Community Knowledge and Experience of Mosquitoes and Personal Prevention and Control Practices in Lhasa, Tibet
Abstract
:1. Introduction
2. Methods
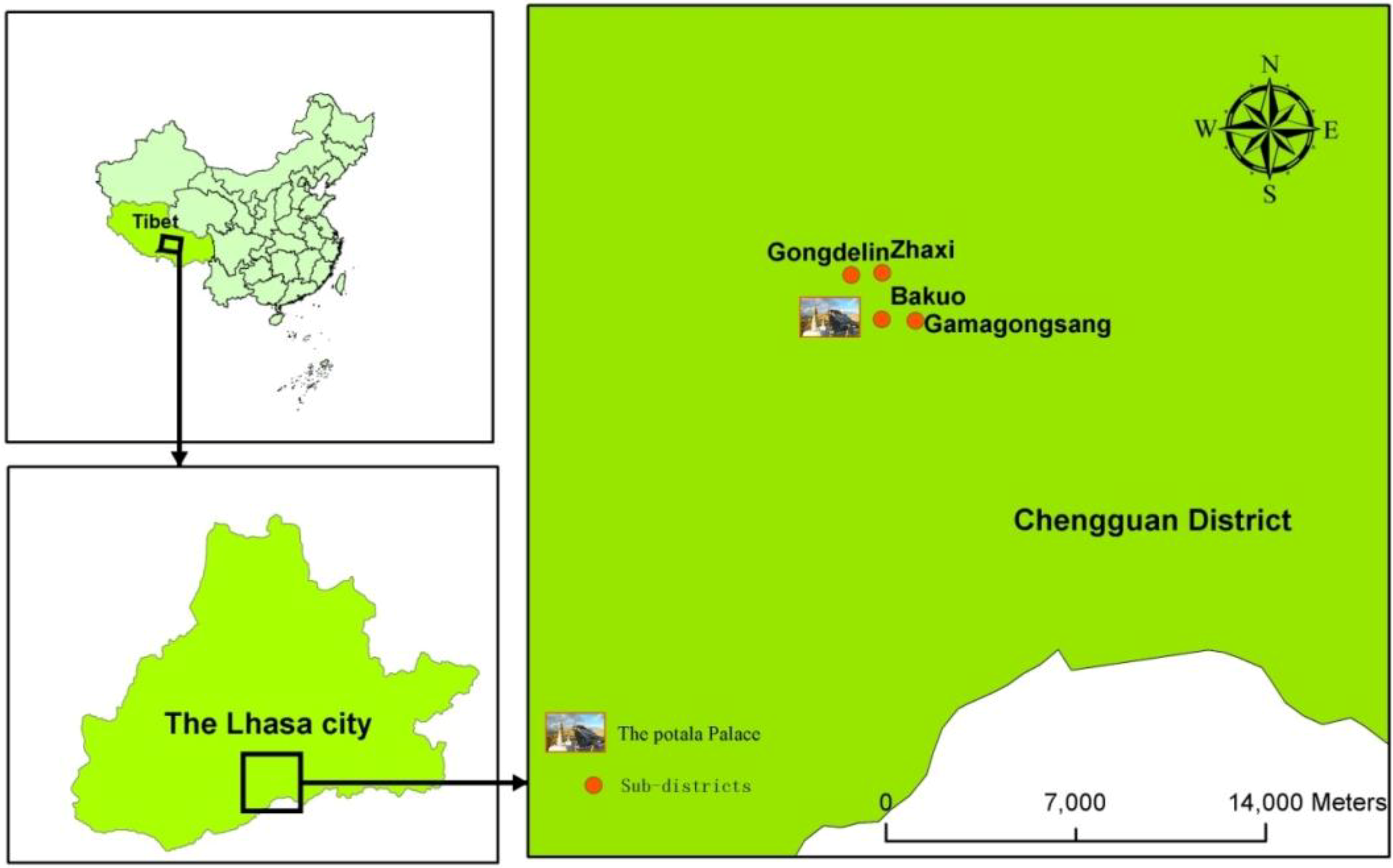
2.1. Study Area
2.2. Study Sample Size and Sampling Procedure
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Approval
3. Results and Discussion
3.1. Socio-Demographic Characteristics
| Variables | Category | Number of Interviewees | Proportion within Each Category (%) |
|---|---|---|---|
| Study sites | Gongdelin | 148 | 25.0 |
| Gamagongsang | 153 | 25.9 | |
| Zhaxi | 125 | 21.2 | |
| Bakuo | 165 | 27.9 | |
| Gender | Male | 226 | 38.2 |
| Female | 365 | 61.8 | |
| Ethnic group | Tibetan | 575 | 97.4 |
| Hui | 2 | 0.3 | |
| Han | 12 | 2.0 | |
| Others | 2 | 0.3 | |
| Register household | Native | 548 | 92.7 |
| Non-native | 43 | 7.3 | |
| Age (y) | 18~ | 90 | 15.3 |
| 30~ | 151 | 25.5 | |
| 42~ | 149 | 25.2 | |
| 54~ | 126 | 21.3 | |
| 65~ | 75 | 12.7 | |
| Education | Illiteracy | 138 | 23.4 |
| Literacy class | 7 | 1.2 | |
| Primary school | 206 | 34.9 | |
| Middle school | 90 | 15.2 | |
| High school | 100 | 16.8 | |
| Junior college and above | 50 | 8.5 | |
| Monthly income (RMB) | Less than 1000 | 266 | 45.0 |
| 1000~ | 167 | 28.3 | |
| 2000~ | 79 | 13.4 | |
| 3000~ | 35 | 5.9 | |
| 4000~ | 23 | 3.9 | |
| Higher than 5000 | 21 | 3.5 | |
| Occupation | Worker | 8 | 1.4 |
| Migrant laborer | 58 | 9.8 | |
| Peasant | 10 | 1.7 | |
| Student | 18 | 3.0 | |
| Cadre and office worker | 107 | 18.1 | |
| Chauffeur | 8 | 1.4 | |
| Teacher | 8 | 1.4 | |
| Medical personnel | 4 | 0.7 | |
| Retired employee | 72 | 12.2 | |
| Catering Service staff | 1 | 0.2 | |
| Self-Employed | 35 | 5.9 | |
| Homemaker | 23 | 3.9 | |
| Unemployed youth | 215 | 36.2 | |
| Unwilling to answer | 21 | 3.6 | |
| Other | 3 | 0.5 |
3.2. Assessment of Mosquito Knowledge
| Items * | Variables | Category | Frequency (%) |
|---|---|---|---|
| Knowledge | Have you heard of mosquitoes prior to this investigation? | Yes | 578 (97.8%) |
| No | 13 (2.2%) | ||
| Do you have access channels to acquire mosquito-related knowledge? | Yes | 427 (73.9%) | |
| No | 151 (26.1%) | ||
| Can mosquitoes be found in a variety of water bodies? | Yes | 234 (40.5%) | |
| No | 344 (59.5%) | ||
| Can mosquitoes suck human or animal blood? | Yes | 415 (71.8%) | |
| No | 163 (28.2%) | ||
| Can mosquitoes transmit some diseases? | Yes | 450 (77.9%) | |
| No | 128 (22.1%) | ||
| Can mosquitoes exert some impacts on people’s daily life? | Yes | 514 (88.9%) | |
| No | 64 (11.1%) | ||
| Experience | Have you ever seen mosquitoes in Lhasa? | Yes | 546 (94.5%) |
| No | 32 (5.5%) | ||
| Have you ever been bitten by mosquitoes in Lhasa? | Yes | 493 (85.3%) | |
| No | 85 (14.7%) | ||
| Practice | Is it necessary to control and prevent mosquitoes in summer? | Yes | 531 (91.9%) |
| No | 47 (8.1%) | ||
