Time Domain Near Infrared Spectroscopy Device for Monitoring Muscle Oxidative Metabolism: Custom Probe and In Vivo Applications
Abstract
:1. Introduction
2. TD NIRS Data Analysis
3. TD NIRS Instrumentation
4. Instrument Characterization
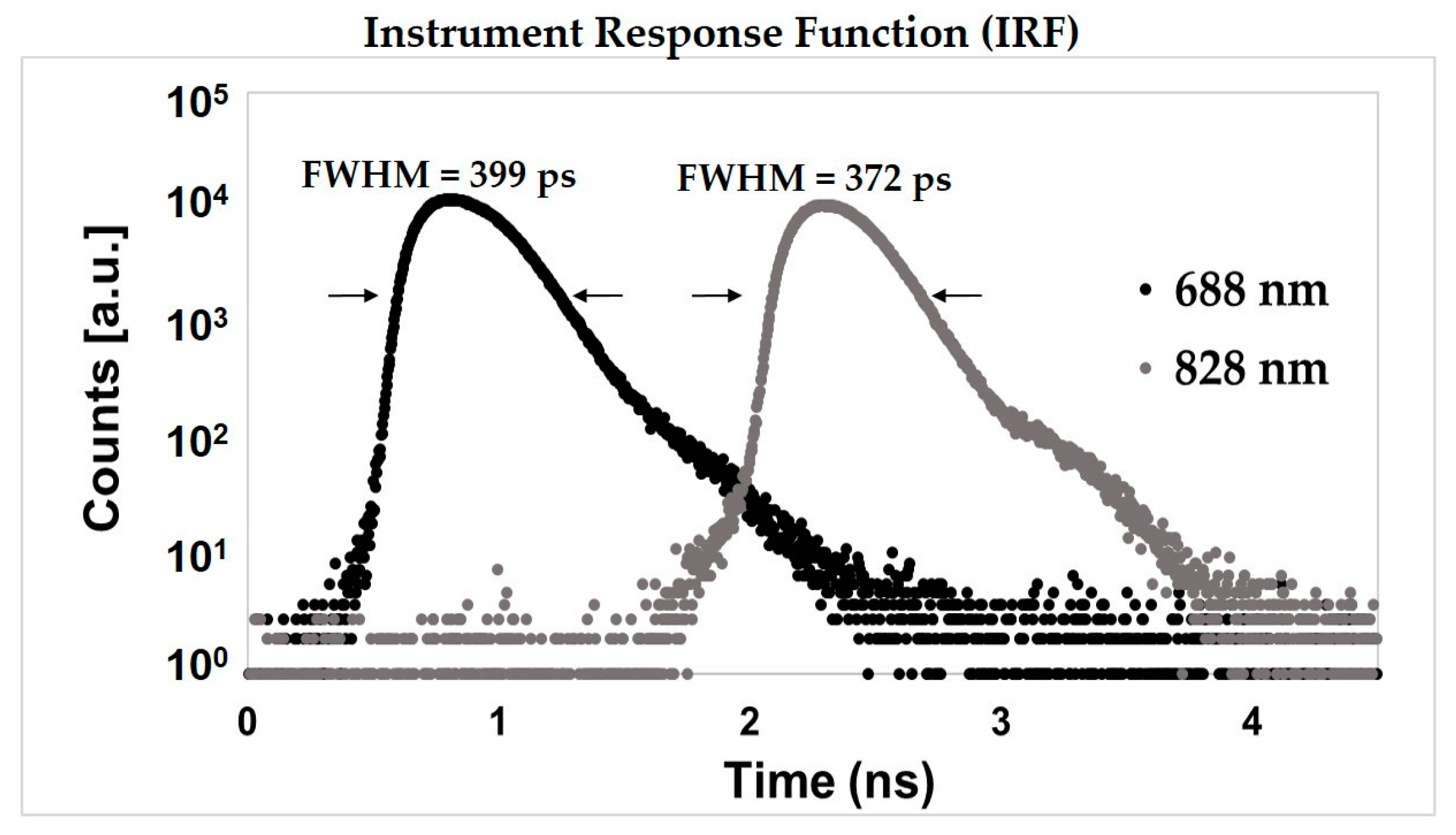
4.1. Basic IRF Characterization
4.2. Linearity on Solid Homogeneous Phantoms
4.3. Deep Absorption Changes Localization
4.4. Reproducbility and Repeatibility on Solid Homogeneous Phantom
5. In Vivo Tests
5.1. In Vivo Repeatability
5.2. Venous-Arterial Arm Occlusion
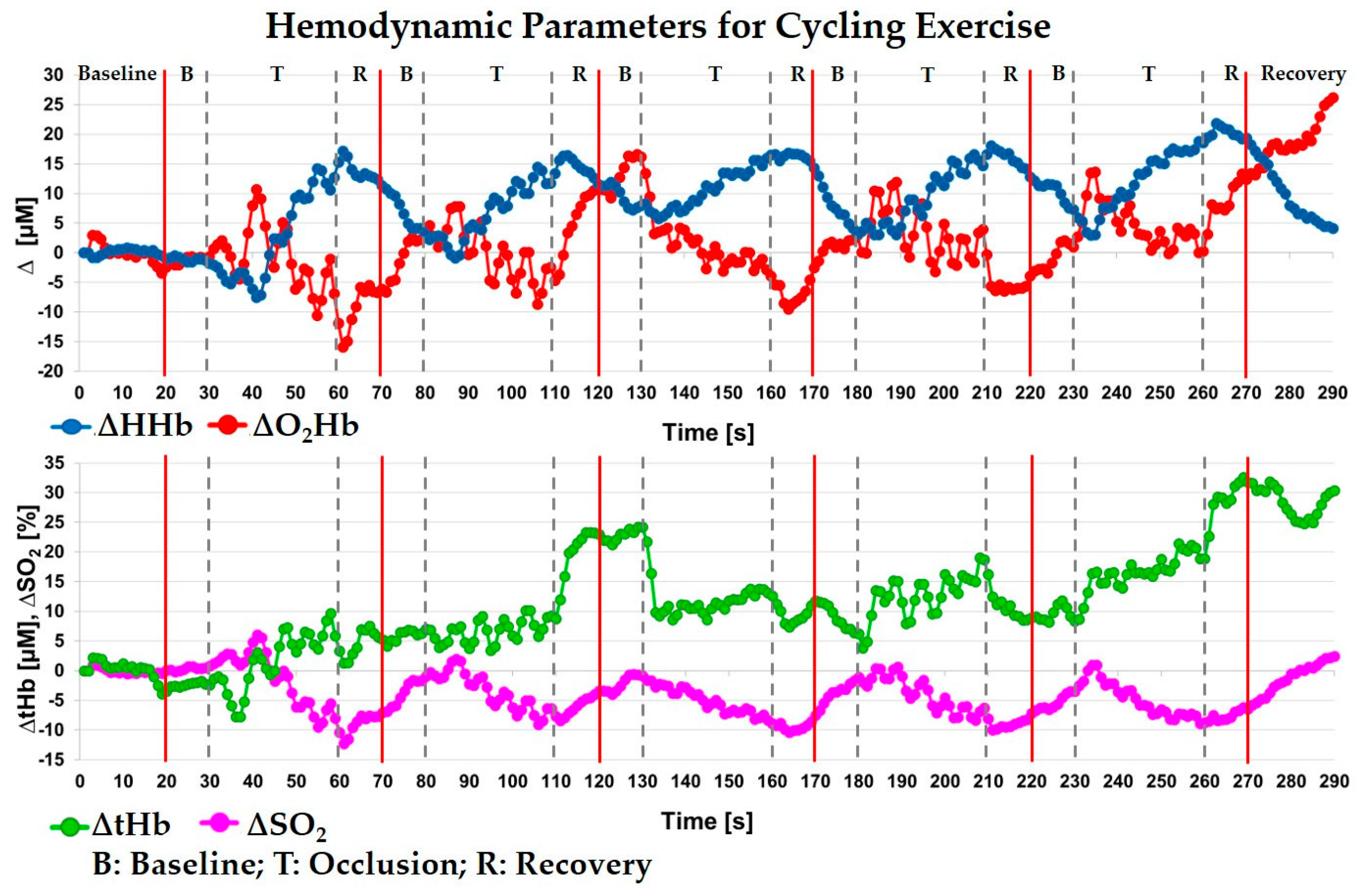
5.3. Cycling Exercise on Vastus Lateralis
5.4. Isometric Exercise on Vastus Lateralis
6. Conclusions
Author Contributions
Conflicts of Interest
References
- Russell, A.P.; Foletta, V.C.; Snow, R.J.; Wadley, G.D. Skeletal muscle mitochondria: A major player in exercise, health and disease. Biochim. Biophys. Acta 2014, 1840, 1276–1284. [Google Scholar] [CrossRef] [PubMed]
- Frontera, W.R.; Ochala, J. Skeletal Muscle: A Brief Review of Structure and Function. Calcif. Tissue Int. 2015, 96, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Willingham, T.B.; McCully, T.B. In vivo Assessment of Mitochondrial Dysfunction in Clinical Populations Using Near-Infrared Spectroscopy. Front. Physiol. 2017, 8, 689. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Quaresima, V. A brief review on the history of human functional near-infrared spectroscopy (fNIRS) development and fields of application. Neuroimage 2012, 63, 921–935. [Google Scholar] [CrossRef] [PubMed]
- Hamaoka, T.; Iwane, H.; Shimomitsu, T.; Katsumura, T.; Murase, N.; Nishio, S.; Osada, T.; Kurosawa, T.; Chance, B. Noninvasive measures of oxidative metabolism on working human muscles by near-infrared spectroscopy. J. Appl. Physiol. 1996, 81, 1410–1417. [Google Scholar] [CrossRef] [PubMed]
- Ryan, T.E.; Southern, W.M.; Brizendine, J.T.; McCully, K.K. Activity-induced changes in skeletal muscle metabolism measured with optical spectroscopy. Med. Sci. Sports Exerc. 2013, 45, 2346–2352. [Google Scholar] [CrossRef] [PubMed]
