Adaptive Interference Cancellation of ECG Signals
Abstract
:1. Introduction
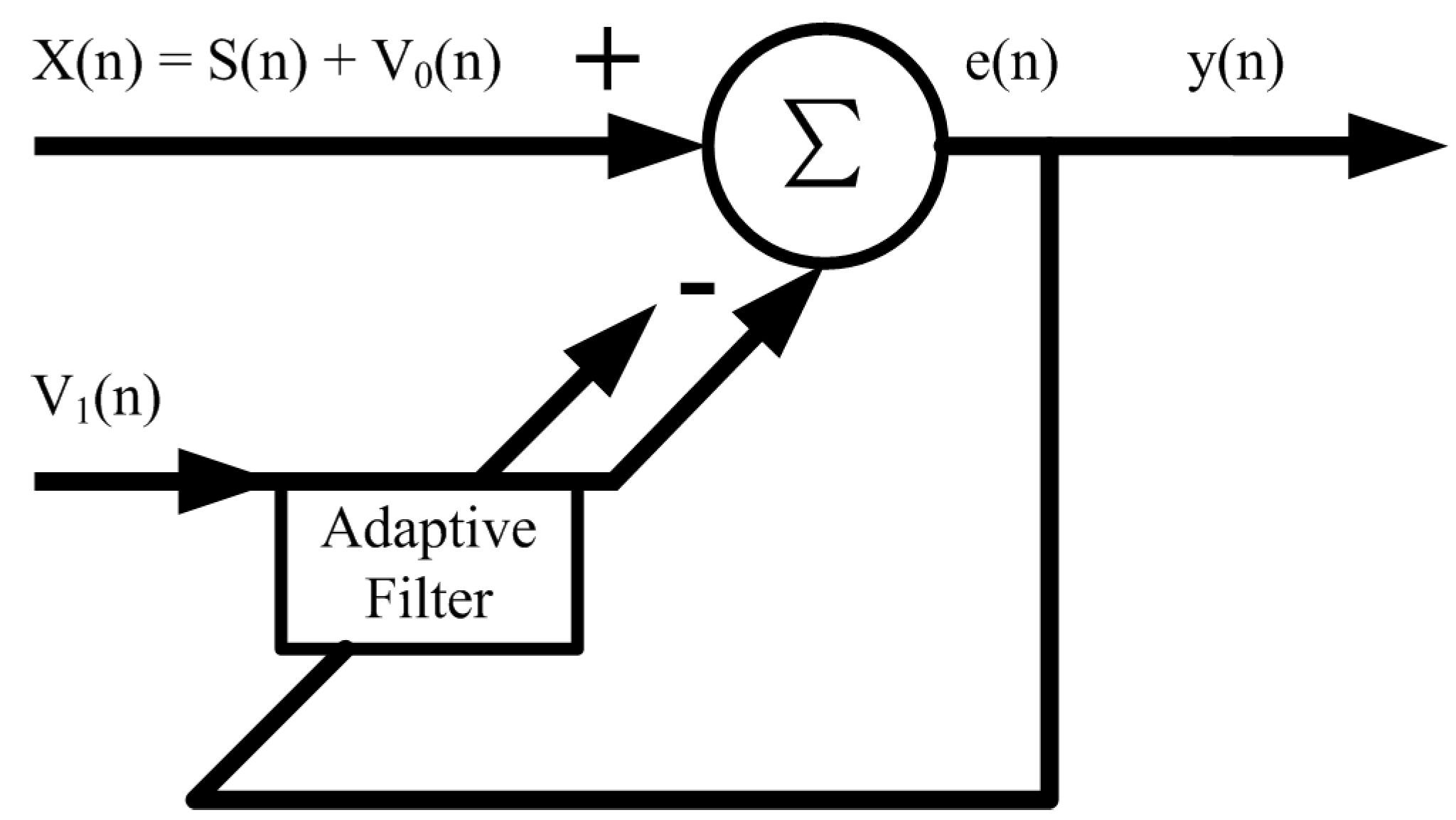
2. Proposed Technique for Adaptive Interference Cancellation
2.1. Adaptive Noise Cancellation Based on LMS Algorithm
- The initial value is set to start the default weight coefficient vector.
- Calculate the output signal of the adaptive FIR filter, wherein the order is L − 1:
- Estimate the error of the current time n:
- Use the steepest descent LMS algorithm to adjust the weight vector of the filter continuously:
- Verify whether the standard deviation of the standard error has been satisfied. If it is, immediately stop iteration; otherwise, continue to the following operation.
