Cluster of Human Infections with Avian Influenza A (H7N9) Cases: A Temporal and Spatial Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Case Definition
2.2. Data Source
2.3. Geographic Information System (GIS) Method
2.4. SatScan Method
3. Results
3.1. Demographic Characteristics of Cases
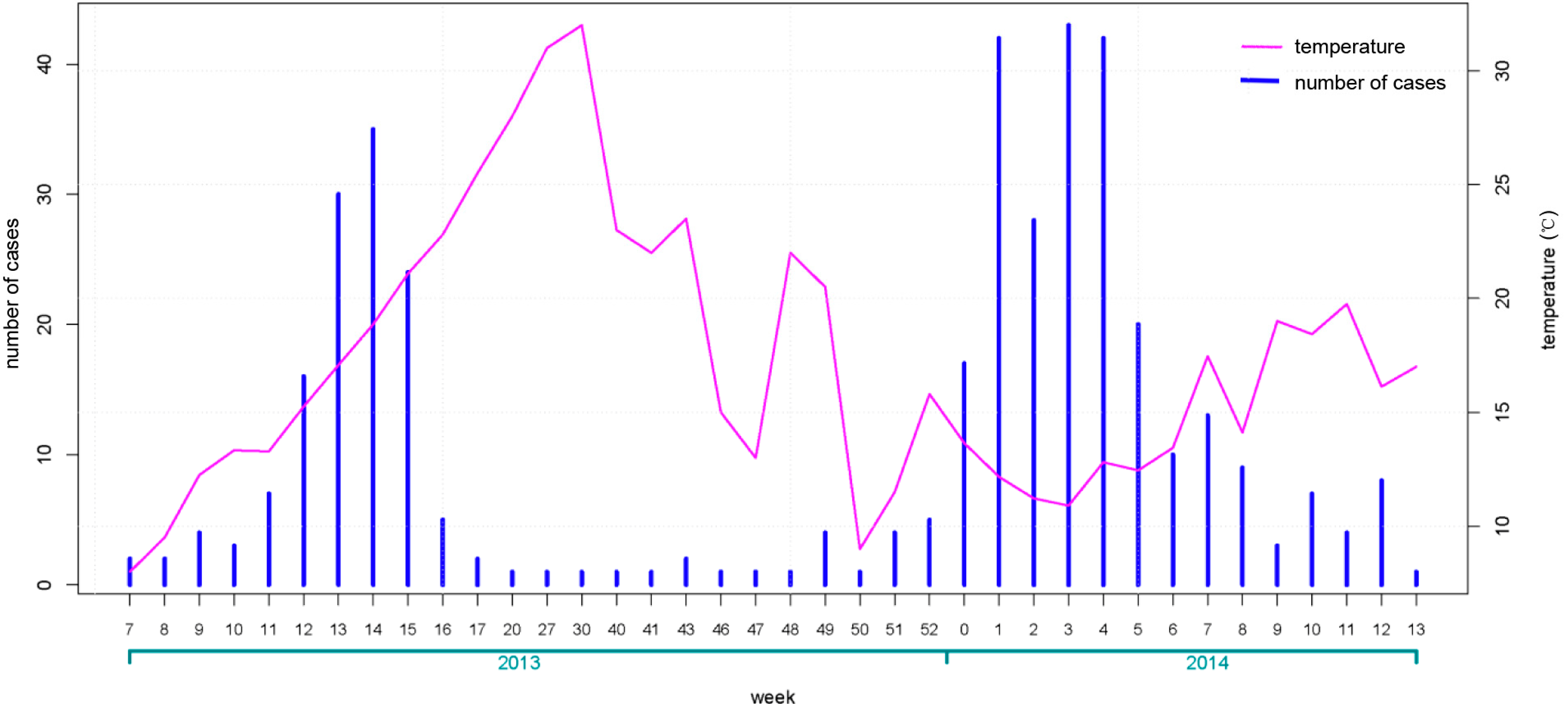
3.2. Temporal Characteristics of Cases
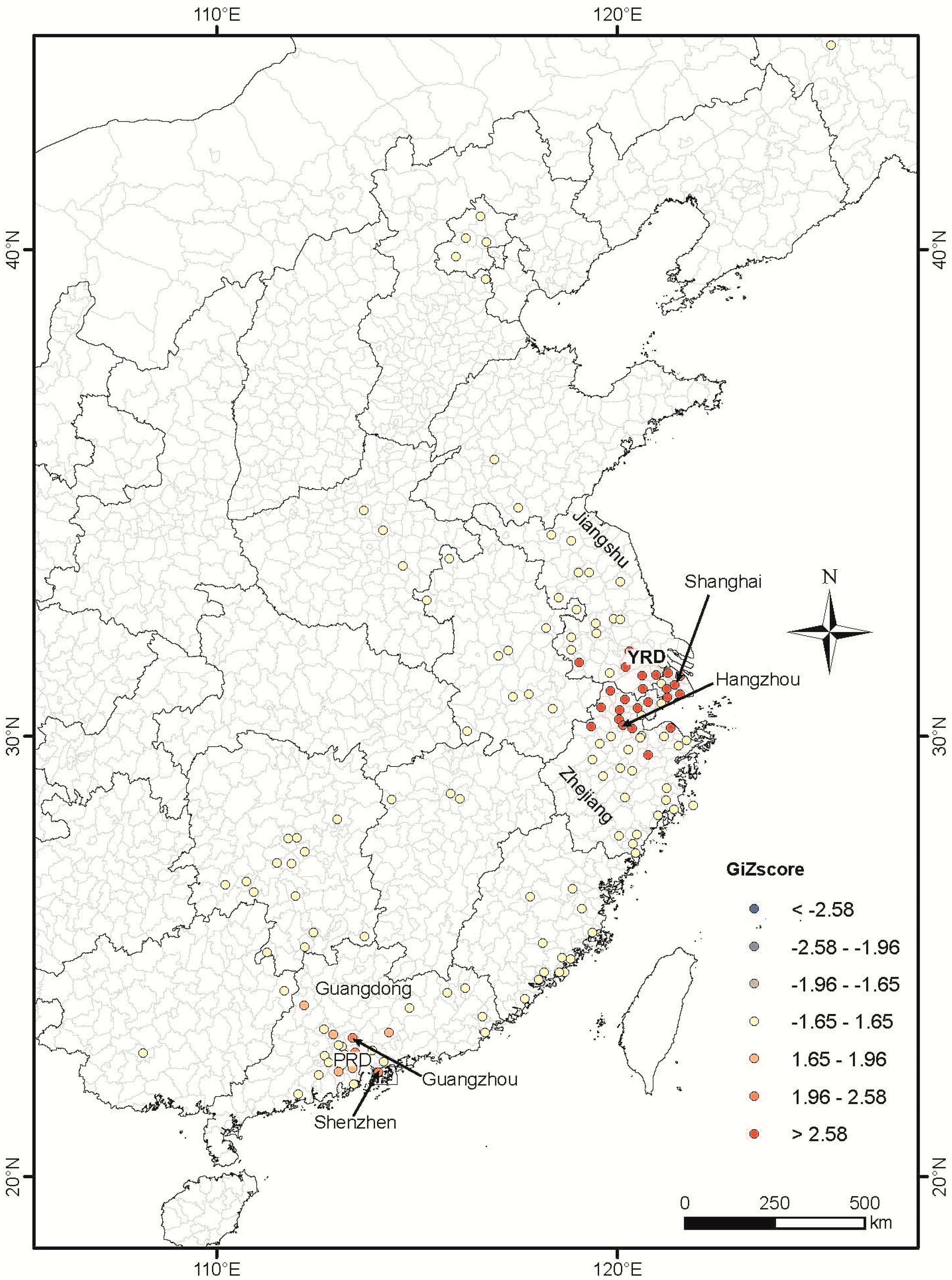
3.3. Spatial Characteristics of Cases

