hilson, G.M. Strengthening artisanal mining research and policy through baseline census activities. Nat. Resour. Forum 2005, 29, 144–153. [Google Scholar] [CrossRef]
- Hilson, G.M.; Maponga, O. How has a shortage of census and geological information impeded the regularization of artisanal and small-scale mining? Nat. Resour. Forum 2004, 28, 22–33. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Long, R.N.; Renne, E.P.; Basu, N. Understanding the Social Context of the ASGM Sector in Ghana: A Qualitative Description of the Demographic, Health, and Nutritional Characteristics of a Small-Scale Gold Mining Community in Ghana. Int. J. Environ. Res. Public Health 2015, 12, 12679-12696. https://doi.org/10.3390/ijerph121012679
Long RN, Renne EP, Basu N. Understanding the Social Context of the ASGM Sector in Ghana: A Qualitative Description of the Demographic, Health, and Nutritional Characteristics of a Small-Scale Gold Mining Community in Ghana. International Journal of Environmental Research and Public Health. 2015; 12(10):12679-12696. https://doi.org/10.3390/ijerph121012679
Chicago/Turabian StyleLong, Rachel N., Elisha P. Renne, and Niladri Basu. 2015. "Understanding the Social Context of the ASGM Sector in Ghana: A Qualitative Description of the Demographic, Health, and Nutritional Characteristics of a Small-Scale Gold Mining Community in Ghana" International Journal of Environmental Research and Public Health 12, no. 10: 12679-12696. https://doi.org/10.3390/ijerph121012679





