Validation of the Apple Watch for Heart Rate Variability Measurements during Relax and Mental Stress in Healthy Subjects
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Setup
2.2. Synchronization and RR Matching
2.3. Validation of RR Series
2.4. Heart Rate Variability Parameters
2.5. Statistical Analysis
3. Results
3.1. Validity of RR Series
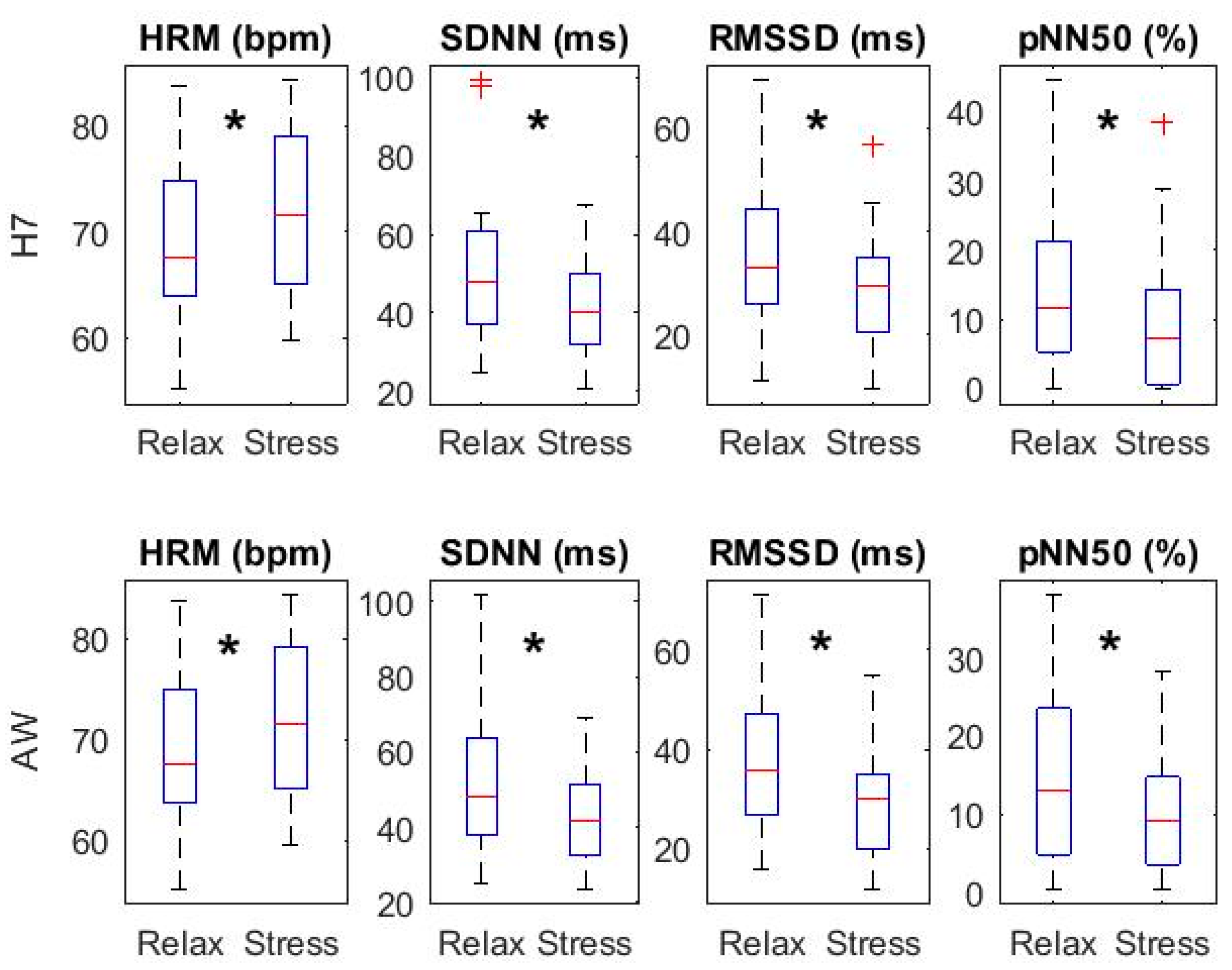
3.2. HRV Parameters: Temporal Domain
3.3. HRV Parameters: Frequency Domain
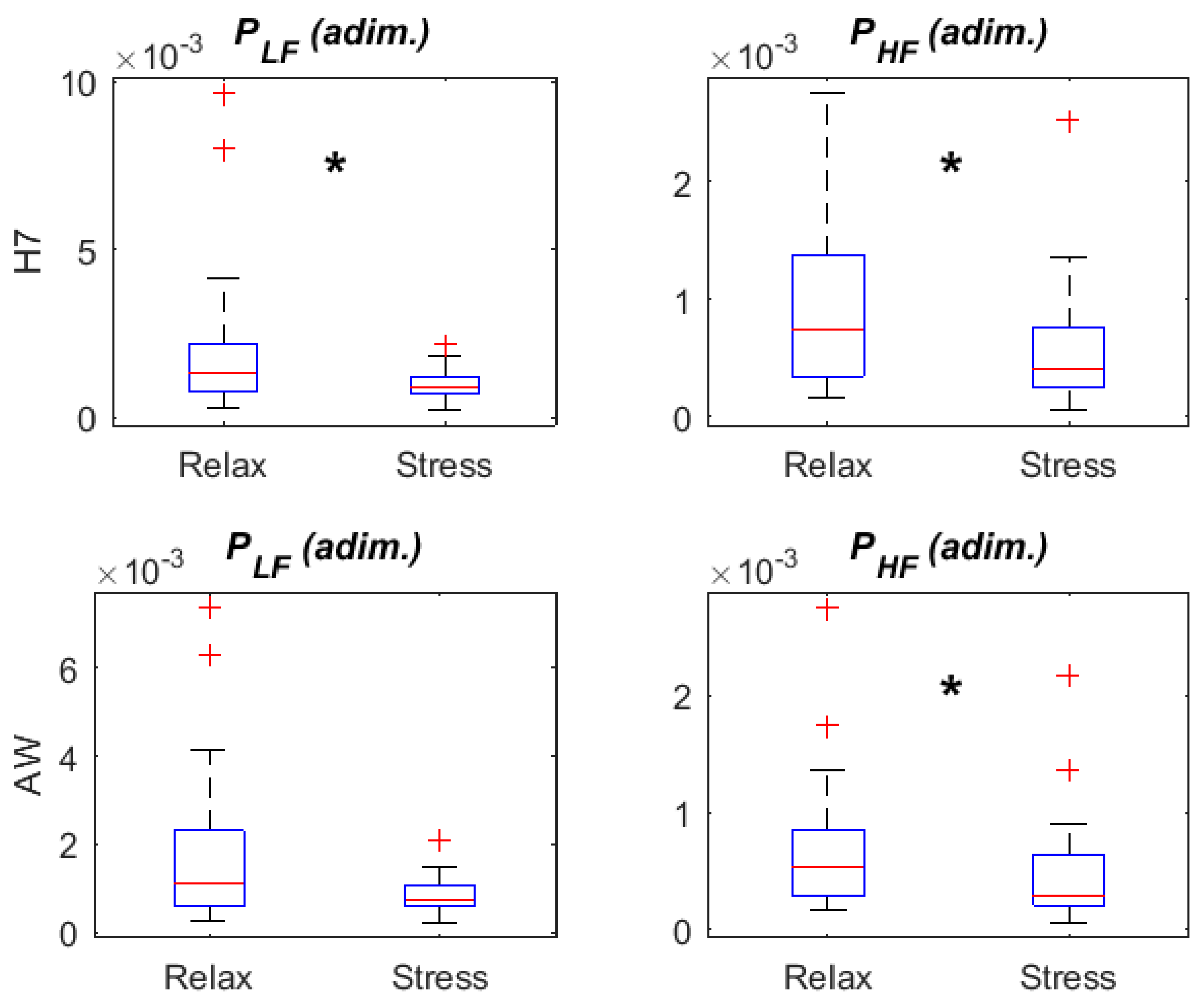
3.4. HRV Parameters: Relax vs. Stress
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Camm, A.J.; Malik, M.; Bigger, J.T.; Brethardt, G.; Cerutti, S.; Cohen, R.J.; Coumel, P.; Fallen, E.L.; Kennedy, H.L.; Kleiger, R.E.; et al. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar]
- Thayer, J.; Ahs, F.; Fredrikson, M.; Sollers, J.; Wager, T. A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neurosci. Biobehav. Rev. 2012, 36, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Billman, G. Heart rate variability—A historical perspective. Front. Physiol. 2011, 2, 86. [Google Scholar] [CrossRef] [PubMed]
- Beauchaine, T.; Thayer, J. Heart rate variability as a transdiagnostic biomarker of psychopathology. Int. J. Psychophysiol. 2015, 98, 338–350. [Google Scholar] [CrossRef] [PubMed]
- Koenig, J.; Kemp, A.; Beauchaine, T.; Thayer, J.; Kaess, M. Depression and resting state heart rate variability in children and adolescents—A systematic review and meta-analysis. Clin. Psychol. Rev. 2016, 46, 136–150. [Google Scholar] [CrossRef] [PubMed]
- Tobaldini, E.; Nobili, L.; Strada, S.; Casali, K.; Braghiroli, A.; Montano, N. Heart rate variability in normal and pathological sleep. Front. Physiol. 2013, 4, 294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Cheon, E.; Bai, D.; Lee, Y.; Koo, B. Stress and heart rate variability: A meta-analysis and review of the literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Hernando, A.; Lázaro, J.; Gil, E.; Arza, A.; Garzón, J.; López-Antón, R.; de la Cámara, C.; Laguna, P.; Aguiló, J.; Bailón, R. Inclusion of respiratory frequency information in heart rate variability analysis for stress assessment. IEEE J. Biomed. Health Inform. 2016, 20, 1016–1025. [Google Scholar] [CrossRef] [PubMed]