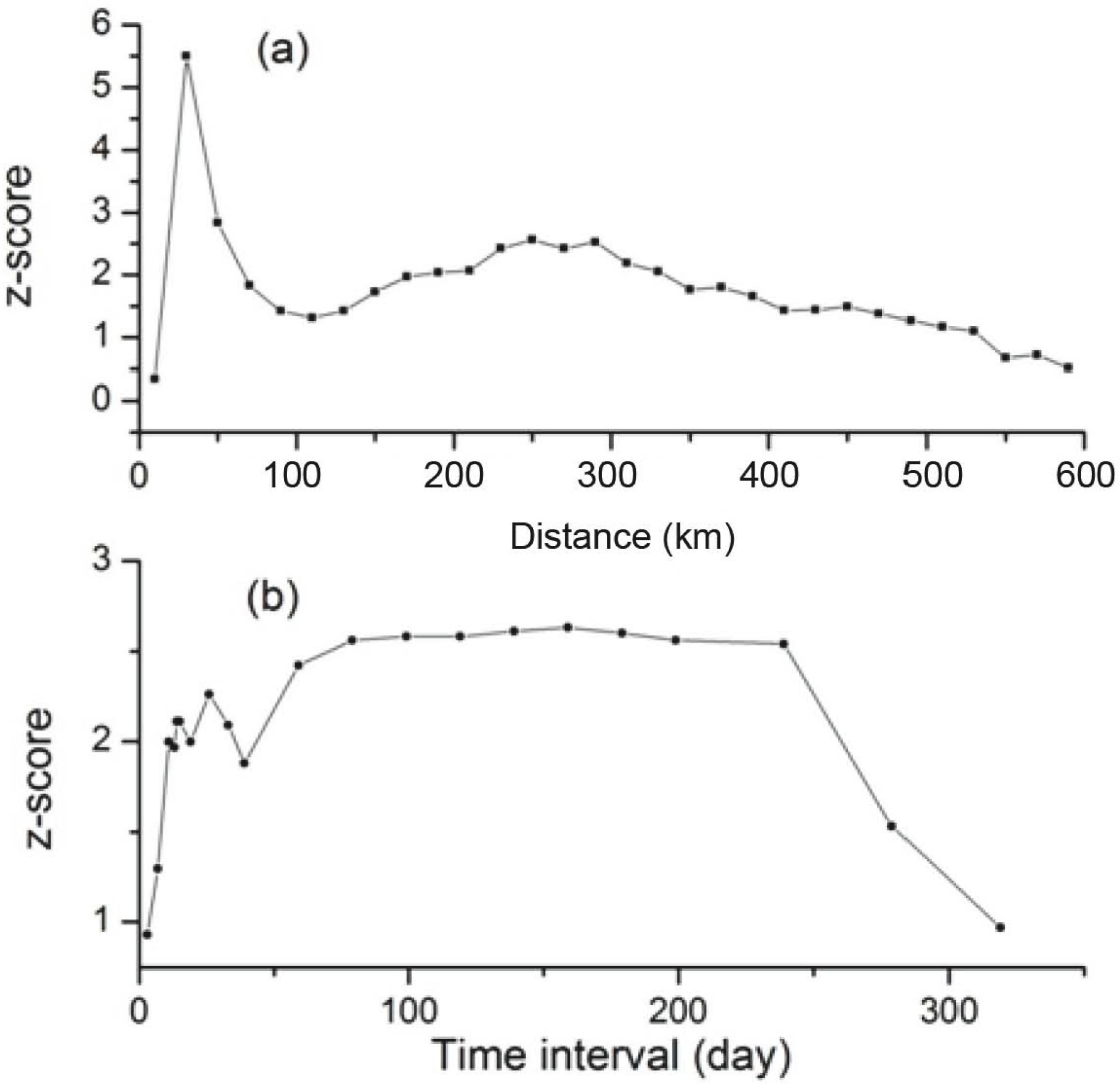
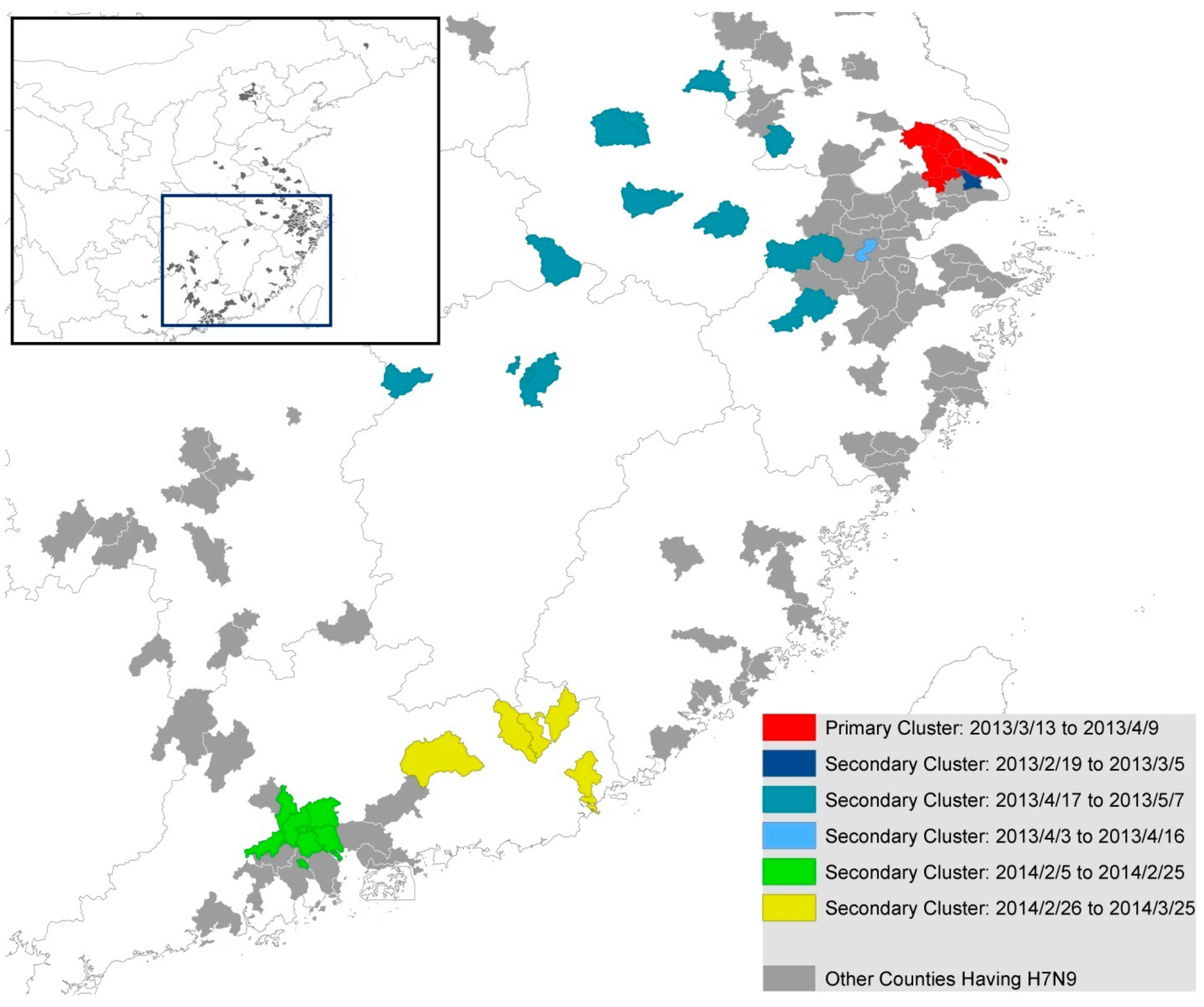
3.4. Spatial-Temporal Analysis
4. Discussion
4.1. The Spatial Distribution Characteristics of Human H7N9 Cases
4.2. The Temporal Distribution Characteristics of Human H7N9 Cases
4.3. The Spatial-Temporal Distribution Characteristics of Human H7N9 Cases
4.4. Study Limitations
5. Conclusions
Ethical Standard
Acknowledgments
Author Contributions
Conflicts of interest
References
- Yu, H.; Cowling, B.J.; Feng, L.; Lau, E.H.Y.; Liao, Q.; Tsang, T.K.; Peng, Z.; Wu, P.; Liu, F.; Fang, V.J.; et al. Human infection with avian influenza A H7N9 virus: An assessment of clinical severity. Lancet 2013, 382, 138–145. [Google Scholar] [CrossRef]
- WHO. Avian Influenza A(H7N9) Rivus. 2013. Available online: www.who.int/influenza/human_animal_interface/influenza_h7n9/10u_ReportWebH7N9Number.pdf (accessed on 1 June 2014).
- Liu, D.; Shi, W.; Shi, Y.; Wang, D.; Xiao, H.; Li, W.; Bi, Y.; Wu, Y.; Li, X.; Yan, J.; et al. Origin and diversity of novel avian influenza A H7N9 viruses causing human infection: Phylogenetic, structural, and coalescent analyses. Lancet 2013, 381, 1926–1932. [Google Scholar] [CrossRef]
- WHO. Background and Summary of Human Infection with Influenza A(H7N9) Virus—As of 5 April 2013. Available online: http://www.who.int/influenza/human_animal_interface/update_20130405/en/ (accessed on 1 June 2014).
