Applications Based on Service-Oriented Architecture (SOA) in the Field of Home Healthcare
Abstract
:1. Introduction
2. Methods
2.1. Literature Search
2.2. Selection Criteria
3. Service Oriented Architecture: SOA
- Operations: Units of functions operating on received data, having specific interfaces and returning structured responses.
- Services: Logical groupings of operations.
- Business processes: Actions or activities to perform specific business goals by invoking multiple services.
- Infrastructure services: Includes security, management and monitoring.
- Business-neutral services: Includes service brokers and notification, scheduling and workflow services.
- Business services: Includes services based on the business logic.
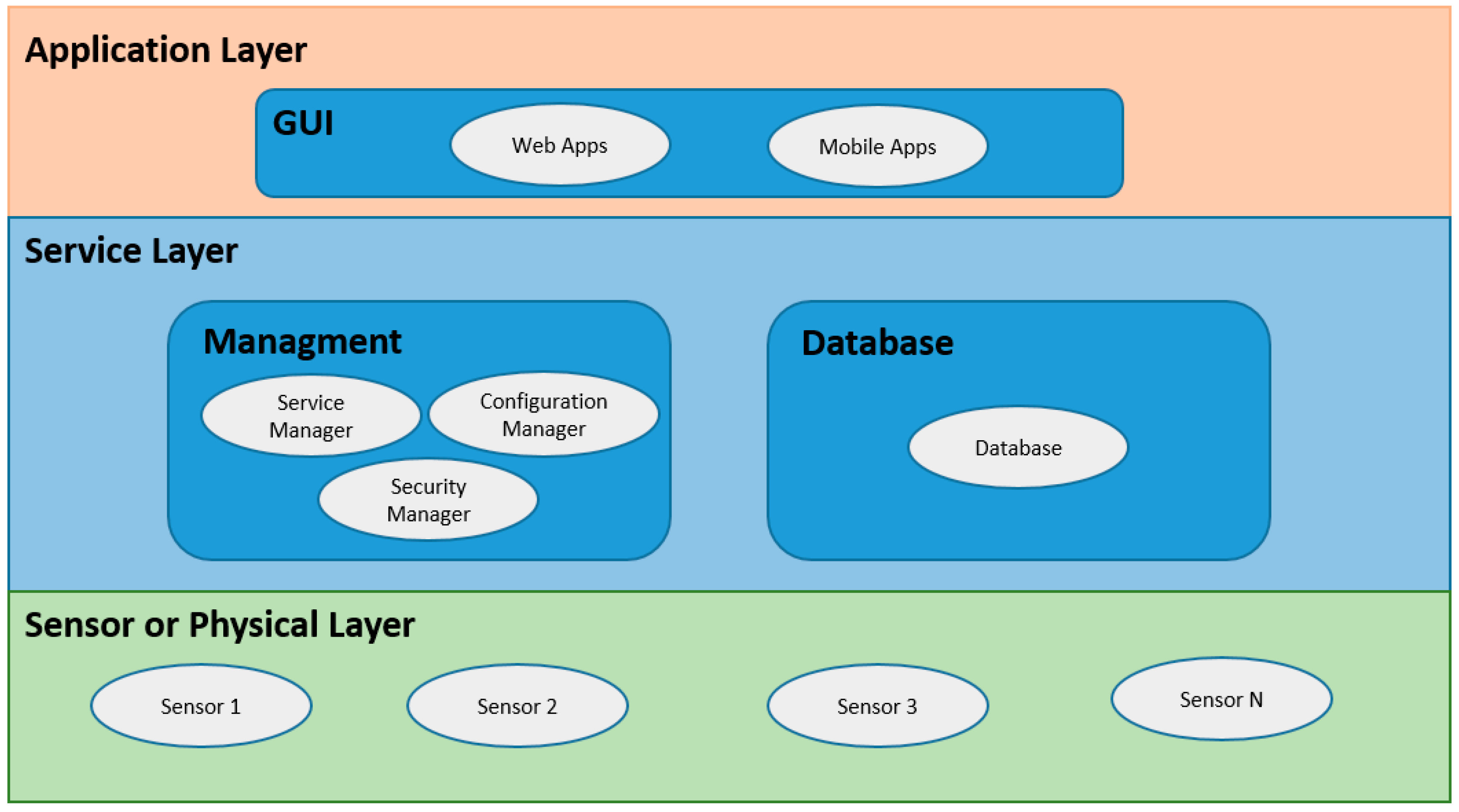
- Layer 1: Operational systems layer; this layer integrates existing systems using SOA integration techniques.
- Layer 2: Enterprise components layer is responsible for realizing functionality and maintaining the quality of service (QoS) of the exposed services.
- Layer 3: Services layer; in this layer, the services selected to be consumed are located.
- Layer 4: Business processes layer, which defines the services exposed in layer 3.
- Layer 5: Access layer; it is created to provide end-to-end solutions to compositions of services.
- Layer 6: Integration layer; it allows the integration of different services.
- Layer 7: Management and security; it is responsible to monitor, manage and maintain security.