- Vicente, J.; Laguna, P.; Bartra, A.; Bailón, R. Drowsiness detection using heart rate variability. Med. Biol. Eng. Comput. 2016, 54, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Kiviniemi, A.; Hautala, A.; Kinnunen, H.; Tulppo, M. Endurance training guided individually by daily heart rate variability measurements. Eur. J. Appl. Physiol. 2007, 101, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Plews, D.; Laursen, P.; Stanley, J.; Kilding, A.; Buchheit, M. Training adaptation and heart rate variability in elite endurance athletes: Opening the door to effective monitoring. Sports Med. 2013, 43, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; He, Z.; Zhao, J.; Tao, D.; Xu, K.; Earnest, C.; McNaughton, L. Heart rate variability threshold values for early-warning nonfunctional overreaching in elite female wrestlers. J. Strength Cond. Res. 2013, 27, 1511–1519. [Google Scholar] [CrossRef] [PubMed]
- Shcherbina, A.; Mattsson, C.; Waggott, D.; Salisbury, H.; Christle, J.; Hastie, T.; Wheeler, M.; Ashley, E. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J. Pers. Med. 2017, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Gil, E.; Orini, M.; Bailón, R.; Vergara, J.; Mainardi, L.; Laguna, P. Photoplethysmography pulse rate variability as a surrogate measurement of heart rate variability during non-stationary conditions. Physiol. Meas. 2010, 31, 1271–1290. [Google Scholar] [CrossRef] [PubMed]
- Eskola, H.; Väisänen, O.; Viik, J.; Hyttinen, J. Evaluation of the accuracy and reliability for photoplethysmography based heart rate and beat-to-beat detection during daily activities. In Proceedings of the Joint Conference of the European Medical and Biological Engineering Conference (EMBEC) and the Nordic-Baltic Conference on Biomedical Engineering and Medical Physics (NBC) 2017, Tampere, Finland, 11–15 June 2017. [Google Scholar]
- Wallen, M.; Gomersall, S.; Keating, S.; Wisløff, U.; Coombes, J. Accuracy of heart rate watches: Implications for weight management. PLoS ONE 2016, 11, e0154420. [Google Scholar] [CrossRef] [PubMed]