2.2. NLMS Algorithm Based on Symbol Function
2.3. Normalized BLMS Algorithm Based on Symbol Function
3. Implementation
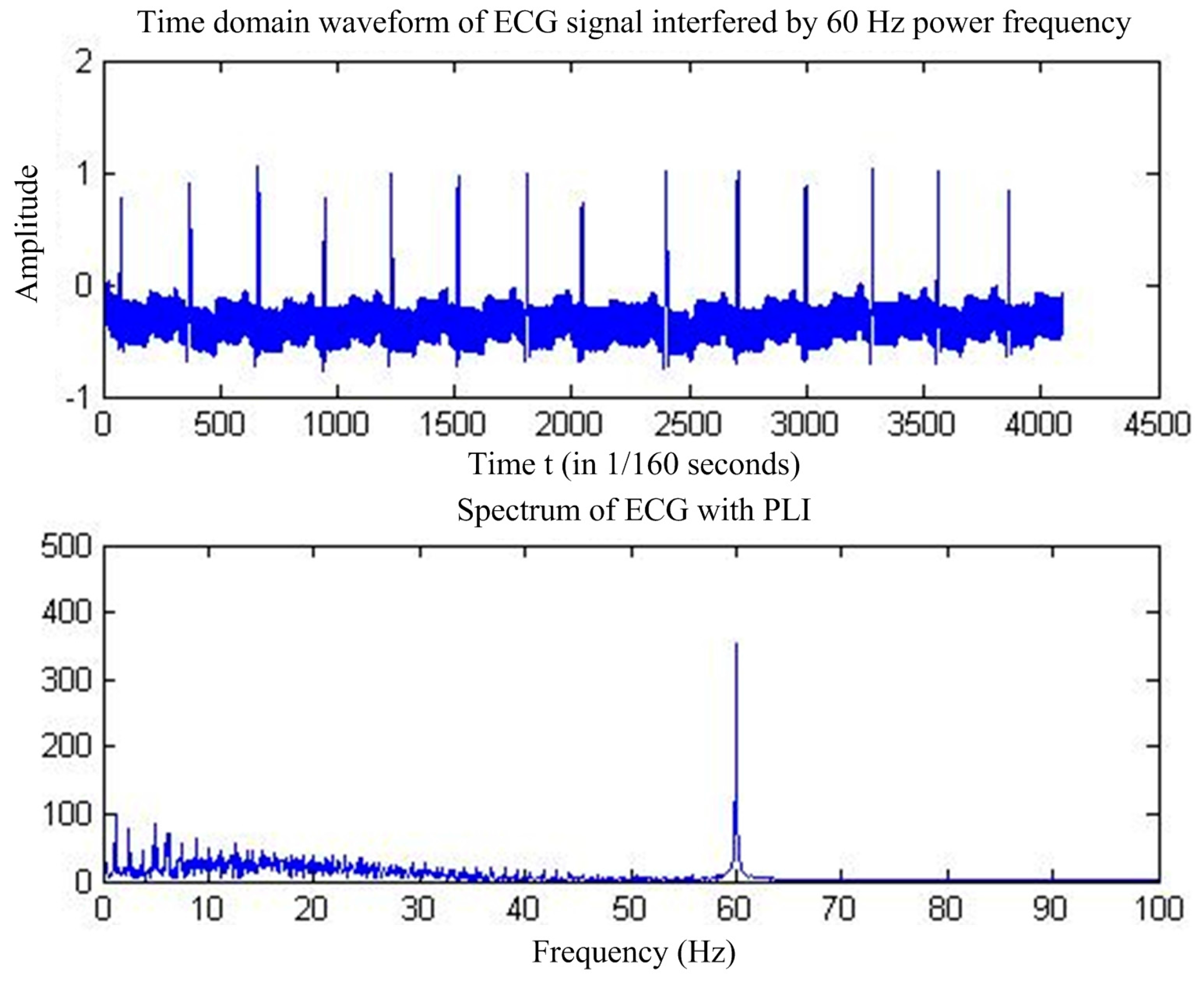
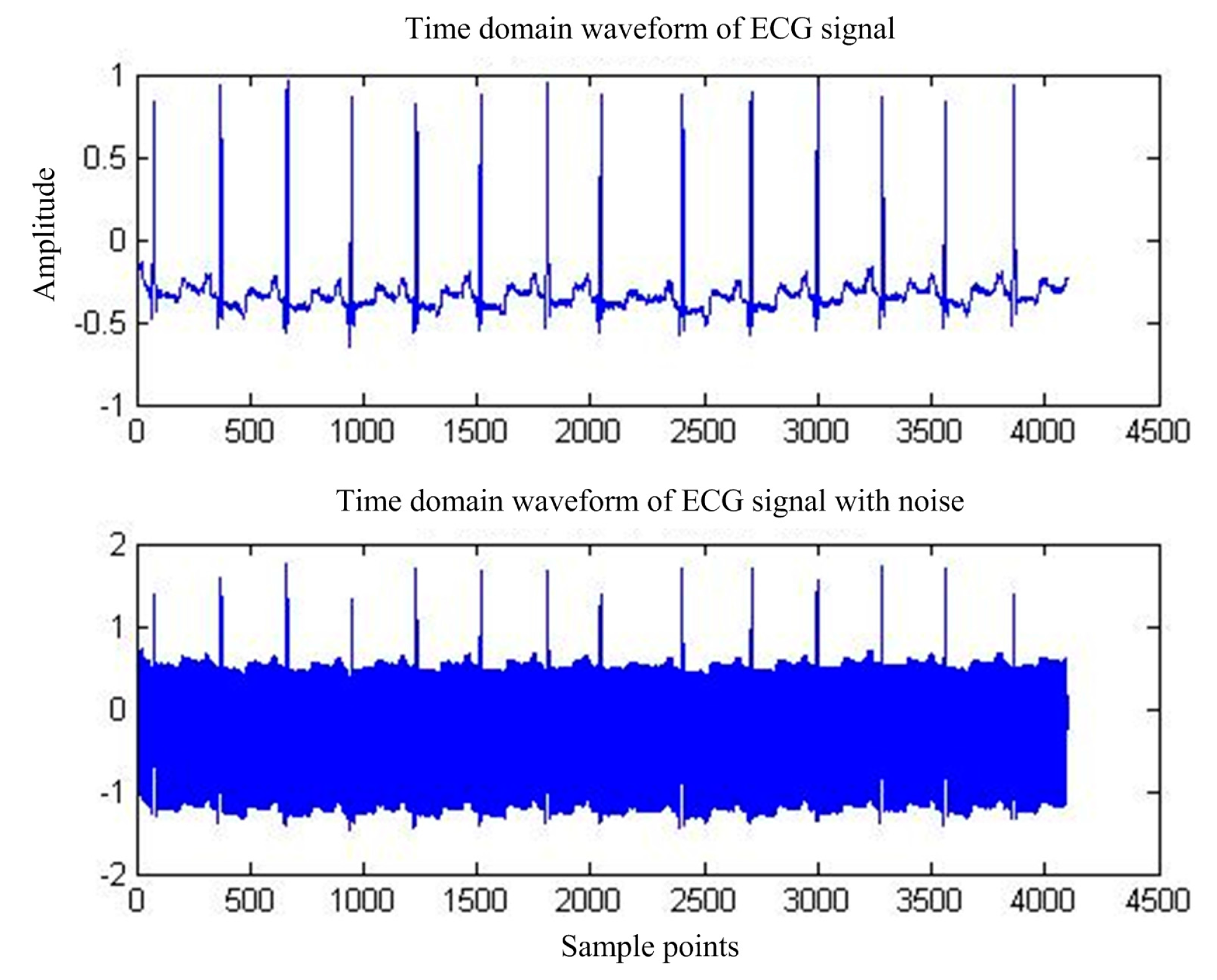
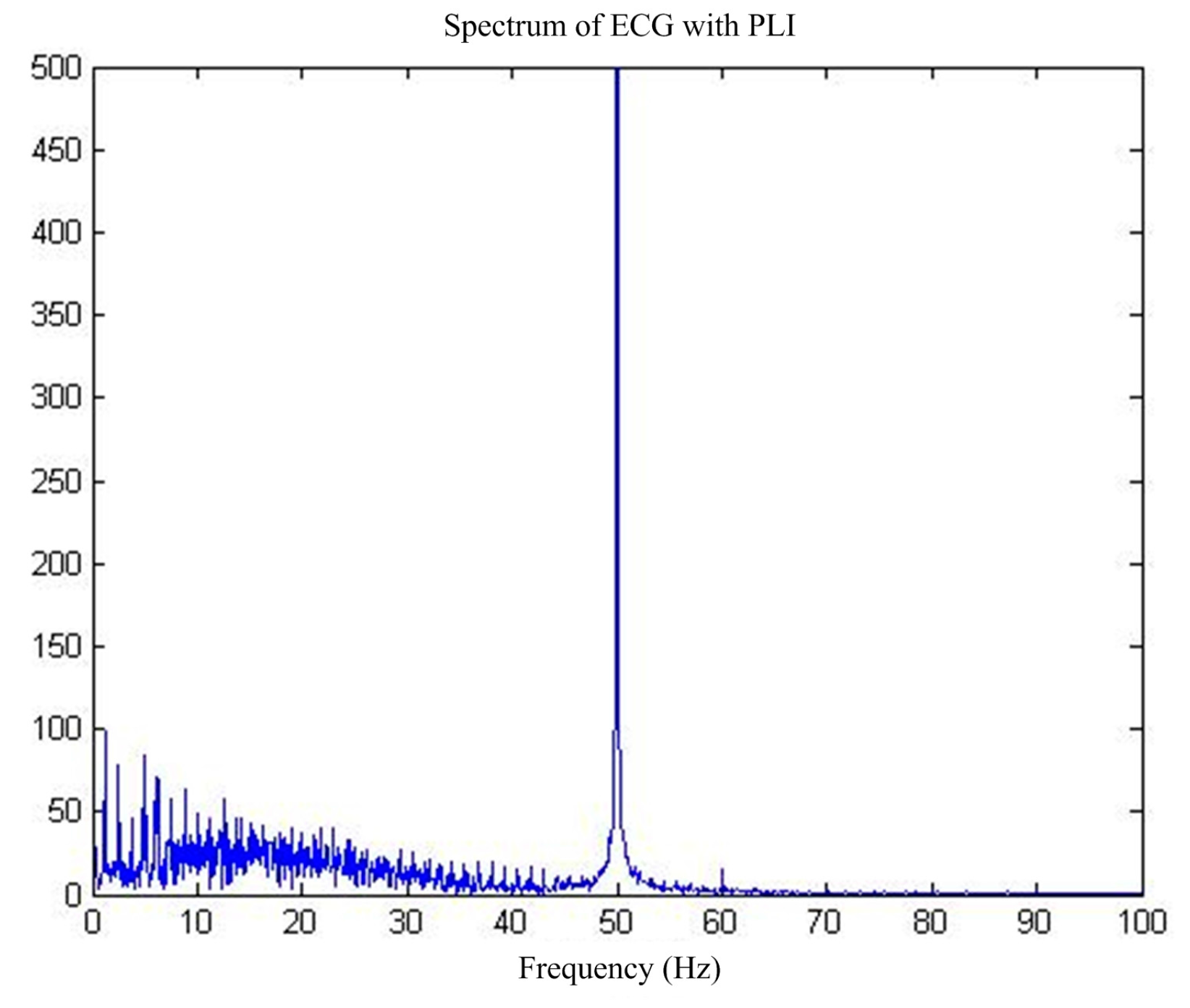
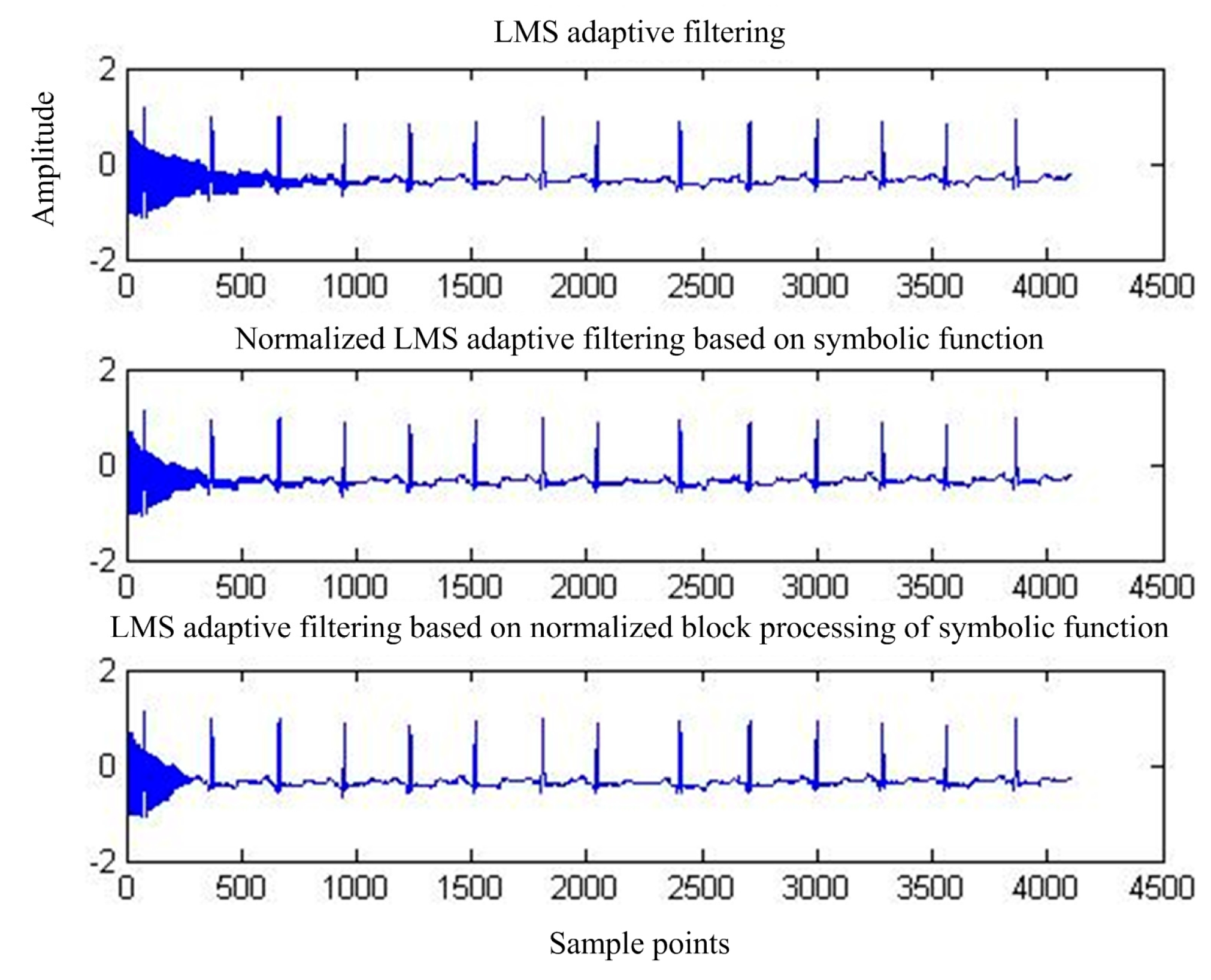
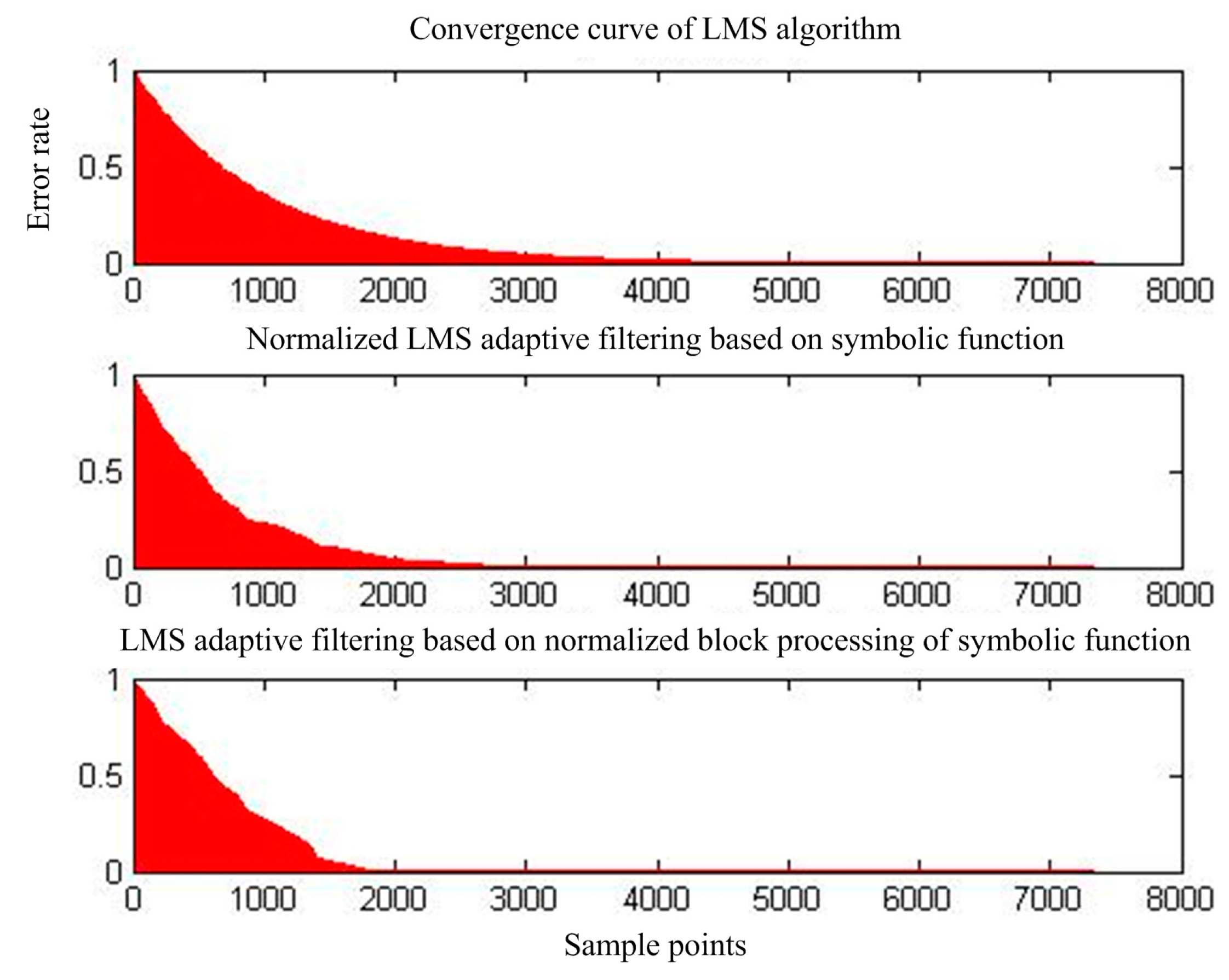
3.1. Adaptive Interference Cancellation to Remove Power Frequency Interference
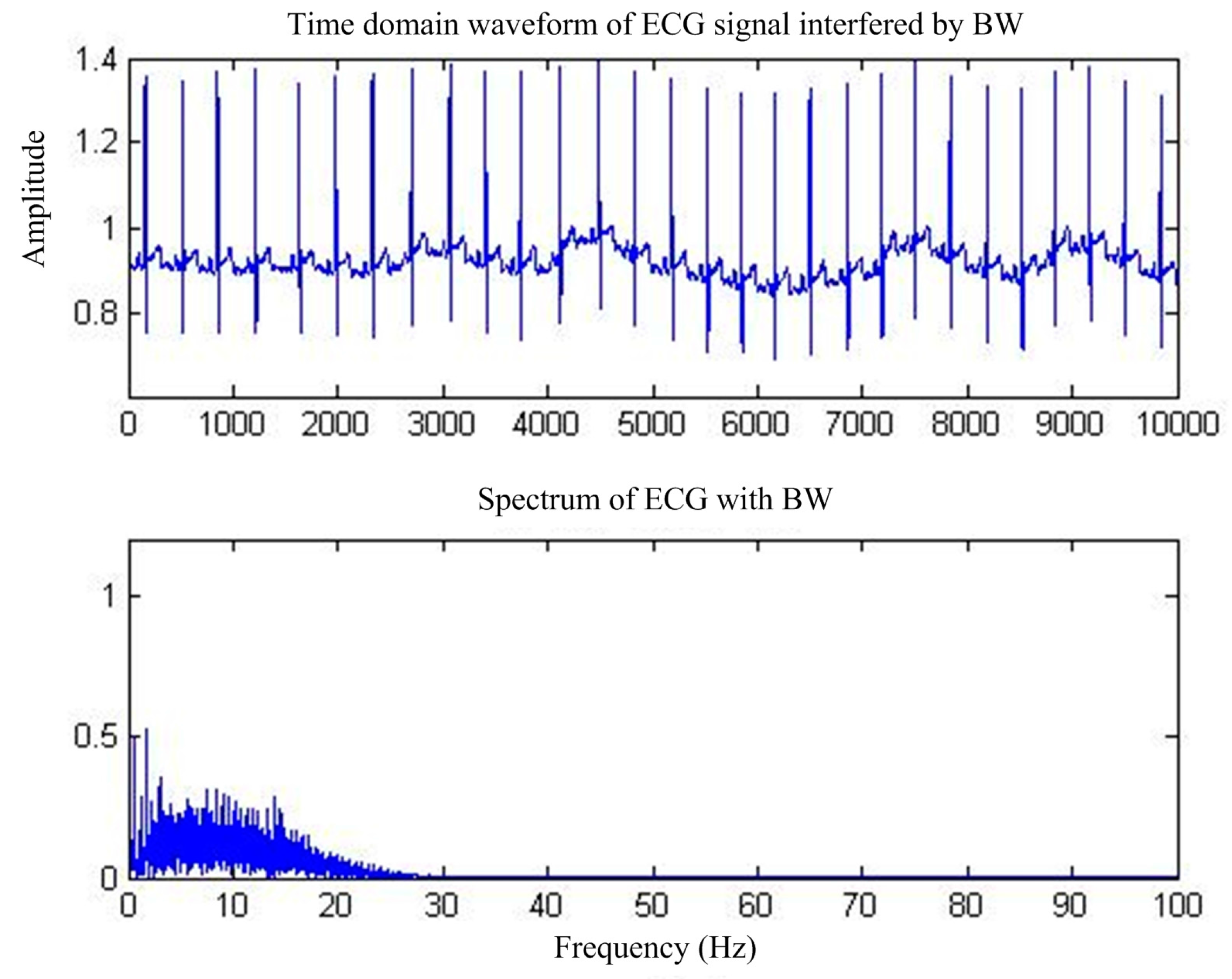
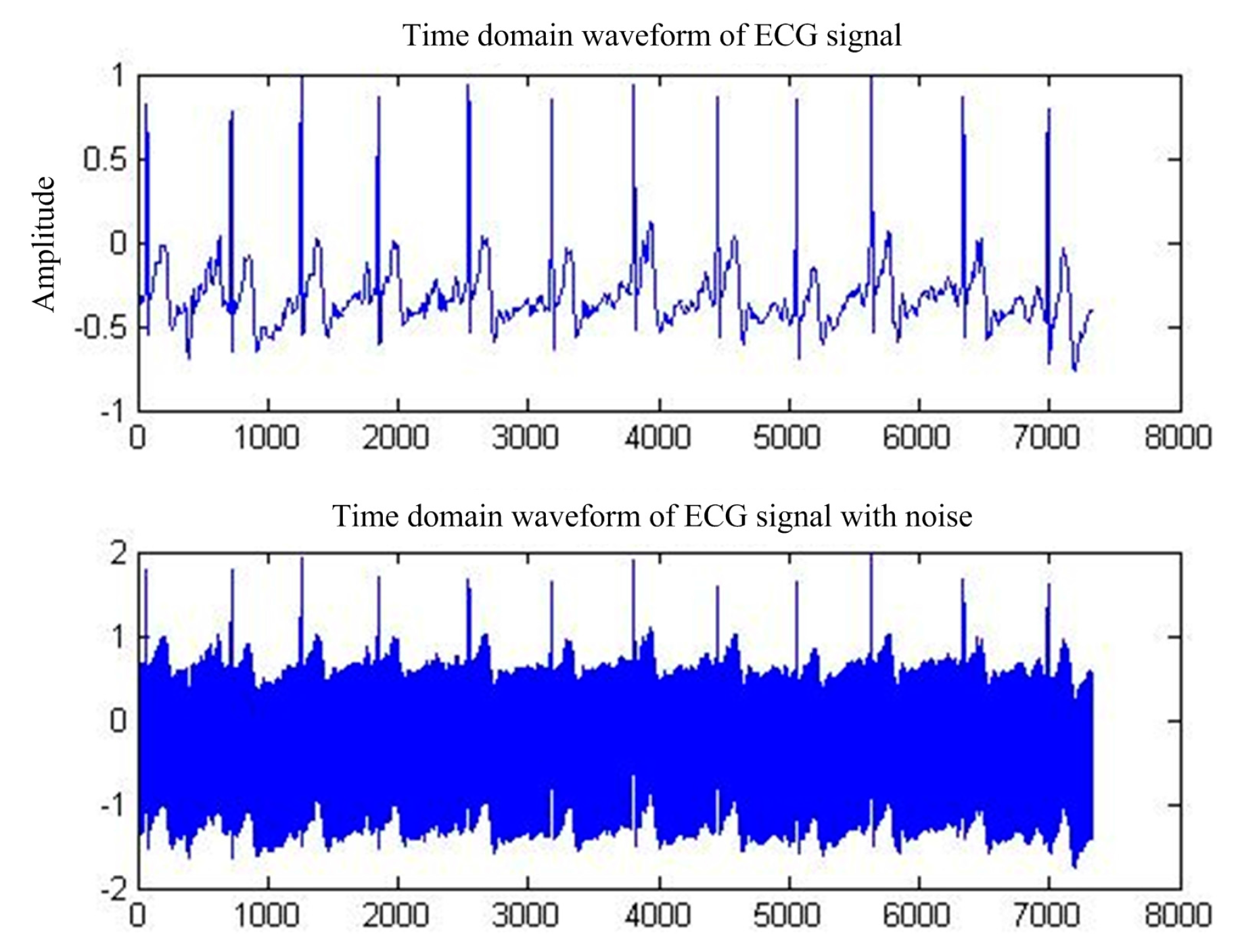
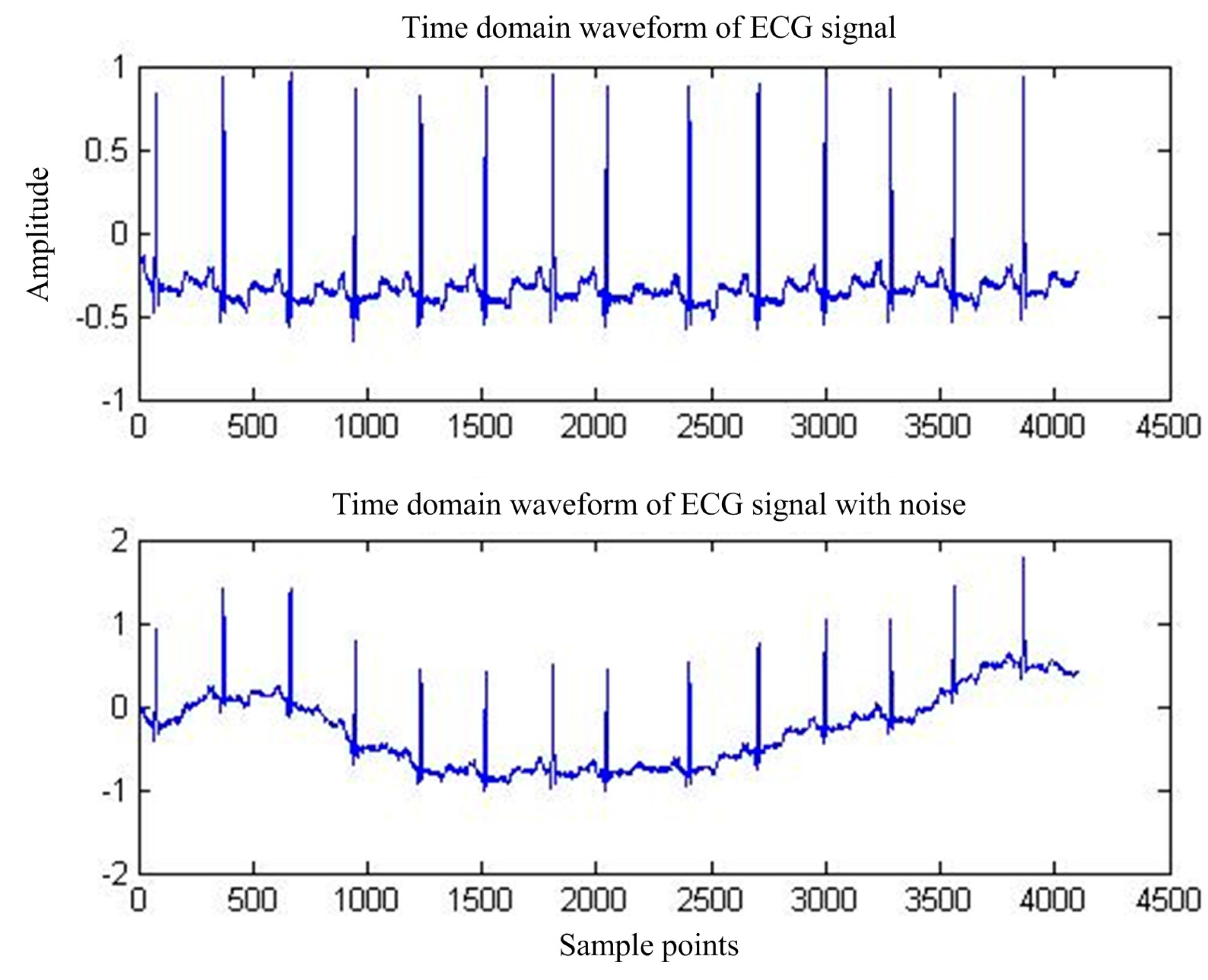
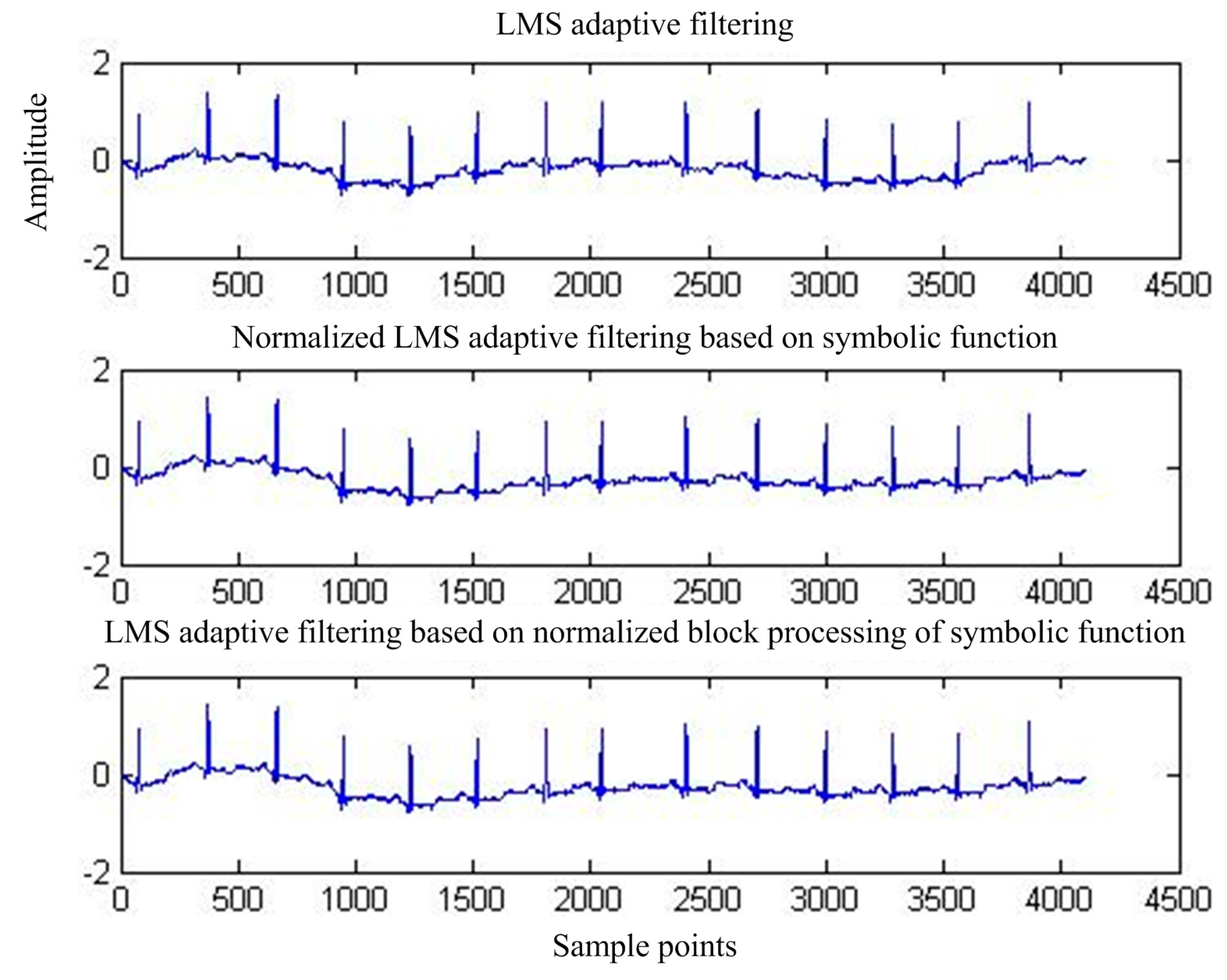
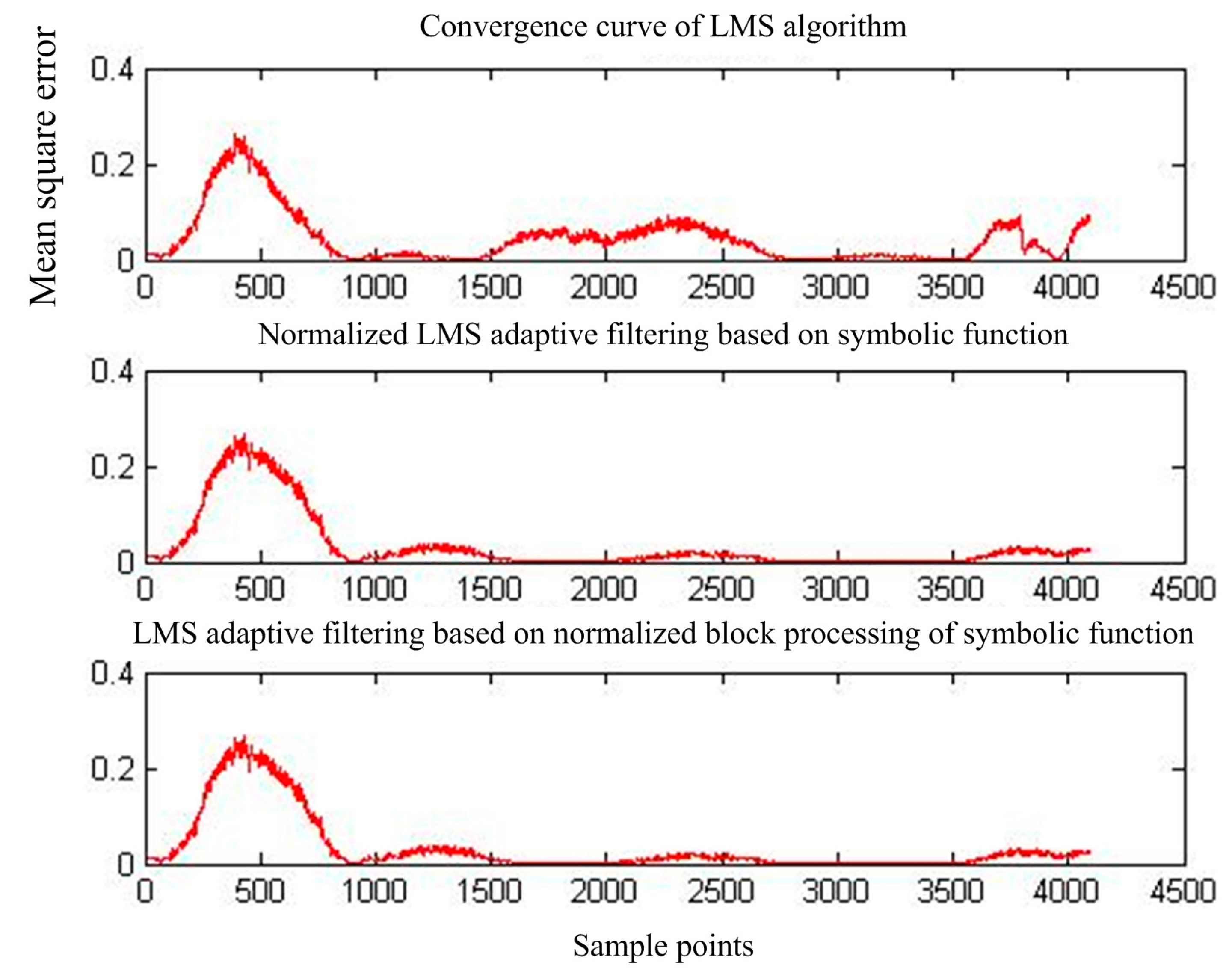
3.2. Adaptive Interference Cancellation Removes BW
4. Conclusions and Analysis
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Sufi, F.; Qiang, F.; Khalil, I.; Mahmoud, S.S. Novel methods of faster cardiovascular diagnosis in wireless telecardiology. IEEE J. Sel. Areas Commun. 2009, 27, 537–552. [Google Scholar] [CrossRef]