Security in SOA Applications
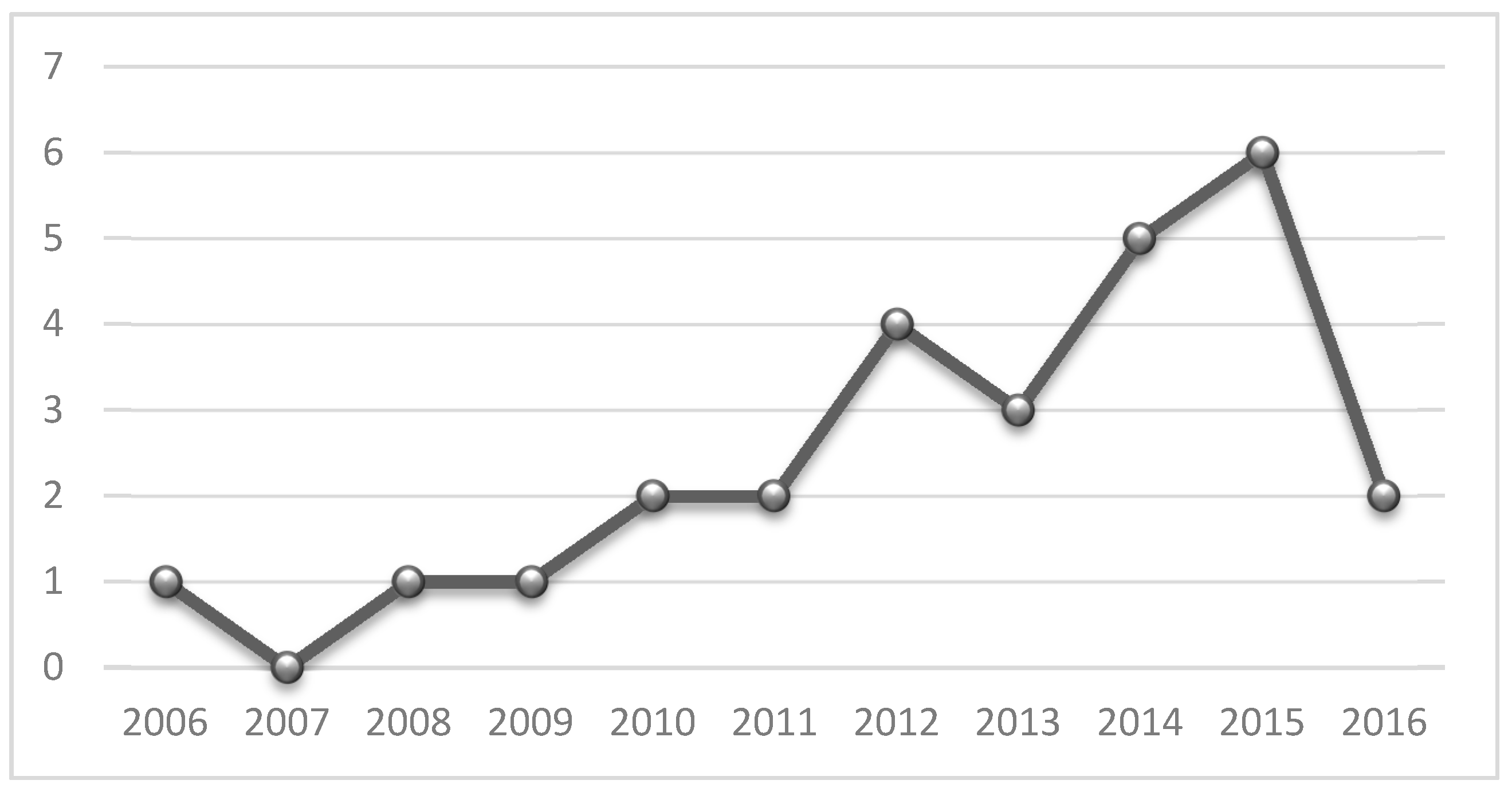
4. Revised SOA Applications
4.1. SOA Application in Healthcare Industry
4.2. SOA Applications in Home Healthcare
5. Analysis from the Perspective of Implemented Functionalities
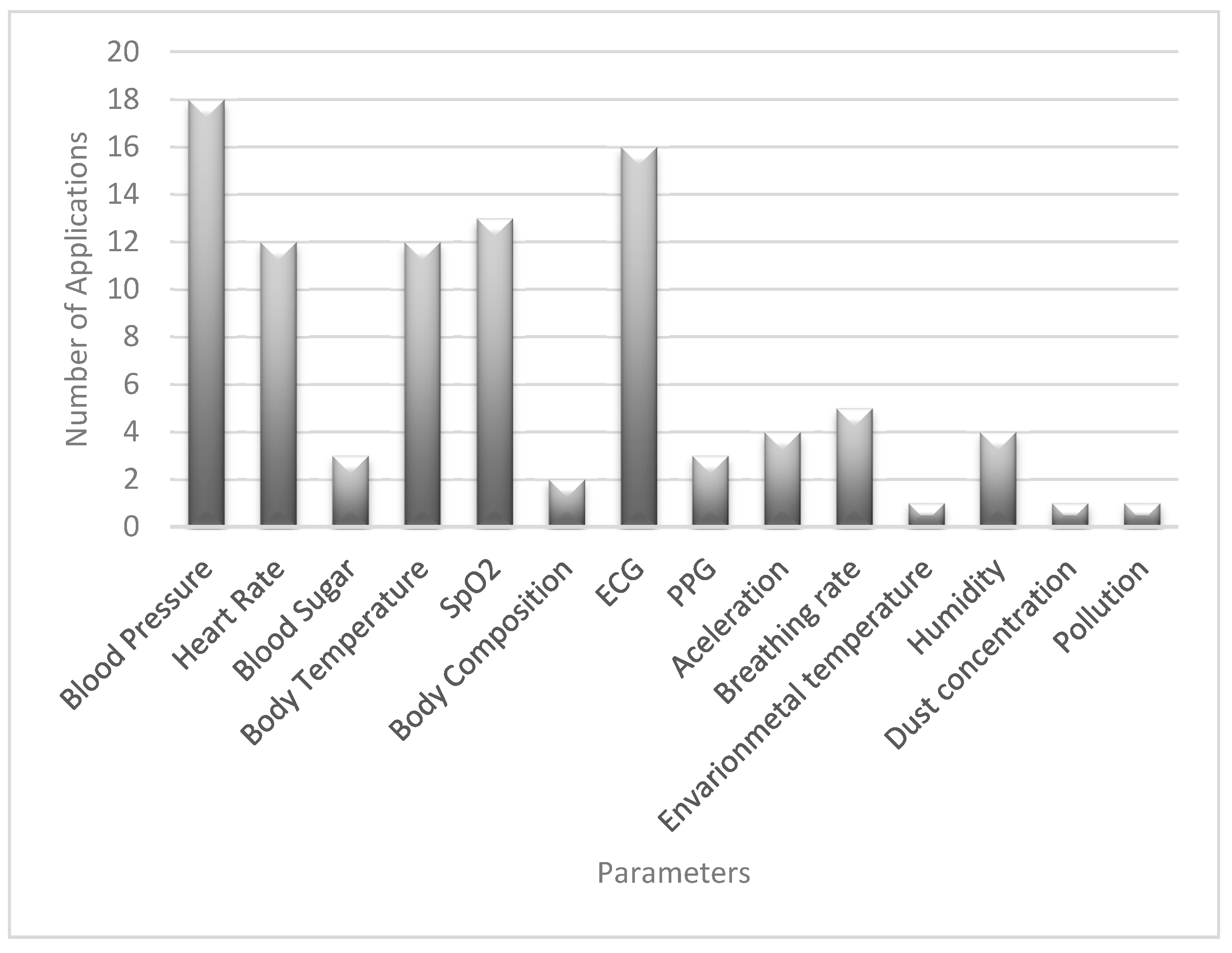
5.1. Measured Variables
- Blood pressure: Pressure of the blood on the walls of the arteries as the heart pumps it around the body.