- Erickson, M.L.; Ryan, T.E.; Backus, D.; McCully, K.K. Endurance neuromuscular electrical stimulation training improves skeletal muscle oxidative capacity in individuals with motor-complete spinal cord injury. Muscle Nerve 2016, 55, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Boushel, R.; Langberg, H.; Olesen, J.; Gonzales-Alonzo, J.; Bülow, J.; Kjær, M. Monitoring tissue oxygen availability with near infrared spectroscopy (NIRS) in health and disease. Scand. J. Med. Sci. Sports 2001, 11, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Quaresima, V.; Lepanto, R.; Ferrari, M. The use of near infrared spectroscopy in sports medicine. J. Sports Med. Phys. Fit. 2003, 43, 1–13. [Google Scholar]
- Ferrari, M.; Muthalib, M.; Quaresima, V. The use of near-infrared spectroscopy in understanding skeletal muscle physiology: Recent developments. Philos. Trans. A Math. Phys. Eng. Sci. 2011, 369, 4577–4590. [Google Scholar] [CrossRef] [PubMed]
- Hamaoka, M.; Hamaoka, T.; McCully, K.K.; Niwayama, M.; Chance, B. The use of muscle near-infrared spectroscopy in sport, health and medical sciences: Recent developments. Philos. Trans. R. Soc. A 2011, 369, 4591–4604. [Google Scholar] [CrossRef] [PubMed]
- Grassi, B.; Quaresima, V. Near-infrared spectroscopy and skeletal muscle oxidative function in vivo in health and disease: A review from an exercise physiology perspective. J. Biomed. Opt. 2016, 21, 091313. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.D.; Marcinek, D.J. Evaluation of in vivo mitochondrial bioenergetics in skeletal muscle using NMR and optical methods. Biochim. Biophys. Acta 2016, 1862, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Scholkmann, F.; Kleiser, S.; Metz, A.J.; Zimmermann, R.; Pavia, J.M.; Wolf, U.; Wolf, M. A review on continuous wave functional near-infrared spectroscopy and imaging instrumentation and methodology. NeuroImage 2014, 85, 6–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, S.; Chiesa, S.T.; Chaturvedi, N.; Hughes, A.D. Recent developments in near-infrared spectroscopy (NIRS) for the assessment of local skeletal muscle microvascular function and capacity to utilise oxygen. Artery Res. 2016, 16, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Torricelli, A.; Contini, D.; Pifferi, A.; Caffini, M.; Re, R.; Zucchelli, L.; Spinelli, L. Time domain functional NIRS imaging for human brain mapping. NeuroImage 2014, 85, 28–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Contini, D.; Zucchelli, L.; Spinelli, L.; Caffini, M.; Re, R.; Pifferi, A.; Cubeddu, R.; Torricelli, A. Brain and Muscle near Infrared Spectroscopy/Imaging Techniques. JNIRS 2012, 20, 15–27. [Google Scholar] [CrossRef]