| Have you ever taken some mosquito control products and measures? | Yes | 446 (77.2%) | |
| No | 132 (22.8%) | ||
| Is it convenient to purchase mosquito repellent products? | Yes | 507 (87.7%) | |
| No | 71 (12.3%) | ||
| Can you give some suggestions to government and stakeholders concerning mosquito control in future? | Yes | 193 (33.4%) | |
| No | 385 (66.6%) |
3.3. Assessment of Experience with Mosquitoes
3.4. Assessment of Prevention and Control Practices of Mosquito
| Variable | N (578 ) | Overall Score (M ± D) | P | Knowledge Score (M ± D) | P | Experience Score (M ± D) | P | Practice Score (M ± D) | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| Study sites | Gongdelin | 147 | 9.068 (1.777) | 0.123 | 4.41 (0.985) | 0.356 | 1.73 (0.568) | 0.169 | 2.93 (0.951) | 0.802 |
| Gamagongsang | 149 | 9.322 (1.713) | 4.52 (1.011) | 1.87 (0.445) | 2.94 (0.932) | |||||
| Zhaxi | 121 | 9.388 (1.614) | 4.64 (1.080) | 1.78 (0.524) | 2.98 (0.790) | |||||
| Bakuo | 161 | 9.167 (1.754) | 4.57 (0.980) | 1.81 (0.503) | 2.79 (0.977) | |||||
| Gender | Male | 218 | 9.262 (1.635) | 0.474 | 4.48 (1.048) | 0.459 | 1.78 (0.505) | 0.040 | 3.00 (0.880) | 0.108 |
| Female | 360 | 9.208 (1.773) | 4.56 (0.988) | 1.81 (0.517) | 2.84 (0.944) | |||||
| Nationality | Tibetan | 562 | 9.228 (1.736) | 0.619 | 4.54 (1.011) | 0.578 | 1.80 (0.511) | 0.919 | 2.89 (0.930) | 0.758 |
| Hui | 2 | 9.500 (0.707) | 4.50 (0.707) | 2.00 (0.000) | 3.00 (0.000) | |||||
| Han | 12 | 9.250 (1.288) | 4.33 (1.155) | 1.75 (0.622) | 3.17 (0.577) | |||||
| others | 2 | 9.000 (0.000) | 4.00 (0.000) | 1.50 (0.707) | 3.50 (0.707) | |||||
| Household register | Native | 540 | 9.228 (1.722) | 0.002 | 4.52 (1.002) | 0.046 | 1.81 (0.490) | 0.731 | 2.89 (0.929) | 0.021 |
| Non-native | 38 | 9.237 (1.731) | 4.68 (1.141) | 1.55 (0.724) | 3.00 (0.838) | |||||
| Age group (y) | 18~ | 88 | 9.386 (1.441) | 0.148 | 4.60 (0.989) | 0.728 | 1.87 (0.424) | 0.113 | 2.91 (0.879) | 0.390 |
| 30~ | 147 | 9.456 (1.627) | 4.64 (0.986) | 1.84 (0.454) | 2.98 (0.910) | |||||
| 42~ | 147 | 9.150 (1.741) | 4.52 (0.995) | 1.80 (0.548) | 2.83 (0.894) | |||||
| 54~ | 122 | 9.254 (1.770) | 4.57 (0.996) | 1.79 (0.502) | 2.90 (0.991) | |||||
| 65~ | 74 | 8.702 (1.991) | 4.18 (1.090) | 1.65 (0.629) | 2.88 (0.950) | |||||
| Education | Illiteracy | 130 | 9.085 (2.004) | 0.343 | 4.47 (1.136) | 0.940 | 1.78 (0.517) | 0.429 | 2.84 (0.963) | 0.512 |
| Literacy class | 7 | 9.143 (1.773) | 4.71 (1.113) | 1.86 (0.378) | 2.57 (0.787) | |||||
| Primary school | 203 | 9.123 (1.752) | 4.51 (0.982) | 1.77 (0.563) | 2.84 (0.977) | |||||
| Middle school | 89 | 9.202 (1.740) | 4.48 (1.035) | 1.80 (0.526) | 2.92 (0.956) | |||||
| High school | 99 | 9.586 (1.385) | 4.70 (0.974) | 1.84 (0.445) | 3.05 (0.761) | |||||
| Junior college and above | 50 | 9.380 (1.276) | 4.48 (0.789) | 1.88 (0.385) | 3.02 (0.820) | |||||