- Abt, G.; Bray, J.; Benson, A. The validity and inter-device variability of the Apple Watch for measuring maximal heart rate. J. Sports Sci. 2017, 36, 1447–1452. [Google Scholar] [CrossRef] [PubMed]
- Khushhal, A.; Nichols, S.; Evans, W.; Gleadall-Siddall, D.; Page, R.; O’Doherty, A.; Carroll, S.; Ingle, L.; Abt, G. Validity and reliability of the AppleWatch for measuring heart rate during exercise. Sports Med. Int. Open 2017, 1, 206–211. [Google Scholar]
- Wang, R.; Blackburn, G.; Desai, M.; Phelan, D.; Gillinov, L.; Houghtaling, P.; Gillinov, M. Accuracy of wrist-worn heart rate monitors. JAMA Cardiol. 2017, 2, 104–106. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Hibbing, P.; Mantis, C.; Welk, G. Comparative evaluation of heart rate-based monitors: Apple Watch vs Fitbit Charge HR. J. Sports Sci. 2017, 36, 1734–1741. [Google Scholar] [CrossRef] [PubMed]
- Canalys. 18 Million Apple Watches Ship in 2017, up 54% on 2016. 2018. Available online: https://www.canalys.com/newsroom/18-million-apple-watches-ship-2017-54-2016 (accessed on 4 July 2018).
- Giles, D.; Draper, N.; Neil, W. Validity of the Polar V800 heart rate monitor to measure RR intervals at rest. Eur. J. Appl. Physiol. 2016, 116, 563–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caminal, P.; Sola, F.; Gomis, P.; Guasch, E.; Perera, A.; Soriano, N.; Mont, L. Validity of the Polar V800 monitor for measuring heart rate variability in mountain running route conditions. Eur. J. Appl. Physiol. 2018, 118, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Valderas, M.T.; Bolea, J.; Laguna, P.; Vallverdú, M.; Bailón, R. Human Emotion Recognition Using Heart Rate Variability Analysis with Spectral Bands Based on Respiration. In Proceedings of the 37nd Annual International Conference of the IEEE EMBS, Milan, Italy, 25–29 August 2015; pp. 6134–6137. [Google Scholar]
- Bland, J.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 8, 307–310. [Google Scholar] [CrossRef]