- Aletti, F.; Re, R.; Pace, V.; Contini, D.; Molteni, E.; Cerutti, S.; Bianchi, A.M.; Torricelli, A.; Spinelli, L.; Cubeddu, R.G. Deep and surface hemodynamic signal from functional time resolved transcranial near infrared spectroscopy compared to skin flowmotion. Comput. Biol. Med. 2012, 42, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Torricelli, A.; Quaresima, V.; Pifferi, A.; Biscotti, G.; Spinelli, L.; Taroni, P.; Ferrari, M.; Cubeddu, R. Mapping of calf muscle oxygenation and haemoglobin content during dynamic plantar flexion exercise by multi-channel time-resolved near-infrared spectroscopy. Phys. Med. Biol. 2004, 49, 685. [Google Scholar] [CrossRef] [PubMed]
- Ferrante, S.; Contini, D.; Spinelli, L.; Pedrocchi, A.; Torricelli, A.; Molteni, F.; Ferrigno, G.; Cubeddu, R. Monitoring muscle metabolic indexes by time-domain near-infrared spectroscopy during knee flex-extension induced by functional electrical stimulation. J. Biomed. Opt. 2009, 14, 044011. [Google Scholar] [CrossRef] [PubMed]
- Koga, S.; Barstow, T.J.; Okushima, D.; Rossiter, H.B.; Kondo, N.; Ohmae, E.; Poole, D.C. Validation of a high-power, time-resolved, near-infrared spectroscopy system for measurement of superficial and deep muscle deoxygenation during exercise. J. Appl. Physiol. 2015, 118, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, G.; Leu, S.Y.; Cerussi, A.; Tromberg, B.; Cooper, D.M.; Galassetti, P. Cerebral and muscle tissue oxygenation during incremental cycling in male adolescents measured by time-resolved near-infrared spectroscopy. Pediatr. Exerc. Sci. 2016, 28, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Okushima, D.; Poole, D.C.; Rossiter, H.B.; Barstow, T.J.; Kondo, N.; Ohmae, E.; Koga, S. Muscle deoxygenation in the quadriceps during ramp incremental cycling: Deep versus superficial heterogeneity. J. Appl. Physiol. 2015, 119, 1313–1319. [Google Scholar] [CrossRef] [PubMed]
- Contini, D.; Martelli, F.; Zaccanti, G. Photon migration through a turbid slab described by a model based on diffusion approximation. I. Theory Appl. Opt. 1997, 36, 4587–4599. [Google Scholar] [CrossRef] [PubMed]
- Oregon Medical Laser Center, Optical Properties Spectra. Available online: http://omlc.org/spectra (accessed on 3 October 2016).
- Zucchelli, L.; Contini, D.; Re, R.; Torricelli, A.; Spinelli, L. Method for the discrimination of superficial and deep absorption variations by time domain fNIRS. Biomed. Opt. Express 2013, 4, 2893–2910. [Google Scholar] [CrossRef] [PubMed]