- Heart rate: Speed of the heartbeat.
- Blood sugar: Sugar concentration in the blood.
- Body temperature.
- SpO2: Oxygen saturation in the blood.
- Body composition: Related to fat, weight, and muscle mass.
- Electrocardiogram (ECG): Reading of electrical activity of the heart.
- Photoplethysmograph PPG: It is used to estimate blood flow to the skin using infrared light [53].
- Breathing rate: Number of breaths per minute.
- Acceleration: Used to detect body movements; it helps to detect abnormal behavior.
- Environmental temperature.
- Humidity.
- Dust concentration.
- Pollution.
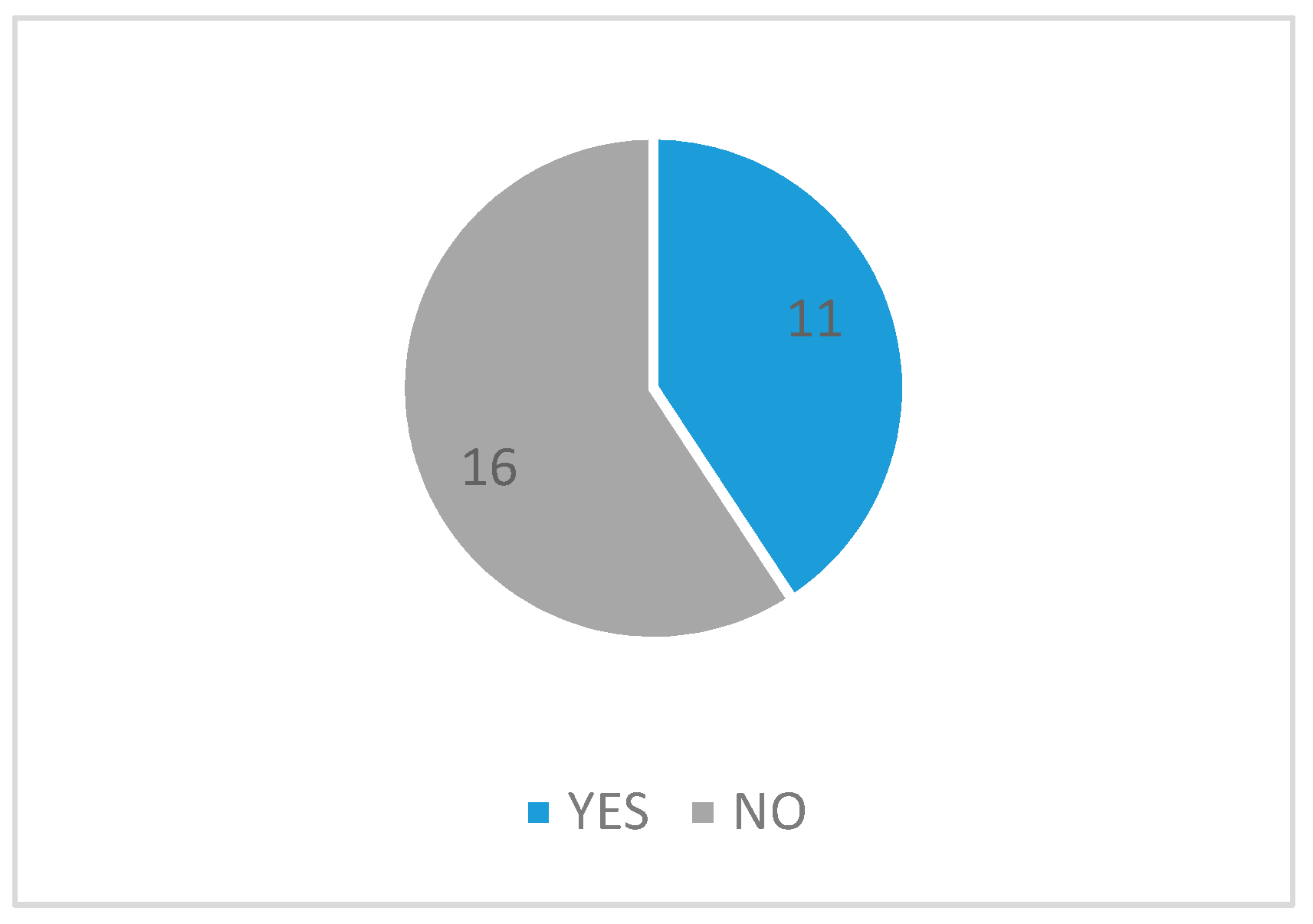
5.2. Semantic Interoperability
6. Analysis from the Perspective of Security Implementations
7. Conclusions
Conflicts of Interest
References
- Albrecht, K.; Michael, K. Connected: To everyone and everything [Guest Editorial: Special section on sensors]. IEEE Technol. Soc. Mag. 2013, 32, 31–34. [Google Scholar] [CrossRef]
- Pang, Z. Technologies and Architectures of the Internet-of-Things (IoT) for Health and Well-Being; Royal Institute of Technology: Stockholm, Sweden, 2013. [Google Scholar]
- Vaidehi, V.; Bhargavi, R.; Ganapathy, K.; Hemalatha, C.S. Multi-sensor based in-home health monitoring using complex event processing. In Proceedings of the 2012 International Conference on Recent Trends in Information Technology (ICRTIT), Chennai, India, 19–21 April 2012; pp. 570–575. [Google Scholar]
- Alshinina, R.; Elleithy, K. Performance and challenges of service-oriented architecture for wireless sensor networks. Sensors 2017, 17, 536. [Google Scholar] [CrossRef] [PubMed]
- Negra, R.; Jemili, I.; Belghith, A. Wireless body area networks: Applications and technologies. Procedia Comput. Sci. 2016, 83, 1274–1281. [Google Scholar] [CrossRef]
- Ganapathy, K.; Vaidehi, V. Medical intelligence for quality improvement in service oriented architecture. In Proceedings of the 2011 International Conference on Recent Trends in Information Technology (ICRTIT), Chennai, India, 3–5 June 2011; pp. 161–166. [Google Scholar]
- Liegl, P. The Strategic Impact of Service Oriented Architectures. In Proceedings of the 14th Annual IEEE International Conference and Workshops on the Engineering of Computer-Based Systems (ECBS’07), Tucson, AZ, USA, 26–29 March 2007; pp. 475–484. [Google Scholar]
- Tsai, W.-T.; Fan, C.; Chen, Y.; Paul, R.A.; Chung, J.-Y. Architecture Classification for SOA-Based Applications. In Proceedings of the Ninth IEEE International Symposium on Object and Component-Oriented Real-Time Distributed Computing (ISORC’06), Gyeongju, Korea, 24–26 April 2006; pp. 1–8. [Google Scholar]
- Karnouskos, S.; Guinard, D.; Savio, D.; Spiess, P.; Baecker, O.; Trifa, V.; de Souza, L.M.S. Towards the real-time enterprise: Service-based integration of heterogeneous SOA-ready industrial devices with enterprise applications. IFAC Proc. Vol. 2009, 42, 2131–2136. [Google Scholar] [CrossRef]
- Gao, F.; Li, L. Study on Security of Information Exchange of SOA Application System. In Applied Mechanics and Materials; Trans Tech Publications Inc.: Bern, Switzerland, 2014; Volumes 484–485, pp. 860–865. [Google Scholar]
- Caporuscio, M.; Mirandola, R.; Trubiani, C. QoS-Based Feedback for Service Compositions. In Proceedings of the 2015 11th International ACM SIGSOFT Conference on Quality of Software Architectures (QoSA), Montreal, QC, Canada, 4–8 May 2015; pp. 37–42. [Google Scholar]