- Lin, L. A concordance correlation coefficient to evaluate reproducibility. Biometrics 1989, 45, 255–268. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R. Statistical Methods for Research Workers; Oliver & Boyd: Edinburgh, UK, 1925. [Google Scholar]
- Costa-Santos, C.; Antunes, L.; Souto, A.; Bernardes, J. Assessment of disagreement: A new information-based approach. Ann. Epidemiol. 2010, 20, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Mateo, J.; Laguna, P. Improved heart rate variability signal analysis from the beat occurrence times according to the IPFM model. IEEE Trans. Biomed. Eng. 2000, 47, 985–996. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bailón, R.; Laouini, G.; Grao, C.; Orini, M.; Laguna, P.; Meste, O. The integral pulse frequency modulation with time-varying threshold: Application to heart rate variability analysis during exercise stress testing. IEEE Trans. Biomed. Eng. 2011, 58, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Sacha, J. Interplay between heart rate and its variability: A. prognostic game. Front. Physiol. 2014, 5, 347. [Google Scholar] [CrossRef] [PubMed]
- Valenza, G.; Garcia, R.; Citi, L.; Scilingo, E.; Tomaz, C.; Barbieri, R. Nonlinear digital signal processing in mental health: Characterization of major depression using instantaneous entropy measures of heartbeat dynamics. Front. Physiol. 2015, 6, 74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weippert, M.; Behrens, K.; Rieger, A.; Stoll, R.; Kreuzfeld, S. Heart rate variability and blood pressure during dynamic and static exercise at similar heart rate levels. PLoS ONE 2013, 8, e83690. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M. Monitoring training status with HR measures: Do all roads lead to Rome? Front. Physiol. 2014, 5, 73. [Google Scholar] [CrossRef] [PubMed]
- Gamelin, F.X.; Baquet, G.; Berthoin, S.; Bosquet, L. Validity of the polar S810 to measure R-R intervals in children. Int. J. Sports Med. 2008, 29, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Nunan, D.; Jakovljevic, D.G.; Donovan, G.; Hodges, L.D.; Sandercock, G.R.; Brodie, D.A. Levels of agreement for RR intervals and short-term heart rate variability obtained from the Polar S810 and an alternative system. Eur. J. Appl. Physiol. 