| Monthly income (RMB) | Less than 1000 | 260 | 9.135(1.875) | 0.083 | 4.51 (1.067) | 0.250 | 1.78 (0.541) | 0.009 | 2.84 (0.956) | 0.287 |
| 1000~ | 164 | 9.433 (1.551) | 4.68 (0.884) | 1.82 (0.495) | 2.93 (0.897) | |||||
| 2000~ | 79 | 9.215 (1.550) | 4.42 (1.057) | 1.85 (0.455) | 2.95 (0.830) | |||||
| 3000~ | 34 | 9.235 (1.372) | 4.29 (0.760) | 1.85 (1.359) | 3.09 (0.965) | |||||
| 4000~ | 22 | 8.546 (2.110) | 4.18 (1.296) | 1.50 (0.598) | 2.86 (1.125) | |||||
| High than 5000 | 19 | 9.579 (1.539) | 4.79 (0.918) | 1.79 (0.535) | 3.00 (0.745) | |||||
| Occupation | Labour | 8 | 9.500 (1.309) | 0.204 | 4.50 (1.195) | 0.383 | 1.75 (0.463) | 0.924 | 3.25 (0.463) | 0.217 |
| Migrant labourer | 57 | 9.263 (1.541) | 4.35 (1.009) | 1.82 (0.504) | 3.09 (0.892) | |||||
| Peasant | 10 | 8.700 (1.703) | 4.00 (1.333) | 2.00 (0.000) | 2.70 (1.160) | |||||
| Student | 18 | 9.611 (1.754) | 4.56 (1.338) | 1.89 (0.471) | 3.17 (0.786) | |||||
| Cadre and office | 106 | 9.528 (1.148) | 4.63 (0.797) | 1.86 (0.424) | 3.04 (0.780) | |||||
| Chauffeur | 7 | 9.143 (1.952) | 4.29 (1.113) | 2.00 (0.000) | 2.86 (0.900) | |||||
| Teacher | 8 | 9.875 (0.834) | 4.25 (0.463) | 2.00 (0.000) | 3.63 (0.518) | |||||
| Medical personnel | 4 | 10.250 (1.258) | 5.00 (0.816) | 1.75 (0.500) | 3.50 (0.577) | |||||
| Retired employee | 70 | 9.457 (1.390) | 4.61 (0.873) | 1.77 (0.456) | 3.07 (0.804) | |||||
| Catering | 1 | 8.000 (-) | 5.00 (-) | 0.00 (-) | 3.00 (-) | |||||
| Self-employed | 33 | 8.879 (2.497) | 4.45 (1.371) | 1.67 (0.645) | 2.76 (0.969) | |||||
| Homemaker | 21 | 9.048 (2.179) | 4.48 (1.030) | 1.67 (0.658) | 2.90 (0.995) | |||||
| Unemployed youth | 213 | 9.066 (1.922) | 4.55 (1.052) | 1.78 (0.552) | 2.73 (0.995) | |||||
| Unwilling to answer | 20 | 8.800 (1.735) | 4.50 (1.051) | 1.80 (0.523) | 2.50 (1.000) | |||||
| Others | 2 | 8.000 (1.414) | 4.00 (0.000) | 2.00 (0.000) | 2.00 (1.414) | |||||
| Total | 578 | 9.228 (1.721) | 4.53 (1.011) | 1.80 (0.512) | 2.90 (0.923) |
3.5. Assessment of Overall Score Concerning Mosquito
3.6. Correlation among Knowledge, Experience, Prevention and Control Practice towards Mosquitoes
| Variable | Correlation Coefficient | P-Value * |
|---|---|---|
| Knowledge & Experience | r = 0.157 | P < 0.01 |
| Experience & Practice | r = 0.221 | P < 0.01 |
| Knowledge & Practice | r = 0.266 | P < 0.01 |
4. Discussion
5. Conclusions
Acknowledgments
Abbreviations
| TAR | the Tibet Autonomous Region |
| KAP | Knowledge, Attitude, and Practice |
| KEP | Knowledge, Experience, and Practice |
Author Contributions
Conflicts of Interest
References
- Dowling, Z.; Armbruster, P.; LaDeau, S.L.; DeCotiis, M.; Mottley, J.; Leisnham, P.T. Linking mosquito infestation to resident socioeconomic status, knowledge, and source reduction practices in suburban Washington, DC. EcoHealth 2013, 10, 36–47. [Google Scholar] [PubMed]
- Epstein, P.R. West Nile virus and the climate. J. Urban Health: Bull. New York Acad. Med. 2001, 78, 367–371. [Google Scholar]