- Re, R.; Contini, D.; Zucchelli, L.; Torricelli, A.; Spinelli, L. Effect of a thin superficial layer on the estimate of hemodynamic changes in a two-layer medium by time domain NIRS. Biomed. Opt. Express 2016, 7, 264–278. [Google Scholar] [CrossRef] [PubMed]
- Re, R.; Contini, D.; Caffini, M.; Cubeddu, R.; Spinelli, L.; Torricelli, A. A compact time-resolved system for near infrared spectroscopy based on wavelength space multiplexing. Rev. Sci. Instrum. 2010, 81, 113101:1–113101:8. [Google Scholar] [CrossRef] [PubMed]
- Re, R.; Contini, D.; Turola, M.; Spinelli, L.; Zucchelli, L.; Caffini, M.; Cubeddu, R.; Torricelli, A. Multi-channel medical device for time domain functional near infrared spectroscopy based on wavelength space multiplexing. Biomed. Opt. Express 2013, 4, 2232–2246. [Google Scholar] [CrossRef] [PubMed]
- International Electrotechnical Commision. IEC 60825–1:2007, 2nd ed.; Safety of Laser Products—Part 1: Equipment Classification and Requirements; International Electrotechnical Commision: Geneva, Switzerland, 2007. [Google Scholar]
- Pifferi, A.; Torricelli, A.; Bassi, A.; Taroni, P.; Cubeddu, R.; Wabnitz, H.; Grosenick, D.; Möller, M.; Macdonald, R.; Swartling, J.; et al. Performance assessment of photon migration instruments: The MEDPHOT protocol. Appl. Opt. 2005, 44, 2104–2114. [Google Scholar] [CrossRef] [PubMed]
- Torricelli, A.; Spinelli, L.; Kaethner, J.; Selbeck, J.; Franceschini, A.; Rozzi, P.; Zude, M. Non-destructive optical assessment of photon path lengths in fruit during ripening: Implications on design of continuous-wave sensors. In Proceedings of the CIGR-AgEng 2012, International Conference of Agricultural Engineering, Valencia, Spain, 8–12 July 2012; ISBN 10-84-615-9928-4. [Google Scholar]
- Martelli, F.; Ninni, P.D.; Zaccanti, G.; Contini, D.; Spinelli, L.; Torricelli, A.; Cubeddu, R.; Wabnitz, H.; Mazurenka, M.; Macdonald, R.; et al. Phantoms for diffuse optical imaging based on totally absorbing objects, part 2: Experimental implementation. J. Biomed. Opt. 2014, 19, 76011:1–76011:10. [Google Scholar] [CrossRef] [PubMed]
- Pifferi, A.; Torricelli, A.; Cubeddu, R.; Quarto, G.; Re, R.; Sekar, S.K.V.; Spinelli, L.; Farina, A.; Martelli, F.; Wabnitz, H. Mechanically switchable solid inhomogeneous phantom for performance tests in diffuse imaging and spectroscopy. J. Biomed. Opt. 2015, 20, 121304:1–121304:10. [Google Scholar] [CrossRef] [PubMed]