- Ati, M.; Omar, W.; Hussain, A. Knowledge Based System Framework for Managing Chronic Diseases Based on Service Oriented Architecture. In Proceedings of the 2012 8th International Conference on Information Science and Digital Content Technology (ICIDT2012), Jeju, Korea, 26–28 June 2012; pp. 20–23. [Google Scholar]
- Setareh, S.; Rezaee, A.; Farahmandian, V.; Hajinazari, P.; Asosheh, A. A Cloud-Based Model for Hospital Information Systems Integration. In Proceedings of the 2014 7th International Symposium on Telecommunications (IST), Teheran, Iran, 9–11 September 2014; pp. 695–700. [Google Scholar]
- Omar, W.M.; Taleb-Bendiab, A. Defining an Ontology for E-Health Autonomic Software Services. In Proceedings of the 2006 Innovations in Information Technology, Dubai, United Arab Emirates, 19–21 November 2006; pp. 1–5. [Google Scholar]
- Mahmood, Z. Service Oriented Architecture: Potential Benefits and Challenges. In Proceedings of the 11th WSEAS International Conference on Computers, Agios Nikolaos, Greece, 26–28 July 2007; pp. 497–501. [Google Scholar]
- Zimmermann, O.; Krogdahl, P.; Gee, C. Elements of Service-Oriented Analysis and Design; IBM DeveloperWorks: Agios Nikolaos, Greece, 2004. [Google Scholar]
- Hohpe, G. Stairway to Heaven; Software Center, The University of Gothenburg: Gothenburg, Germany, 2002. [Google Scholar]
- Arsanjani, A. Service-Oriented Modeling and Architecture. Available online: https://www.ibm.com/developerworks/library/ws-soa-design1/ (accessed on 20 July 2017).
- Boonyarattaphan, A.; Bai, Y.; Chung, S.; Poovendran, R. Spatial-Temporal Access Control for E-Health Services. In Proceedings of the 2010 IEEE Fifth International Conference on Networking, Architecture and Storage (NAS), Macau, China, 15–17 July 2010; pp. 269–276. [Google Scholar]
- Cummins, F.A. SOA Security. In Building the Agile Enterprise; Morgan Kaufmann: Burlington, MA, USA, 2009; Chapter 6; pp. 155–185. [Google Scholar]
- Rafe, V.; Hosseinpouri, R. A security framework for developing service-oriented software architectures. Secur. Commun. Netw. 2015, 8, 2957–2972. [Google Scholar] [CrossRef]
- Zhang, L.; Zhu, S.; Tang, S. Privacy protection for telecare medicine information systems using a chaotic map-based three-factor authenticated key agreement scheme. IEEE J. Biomed. Health Inform. 2017, 21, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.D.; Gummadikayala, R.; Mudumbi, S. A Web-Based Wireless Mobile System Design of Security and Privacy Framework for U-Healthcare. In Proceedings of the 10th International Conference on E-Health Networking, Applications and Services (HealthCom 2008), Singapore, 7–9 July 2008; pp. 96–101. [Google Scholar]
- Kart, F.; Moser, L.E.; Melliar-Smith, P.M. Building a distributed e-healthcare system using SOA. IT Prof. 2008, 10, 24–30. [Google Scholar] [CrossRef]
- Shen, H.; Ma, D.; Zhao, Y.; Ye, R. Collaborative Annotation of Medical Images via Web Browser for Teleradiology. In Proceedings of the 2012 International Conference on Computerized Healthcare (ICCH), Hong Kong, China, 17–18 December 2012; pp. 127–133. [Google Scholar]
- Miori, V.; Russo, D. Anticipating Health Hazards Through an Ontology-Based, IoT Domotic Environment. In Proceedings of the 2012 Sixth International Conference on Innovative Mobile and Internet Services in Ubiquitous Computing (IMIS), Palermo, Itay, 4–6 July 2012; pp. 745–750. [Google Scholar]
