Knowledge, Attitudes and Practices Regarding Cervical Cancer and Screening among Haitian Health Care Workers
Abstract
:1. Introduction
2. Experimental Section
3. Results and Discussion
3.1. Survey Results
3.1.1. Knowledge
| Demographic | Total (N) |
|---|---|
| Age | |
| ≤30 | 8 |
| >31 | 11 |
| Gender | |
| Female | 19 |
| Male | 1 |
| Ethnic Group | |
| Haitian | 21 |
| Other | - |
| Primary Language | |
| Creole | 19 |
| French | 2 |
| English | 1 |
| Primary Job | |
| Medical Student | 1 |
| Nurse | 4 |
| OBGYN Physician | 1 |
| Other | 15 |
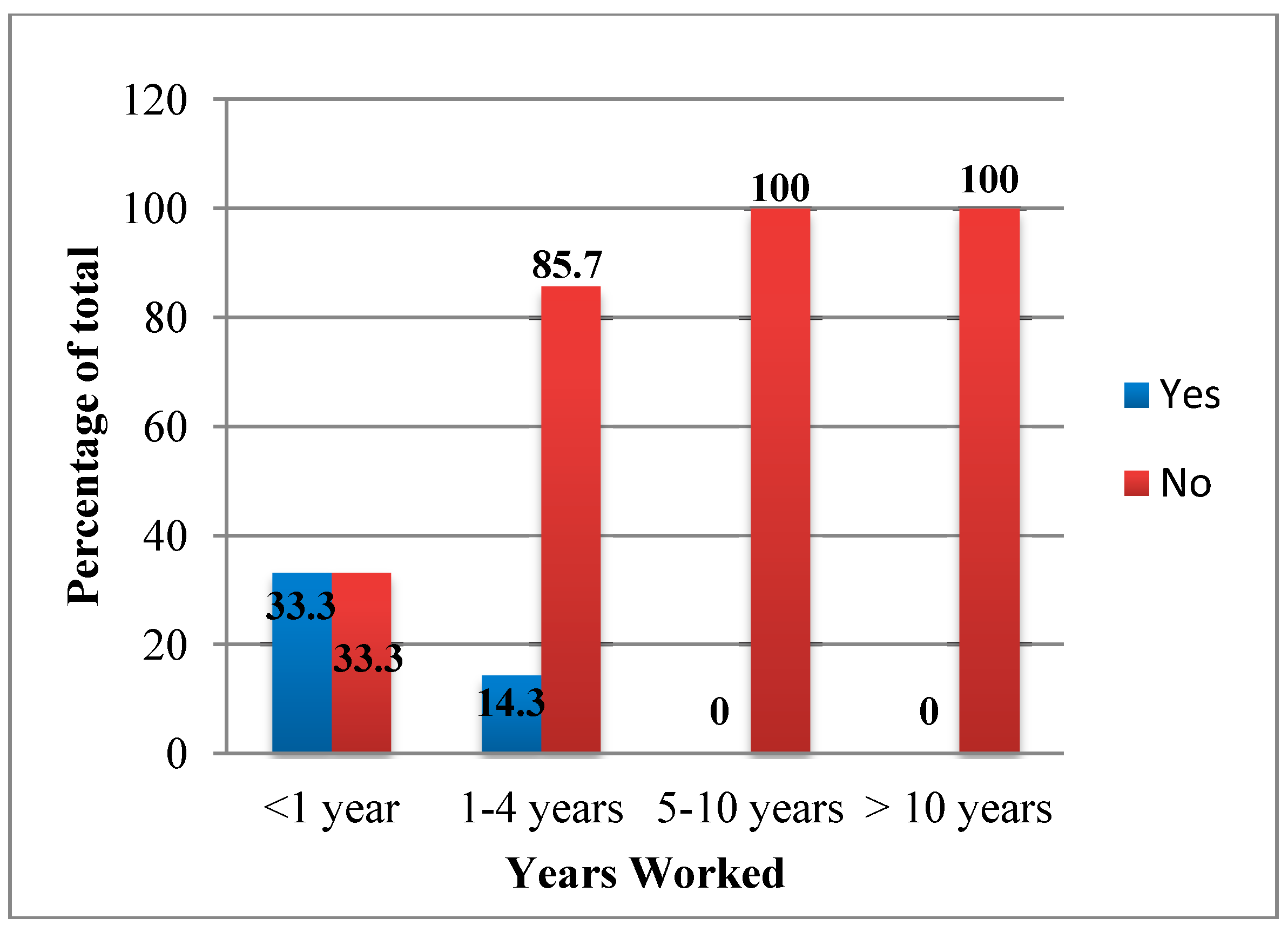
| Length of Time at Current Job | |
| <1 year | 5 |
| 1–4 years | 9 |
| 5–10 years | 4 |
| >10 years | 3 |
3.1.2. Attitudes
3.1.3. Practices
3.2. Discussion
4. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Summary Report on HPV and Cervical Cancer Statistics in Haiti; WHO/ICO Information Center on HPV and Cervical Cancer: Barcelona, Spain, 2010.
