A Portable Wireless Communication Platform Based on a Multi-Material Fiber Sensor for Real-Time Breath Detection
Abstract
:1. Introduction
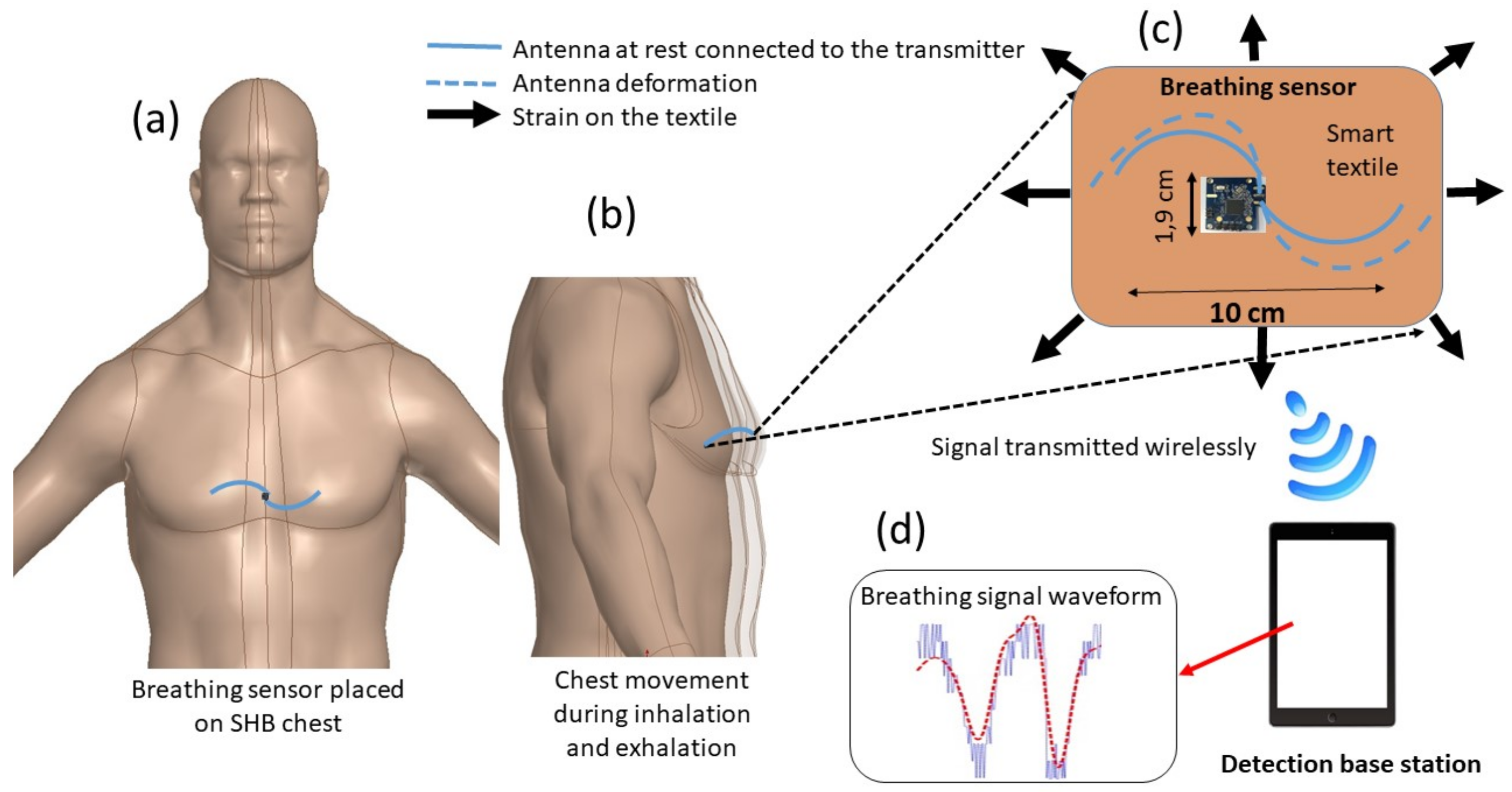
2. System Description
2.1. Fiber Antenna
2.2. Electronic System Description
3. Results and Discussion
3.1. Design and Characteristics of the Fiber Antenna
3.1.1. Sensitivity of the Fiber Antenna in Free Space
3.1.2. The Fiber Antenna’s Performance on a Simulated Human Body
3.2. Experimental Detection
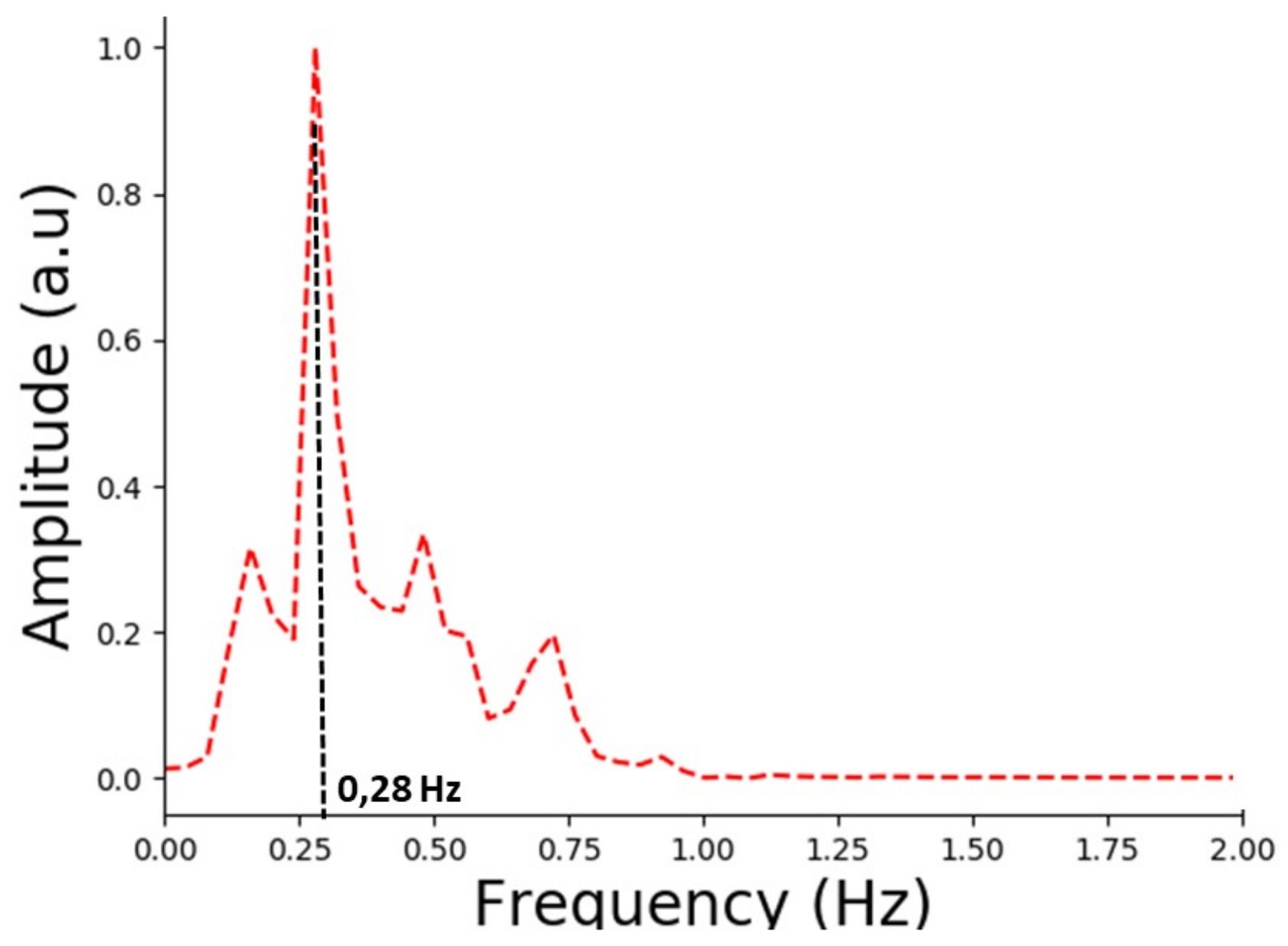
3.2.1. Breathing Rate Results
3.2.2. Detection of Different Breathing Patterns
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lumb, A.B. Physiology Of Pulmonary Disease. In Nunn’s Applied Respiratory Physiology, 8th ed.; Elsevier Health Sciences: Oxford, UK, 2016. [Google Scholar]
- Sebel, P.; Stoddart, M.; Waldhorn, R.E.; Waldman, C.; Whitfield, P. Respiration: The Breath of Life. In Human Body; Torstar Books: New York, NY, USA, 1985. [Google Scholar]
- Murray, J.F. The Basis for Diagnosis and Treatment of Pulmonary Disease. In The Normal Lung, 2nd ed.; W.B. Saunders Co.: Philadelphia, PA, USA, 1985. [Google Scholar]
- Walker, H.K.; Hall, W.D.; Willis Hurst, J. The History, Physical, and Laboratory Examinations. In Clinical Methods, 3rd ed.; Butterworths: Boston, MA, USA, 1990. [Google Scholar]
- Elliott, M. A Narrative Review: Why is Respiratory Rate the Neglected Vital Sign? Int. Arch. Nurs. Health Care 2016, 2, 50. [Google Scholar] [CrossRef]
- Flenady, T.; Dwyer, T.; Applegarth, J. Accurate respiratory rates count: So should you! Australas. Emerg. Nurs. J. 2017, 20, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Qudsi, H. Low Cost Thermistor based Respiratory Monitor. In Proceedings of the 39th Annual Northeast Bioengineering Conference, Syracuse, NY, USA, 5–7 April 2013; pp. 287–288. [Google Scholar]
- Fabiola, A.C. Respiratory Monitoring System Based on the Thoracic Expansion Measurement. Master’s Thesis, Department of Electrical Engeering, University of South Florida, Tampa, FL, USA, January 2012. [Google Scholar]
- Bello, P.J.; Darling, C.J.; Lipoma, T.S. SOMNUS: A Sleep Diagnostics Shirt Employing Respiratory Patterns Through Chest Expansion. In Proceedings of the International Conference on Design of Medical Devices, Minneapolis, MN, USA, 12–14 April 2011; pp. 1–5. [Google Scholar]