- Trinugroho, Y.B.D.; Reichert, F.; Fensli, R.W. A SOA-Based Health Service Platform in Smart Home Environment. In Proceedings of the 2011 13th IEEE International Conference on E-Health Networking Applications and Services (Healthcom), Columbia, MO, USA, 13–15 June 2011; pp. 201–204. [Google Scholar]
- Omar, W.M.; Taleb-Bendiab, A. Service Oriented Architecture for E-Health Support Services Based on Grid Computing Over. In Proceedings of the 2006 IEEE International Conference on Services Computing (SCC’06), Chicago, IL, USA, 18–22 September 2006; pp. 135–142. [Google Scholar]
- Lee, S.H.; Song, J.H.; Ye, J.H.; Lee, H.J.; Yi, B.K.; Kim, I.K. SOA-Based Integrated Pervasive Personal Health Management System Using PHDs. In Proceedings of the 2010 4th International Conference on Pervasive Computing Technologies for Healthcare, Munich, Germany, 22–25 March 2010; pp. 1–4. [Google Scholar]
- Hein, A.; Eichelberg, M.; Nee, O.; Schulz, A.; Helmer, A.; Lipprandt, M. A Service Oriented Platform for Health Services and Ambient Assisted Living. In Proceedings of the International Conference on Advanced Information Networking and Applications Workshops (WAINA’09), Bradford, UK, 26–29 May 2009; pp. 531–537. [Google Scholar]
- Koutkias, V.G.; Chouvarda, I.; Triantafyllidis, A.; Malousi, A.; Giaglis, G.D.; Maglaveras, N. A personalized framework for medication treatment management in chronic care. IEEE Trans. Inform. Technol. Biomed. 2010, 14, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Rao, I.H.; Amir, N.A.; Dagale, H.; Kuri, J. E-Surakshak: A Cyber-Physical Healthcare System with Service Oriented Architecture. In Proceedings of the 2012 International Symposium on Electronic System Design (ISED), Kolkata, India, 19–22 December 2012; pp. 177–182. [Google Scholar]
- Rocha, A.; Martins, A.; Freire Junior, J.C.; Kamel Boulos, M.N.; Vicente, M.E.; Feld, R.; van de Ven, P.; Nelson, J.; Bourke, A.; ÓLaighin, G.; et al. Innovations in health care services: The CAALYX system. Int. J. Med. Inform. 2013, 82, e307–e320. [Google Scholar] [CrossRef] [PubMed]
- Benharref, A.; Serhani, M.A. Novel cloud and SOA-based framework for e-health monitoring using wireless biosensors. IEEE J. Biomed. Health Inform. 2014, 18, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Gazzarata, R.; Vergari, F.; Cinotti, T.S.; Giacomini, M. A standardized SOA for clinical data interchange in a cardiac telemonitoring environment. IEEE J. Biomed. Health Inform. 2014, 18, 1764–1774. [Google Scholar] [CrossRef] [PubMed]
- Yeh, K.-H. Bsncare+: A robust IoT-oriented healthcare system with non-repudiation transactions. Appl. Sci. 2016, 6, 418. [Google Scholar] [CrossRef]
- Gope, P.; Hwang, T. Bsn-care: A secure IoT-based modern healthcare system using body sensor network. IEEE Sens. J. 2016, 16, 1368–1376. [Google Scholar] [CrossRef]
- Fortino, G.; Gravina, R.; Russo, W. Activity-Aaservice: Cloud-Assisted, BSN-Based System for Physical Activity Monitoring. In Proceedings of the 2015 IEEE 19th International Conference on Computer Supported Cooperative Work in Design (CSCWD), Calabria, Italy, 6–8 May 2015; pp. 588–593. [Google Scholar]
- MengChu, Z.; Han-Xiong, L.; Margot, W. Accelerometer-based Body Sensor Network (BSN) for Medical Diagnosis Assessment and Training. In Contemporary Issues in Systems Science and Engineering; Wiley-IEEE Press: Hoboken, NJ, USA, 2015; pp. 1–888. [Google Scholar]
- Tan, B.; Tian, O. Short Paper: Using BSN for Tele-Health Application in Upper Limb Rehabilitation. In Proceedings of the 2014 IEEE World Forum on Internet of Things (WF-IoT), Seoul, Korea, 6–8 March 2014; pp. 169–170. [Google Scholar]
