A Health Impact Assessment Framework for Assessing Vulnerability and Adaptation Planning for Climate Change
Abstract
:1. Introduction
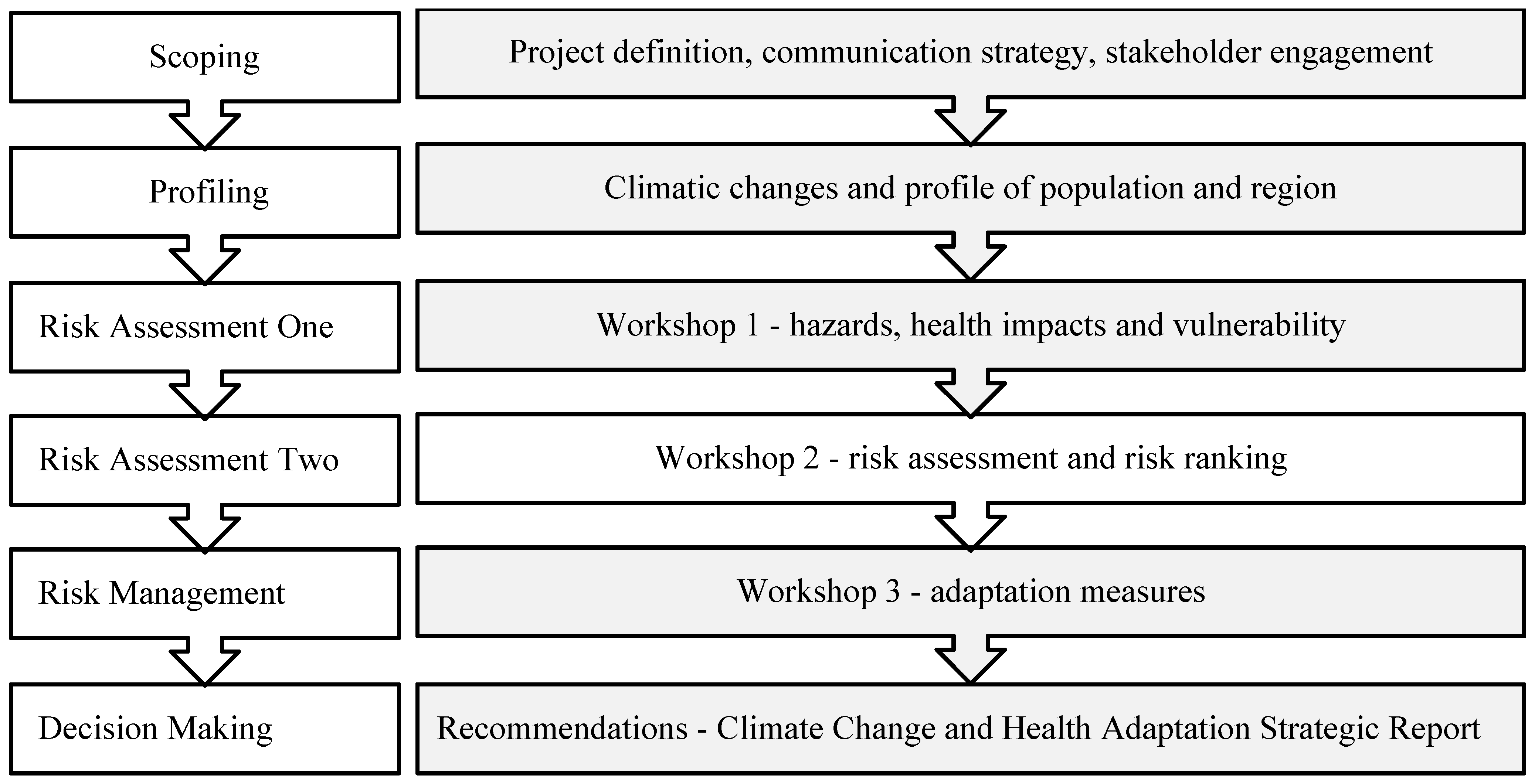
2. The Process
2.1. Step 1—Scoping
- the establishment of the Project Team and Terms of Reference
- development of a communication strategy
- development of a stakeholder engagement strategy
- a shared understanding of the definition of health and of climate-related health impacts
- spatial and temporal boundaries of the HIA
- roles and responsibilities of members
- decision making processes within the Team including agreement on methodologies for the project
- resource requirements (e.g., funding, time, budgets, staff)
- time lines for activities
- final output (e.g., recommendations for decision makers)
Direct Effects of Extreme Climate Events
| |
| Indirect Effects of Climate Change | |
Environmental factors
| Ecological factors
|
Socio-economic factors
| Psychosocial factors
|
Lifestyle factors
| Technological factors
|
Services
| Insert other factors as required
|
2.1.1. Vulnerability
2.1.2. Communications and Stakeholder Engagement Strategies
- Who should take responsibility for consultation?