- Grlica, J.; Martinoviü, T.; DŽapo, H. Capacitive Sensor for Respiration Monitoring. In Proceedings of the 2015 IEEE Sensors Applications Symposium, Zadar, Croatia, 13–15 April 2015; pp. 1–6. [Google Scholar]
- Abbas, A.K.; Heimann, K.; Jergus, K.; Orlikowsky, T.; Leonhardt, S. Non-contact respiratory monitoring based on real-time infrared thermography. Biomed. Eng. Online 2011, 10, 93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, C.H.; Chow, C.J. Design and clinic monitoring of monitoring of a newly developed non-attached infant apnea monitor. Biomed. Eng. Appl. Basis Commun. 2005, 17, 126–134. [Google Scholar] [CrossRef]
- Zhu, Z.; Fei, J.; Pavlidis, I. Tracking Human Breath in Infrared Imaging. In Proceedings of the 5th IEEE Symposium on Bioinformatics and Bioengineering (BIBE’05), Minneapolis, MN, USA, 19–21 October 2005; pp. 227–231. [Google Scholar]
- Bartula, M.; Tigges, T.; Muehlsteff, J. Camera-based System for Contactless Monitoring of Respiration. In Proceedings of the 2013 of the 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 2672–2675. [Google Scholar]
- Tan, K.S.; Saatchi, R.; Elphick, H.; Burke, D. Real-time vision based respiration monitoring system. In Proceedings of the 2010 7th International Symposium on Communication Systems, Networks and Digital Signal Processing (CSNDSP 2010), Newcastle, UK, 21–23 July 2010; pp. 770–774. [Google Scholar]
- Fletcher, R.; Han, J. Low-cost differential front-end for doppler radar vital sign monitoring. In Proceedings of the 2009 IEEE MTT-S International Microwave Symposium Digest, Boston, MA, USA, 7–12 June 2009; pp. 1325–1328. [Google Scholar]
- Liu, L.; Liu, Z.; Barrowes, B. Through-wall bio-radiolocation with uwb impulse radar: Observation, simulation and signal extraction. IEEE J-STARS 2011, 4, 791–798. [Google Scholar] [CrossRef]
- Li, W.; Tan, B.; Piechocki, R.J. Non-Contact Breathing Detection Using Passive Radar. In Proceedings of the 2016 IEEE International Conference on Communications (ICC), Kuala Lumpur, Malaysia, 22–27 May 2016; pp. 1–6. [Google Scholar]