- Kañtoch, E. Technical Verification of Integrating Wearable Sensors into BSN-Based Telemedical Monitoring System. In Proceedings of the 2013 12th International Conference on Machine Learning and Applications, Miami, FL, USA, 4–7 December 2013; pp. 432–435. [Google Scholar]
- Kańtoch, E. Telemedical Human Activity Monitoring System Based on Wearable Sensors Network. In Proceedings of the Computing in Cardiology 2014, Cambridge, MA, USA, 7–10 September 2014; pp. 469–472. [Google Scholar]
- Nandkishor, B.R.; Shinde, A.; Malathi, P. Android Smartphone Based Body Area Network for Monitoring and Evaluation of Medical Parameters. In Proceedings of the 2014 First International Conference on Networks & Soft Computing (ICNSC2014), Guntur, India, 19–20 August 2014; pp. 284–288. [Google Scholar]
- Andrès, E.; Talha, S.; Ahmed Benyahia, A.; Keller, O.; Hajjam, M.; Moukadem, A.; Dieterlen, A.; Hajjam, J.; Ervé, S.; Hajjam, A. E-health: A promising solution for optimizing management of chronic diseases. Example of the national e-health project e-care based on an e-platform in the context of chronic heart failure. Eur. Res. Telemed. 2015, 4, 87–94. [Google Scholar] [CrossRef]
- Singh, S.R.; Jayasuriya, J.; Zhou, C.; Motani, M. A Restful Web Networking Framework for Vital Sign Monitoring. In Proceedings of the 2015 IEEE International Conference on Communications (ICC), London, UK, 8–12 June 2015; pp. 524–529. [Google Scholar]
- Chen, I.Y.; Tsai, C.H. Pervasive Digital Monitoring and Transmission of Pre-Care Patient Biostatics with An OSGI, MOM and SOA Based Remote Health Care System. In Proceedings of the Sixth Annual IEEE International Conference on Pervasive Computing and Communications (PerCom 2008), Hong Kong, China, 17–21 March 2008; pp. 704–709. [Google Scholar]
- Hofer, T.; Schumacher, M.; Bromuri, S. Compass: An Interoperable Personal Health System to Monitor and Compress Signals in Chronic Obstructive Pulmonary Disease. In Proceedings of the 2015 9th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth), Istanbul, Turkey, 20–23 May 2015; pp. 304–311. [Google Scholar]
- Ganapathy, K.; Priya, B.; Priya, B.; Dhivya; Prashanth, V.; Vaidehi, V. SOA framework for geriatric remote health care using wireless sensor network. Procedia Comput. Sci. 2013, 19, 1012–1019. [Google Scholar] [CrossRef]
- Abousharkh, M.; Mouftah, H. XMPP-Enabled SOA-Driven Middleware for Remote Patient Monitoring System. In Proceedings of the 2012 International Conference on Information Technology and E-Services, Sousse, Tunisia, 24–26 March 2012; pp. 1–5. [Google Scholar]
- Abousharkh, M.; Mouftah, H. A SOA-Based Middleware for WBAN. In Proceedings of the 2011 IEEE International Symposium on Medical Measurements and Applications, Bari, Italy, 30–31 May 2011; pp. 257–260. [Google Scholar]
- Iancu-Constantin, R.; Serbanati, L.D.; Chera, C.; Gheorghe-Pop, I.D.; Ertl, B. An E-Health Approach for Remote Cardiac Rehabilitation. In Proceedings of the 2015 20th International Conference on Control Systems and Computer Science, Bucharest, Romania, 27–29 May 2015; pp. 205–210. [Google Scholar]
- Bazzani, M.; Conzon, D.; Scalera, A.; Spirito, M.A.; Trainito, C.I. Enabling the IoT Paradigm in E-Health Solutions through the Virtus Middleware. In Proceedings of the 2012 IEEE 11th International Conference on Trust, Security and Privacy in Computing and Communications, Liverpool, UK, 25–27 June 2012; pp. 1954–1959. [Google Scholar]