- Ferlay, J.; Bray, F.; Pisani, P.; Parkin, D.M. Globocan 2000: Cancer Incidence,Mortality and Prevalence Worldwide; IARC Press: Lyon, France, 2001. [Google Scholar]
- Ferlay, J.; Shin, H.R.; Bray, F.; Forman, D.; Mathers, C.; Parkin, D.M. Estimates of worldwide burden of cancer in 2008. Int. J. Cancer 2008, 127, 2893–2917. [Google Scholar]
- Brinton, L.A.; Hamman, R.F.; Huggins, G.R.; Lehman, H.F.; Levine, R.S.; Mailin, K.; Fraumeni, J.F. Sexual and reproductive risk factors for invasive squamous cell cervical cancer. J. Natl. Cancer Inst. 1987, 7, 23–30. [Google Scholar]
- Blumenthal, P.D.; Gaffikin, L. Cervical cancer prevention: making programs more appropriate and pragmatic. JAMA 2005, 294, 2225–2228. [Google Scholar]
- Bosch, F.X.; Burchell, A.N.; Schiffman, M.; Giullian, A.R.; de Sanjose, S.; Bruni, L.; Tortolero-Luna, G.; Kjaer, S.K.; Munoz, N. Epidemiology and natural history of human papillomavirus infections and type-specific implications in cervical neoplasia. Vaccine 2008, 26, 1–16. [Google Scholar]
- Smith, J.S.; Lindsay, L.; Hoots, B.; Keys, J.; Franceschi, S.; Winer, R.; Clifford, G.M. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: A meta-analysis update. Int. J. Cancer 2007, 121, 621–632. [Google Scholar]
- Kahn, J.A. HPV vaccination for the prevention of cervical intraepithelial neoplasia. N. Engl. J. Med. 2009, 361, 271–278. [Google Scholar]
- Blumberg, H.; Goedken, J.; Kress, C. Knowledge,Attitudes, and Practices Regarding Cervical Cancer and Screening among Ethiopian Healthcare Workers. Available online: http://applications.emro.who.int/emhj/V17/11/17_11_2011_0855_0861.pdf (accessed on 6 November 2014).
- Goldie, S.J.; Gaffikin, L.; Goldhaber-Fiebert, J.D.; Gordillo-Tobar, A.; Levin, C.; Mahe, C.; Wright, T. Cost-effectiveness of cervical-cancer screening in five developing countries. N. Engl. J. Med. 2005, 35, 2158–2168. [Google Scholar]
- Ottaviano, M.; la Torre, P. Examination of the cervix with the naked eye using acetic acid test. Amer. J. Obstet. Gynecol. 1982, 143, 139–142. [Google Scholar]
- Qiao, Y.L.; Sellors, J.W.; Eder, P.S.; Bao, Y.P.; Lim, J.M.; Zhao, F.H.; Weigl, B.; Zhang, W.H.; Peck, R.B.; Li, L.; et al. A new HPV-DNA test for cervical-cancer screening in developing regions: A cross-sectional study of clinical accuracy in rural China. Lancet Oncol. 2008, 9, 929–936. [Google Scholar]
- Gaffikin, L.; Lauterbach, M.; Blumenthal, P.D. Performance of visual inspection with acetic acid for cervical cancer screening: A qualitative summary of evidence to date. Obstet. Gynecol. Surv. 2008, 58, 543–550. [Google Scholar]
- Sankaranarayanan, R.; Basu, P.; Wesley, R.S.; Mahe, C.; Keita, N.; Mbalawa, C.C.; Sharm, R.; Dolo, A.; Shastri, S.S.; Nacoulma, M.; et al. Accuracy of visual screening for cervical neoplasia: Results from an IARC multicenter study in India and Africa. Int. J. Cancer 2004, 110, 907–913. [Google Scholar]
- Denny, L.; Kuhn, L.; de Souza, M.; Pollack, A.E.; Dupree, W.; Wright, T.C. Screen-and-treat approaches for cervical cancer prevention in low-resource settings: A randomized controlled trial. JAMA 2005, 294, 2173–2181. [Google Scholar]
- Gaffikin, L.; Blumenthal, P.D.; Emerson, M.; Limpaphayom, K. Safety, acceptability, and feasibility of a single-visit approach to cervical-cancer prevention in rural Thailand: A demonstration project. Lancet 2003, 361, 814–820. [Google Scholar]