- Al Khalidi, F.Q.; Saatchi, R.; Burke, D.; Elphick, H. Facial tracking method for noncontact respiration rate monitoring. In Proceedings of the 2010 7th International Symposium on Communication Systems, Networks an Digital Signal Processing (CSNDSP 2010), Newcastle, UK, 21–23 July 2010; pp. 751–754. [Google Scholar]
- Al Khalidi, F.Q.; Saatchi, R.; Burke, D.; Elphick, H.; Tan, S. Respiration rate monitoring methods: A review. Pediatr. Pulmonol. 2011, 46, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Atalay, O.; Kennon, W.R.; Demirok, E. Weft-knitted strain sensor for monitoring respiratory rate and its electro-mechanical modeling. IEEE Sens. J. 2015, 15, 110–122. [Google Scholar] [CrossRef]
- Zhao, Z.; Yan, C.; Liu, Z.; Fu, X.; Peng, L.M.; Hu, Y.; Zheng, Z. Machine-Washable Textile Tribo electric Nano generators for Effective Human Respiratory Monitoring through Loom Weaving of Metallic Yarns. Adv. Mater. 2016, 28, 10267–10274. [Google Scholar] [CrossRef] [PubMed]
- Mahbub, I.; Pullano, S.A.; Wang, H.; Islam, S.K.; Fiorillo, A.S.; To, G.; Mahfouz, M.R. A Low-Power Wireless Piezoelectric Sensor-Based Respiration Monitoring System Realized in CMOS Process. IEEE Sens. J. 2017, 17, 1858–1864. [Google Scholar] [CrossRef]
- Witt, J.; Narbonneau, F.; Schukar, M.; Krebber, K.; De Jonckheere, J.; Jeanne, M.; Kinet, D.; Paquet, B.; Deprè, A.; D’Angelo, L.T.; et al. Medical Textiles With Embedded Fiber Optic Sensors for Monitoring of Respiratory Movement. IEEE Sens. J. 2012, 12, 246–254. [Google Scholar] [CrossRef]
- Ciocchetti, M.; Massaroni, C.; Saccomandi, P.; Caponero, M.A.; Polimadei, A.; Formica, D.; Schena, E. Smart Textile Based on Fiber Bragg Grating Sensors for Respiratory Monitoring: Design and Preliminary Trials. Biosensors 2015, 5, 602–615. [Google Scholar] [CrossRef] [PubMed]
- Presti, D.L.; Massaroni, C.; Formica, D.; Saccomandi, P.; Giurazza, F.; Caponero, M.A.; Schena, E. Smart Textile Based on 12 Fiber Bragg Gratings Array for Vital Signs Monitoring. IEEE Sens. J. 2017, 17, 6037–6043. [Google Scholar] [CrossRef]
- Gorgutsa, S.; Blais-Roberge, M.; Viens, J.; LaRochelle, S.; Messaddeq, Y. User-Interactive and Wireless-Communicating RF Textiles. Adv. Mater. Technol. 2016, 1, 1600032. [Google Scholar] [CrossRef]
- Gorgutsa, S.; Khalil, M.; Belanger-Garnier, V.; Viens, J.; Gosselin, B.; LaRochelle, S.; Messaddeq, Y. Emissive Properties of Wearable Wireless-Communicating Textiles Made from Multimaterial Fibers. IEEE Trans. Antennas Propag. 2016, 64, 2457–2464. [Google Scholar] [CrossRef]