- Wabnitz, H.; Jelzow, A.; Mazurenka, M.; Steinkellner, O.; Macdonald, R.; Milej, D.; Zołek, N.; Kacprzak, M.; Sawosz, P.; Maniewski, R.; et al. Performance assessment of time-domain optical brain imagers, part 2: nEUROPt protocol. J. Biomed. Opt. 2014, 19, 086012:1–086012:12. [Google Scholar] [CrossRef] [PubMed]
- Grassi, B.; Pogliaghi, S.; Rampichini, S.; Quaresima, V.; Ferrari, M.; Marconi, C.; Cerretelli, P. Muscle oxygenation and pulmonary gas exchange kinetics during cycling exercise on-transitions in humans. J. Appl. Physiol. 2003, 95, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Sako, T.; Hamaoka, T.; Higuchi, H.; Kurosawa, Y.; Katsumura, T. Validity of NIR spectroscopy for quantitatively measuring muscle oxidative metabolic rate in exercise. J. Appl. Physiol. 2001, 90, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Dumanoir, G.R.; Delorey, D.S.; Kowalchuk, J.M.; Paterson, D.H. Kinetics of VO2 limb blood flow and regional muscle deoxygenation in young adults durting moderate intensity, knee-extension exercise. Eur. J. Appl. Physiol. 2010, 108, 607–617. [Google Scholar] [CrossRef] [PubMed]
- Re, R.; Martinenghi, E.; Dalla Mora, A.; Contini, D.; Pifferi, A.; Torricelli, A. Probe-hosted silicon photomultipliers for time-domain functional nearinfrared spectroscopy: phantom and in vivo tests. Neurophptonics. 2016, 3, 045004. [Google Scholar] [CrossRef] [PubMed]






© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Re, R.; Pirovano, I.; Contini, D.; Spinelli, L.; Torricelli, A. Time Domain Near Infrared Spectroscopy Device for Monitoring Muscle Oxidative Metabolism: Custom Probe and In Vivo Applications. Sensors 2018, 18, 264. https://doi.org/10.3390/s18010264
Re R, Pirovano I, Contini D, Spinelli L, Torricelli A. Time Domain Near Infrared Spectroscopy Device for Monitoring Muscle Oxidative Metabolism: Custom Probe and In Vivo Applications. Sensors. 2018; 18(1):264. https://doi.org/10.3390/s18010264
Chicago/Turabian StyleRe, Rebecca, Ileana Pirovano, Davide Contini, Lorenzo Spinelli, and Alessandro Torricelli. 2018. "Time Domain Near Infrared Spectroscopy Device for Monitoring Muscle Oxidative Metabolism: Custom Probe and In Vivo Applications" Sensors 18, no. 1: 264. https://doi.org/10.3390/s18010264