- Elgendi, M. On the analysis of fingertip photoplethysmogram signals. Curr. Cardiol. Rev. 2012, 8, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Meo, P.D.; Quattrone, G.; Ursino, D. Integration of the HL7 standard in a multiagent system to support personalized access to e-health services. IEEE Trans. Knowl. Data Eng. 2011, 23, 1244–1260. [Google Scholar] [CrossRef]
- Batra, U.; Sachdeva, S.; Mukherjee, S. Implementing healthcare interoperability utilizing SOA and data interchange agent. Health Policy Technol. 2015, 4, 241–255. [Google Scholar] [CrossRef]
- Kiljander, J.; D’elia, A.; Morandi, F.; Hyttinen, P.; Takalo-Mattila, J.; Ylisaukko-Oja, A.; Soininen, J.P.; Cinotti, T.S. Semantic interoperability architecture for pervasive computing and Internet of Things. IEEE Access 2014, 2, 856–873. [Google Scholar] [CrossRef]
- Jabbar, S.; Ullah, F.; Khalid, S.; Khan, M.; Han, K. Semantic interoperability in heterogeneous IoT infrastructure for healthcare. Wirel. Commun. Mob. Comput. 2017, 2017, 10. [Google Scholar] [CrossRef]
- Bui, V.; Brandt, P.; Liu, H.; Basten, T.; Johan, L. Semantic Interoperability in Body Area Sensor Networks and Applications. In Proceedings of the 9th International Conference on Body Area Networks, London, UK, 29 Septermber–1 October 2014; pp. 210–216. [Google Scholar]
- Brandt, P.; Basten, T.; Stuiik, S.; Bui, V.; Clercq, P.D.; Pires, L.F.; Sinderen, M.V. Semantic Interoperability in Sensor Applications Making Sense of Sensor Data. In Proceedings of the 2013 IEEE Symposium on Computational Intelligence in Healthcare and e-Health (CICARE), Singapore, 16–19 April 2013; pp. 34–41. [Google Scholar]
- Amato, F.; Mazzeo, A.; Moscato, V.; Picariello, A. A Framework for Semantic Interoperability over the Cloud. In Proceedings of the 2013 27th International Conference on Advanced Information Networking and Applications Workshops, Barcelona, Spain, 25–28 March 2013; pp. 1259–1264. [Google Scholar]
- Han, S.N.; Lee, G.M.; Crespi, N.; Luong, N.V.; Heo, K.; Brut, M.; Gatellier, P. Dpwsim: A devices profile for web services (DPWS) simulator. IEEE Internet Things J. 2015, 2, 221–229. [Google Scholar] [CrossRef]
- Daemen, J.; Rijmen, V. The Design of Rijndael: AES—The Advanced Encryption Standard; Springer Science & Business Media: Berlin, Germany, 2013. [Google Scholar]
| Key Words | Database | Results |
|---|---|---|
| Healthcare system using SOA | IEEE | 57 |
| Science Direct | 665 | |
| Scopus | 326 | |
| SOA and healthcare systems | IEEE | 87 |
| Science Direct | 665 | |
| Scopus | 326 | |
| Security aspects in SOA | IEEE | 89 |
| Science Direct | 1732 | |
| Scopus | 180 | |
| SOA architecture | IEEE | 4688 |
| Science Direct | 4199 | |
| Scopus | 12,985 | |
| SOA applications review | IEEE | 84 |
| Science Direct | 6366 | |
| Scopus | 162 |
| Category Sensor | Device | Parameters |
|---|---|---|
| Physiological sensor | Body scale | Body composition |
| Blood pressure monitor | Blood pressure, heart rate | |
| Pulse oximenter | SpO2, heart rate, PPG | |
| Wearable vital signal monitor | Heart rate, breathing rate, body temperature | |
| ECG | Electrical activity of the heart | |
| Environmental sensor | Accelerometer | Acceleration, body movements |
| Environmental monitor | Environmental temperature, humidity, dust concentration, pollution |
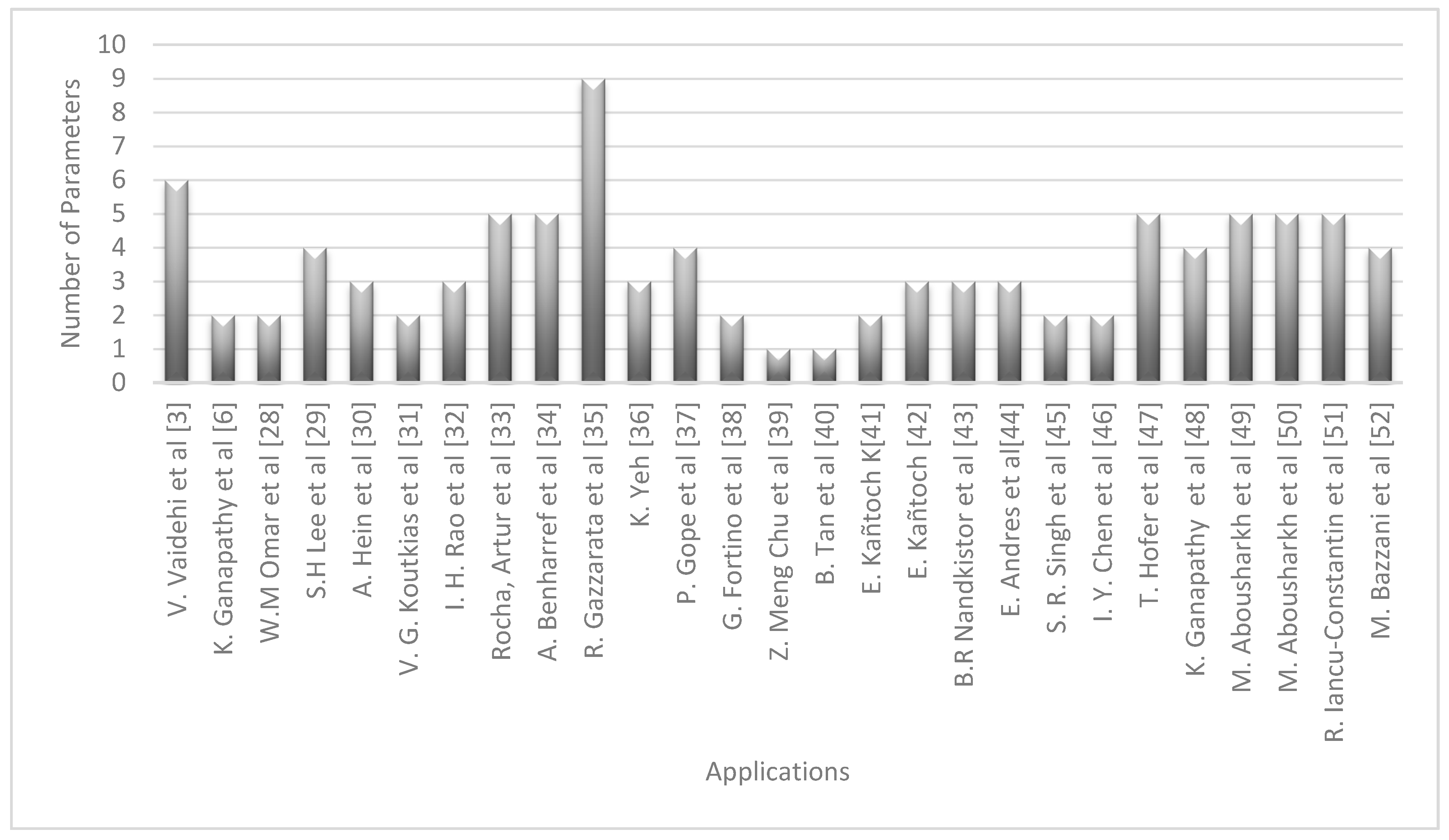
| Reference | Physiological Sensor | Environmental Sensor |
|---|---|---|
| Vaidehi et al. [3] | Blood Pressure, Heart Rate, Body Temperature, SpO2, ECG, Breathing rate | N/A |
