1. Introduction
Microwave imaging for biomedical applications has gained much attention in the last two decades. The relatively long wavelength allows for penetration in living tissue as deep as ten centimeters, especially at the low-gigahertz range. This makes microwave technology a promising candidate in diagnostic applications such as breast-cancer screening [
1,
2,
3,
4,
5], bone-disease monitoring [
6,
7], brain-stroke [
8,
9,
10] and lung-cancer diagnostics [
11,
12].
Currently, the main effort is in improving the image resolution and the diagnostic performance of the modality. There are several inherent challenges associated with this effort, which have so far hindered deployment in clinical practice. These include the complex pattern of the microwave propagation through the tissue [
1,
13], the wide statistical spread in the (complex) permittivity values of healthy tissues, which may overlap those of malignant tissues (e.g., in the breast), the uncertainties in the measured tissue dielectric properties, as well as the strong dissipation [
1,
14,
15,
16,
17]. Many of these challenges are addressed through improvements in the reconstruction algorithms; however, the improvement of the hardware and the data quality is critically important.
This work focused on hardware development, which promises substantial improvement of the signal-to-noise ratio (SNR) and the dynamic range of the microwave acquisition system. With the advent of on-chip radio components such as low-noise amplifiers (LNAs) and mixers, it is now possible to integrate these with the antenna in a single active radio sensor whose output is at an intermediate frequency (IF) in the low megahertz range. This makes the sensor multiplexing simpler and cheaper since it circumvents the need for radio-frequency (RF) switches, transmission lines and connectors, which introduce loss and signal distortion. These RF components are also sensitive to operational factors such as temperature, bending, twisting, and poor contact, which lead to phase errors, measurement uncertainties and problematic trouble-shooting.
With the sensor’s output being at IF, it is possible to multiplex hundreds of sensors to a common IF port, where the signal can be further processed to extract magnitude and phase information. At IF, the required transmission lines are electrically very short, the losses are low and the impedance matching is simpler. This is a significant advantage over the existing RF-switched arrays. To our knowledge, the largest RF-switched antenna array for tissue imaging is the one reported by Klemm et al. [
18], where 60 antennas are arranged on a hemispherical surface. In such arrays, each antenna connects to a large RF switching network through a high-quality RF cable and connectors. Careful calibration is required to account for the impact of the impedance match, the losses and the phase delays of all RF components.
When the number of array elements and their spacing do not provide sufficient spatial sampling, the RF-switched arrays are combined with mechanical scanning. For example, in [
19], a hand-held compact impulse-radar detector is developed using
cross-shaped dome antenna array. Two single-pole-eight-throw (SP8T) RF switches are used to control the antenna array element in RF frequency. To overcome the drawback of the limited number of the elements, this prototype also employs rotation in order to obtain sufficient spatial sampling. This increases the scanning time and may lead to positioning uncertainties.
It should be noted that RF-switched antenna arrays offer significant improvement over the mechanically scanned systems (see, e.g., [
20,
21]), where positioning uncertainties and long acquisition times impede the implementation in clinical practice. Nonetheless, the number of elements that RF switches can multiplex remains limited.
To overcome the drawbacks of RF-switched arrays, the modulated scatterer technique (MST) has been proposed [
22,
23,
24,
25,
26]. With this technique, the modulated scatterers are connected wirelessly to a single RF port, making the system flexible and capable of handling many sensing elements. However, these systems have relatively small dynamic range and narrow bandwidths.
The multiplexing of the active sensors in the imaging array can be conveniently carried out by switching on and off the bias of its active circuits (the LNA, the mixer and/or the IF amplifier). This is realized using a digital network, the design and fabrication of which is simple compared to an RF distribution network.
Table 1 provides a summary of the advantages of the bias-switched active-sensor array in comparison with the RF-switched, MST and scanned antenna arrays.
It should be noted that the MST arrays can be also viewed as RF-to-low-frequency converters.