- Epstein, P.R. Chikungunya Fever resurgence and global warming. Am. J. Trop. Med. Hyg. 2007, 76, 403–404. [Google Scholar] [PubMed]
- Rochlin, I.; Ninivaggi, D.V.; Hutchinson, M.L.; Farajollahi, A. Climate change and range expansion of the Asian tiger mosquito (Aedes albopictus) in Northeastern USA: Implications for public health practitioners. PloS one 2013, 8. [Google Scholar] [CrossRef]
- Epstein, P.R.; Diaz, H.F.; Elias, S.; Grabherr, G.; Graham, N.E.; Martens, W.J.M.; Mosley-Thompson, E.; Susskind, J. Biological and physical signs of climate change: Focus on mosquito-borne diseases. Bull. Amer. Meteor. Soc. 1998, 79, 409–417. [Google Scholar]
- Bai, L.; Morton, L.C.; Liu, Q. Climate change and mosquito-borne diseases in China: A review. Glob. Health 2013, 9. [Google Scholar] [CrossRef]
- Liu, Q.; Liu, X.; Cirendunzhu; Woodward, A.; Pengcuociren; Bai, L.; Baimaciwang; Sang, S.; Dazhen; Wan, F.; et al. Mosquitoes established in Lhasa city, Tibet, China. Parasites Vectors 2013, 6. [Google Scholar] [CrossRef] [PubMed]
- Weitzel, T.; Collado, A.; Jost, A.; Pietsch, K.; Storch, V.; Becker, N. Genetic differentiation of populations within the Culex pipiens complex and phylogeny of related species. J. Am. Mosq. Control. Assoc. 2009, 25, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, D.M.; Keyghobadi, N.; Malcolm, C.A.; Mehmet, C.; Schaffner, F.; Mogi, M.; Fleischer, R.C.; Wilkerson, R.C. Emerging vectors in the Culex pipiens complex. Science 2004, 303, 1535–1538. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Badillo, A.; Bolling, B.G.; Perez-Ramirez, G.; Moore, C.G.; Martinez-Munoz, J.P.; Padilla-Viveros, A.A.; Camacho-Nuez, M.; Diaz-Perez, A.; Beaty, B.J.; Munoz Mde, L. The distribution of potential West Nile virus vectors, Culex pipiens pipiens and Culex pipiens quinquefasciatus (Diptera: Culicidae), in Mexico City. Parasites Vectors 2011, 4. [Google Scholar] [CrossRef] [PubMed]
- Amraoui, F.; Krida, G.; Bouattour, A.; Rhim, A.; Daaboub, J.; Harrat, Z.; Boubidi, S.C.; Tijane, M.; Sarih, M.; Failloux, A.B. Culex pipiens, an experimental efficient vector of West Nile and Rift Valley fever viruses in the Maghreb region. PloS ONE 2012, 7. [Google Scholar] [CrossRef]
- Hamer, G.L.; Kitron, U.D.; Brawn, J.D.; Loss, S.R.; Ruiz, M.O.; Goldberg, T.L.; Walker, E.D. Culex pipiens (Diptera: Culicidae): A bridge vector of West Nile virus to humans. J. Med. Entomol. 2008, 45, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Farajollahi, A.; Fonseca, D.M.; Kramer, L.D.; Marm Kilpatrick, A. “Bird biting” mosquitoes and human disease: A review of the role of Culex pipiens complex mosquitoes in epidemiology. Infect. Genet. Evol. 2011, 11, 1577–1585. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.L.; Fonseca, D.M. Rapid assays for identification of members of the Culex (Culex) pipiens complex, their hybrids, and other sibling species (Diptera: culicidae). Am. J. Trop. Med. Hyg. 2004, 70, 339–345. [Google Scholar] [PubMed]