2008, 103, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, M.P.; da Silva, N.T.; de Azevedo, F.M.; Pastre, C.M.; Vanderlei, L.C. Comparison of Polar® RS800G3™ heart rate monitor with Polar® S810i™ and electrocardiogram to obtain the series of RR intervals and analysis of heart rate variability at rest. Clin. Physiol. Funct. Imaging 2016, 36, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Hernando, D.; Garatachea, N.; Almeida, R.; Casajús, J.A.; Bailón, R. Validation of Heart Rate Monitor Polar RS800 for Heart Rate Variability Analysis During Exercise. J. Strength Cond. Res. 2018, 32, 716–725. [Google Scholar] [CrossRef] [PubMed]
- Porges, S. Cardiac vagal tone: A physiological index of stress. Neurosci. Biobehav. Rev. 1995, 19, 225–233. [Google Scholar] [CrossRef]




| RELAX | STRESS | |
|---|---|---|
| Mean (SD) H7 RR intervals (ms) | 869.28 (114.01) | 834.78 (97.43) |
| Mean (SD) AW RR intervals (ms) | 869.23 (114.39) | 834.70 (97.84) |
| CCC (90% CI) | 0.989 (0.981, 0.998) | 0.977 (0.970, 0.985) |
| ICC (90% CI) | 0.989 (0.984, 0.996) | 0.982 (0.977, 0.987) |
| A (90% CI) | 0.993 (0.987, 0.999) | 0.983 (0.975, 0.991) |
| Bias (Out LOA) | 0.049 (3.29%) | 0.078 (3.93%) |
| Mean (SD)% missed RR intervals | 10.98 (9.78) | 9.45 (7.30) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernando, D.; Roca, S.; Sancho, J.; Alesanco, Á.; Bailón, R. Validation of the Apple Watch for Heart Rate Variability Measurements during Relax and Mental Stress in Healthy Subjects. Sensors 2018, 18, 2619. https://doi.org/10.3390/s18082619
Hernando D, Roca S, Sancho J, Alesanco Á, Bailón R. Validation of the Apple Watch for Heart Rate Variability Measurements during Relax and Mental Stress in Healthy Subjects. Sensors. 2018; 18(8):2619. https://doi.org/10.3390/s18082619
Chicago/Turabian StyleHernando, David, Surya Roca, Jorge Sancho, Álvaro Alesanco, and Raquel Bailón. 2018. "Validation of the Apple Watch for Heart Rate Variability Measurements during Relax and Mental Stress in Healthy Subjects" Sensors 18, no. 8: 2619. https://doi.org/10.3390/s18082619