- Tang, R.B.; Chen, H.L. An overview of the recent outbreaks of the avian-origin influenza A (H7N9) virus in the human. J. Chin. Med. Assoc. 2013, 76, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Qian, Y.H.; Bao, C.J.; Guo, X.L.; Cui, L.B.; Tang, F.Y.; Ji, H.; Huang, Y.; Cai, P.Q.; Lu, B.; et al. Probable person to person transmission of novel avian influenza A (H7N9) virus in Eastern China, 2013: Epidemiological investigation. BMJ 2013, 347. [Google Scholar] [CrossRef] [PubMed]
- Poovorawan, Y. Epidemic of avian influenza A (H7N9) virus in China. Pathog. Glob. Health. 2014, 108, 169–170. [Google Scholar] [CrossRef] [PubMed]
- Uyeki, T.M.; Cox, N.J. Global concerns regarding novel influenza A (H7N9) virus infections. N Engl. J. Med. 2013, 368, 1862–1864. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.; Wong, N.S. Reconstruction of epidemic curves for pandemic influenza A (H1N1) 2009 at city and sub-city levels. Virol. J. 2010, 7. [Google Scholar] [CrossRef] [PubMed]
- Lai, P.C.; Wong, C.M.; Hedley, A.J.; Hedley, A.J.; Lo, S.V.; Leung, P.Y.; Kong, J.; Leung, G.M. Understanding the spatial clustering of severe acute respiratory syndrome (SARS) in Hong Kong. Environ. Health Perspect. 2004, 112, 1550–1556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fournie, G.; Pfeiffer, D.U. Can closure of live poultry markets halt the spread of H7N9? Lancet 2014, 383, 496–497. [Google Scholar] [CrossRef] [PubMed]
- Lau, E.H.; Zheng, J.; Tsang, T.K.; Liao, Q.; Lewis, B.; Brownstein, J.S.; Sanders, S.; Wong, J.Y.; Mekaru, S.R.; Rivers, C.; et al. Accuracy of epidemiological inferences based on publicly available information: Retrospective comparative analysis of line lists of human cases infected with influenza A (H7N9) in China. BMC Med. 2014, 12. [Google Scholar] [CrossRef] [Green Version]
- Xiang, N.; Havers, F.; Chen, T.; Song, Y.; Tu, W.; Li, L.; Cao, Y.; Liu, B.; Zhou, L.; Meng, L.; et al. Use of national pneumonia surveillance to describe influenza A (H7N9) virus epidemiology, China, 2004–2013. Emerg. Infect. Dis. 2013, 19, 1784–1790. [Google Scholar] [PubMed]
- Han, J.; Jin, M.; Zhang, P.; Liu, J.; Wang, L.; Wen, D.; Wu, X.; Liu, G.; Zou, Y.; Lv, X.; et al. Epidemiological link between exposure to poultry and all influenza A (H7N9) confirmed cases in Huzhou city, China, March to May 2013. Euro Surveill. 2013, 18, 1–6. [Google Scholar] [PubMed]
- The National Health and Family Planning Commission of the People’s Republic of China. Diagnosis and Treatment Programs of Human Infections with H7N9 Virus. 2009. Available online: http://www.nhfpc.gov.cn/yzygj/s3593g/201306/5fc4b2d158d7475fa0da32e959f9a7ac.shtml (accessed on 12 October 2009). [Google Scholar]
- Ord, J.K.; Getis, A. Local spatial autocorrelation statistics: Distributional issues and an application. Geogr. Anal. 1995, 27, 286–306. [Google Scholar] [CrossRef]
- Kulldorff, M.; Heffernan, R.; Hartman, J.; Assuncao, R.; Mostashari, F. A space-time permutation scan statistic for disease outbreak detection. PLoS Med. 2005, 2. [Google Scholar] [CrossRef] [Green Version]
- Kulldorff, M.; Information Management Services, Inc. SaTScanTM v9.1: Software for the Spatial and Space-Time Scan Statistics. Available online: http://www.satscan.org/ (accessed on 1 June 2014).