- Gravina, R.; Alinia, P.; Ghasemzadeh, H.; Fortino, G. Multi-sensor fusion in body sensor networks: State-of-the-art and research challenges. Inf. Fusion 2017, 35, 68–80. [Google Scholar] [CrossRef]
- Fortino, G.; Giannantonio, R.; Gravina, R.; Kuryloski, P.; Jafari, R. Enabling Effective Programming and Flexible Management of Efficient Body Sensor Network Applications. IEEE Trans. Hum. Mach. Syst. 2013, 43, 115–133. [Google Scholar] [CrossRef]
- Lin, Y.D.; Hu, Y.H. Power-line interference detection and suppression in ECG signal processing. IEEE Trans. Biomed. Eng. 2008, 55, 354–357. [Google Scholar] [CrossRef] [PubMed]
- Kiremire, B.; Marwala, T. Nonstationarity detection: The use of the cross correlation integral in ECG, and EEG profile analysis. In Proceedings of the Congress on Image and Signal Processing (CISP’08), Sanya, China, 27−30 May 2008; pp. 373–378. [Google Scholar]
- Bhavani Sankar, A.; Kumar, D.; Seethalakshmi, K. Performance Study of Various Adaptive Filter Algorithms for Noise Cancellation in Respiratory Signals. Signal Process. Int. J. 2010, 4, 267–278. [Google Scholar]
- Covello, R.; Fortino, G.; Gravina, R.; Aguilar, A.; Breslin, J.G. Novel method and real-time system for detecting the Cardiac Defense Response based on the ECG. In Proceedings of the 2013 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Gatineau, QC, Canada, 4–5 May 2013; pp. 53–57. [Google Scholar]
- Leski, J.M.; Henzel, N. ECG Baseline Wander Powerline Interface Reduction Using Nonlinear Filter Bank. Signal Process. 2004, 35, 781–793. [Google Scholar]
- Blanco-Velasco, M.; Weng, B.; Barner, K.E. ECG Signal Denoising and Baseline Wander Correction Based on the Empirical Mode Decomposition. Comput. Biol. Med. 2008, 38, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Gravina, R.; Fortino, G. Automatic Methods for the Detection of Accelerative Cardiac Defense Response. IEEE Trans. Affect. Comput. 2016, 7, 286–298. [Google Scholar] [CrossRef]