- Solomon, T. Flavivirus encephalitis. New Engl. J. Med. 2004, 351, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Cui, F.; Tan, Y.; Qiao, C.L. Filariasis vector in China: insecticide resistance and population structure of mosquito Culex pipiens complex. Pest. Manag. Sci. 2007, 63, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.L.; Eldridge, B.F.; Hayes, D.E.; Watts, D.M.; Tammariello, R.F.; Dalrymple, J.M. Isolation of St. Louis encephalitis virus from overwintering Culex pipiens mosquitoes. 1978, 199, 1346–1349. [Google Scholar]
- Turell, M.J. Members of the Culex pipiens complex as vectors of viruses. J. Am. Mosq. Control. Assoc. 2012, 28, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Benitez, M.A. Climate change could affect mosquito-borne diseases in Asia. Lancet 2009, 373. [Google Scholar] [CrossRef] [PubMed]
- Tuiten, W.; Koenraadt, C.J.; McComas, K.; Harrington, L.C. The effect of West Nile virus perceptions and knowledge on protective behavior and mosquito breeding in residential yards in upstate New York. EcoHealth 2009, 6, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Ul Haq, N.; Hassali, M.A.; Shafie, A.A.; Saleem, F.; Farooqui, M.; Aljadhey, H. A cross sectional assessment of knowledge, attitude and practice towards Hepatitis B among healthy population of Quetta, Pakistan. BMC Public Health 2012, 12. [Google Scholar] [CrossRef]
- Zhang, L.L.; Dalal, K.; Yin, M.M.; Yuan, D.G.; Andrews, J.Y.; Wang, S.M. The KAP evaluation of intervention on fall-induced injuries among elders in a safe community in Shanghai, China. PloS ONE 2012, 7. [Google Scholar] [CrossRef]
- Raychaudhuri, S.; Mandal, S. Current Status of Knowledge, Attitude and Practice (KAP) and screening for cervical cancer in countries at different levels of development. Asian Pac. J. Cancer Prev.: APJCP 2012, 13, 4221–4227. [Google Scholar]
- Passey, M.E.; D’Este, C.A.; Sanson-Fisher, R.W. Knowledge, attitudes and other factors associated with assessment of tobacco smoking among pregnant Aboriginal women by health care providers: A cross-sectional survey. BMC Public Health 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Kharkar, M.; Bowalekar, S. Knowledge, attitude and perception/practices (KAP) of medical practitioners in India towards adverse drug reaction (ADR) reporting. Perspect. Clin. Res. 2012, 3, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Bashar, K.; Al-Amin, H.M.; Reza, M.S.; Islam, M.M.; Asaduzzaman; Ahmed, T.U. Socio-demographic factors influencing knowledge, attitude and practice (KAP) regarding malaria in Bangladesh. BMC Public Health 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Worku, H.; Teklu, S. Knowledge, attitudes and practices (KAP) regarding emergency contraception among drug dispensers working in retail outlets of Addis Ababa. Ethiop. Med. J. 2011, 49, 7–15. [Google Scholar] [PubMed]