| Ganapathy et al. [6] | Blood Pressure, Heart Rate | N/A |
| Omar et al. [28] | Blood pressure | N/A |
| Lee et al. [29] | SpO2, Body Composition, Blood Sugar, Blood pressure | N/A |
| Hein et al. [30] | Blood Pressure, SpO2, ECG | N/A |
| Koutkias et al. [31] | Blood Pressure, Heart Rate | N/A |
| Rao et al. [32] | Blood Pressure, Heart Rate, SpO2 | N/A |
| Rocha et al. [33] | Body Temperature, SpO2, ECG, PPG | Acceleration |
| Benharref et al. [34] | Blood Pressure, Heart Rate, Blood Sugar, Body Temperature, SpO2 | N/A |
| Gazzarata et al. [35] | Blood Pressure, Heart Rate, Body Temperature, SpO2, Body Composition | Environmental temperature, Humidity, Dust concentration, Pollution |
| Yeh [36] | ECG, Blood pressure, Temperature | Humidity |
| Gope et al. [37] | ECG, Blood pressure, Temperature | N/A |
| Fortino et al. [38] | ECG, PPG | N/A |
| Meng et al. [39] | N/A | Acceleration |
| Tan et al. [40] | N/A | Acceleration |
| Kañtoch [41] | ECG, PPG | N/A |
| Kañtoch [42] | ECG, Temperature | Humidity |
| Nandkistor et al. [43] | ECG, Temperature, Heart rate | N/A |
| Andres et al. [44] | ECG, Blood Pressure, SpO2 | N/A |
| Singh et al. [45] | ECG | Acceleration |
| Chen et al. [46] | Blood Pressure, ECG | N/A |
| Hofer et al. [47] | Blood Pressure, Heart Rate, Body Temperature, SpO2 | Acceleration |
| Ganapathy et al. [48] | Heart Rate, ECG, Breathing rate | Acceleration |
| Abousharkh et al. [49] | ECG, Blood Pressure, Body Temperature, SpO2, Heart Rate | N/A |
| Abousharkh et al. [50] | ECG, Blood Pressure, Body Temperature, SpO2, Heart Rate | N/A |
| Iancu-Constantin et al. [51] | ECG, Blood Pressure, SpO2, Heart Rate | Acceleration |
| Bazzani et al. [52] | Blood Pressure, Blood Sugar, Body Temperature, SpO2 | N/A |
| Reference | Type of Solution | Standards Used |
|---|---|---|
| [54] | 2 types of intermediate agents | Not defined |
| [55] | 3 types of intermediate agents | XML |
| [56] | Mid-tier agents | RDF, OWL |
| [57] | Ontology mappers | OWL |
| [58] | Semantic mediator layer | RDF, SPARQL |
| [59] | Ontology to represent concepts and data | XML |
| [60] | Ontology decoders and encoders based on cloud | XML, RDF |
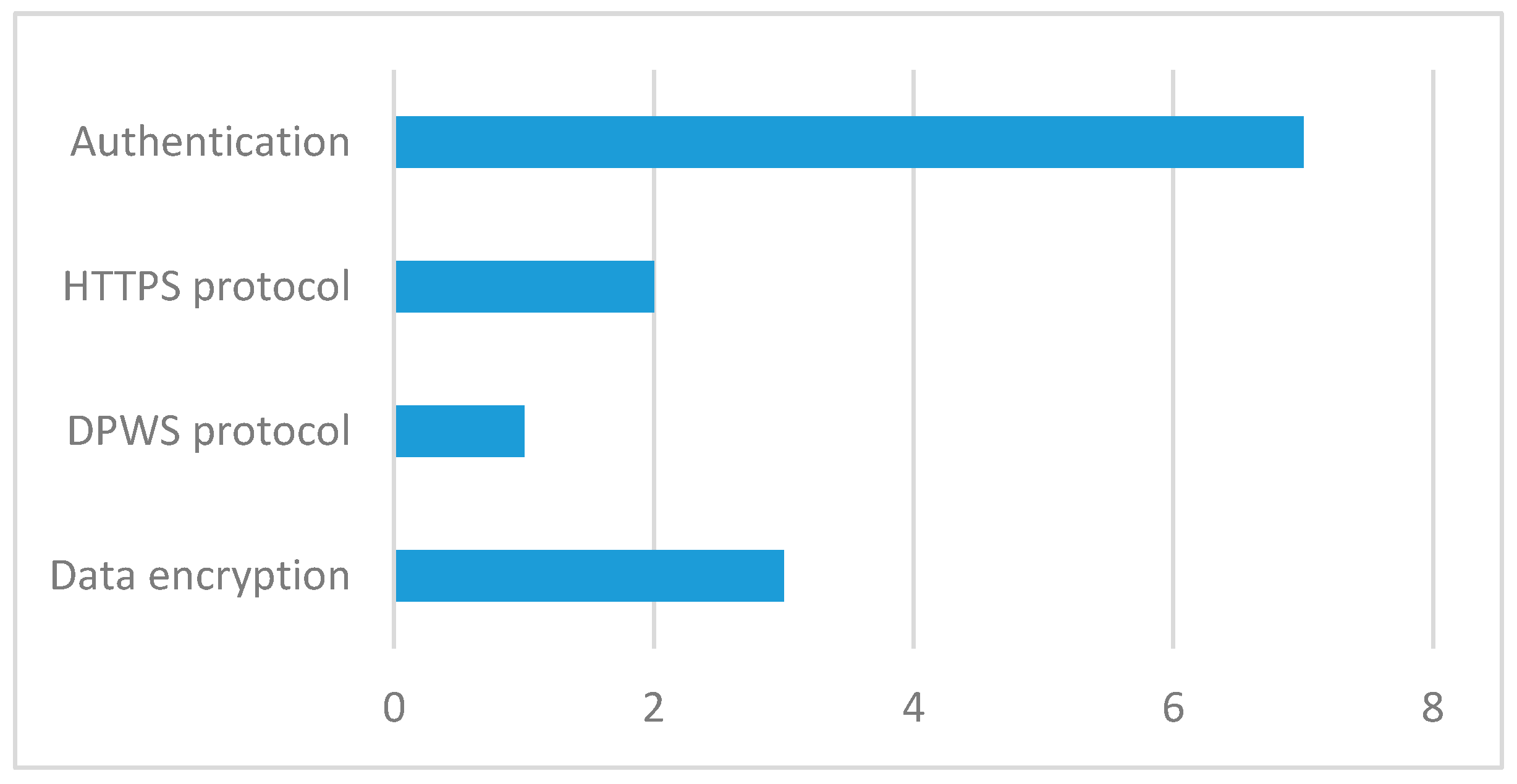
| Reference | Reference Year | How Security Was Implemented? |
|---|---|---|
| Hein et al. [30] | 2009 | Data encryption |
| Koutkias et al. [31] | 2010 | DPWS protocol |
| Benharref et al. [34] | 2014 | HTTPS |
| Gazzarata et al. [35] | 2014 | HTTPS |
| Yeh [36] | 2016 | Login |
| Gope et al. [37] | 2016 | Login |
| Hofer et al. [47] | 2015 | Login |
| Ganapathy et al. [48] | 2013 | Login |
| Abousharkh et al. [49] | 2012 | Login |
| Iancu-Constantin et al. [51] | 2015 | Data encryption, login |
| Bazzani et al. [52] | 2012 | Data encryption, login |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avila, K.; Sanmartin, P.; Jabba, D.; Jimeno, M. Applications Based on Service-Oriented Architecture (SOA) in the Field of Home Healthcare. Sensors 2017, 17, 1703. https://doi.org/10.3390/s17081703
Avila K, Sanmartin P, Jabba D, Jimeno M. Applications Based on Service-Oriented Architecture (SOA) in the Field of Home Healthcare. Sensors. 2017; 17(8):1703. https://doi.org/10.3390/s17081703
Chicago/Turabian StyleAvila, Karen, Paul Sanmartin, Daladier Jabba, and Miguel Jimeno. 2017. "Applications Based on Service-Oriented Architecture (SOA) in the Field of Home Healthcare" Sensors 17, no. 8: 1703. https://doi.org/10.3390/s17081703