- Akinwuntan, A.L.; Adesina, O.A.; Okolo, C.A.; Oluwasola, O.A.; Oladokun, A.; Ifemeje, A.A.; Adewole, I.F. Correlation of cervical cytology and visual inspection with acetic acid in HIV-positive women. J. Obstet. Gynaecol. 2008, 28, 638–641. [Google Scholar]
- Sankaranarayanan, R.; Nene, B.M.; Shastri, S.S.; Jayant, K.; Muwonge, R.; Budukh, A.M.; Hingmire, S.; Malvi, S.G.; Thorat, R.; Kothari, A.; et al. HPV screening for cervical cancer in rural India. N. Engl. J. Med. 2009, 360, 1385–1394. [Google Scholar]
- Pfaendler, K.S.; Mwanahamuntu, M.H.; Sahasrabuddhe, V.V.; Mudenda, V.; Stringer, J.S.; Parham, G.P. Management of cryotherapy-ineligible women in a “screen-and-treat” cervical cancer prevention program targeting HIV-infected women in Zambia: lessons from the field. Gynecol. Oncol. 2008, 110, 402–407. [Google Scholar]
- Sankaranarayanan, R.; Rajkumar, R.; Esmy, P.O.; Fayette, J.M.; Shanthakumary, S.; Frappart, L.; Thara, S.; Cherian, J. Effectiveness, safety and acceptability of “see and treat” with cryotherapy by nurses in a cervical screening study in India. Brit. J. Cancer 2007, 96, 738–743. [Google Scholar]
- Goldie, S.J.; Kuhn, L.; Denny, L.; Pollack, A.; Wright, T.C. Policy analysis of cervical cancer screening strategies in low-resource settings: Clinical benefits and cost-effectiveness. JAMA 2001, 285, 3107–3115. [Google Scholar]
- Mandelblatt, J.S.; Lawrence, W.F.; Gaffikin, L.; Limpahayom, K.K.; Lumbiganon, P.; Warakamin, S.; King, J.; Yi, B.; Ringers, P.; Blumenthal, P.; et al. Costs and benefits of different strategies to screen for cervical cancer in less-developed countries. J. Natl. Cancer Inst. 2002, 94, 1469–1483. [Google Scholar]
- Shi, J.F.; Canfell, K.; Lew, J.B.; Zhao, F.H.; Legood, R.; Ning, Y.; Simonella, L.; Ma, L.; Kang, Y.J.; Zhang, Y.Z.; et al. Evaluation of primary HPV-DNA testing in relation to visual inspection methods for cervical cancer screening in rural China: An epidemiologic and cost-effectiveness modelling study. BMC Cancer 2011, 11. [Google Scholar] [CrossRef]
- Gage, J.C.; Ajenifuja, K.O.; Wentzensen, N.; Adepiti, A.C.; Stoler, M.; Eder, P.S.; Bell, L.; Shrestha, N.; Eklund, C.; Reilly, M.; et al. Effectiveness of a simple rapid human papillomavirus DNA test in rural Nigeria. Int. J. Cancer 2011, 131, 2903–2909. [Google Scholar]
- Luciani, S.; Gonzales, M.; Munoz, S.; Jeronimo, J.; Robles, S. Effectiveness of cryotherapy treatment for cervical intraepithelial neoplasia. Int. J. Gynaecol. Obstet. 2008, 101, 172–177. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zahedi, L.; Sizemore, E.; Malcolm, S.; Grossniklaus, E.; Nwosu, O. Knowledge, Attitudes and Practices Regarding Cervical Cancer and Screening among Haitian Health Care Workers. Int. J. Environ. Res. Public Health 2014, 11, 11541-11552. https://doi.org/10.3390/ijerph111111541
Zahedi L, Sizemore E, Malcolm S, Grossniklaus E, Nwosu O. Knowledge, Attitudes and Practices Regarding Cervical Cancer and Screening among Haitian Health Care Workers. International Journal of Environmental Research and Public Health. 2014; 11(11):11541-11552. https://doi.org/10.3390/ijerph111111541
Chicago/Turabian StyleZahedi, Leilah, Emma Sizemore, Stuart Malcolm, Emily Grossniklaus, and Oguchi Nwosu. 2014. "Knowledge, Attitudes and Practices Regarding Cervical Cancer and Screening among Haitian Health Care Workers" International Journal of Environmental Research and Public Health 11, no. 11: 11541-11552. https://doi.org/10.3390/ijerph111111541