- Singh, S.; Yadav, K.L. Performance evaluation of different adaptive filters for ECG signal processing. Int. J. Comput. Sci. Eng. 2010, 40, 1880–1883. [Google Scholar]
- Esposito, A.; D’Andria, P. An Adaptive Learning Algorithm for ECG Noise and Baseline Drift Removal. In Italian Workshop on Neural Nets; Springer: Berlin/Heidelberg, Germany, 2003; pp. 139–147. [Google Scholar]
- Sayadi, O.; Shamsollahi, M.B. ECG Denoising and Compression Using a Modified Extended Kalman Filter Structure. IEEE Trans. Biomed. Eng. 2008, 55, 2240–2248. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Ahmad, I.; Rai, P. Signal Processing of ECG Using Matlab. Int. J. Sci. Res. Publ. 2012, 12, 601–604. [Google Scholar]
- Jagtap, S.K.; Chavan, M.S.; Wagvekar, R.C.; Uplane, M.D. Application of the digital filter for noise reduction in electrocardiogram. J. Instrum. 2010, 40, 83–86. [Google Scholar]
- Koike, S. Analysis of adaptive filters using normalized signed regressor LMS algorithm. IEEE Trans. Signal Process. 1999, 47, 2710–2723. [Google Scholar] [CrossRef]
- Eweda, E. Analysis and design of a signed regressor LMS algorithm for stationary and nonstationary adaptive filtering with correlated Gaussian data. IEEE Trans. Circuits Syst. 1990, 37, 1367–1374. [Google Scholar] [CrossRef]
- Rahman, M.Z.U.; Shaik, R.A.; Reddy, D.R.K. Efficient sign based normalized adaptive filtering techniques for cancelation of artifacts in ECG signals: Application to wireless biotelemetry. Signal Process. 2011, 91, 225–239. [Google Scholar] [CrossRef]









| Algorithm Name | Times of Multiply-Add Operation | Times of Division |
|---|---|---|
| Basic LM Salgorithm | L + 1 | 0 |
| NLMS algorithm based on symbol function | 1 | 1 |
| Normalized BLMS algorithm based on symbol function | 1 | 1 |