- Who are the key stakeholder groups at the national, regional and local level?
- How are the needs of and consultation with vulnerable groups to be addressed?
- Can representation for the needs of particular groups be obtained and is this useful?
- What should the outcomes of the consultation be used for?
- Are there different timeframes required for consultation, communication and dissemination of information?
2.2. Step 2—Profiling of Climate, Region and Population
- Gradual changes—temperature, rainfall and sea level
- Extreme climatic events—Heat waves, cold snaps, tropical cyclones, storm surges, floods, droughts and bushfires
2.3. Step 3—Risk Assessment One
Step 3—Workshop 1
Hazard Identification
- Biophysical—air, water, food. Includes environmental-related illness related to air, water and food quality and vector-borne diseases
- Social—economy, lifestyle, housing, workforce, population displacement, psychosocial factors and community services
- Infrastructure –energy, transport, built environment, telecommunications, water, waste
| Climatic Variable | Biophysical Category |
|---|---|
| Insert List of Relevant Health-Related Hazards | |
| Temperature (Sheet 1) | Ground-level ozone likely to increase with higher summer temperatures |
| Rainfall (Sheet 2) | Reductions in rainfall—reduced water quality, water stress. |
| Sea-level (Sheet 3) | Mosquito breeding sites may be affected |
| Extreme Events (Sheet 4) | Heatwaves—direct heat-related effects, air quality Bushfire—air quality, potential contamination of water supplies, impact on food production |
Health Impacts and Vulnerability Assessment
| Climate Variable | Health Hazards & Impacts | Vulnerability (Exposure, Sensitivity, Adaptive Capacity) | Evidence/ Uncertainty | ||||
|---|---|---|---|---|---|---|---|
| Gradual Changes | Hazards (Tansfer from working table 3) | Health Impacts Direct & indirect | Regional | Economic | Social | Infrastructure | |
| Temperature increase | Ground-level ozone likely to increase | Respiratory and cardio-vascular effects, including increase in mortality, hospitalisations and doctor visits. | Exposure likely to be higher in urban areas | - | Exposure tends to be higher outdoors → lifestyle and occupational factors may increase exposure. | Flow-on effects to health sector. May be heightened during heatwaves. | Link between ozone levels and temperature, and health effects of ozone exposure are well-established. |
| Increase in aeroallergens | Asthma | Sensitive groups—existing respiratory conditions, including asthma. | Effect on aeroallergens is complex and uncertain. | ||||
| Extreme Events Heatwaves | Exposure to extreme heat | Heat-related illnesses | Areas with higher temperatures. Urban areas due to urban heat island effect. Higher proportion of sensitive groups in some regions (elderly, isolated). | Low income groups—lower adaptive capacity and affected more by energy costs incurred during heatwaves. Food producers who may face crop losses, possible impact on tourism. | Elderly, isolated, pre-existing medical conditions. Low adaptive capacity—low income groups, homeless Higher exposure—certain occupations or lifestyles | Power cuts caused by high levels of peak demand. Damage to transport systems. Flow on effects to industry. Increased demand on health services. | Link between exposure to heat and health is well-established. Possible synergistic effects of exposure to heat and air pollutants should be considered. |
Current Management Practices and Limitations
| Impact Type | Current Management Practices | Potential Limitations in 2030 | Sector Column |
|---|---|---|---|
| Air quality—range of respiratory effects | Air Quality Management Program Medical treatment | Air Quality Management Plan requires updating Lack of resources | Environment Health Transport |
| Heatwaves - Direct heat-related effects | State Emergency Management Committee All West Australian Reducing Emergencies (AWARE) | More extreme events—will be more demand Ageing population—larger vulnerable group Lack of specific heat-wave response plan Lack of preparedness/education especially in remote indigenous communities Impact of energy blackouts on vulnerable groups | Emergency Services, Health, Energy, Indigenous Affairs |
2.4. Step 4—Risk Assessment Two: Workshop 2
- Extreme Events
- Temperature Increase and Related Changes
- Water-borne Disease and Water Quality
- Vector-borne diseases
- Air Quality
- Food-borne diseases
- Food Production
- Social Impact/Community Lifestyle—e.g., Dislocation, Mental Health
- the climate change projections and year as outlined by the Project Team
- a consideration of current management practices for each health impact
- the level of excess or additional risk linked to climate change
| Impact | Consequence | Likelihood | Risk | Rationale/Further Evidence. |
|---|---|---|---|---|