- Liu, B.; Havers, F.; Chen, E.; Yuan, Z.; Yuan, H.; Ou, J.; Shang, M.; Kang, K.; Liao, K.; Liu, F.; et al. Risk Factors for Influenza A(H7N9) Disease—China, 2013. Clin. Infect. Dis. 2014, 59, 787–794. [Google Scholar] [CrossRef]
- Fang, L.Q.; Li, X.L.; Liu, K.; Li, Y.J.; Yao, H.W.; Liang, S.; Yang, Y.; Feng, Z.J.; Gray, G.C.; Cao, W.C. Mapping spread and risk of avian influenza A (H7N9) in China. Sci. Rep. 2013, 3. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.I.; Lu, C.L.; Tseng, W.C.; Li, H.A. A spatiotemporal statistical model of the risk factors of human cases of H5N1 avian influenza in South-east Asian countries and China. Public Health 2009, 123, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Martin, V.; Pfeiffer, D.U.; Zhou, X.; Xiao, X.; Prosser, D.J.; Guo, F.; Gilbert, M. Spatial distribution and risk factors of highly pathogenic avian influenza (HPAI) H5N1 in China. PLoS Pathog. 2011, 7. [Google Scholar] [CrossRef]
- Yu, W.; Du, P.; Chen, C.; Lu, S.; Kan, B.; Du, X.; Xu, J. Investigation of geographic relationship between farmer’s market with live birds and human infections with avian influenza A (H7N9) virus based on internet data analysis. Chin. J. Epidemiol. 2014, 35, 266–270. (In Chinese) [Google Scholar]
- Zhang, Y.; Feng, C.; Ma, C.; Yang, P.; Tang, S.; Lau, A.; Sun, W.; Wang, Q. The impact of temperature and humidity measures on influenza A (H7N9) outbreaks-evidence from China. Int. J. Infect. Dis. 2014, 30, 122–124. [Google Scholar] [CrossRef]
- Xu, J.; Lu, S.; Wang, H.; Chen, C. Reducing exposure to avian influenza H7N9. Lancet 2013, 381, 1815–1816. [Google Scholar] [CrossRef] [PubMed]
- Murhekar, M.; Arima, Y.; Horby, P.; Vandemaele, K.A.; Vong, S.; Zijian, F.; Lee, C.K.; Li, A.; World Health Organization Regional Office for the Western Pacific Event Management Team. Avian influenza A (H7N9) and the closure of live bird markets. Western Pac. Surveill. Response J. 2013, 4, 4–7. [Google Scholar]
- Kelland, K. Study Shows Poultry Market Closures Dramatically Cut Cases Of China Bird Flu, Reuters. 2013. Avaliable online: http://www.huffingtonpost.com/2013/10/31/poultry-market-closures-china-bird-flu_n_4180309.html (accessed on 23 Janurary 2014).
- Yu, H.; Wu, J.T.; Cowling, B.J.; Liao, Q.; Fang, V.J.; Zhou, S.; Wu, P.; Zhou, H.; Lau, E.H.; Guo, D. Effect of closure of live poultry markets on poultry-to-person transmission of avian influenza A H7N9 virus: An ecological study. Lancet 2014, 383, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Havers, F.; Wang, L.; Chen, T.; Shi, J.; Wang, D.; Yang, J.; Yang, L.; Widdowson, M.A.; Shu, Y. Monitoring avian influenza A (H7N9) virus through national influenza-like illness surveillance, China. Emerg. Infect. Dis. 2013, 19, 1289–1292. [Google Scholar] [PubMed]
- Xu, W.; Lu, L.; Shen, B.; Li, J.; Xu, J.; Jiang, S. Serological investigation of subclinical influenza A (H7H9) infection among healthcare and non-healthcare workers in Zhejiang Province, China. Clin. Infect. Dis. 2013, 57, 919–921. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Shen, Z.; Ma, C.; Jiang, C.; Feng, C.; Shankar, N.; Yang, P.; Sun, W.; Wang, Q. Cluster of Human Infections with Avian Influenza A (H7N9) Cases: A Temporal and Spatial Analysis. Int. J. Environ. Res. Public Health 2015, 12, 816-828. https://doi.org/10.3390/ijerph120100816
Zhang Y, Shen Z, Ma C, Jiang C, Feng C, Shankar N, Yang P, Sun W, Wang Q. Cluster of Human Infections with Avian Influenza A (H7N9) Cases: A Temporal and Spatial Analysis. International Journal of Environmental Research and Public Health. 2015; 12(1):816-828. https://doi.org/10.3390/ijerph120100816
Chicago/Turabian StyleZhang, Yi, Zhixiong Shen, Chunna Ma, Chengsheng Jiang, Cindy Feng, Nivedita Shankar, Peng Yang, Wenjie Sun, and Quanyi Wang. 2015. "Cluster of Human Infections with Avian Influenza A (H7N9) Cases: A Temporal and Spatial Analysis" International Journal of Environmental Research and Public Health 12, no. 1: 816-828. https://doi.org/10.3390/ijerph120100816