- Tran, N.T.; Taylor, R.; Choe, S.I.; Pyo, H.S.; Kim, O.S.; So, H.C. Knowledge, attitude and practice (KAP) concerning cervical cancer and screening among rural and urban female healthcare practitioners in the Democratic People’s Republic of Korea. Asian Pac. J. Cancer Prev. 2011, 12, 3023–3028. [Google Scholar] [PubMed]
- Ndetei, D.M.; Khasakhala, L.I.; Mutiso, V.; Mbwayo, A.W. Knowledge, attitude and practice (KAP) of mental illness among staff in general medical facilities in Kenya: Practice and policy implications. Afr. J. Psychiatry 2011, 14, 225–235. [Google Scholar] [CrossRef]
- Hussain, M.F.; Khanani, M.R.; Siddiqui, S.E.; Manzar, N.; Raza, S.; Qamar, S. Knowledge, attitudes & practices (KAP) of general practitioners (GPS) regarding sexually transmitted diseases (STDS) and HIV/AIDS in Karachi, Pakistan. J. Pak. Med. Assoc. 2011, 61, 202–205. [Google Scholar] [PubMed]
- Yang, H.J.; Tsao, W.Y.; Lay, Y.L.; Chen, M.; Liou, Y.C. Prior language experience and language anxiety as predictors for non-native language commercial website use intention. Int. J. Human-Computer Stud. 2008, 66, 678–687. [Google Scholar]
- Yoder, P.S. Negotiating relevance: Belief, knowledge, and practice in international health projects. Med. Anthropol. Q. 1997, 11, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Kaul, S.M.; Verma, A.K.; Jain, D.C.; Gupta, R.S.; Dutta, A. Community perception of mosquitos and mosquito control in some areas of urban Delhi and rural Alwar, Rajasthan. J. Commun. Dis. 1995, 27, 215–222. [Google Scholar] [PubMed]
- Hlongwana, K.W.; Mabaso, M.L.; Kunene, S.; Govender, D.; Maharaj, R. Community knowledge, attitudes and practices (KAP) on malaria in Swaziland: A country earmarked for malaria elimination. Malar. J. 2009, 8. [Google Scholar] [CrossRef] [PubMed]
- Hairi, F.; Ong, C.H.; Suhaimi, A.; Tsung, T.W.; bin Anis Ahmad, M.A.; Sundaraj, C.; Soe, M.M. A knowledge, attitude and practices (KAP) study on dengue among selected rural communities in the Kuala Kangsar district. Asia-Pac. J. Public Health/Asia-Pac. Acad. Consort. Public Health 2003, 15, 37–43. [Google Scholar]
- Wilder-Smith, A.; Khairullah, N.S.; Song, J.H.; Chen, C.Y.; Torresi, J. Travel health knowledge, attitudes and practices among Australasian travelers. J. Travel Med. 2004, 11, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Bai, L.; Cirendunzhu; Pengcuociren; Dawa; Woodward, A.; Liu, X.; Baimaciwang; Dazhen; Sang, S.; Wan, F.; et al. Rapid warming in Tibet, China: Public perception, response and coping resources in urban Lhasa. Environ. Health 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Xiang, N.; Shi, Y.; Wu, J.; Zhang, S.; Ye, M.; Peng, Z.; Zhou, L.; Zhou, H.; Liao, Q.; Huai, Y.; et al. Knowledge, attitudes and practices (KAP) relating to avian influenza in urban and rural areas of China. BMC Infect. Dis. 2010, 10. [Google Scholar] [CrossRef] [PubMed]