| Heat-related health effects during heatwaves | Catastrophic | Very Likely | Extreme | Strong evidence of link between heatwaves and health. Studies indicate increase in multiple heat-related fatalities due to climate change in Perth in 2030 [25]. Ageing population will increase size of vulnerable population. |
| Bushfires | Very High | Likely | High | Drier and hotter conditions in WA are likely to increase risk of fires. Possible fatalities and injuries, exposure to high particulate levels, significant psychosocial and socioeconomic costs. Vulnerable populations—bushfire prone areas, South-West WA. |
2.5. Step 5—Risk Management or Adaptation
| Risk Levels | Description of Management Action |
|---|---|
| Extreme | Risks require urgent attention at the most senior level and cannot simply be accepted by the community |
| High | Risk are the most severe that can be accepted by the community and need planned action |
| Medium | Risks can be expected to be part of normal circumstances but maintained under review by appropriate sectors |
| Low | Risks will be maintained under review but it is expected that existing controls will be sufficient and not further action will be required to treat them unless they become more severe |
Workshop 3—Adaptation Measures
| Categories of Adaptation | What Is Our Capacity *—In General and for Vulnerable Regions and Groups? | Suggestions for Implementation or Upgrading | Sectors Involved | |
|---|---|---|---|---|
| 1. Legislative or Regulatory | ||||
| • Cost sharing mechanisms for compensation and adaptation initiatives. | N | Only private insurance | Appropriate upgrades of procedures and assessments as climate change projections and assessments dictate. | Treasury, Insurance Planning, Housing Consumer Affairs, Emergency Services |
| • Regulations for minimum building standards to withstand extreme events in vulnerable regions. | A | Amend regulations as required | ||
| • Regulations regarding fire management, property management to reduce risk of injuries. | A | Amend regulations as required | ||
| • Mid to long-term strategies for land use planning that accounts for likely impacts | N | |||
| 2. Public Education & Communication | Wider community engagement needed Modern communication should be available to all (e.g., broadband) | Communication Health Local Government | ||
| • Improvement in communicating risks of extreme events to vulnerable regions and groups. | I/D | Continued improvement and greater investment required. | ||
| • Education of measures to reduce risk of damage or injuries | D | Coordination with Federal government is required. | ||
| • Evaluation of the effectiveness of educational materials. | I | |||
| 3. Surveillance and Monitoring | Access to GP data Up to date environmental and population forecasts Monitoring needs upgraded as required | Health, Planning, Environment, Climate Research Emergency Services Insurance industry | ||
| • Standardization of information collected after disasters to more accurately measure morbidity and mortality. | I | Long-term follow up is not adequate Hospital morbidity data is okay | ||
| • Evaluation of responses and health outcomes of extreme events. | I | |||
| 4. Ecosystem Intervention | Upgrade as needed Mostly mitigation but needs to address adaptation and prediction | Environment Agriculture Research Water, Planning | ||
| • Monitor the effects of altered land use on vulnerability to extreme weather events. | A | - | ||
| 5. Infrastructure Development | Emergency system needs to expand to cope with more frequent and more severe extreme events | Emergency Services, Health, Local Gov’t Planning, Water Energy, Transport | ||
| • Create or enhance emergency management—communication, preparation, training, volunteer recruitment, emergency response coordination, resource allocation. | I/D | North-west seen as vulnerable | ||
| • Mapping of potential risks from extreme events—location of hazardous facilities, vulnerable properties/people. | I/D | All understood to some extent | ||
| • Land use planning and management to minimize impacts from cyclones, flooding and fire (protective structures, controlled burning). | I/D | Need to highlight the necessity to Treasury to upgrade infrastructure as necessary. | ||
| 6. Technological or Engineering | ||||
| • Improvement of systems to provide early and accessible warning to the populations most likely to be affected. | D/A | Systems are in place The main issues are access to information and the community response to early warning systems. | Expand resources as required | Climate Research Building Health |
| • Modification of building codes for structures in vulnerable areas. | ||||
| 7. Health Intervention | ||||
| • Improved training programmes and information on emergency management. | A | Enhance responses to rural and regional areas | Continue development | Health Emergency Services |
| Research/ Information | ||||
| • Regional assessments of vulnerability to extreme events. | All either I or D | - | - | Whole of Government Health Research Climate Local Gov’ tIndigenous |