- Ravichandran, R.; Saba, E.; Chen, K.-Y.; Goel, M.; Gupta, S.; Patel, S.N. WiBreathe: Estimating Respiration Rate Using Wireless Signals in Natural Settings in the Home. In Proceedings of the 2015 IEEE International Conference on Pervasive Computing and Communications (PerCom), St. Louis, MO, USA, 23–27 March 2015; pp. 131–139. [Google Scholar]
- Patwari, N.; Wilson, J.; Ananthanarayanan, S.; Kasera, S.K.; Westenskow, D.R. Monitoring Breathing via Signal Strength in Wireless Networks. IEEE Trans. Mob. Comput. 2014, 13, 1774–1786. [Google Scholar] [CrossRef]
- Kaltiokallio, O.; Yigitler, H.; Jantti, R.; Patwari, N. Non-invasive respiration rate monitoring using a single COTS TX-RX pair. In Proceedings of the 13th International Symposium on Information Processing in Sensor Networks, Berlin, Germany, 15–17 April 2014; pp. 59–69. [Google Scholar]
- Kaltiokallio, O.; Yigitler, H.; Jantti, R.; Patwari, N. Catch a Breath: Non-invasive Respiration Rate Monitoring via Wireless Communication. arXiv, 2013; arXiv:1307.0084. [Google Scholar]
- Guay, P.; Gorgutsa, S.; LaRochelle, S.; Messaddeq, Y. Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile. Sensors 2017, 17, 1050. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, J.E.; Yeung, L.Y.; Yeung, D.T.; Kay, R.L.; Tomlinson, B.; Critchley, J.A.; Woo, K.S.; Bernardi, L. Impact of changes in respiratory frequency and posture on power spectral analysis of heart rate and systolic blood pressure variability in normal subjects and patients with heart failure. Clin. Sci. (Lond.) 1996, 91, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Grestyb, M.; Bronsteinb, A.; Beytsc, J. Changes in heart rate and respiration rate in patients with vestibular dysfunction following head movements which provoke dizziness. Biol. Psychol. 1996, 49, 95–108. [Google Scholar] [CrossRef]
- Shaw, J.A. Radiometry and the Friis Transmission Equation. Am. J. Phys. 2013, 81, 33–37. [Google Scholar] [CrossRef]
- Fawwaz, T.U.; Michelssen, E.; Ravaioli, U. Fondamental of Applied Electromagnetics, 6th ed.; Pearson: Hong Kong, China, 2010; pp. 33–37. [Google Scholar]
- Moore, R.K. Effects of a Surrounding Conducting Medium on Antenna Analysis. Antennas Propag. IEEE Trans. 1963, 11, 216–225. [Google Scholar] [CrossRef]