- Panagakou, S.G.; Theodoridou, M.N.; Papaevangelou, V.; Papastergiou, P.; Syrogiannopoulos, G.A.; Goutziana, G.P.; Hadjichristodoulou, C.S. Development and assessment of a questionnaire for a descriptive cross-sectional study concerning parents’ knowledge, attitudes and practises in antibiotic use in Greece. BMC Infect. Dis. 2009, 9. [Google Scholar] [CrossRef] [PubMed]
- Anand, D.; Puri, S. Nutritional knowledge, attitude, and practices among HIV-positive individuals in India. J. Health Popul. Nutr. 2013, 31, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Koenraadt, C.J.; Tuiten, W.; Sithiprasasna, R.; Kijchalao, U.; Jones, J.W.; Scott, T.W. Dengue knowledge and practices and their impact on Aedes aegypti populations in Kamphaeng Phet, Thailand. Am. J. Trop. Med. Hyg. 2006, 74, 692–700. [Google Scholar] [PubMed]
- Liu, Q.; Liu, X.; Cirendunzhu, C.; Woodward, A.; Pengcuociren, P.; Bai, L.; Baimaciwang, B.; Sang, S.; Dazhen, D.; Wan, F.; et al. Mosquitoes established in Lhasa city, Tibet, China. Parasites Vectors 2013, 6. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Fuentes, S.; Hayden, M.H.; Welsh-Rodriguez, C.; Ochoa-Martinez, C.; Tapia-Santos, B.; Kobylinski, K.C.; Uejio, C.K.; Zielinski-Gutierrez, E.; Monache, L.D.; Monaghan, A.J.; Steinhoff, D.F.; Eisen, L. The dengue virus mosquito vector Aedes aegypti at high elevation in Mexico. Am. J. Trop. Med. Hyg. 2012, 87, 902–909. [Google Scholar] [CrossRef] [PubMed]
- Eisen, L.; Bolling, B.G.; Blair, C.D.; Beaty, B.J.; Moore, C.G. Mosquito species richness, composition, and abundance along habitat-climate-elevation gradients in the northern Colorado Front Range. J. Med. Entomol. 2008, 45, 800–811. [Google Scholar] [CrossRef] [PubMed]
- Henrickson, S.E.; Wong, T.; Allen, P.; Ford, T.; Epstein, P.R. Marine swimming-related illness: Implications for monitoring and environmental policy. Environ. Health Perspect. 2001, 109, 645–650. [Google Scholar] [CrossRef] [PubMed]
- Imbahale, S.S.; Fillinger, U.; Githeko, A.; Mukabana, W.R.; Takken, W. An exploratory survey of malaria prevalence and people’s knowledge, attitudes and practices of mosquito larval source management for malaria control in western Kenya. Acta. Tropica 2010, 115, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Purohit, B.M.; Bhambal, A.; Saxena, S.; Singh, A.; Gupta, A. Knowledge, attitudes and practice regarding infection control measures among dental students in Central India. Int. J. Infect. Control. 2011, 75, 421–427. [Google Scholar]
- Reiter, P. Climate change and mosquito-borne disease. Environ. Health Perspect. 2001, 109, 141–161. [Google Scholar] [CrossRef] [PubMed]
- Zell, R. Global climate change and the emergence/re-emergence of infectious diseases. Int. J. Med. Microbiol. 2004, 293, 16–26. [Google Scholar] [PubMed]