The limiting factor in the electronic switching of a frequency-sweep sensor such as ours is the settling time in the receiver’s local oscillator. This settling time is particularly stringent in a coherent receiver, which employs a phase-locking loop, as explained in [
27]. Depending on the IF bandwidth, the settling time ranges from tens of microseconds to tens of milliseconds [
28,
29], which sets the lower limit on the time required to perform the measurement at one frequency before moving to the next. In our bias-switched array, the bias is switched ON one element at a time. Once the bias for a given array element is ON, the frequency sweep is performed. Therefore, the period during which the bias of an element is ON equals
, where
is the number of frequency samples and
is the settle time of the local oscillator. Equivalently, the rate at which the bias is switched is
times lower than the rate at which the frequency hopping is performed.
The proposed sensor is suitable for applications in various configurations including planar, spherical and cylindrical surfaces. This is because the antennas are very small and can be easily deployed on curved surfaces. This is evident from the fact that the original antenna design has been used in a hemispherical array [
19] which employs RF switching.
Here, the first application of the radio sensor is in a planar scenario. A planar microwave breast imaging system has already been reported in [
30]. There, it is recognized that the planar configuration has certain advantages such as the fact that it is independent of the organ size. Furthermore, it is pointed out that the signal paths are shorter than those in hemi-spherical or cylindrical breast imaging, leading to better signal quality. At the same time, the compression is less than that in mammography.
A bias-switched UWB radio sensor for tissue imaging was first proposed in [
31,
32], where mixed-signal simulations suggested that a dynamic range as high as 127 dB can be achieved provided the IF receiver noise floor is sufficiently low, i.e.,
dBm at a resolution bandwidth of 1 Hz. Here, we show the experimental results with a prototype of the radio sensor, which demonstrate a dynamic range of 118 dB when the resolution bandwidth is set at 100 Hz.
In
Section 2, the design of the antenna array is discussed along with the tissue phantoms used in the experiments.
Section 3 discusses the integration of the antenna array with the LNA and the mixer.
Section 4 describes the measurements of the dynamic range of the active sensor. Discussion and conclusions are provided in
Section 5 and
Section 6, respectively.
5. Discussion
This manuscript proposes a new approach to designing microwave-imaging hardware; it does not propose a new imaging method. In particular, it proposes a new active sensor, which incorporates both an antenna and a radio front end. The sensor is controlled to assume an ON and an OFF state by simply switching the radio bias on and off. The goal of developing a bias-switched active radio sensor, is to enable the multiplexing of hundreds to thousands of sensors in an array. Such large-scale multiplexing is practical only if the output of each sensor is at a low narrow-band frequency range (in the low mega-hertz range), so that the signal transmission and distribution networks are simple, low-loss and low-distortion. Thereby, the sensor output must be at IF. Such technological development would be beneficial to microwave imaging in general but tissue imaging can benefit the most as it suffers from poor data quality due to high loss, high noise, uncertainty, and insufficient spatial sampling. Current RF-switched technology is limited to several tens of antennas, resulting in insufficient spatial sampling. Antenna scanning can provide fine sampling but is prohibitively slow and suffers from positioning uncertainties. The proposed active sensor array offers a solution where scanning is avoided, yet thousands of spatial samples can be gathered within seconds through electronic switching of the bias network of the array.