- Karacolak, T.; Hood, A.Z.; Topsakal, E. Design of a Dual-Band Implantable Antenna and Development of Skin Mimicking Gels for Continuous Glucose Monitoring. IEEE Trans. Microw. Theory Tech. 2008, 56, 1001–1008. [Google Scholar] [CrossRef]
- 3D Content Central. Human Heart. Available online: http://www.3dcontentcentral.com (accessed on 6 February 2018).
- FCC. Body Tissue Dielectric Parameters. Available online: https://www.fcc.gov/general/body-tissue-dielectric-parameters (accessed on 6 February 2018).
- Italian National Research Council. Body Tissue Dielectric Parameters. Available online: http://niremf.ifac.cnr.it/tissprop/htmlclie/htmlclie.php (accessed on 6 February 2018).
- Youn, K.A.; Wise, A.J.; DeSaix, P.; Kruse, D.H.; Poe, B.; Johnson, E.; Johnson, J.E.; Korol, O.; Betts, J.G.; Womble, M. The Respiratory System. In Anatomy and Physiology; OpenStax College: Houston, TX, USA, 2013; pp. 145–152. [Google Scholar]









| Deformation | Sensitivity (MHz/mm) |
|---|---|
| Stretching | 14.2 |
| Compressing | 11.8 |
| Bending | 10.0 |
| Folding | 14.0 |
| Volunteer | Age(years) | W (Kg) | H (cm) | BC | BF (Hz) | BR (bpm) |
|---|---|---|---|---|---|---|
| 1 | 35 | 102 | 190 | 5.5 | 0.183 | 11 |
| 2 | 38 | 95 | 185 | 4.5 | 0.150 | 9 |
| 3 | 22 | 65 | 160 | 5.0 | 0.167 | 10 |
| 4 | 31 | 88 | 185 | 6.0 | 0.200 | 12 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roudjane, M.; Bellemare-Rousseau, S.; Khalil, M.; Gorgutsa, S.; Miled, A.; Messaddeq, Y. A Portable Wireless Communication Platform Based on a Multi-Material Fiber Sensor for Real-Time Breath Detection. Sensors 2018, 18, 973. https://doi.org/10.3390/s18040973
Roudjane M, Bellemare-Rousseau S, Khalil M, Gorgutsa S, Miled A, Messaddeq Y. A Portable Wireless Communication Platform Based on a Multi-Material Fiber Sensor for Real-Time Breath Detection. Sensors. 2018; 18(4):973. https://doi.org/10.3390/s18040973
Chicago/Turabian StyleRoudjane, Mourad, Simon Bellemare-Rousseau, Mazen Khalil, Stepan Gorgutsa, Amine Miled, and Younes Messaddeq. 2018. "A Portable Wireless Communication Platform Based on a Multi-Material Fiber Sensor for Real-Time Breath Detection" Sensors 18, no. 4: 973. https://doi.org/10.3390/s18040973