| • Regional identification of vulnerable communities and individual. | ||||
| • Evaluate effectiveness of early warning systems. | ||||
| • Further development of early warning systems—tropical cyclones, fires, droughts. | ||||
| • Modelling of affected regions | ||||
2.6. Step 6: Decision-Making
- A clear health impact statement including the final risk rankings and vulnerabilities
- Key adaptation actions, especially for priority risks and vulnerable groups
| Strategies | Actions | Lead Government Agencies | Support Agencies | |
|---|---|---|---|---|
| Heatwaves: Risk Level = Extreme | ||||
| 1. Legislative or regulatory | ||||
| Heat Event Response Plan | Extend state emergency plan to include heatwaves | Health, Emergency Services | Housing Planning Aged Care | |
| Limit power use in emergency periods | Sectors to discuss feasibility | Energy, Health | Planning Local Government | |
| Regulations for minimum energy efficiencies in homes | Expand energy star codes to existing homes. | Housing, energy | Building industry Businesses | |
| 2. Public education and communication (complete for all 8 categories) | ||||
- Strategic Direction—incorporation of climate change adaptation strategies into key sustainable development and health plans
- Government Responses—identify lead and support stakeholders particularly with respect to high risk impacts and ensure that high level management are aware of the report and the role of their sector in ensuring appropriate responses to climate change. The health sector should take a lead role by increasing cross-sectoral awareness of connections between health and climate and encouraging appropriate actions to protect the health of the community.
- Community Involvement—education programs regarding the potential health impacts of climate change and the key role of local government or councils with respect to community education.
- Key Activities/Projects—outline the specific projects required. Include cross-cutting measures that have the potential to affect multiple impacts or reduce multiple vulnerabilities. Highlight the potential need for more detailed assessment by other sectors with respect to their role in addressing high priority health risks.
3. Discussion
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Confalonieri, U.; Menne, B.; Akhtar, R.; Ebi, K.; Hauengue, M.; Kovats, R.; Revich, B.; Woodward, A. Human health. In Climate Change 2007: Impacts, Adaptation and Vulnerability; Cambridge University Press: Cambridge, UK, 2007; pp. 391–431. [Google Scholar]
- McMichael, A.; Haines, A. Global climate change: The potential effects on health. BMJ 1997, 315, 805–809. [Google Scholar] [CrossRef] [PubMed]
- McMichael, A.J.; Woodruff, R.E.; Hales, S. Climate change and human health: Present and future risks. Lancet 2006, 367, 859–869. [Google Scholar] [CrossRef] [PubMed]
- Fussel, H.; Klein, R. Climate change vulnerability assessments: An evolution of conceptual thinking. Clim. Change 2006, 75, 301–329. [Google Scholar] [CrossRef]
- Fussel, H.M. An updated assessment of the risks from climate change based on research published since the IPCC fourth assessment report. Clim. Change 2009, 97, 469–482. [Google Scholar] [CrossRef]
- World Health Organisation. Gothenburg Consensus Paper; WHO Regional Office for Europe: Copenhagen, Denmark, 1999; p. 4. [Google Scholar]
- Harris-Roxas, B.; Harris, E. Differing forms, differing purposes: A typology of health impact assessment. Environ. Impact Assess. Rev. 2011, 31, 396–403. [Google Scholar] [CrossRef]
- National Academy of Sciences. Improving Health in the United States: The Role of Health Impact Assessment; National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Patz, J.; Campbell-Lendrum, D.; Gibbs, H.; Woodruff, R. Health impact assessment of global climate change: Expanding on comparative risk assessment approaches for policy making. Annu. Rev. Public Health 2008, 29, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Spickett, J.T.; Brown, H.L.; Katscherian, D. Adaptation strategies for health impacts of climate change in Western Australia: Application of a health impact assessment framework. Environ. Impact Assess. Rev. 2011, 31, 297–300. [Google Scholar] [CrossRef]
- World Health Organisation. Climate Change and Human Health Risks and Responses; WHO: Geneva, Switzerland, 2003. [Google Scholar]
- Spickett, J.; Brown, H.; Katscherian, D. Health Impacts of Climate Change: Adaptation Strategies for Western Australia; Government of Western Australia: Perth, Australia, 2007. [Google Scholar]
- Spickett, J.; Katscherian, D.; Brown, H. Climate Change, Vulnerability and Health: A Guide to Assessing and Addressing the Health Impacts. Curtin University: Bentley, Australia, 2012. Available online: http://ehia.curtin.edu.au/local/docs/ClimateChangeHealthVulnerabilityGuidelines2012.pdf (accessed on 3 November 2014).