| Algorithm Name | Before Filtering SNR (dB) | After Filtering SNR (dB) | SNRI (dB) |
|---|---|---|---|
| Basic LMS algorithm | −13.5234 | 19.6638 | 33.1872 |
| NLMS algorithm based on symbol function | −13.5234 | 23.3935 | 36.9168 |
| Normalized BLMS algorithm based on symbol function | −13.5234 | 23.4859 | 37.0093 |
| Algorithm Name | BeforeFiltering SNR(dB) | AfterFiltering SNB(dB) | SNRI (dB) |
|---|---|---|---|
| Basic LMS algorithm | −12.600 | 7.4272 | 20.027 |
| NLMS algorithm based on symbol function | −12.600 | 10.973 | 23.572 |
| Normalized BLMS algorithm based on symbol function | −12.600 | 10.672 | 23.271 |
| Algorithm Name | Before Filtering SNR (dB) | AfterFiltering SNR (dB) | SNRI (dB) |
|---|---|---|---|
| Basic LMS algorithm | −3.2003 | 9.3806 | 12.5809 |
| NLMS algorithm based on symbol function | −3.2003 | 12.6214 | 15.8217 |
| Normalized BLMS algorithm based on symbol function | −3.2003 | 12.6334 | 15.8337 |
| Algorithm Name | Before Filtering SNR (dB) | After Filtering SNR (dB) | SNRI (dB) |
|---|---|---|---|
| Basic LMS algorithm | −2.7754 | 11.1474 | 13.9228 |
| NLMS algorithm based on symbol function | −2.7754 | 13.8366 | 16.6120 |
| Normalized BLMS algorithm based on symbol function | −2.7754 | 13.8404 | 16.6158 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ren, A.; Du, Z.; Li, J.; Hu, F.; Yang, X.; Abbas, H. Adaptive Interference Cancellation of ECG Signals. Sensors 2017, 17, 942. https://doi.org/10.3390/s17050942
Ren A, Du Z, Li J, Hu F, Yang X, Abbas H. Adaptive Interference Cancellation of ECG Signals. Sensors. 2017; 17(5):942. https://doi.org/10.3390/s17050942
Chicago/Turabian StyleRen, Aifeng, Zhenxing Du, Juan Li, Fangming Hu, Xiaodong Yang, and Haider Abbas. 2017. "Adaptive Interference Cancellation of ECG Signals" Sensors 17, no. 5: 942. https://doi.org/10.3390/s17050942