- Patz, J.A.; Epstein, P.R.; Burke, T.A.; Balbus, J.M. Global climate change and emerging infectious diseases. J. Am. Med. Assoc. 1996, 275, 217–223. [Google Scholar] [CrossRef]
- Rydzanicz, K.; Kiewra, D.; Lonc, E. Changes in range of mosquito-borne diseases affected by global climatic fluctuations Wiadomosci. Parazytologiczne 2006, 52, 73–83. [Google Scholar]
- Stachowicz, J.J.; Terwin, J.R.; Whitlatch, R.B.; Osman, R.W. Linking climate change and biological invasions: Ocean warming facilitates nonindigenous species invasions. Proc. Natl. Acad. Sci. USA 2002, 99, 15497–15500. [Google Scholar] [CrossRef] [PubMed]
- McBeath, J.H.; McBeath, J. Invasive Species and Food Security. In Environmental Change and Food Security in China; Springer Netherlands: Berlin, Heidelberg, Germany, 2010. [Google Scholar]
- Liu, X.; Chen, B. Climatic warming in the Tibetan Plateau during recent decades. Int. J. Climatol. 2000, 20, 1729–1742. [Google Scholar] [CrossRef]
- Kerr, R.A. Global warming is changing the world. Science 2007, 316, 188–190. [Google Scholar] [CrossRef] [PubMed]
- Jun, D. Change of temperature in Tibetan Plateau From 1961 to 2000 (In Chinese). Acta Geographica Sinica 2001, 56, 682–690. [Google Scholar]
- Huang, X. Climatic change of maximum and minimum temperature in Lasa (In Chinese). Meteorol. Mon. 2000, 26, 47–50. [Google Scholar]
- Loevinsohn, M.E. Climatic warming and increased malaria incidence in Rwanda. Lancet 1994, 343, 714–718. [Google Scholar] [CrossRef] [PubMed]
- Reiter, P. Global warming and mosquito-borne disease in USA. Lancet 1996, 348, 622–840. [Google Scholar] [CrossRef] [PubMed]
- Patz, J.A.; Campbell-Lendrum, D.; Holloway, T.; Foley, J.A. Impact of regional climate change on human health. Nature 2005, 438, 310–317. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Liu, X.; Wan, F.; Cirendunzhu; Cirenwangla; Bai, L.; Pengcuociren; Zhou, L.; Baimaciwang; Guo, Y.; Dazhen; et al. Community Knowledge and Experience of Mosquitoes and Personal Prevention and Control Practices in Lhasa, Tibet. Int. J. Environ. Res. Public Health 2014, 11, 9919-9937. https://doi.org/10.3390/ijerph110909919
Liu X, Wan F, Cirendunzhu, Cirenwangla, Bai L, Pengcuociren, Zhou L, Baimaciwang, Guo Y, Dazhen, et al. Community Knowledge and Experience of Mosquitoes and Personal Prevention and Control Practices in Lhasa, Tibet. International Journal of Environmental Research and Public Health. 2014; 11(9):9919-9937. https://doi.org/10.3390/ijerph110909919
Chicago/Turabian StyleLiu, Xiaobo, Fangjun Wan, Cirendunzhu, Cirenwangla, Li Bai, Pengcuociren, Lin Zhou, Baimaciwang, Yuhong Guo, Dazhen, and et al. 2014. "Community Knowledge and Experience of Mosquitoes and Personal Prevention and Control Practices in Lhasa, Tibet" International Journal of Environmental Research and Public Health 11, no. 9: 9919-9937. https://doi.org/10.3390/ijerph110909919