- World Health Organisaton. Preamble to the Constitution of the World Health Organization; WHO: Geneva, Switzerland, 1948. [Google Scholar]
- IPCC. Climate Change 2007: Impacts, Adaptation and Vulnerability; Cambridge University Press: Cambridge, UK, 2007; p. 976. [Google Scholar]
- Harris, P.; Harris-Roxas, B.; Harris, E.; Kemp, L. Health Impact Assessment: A Practical Guide; UNSW Research Centre for Primary Health Care and Equity and NSW Health: Sydney, Australia, 2007. [Google Scholar]
- Nelson, R.; Kokic, P.; Crimp, S.; Meinke, H.; Howden, S.M. The vulnerability of Australian rural communities to climate variability and change: Part I—Conceptualising and measuring vulnerability. Environ. Sci. Policy 2010, 13, 8–17. [Google Scholar] [CrossRef]
- Patz, J.; McGeehin, M.; Bernard, S.; Ebi, K.; Epstein, P.; Grambsch, A.; Gubler, D.; Reiter, P.; Romieu, I.; Rose, J. The potential health impacts of cimate variability and change for the United States: Executive summary of the report of the health sector of the US national assessment. Environ. Health Perspect. 2000, 108, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Synnott, G.; Katscherian, D. Public Health Consultation: A Guide for Developers; Department of Health: Perth, Australia, 2006. [Google Scholar]
- Spickett, J.T.; Katscherian, D. Health impacts of climate change in the Solomon Islands: An assessment and adaptation action plan. Glob. J. Health Sci. 2014, 6. [Google Scholar] [CrossRef]
- Spickett, J.T.; Katscherian, D.; McIver, L. Health impacts of climate change in Vanuatu: An assessment and adaptation action plan. Glob. J. Health Sci. 2013, 5. [Google Scholar] [CrossRef]
- Brown, H.; Spickett, J. Health consequence scales for use in health impact assessments of climate change. Int. J. Environ. Res. Public Health 2014, 11, 9607–9620. [Google Scholar] [CrossRef] [PubMed]
- Hames, D.; Vardoulakis, S. Climate Change Risk Assessment for the Health Sector; Department for Environment, Food and Rural Affairs: London, UK, 2012. [Google Scholar]
- Mastrandrea, M.; Field, C.; Stocker, T.; Edenhofer, O.; Ebi, K.; Frame, D.; Held, H.; Kriegler, E.; Mach, K.; Matschoss, P.; et al. Guidance Note for Lead Authors of the IPCC Fifth Assessment Report on Consistent Treatment of Uncertainties; IPCC: Copenhagen, Denmark, 2010. [Google Scholar]
- Bambrick, H.; Dear, K.; Woodruff, R.; Hanigan, I.; McMichael, A. The Impacts of Climate Change on Three Health Outcomes: Temperature-Related Mortality and Hospitalisations, Salmonellosis and Other Bacterial Gastroenteritis, and Population at Risk from Dengue. Available online: http://garnautreview.org.au/CA25734E0016A131/WebObj/03-AThreehealthoutcomes/$File/03-A%20Three%20health%20outcomes.pdf (accessed on 3 November 2014).
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, H.; Spickett, J.; Katscherian, D. A Health Impact Assessment Framework for Assessing Vulnerability and Adaptation Planning for Climate Change. Int. J. Environ. Res. Public Health 2014, 11, 12896-12914. https://doi.org/10.3390/ijerph111212896
Brown H, Spickett J, Katscherian D. A Health Impact Assessment Framework for Assessing Vulnerability and Adaptation Planning for Climate Change. International Journal of Environmental Research and Public Health. 2014; 11(12):12896-12914. https://doi.org/10.3390/ijerph111212896
Chicago/Turabian StyleBrown, Helen, Jeffery Spickett, and Dianne Katscherian. 2014. "A Health Impact Assessment Framework for Assessing Vulnerability and Adaptation Planning for Climate Change" International Journal of Environmental Research and Public Health 11, no. 12: 12896-12914. https://doi.org/10.3390/ijerph111212896