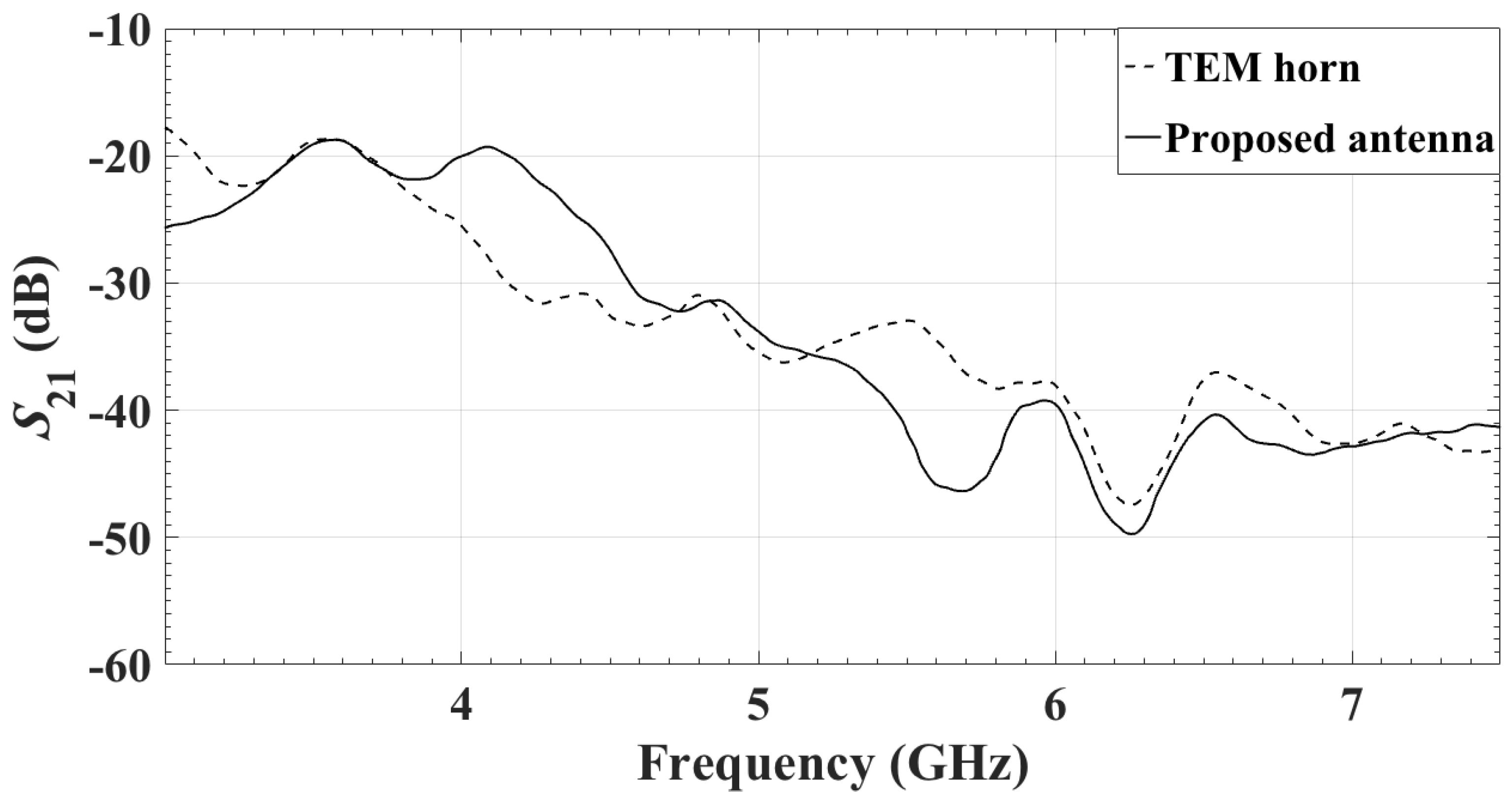
The active radio sensor investigated here is to be used in an UWB bias-switched array for microwave imaging of the breast. This leads to the antenna design requirements, such as UWB bandwidth (preferably between 3 GHz and 7 GHz or more), small size ( mm on a side), light weight, and PCB technology. We have demonstrated that the sensor can be used to easily build a large planar array on a PCB ( elements providing an acquisition surface of mm). The sensor is sufficiently small to be used in building arrays of any desired shape and size.
We emphasize that the proposed array is receiving, i.e., it does not transmit. The illumination of the object under test (OUT) can be realized by any desired antenna or an antenna array. To validate the performance of the proposed bias-switched radio sensor, we use an in-house UWB TEM horn antenna here [
51]. It is also possible to modify this array to include not only receiving elements but also transmitting elements thereby enabling single-sided (or back-scattering) measurements.
It is worth mentioning that a prototype of the radio sensor was also built based on a passive mixer. The advantages of the passive mixer are in its broader bandwidth and a higher 1-dB compression point. Its disadvantage is in the conversion loss, which requires an additional IF amplifier, which would make the integration and the miniaturization of the sensor more difficult. Without an additional IF amplifier, the sensor based on a passive mixer has a lower dynamic range.